Abstract
Atrial fibrillation (AF) is the most common arrhythmia worldwide and a potent independent risk factor for stroke. This study aimed to determine the prevalence of AF in a population-based sample of adults in a rural region of Korea. Between January 2005 and December 2009, 4,067 individuals (60.2 ± 11.2 yr old, M: F = 1,582:2,485) over 21 who were residents of the county of Yangpyeong, Korea, participated in the study. AF was assessed on a resting 12-lead electrocardiogram (ECG) in 4,053 of the participants. Blood tests and transthoracic echocardiography (TTE) were also performed to investigate the relationship between left ventricular mass and AF in the study group. Fifty-four cases (32 men) were diagnosed as AF among the 4,053 subjects. The crude prevalence of AF was 1.3%. It was highest (2.3%) among sixty- and seventy- year olds, and higher in men than women in all age groups over 50. The prevalence in men was 2.0%, and in women 0.9%. In univariate analysis, age, male gender, body mass index, total serum cholesterol, alanine transaminase, serum creatinine, adiponectin level, and ischemic heart disease were associated with AF. Among the TTE parameters, systolic and diastolic left ventricular systolic internal dimension (LVID), and LV ejection fraction were associated with AF. In this relatively healthy population in a rural area of Korea, the prevalence of AF is 1.3%, and increases with age. Of the TTE parameters, systolic and diastolic LVID and left atrial diameter are related to prevalence of AF.
Graphical Abstract
Keywords: Atrial Fibrillation, Prevalence, Electrocardiography, Echocardiography, Community-based Cohort
INTRODUCTION
Atrial fibrillation (AF) is the most common sustained arrhythmia in clinical practice. Its prevalence in the western world is increasing (1,2). The lifetime risk of developing AF is approximately 25%, and it mainly affects the elderly. The reason for the increase in prevalence has not yet been fully determined. We guess that the main reasons include the aging population and longer survival from other cardiovascular diseases. Therefore, the increased awareness of AF events could play an important role in reducing cardiovascular mortality and morbidity. Epidemiological studies in Europe and North America have shown that the prevalence of AF increases with age, from less than 1% in the under 60s to approximately 10% in the over 80s (3,4). Data from Asian countries such as Japan (5) and Singapore (6) point to a lower frequency of AF than in Western countries.
The economic burden of AF in Korea is increasing substantially and presents a problem in planning the national health care system. In Korea AF is diagnosed by a screening programming according to several criteria. In other countries including Europe, data on AF has been obtained mainly from registries and hospital databases. Studies of the incidence of AF in Korea have been limited to hospitals and national health insurance cooperation data (7) and may underestimate the actual burden of AF. To our knowledge, no data on the prevalence of AF in nonhospitalized participants and the associated echocardiographic factors are available in Korea. The aim of this study was to assess the prevalence of AF and the known risk factors for stroke in the YangPyeong Cardiovascular Disease Cohort (YPCDC) in a healthy rural population.
MATERIALS AND METHODS
Study participants
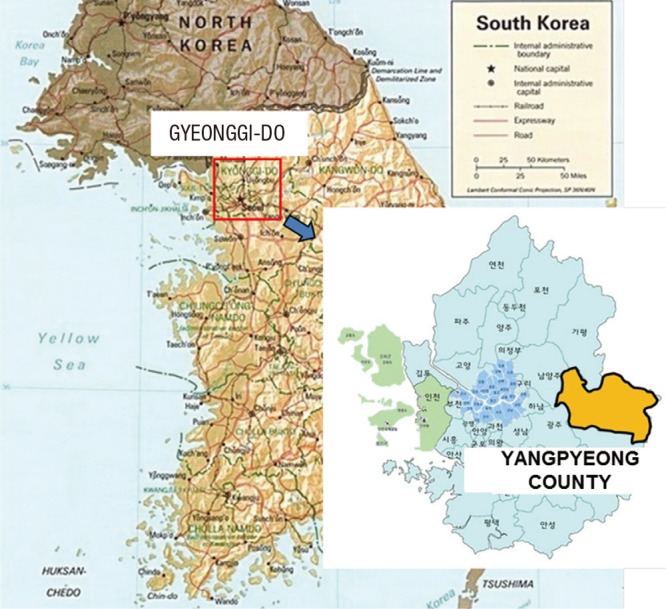
The YPCDC is a longitudinal community-based cohort established within a multi-rural community project, which is part of the Korean Genetic Epidemiology Study funded by the Korean Centers for Disease Control and Prevention. It is a prospective population-based investigation of risk factors for AF in men and women ≥ 21 yr old. We enrolled 4,070 adult residents in Yangpyeong county (Fig. 1) who participated in this cohort from 2004 to 2008. Total populations of Yangpyeong county were 75,314 in 2005 and 82,802 in 2010 from Population and Housing Census data. We included all residents who were relatively asymptomatic healthy participants and underwent both electrocardiographic examination and serum blood test. Otherwise, we excluded 17 out of the 4,070 residents because of the absence of electrocardiography (ECG) data. Therefore, a total of 4,053 residents (mean age: 60.2±11.2 yr old; 1,582 men) participated in the present investigation. The majority of the subjects were farmers and housewives. A questionnaire about health status including past medical history and family history was filled out by the participants. Information on demographics, smoking, alcohol intake, medical history, and medications were collected using the questionnaire administered by well-trained interviewers. Among them, 943 participants answered questions about their medical history: hypertension, diabetes mellitus, hypercholesterolemia, ischemic heart disease, and stroke, as well as smoking and drinking status. All the participants underwent physical examinations, including blood pressure measurements, ECG, and blood tests after fasting for at least 8 hr (total cholesterol, serum fasting glucose, high density lipoprotein, triglycerides, serum uric acid, liver enzyme, blood urea nitrogen, serum creatinine, C-reactive protein, serum insulin, and adiponectin) which were analyzed by an ADVIA1650 Automatic Analyzer (Siemens, New York, NY, USA). Blood pressure was measured to the nearest 2 mmHg with a standard mercury sphygmo-manometer (Baumanometer) using the first and fifth Korotkoff sounds. Standardized measurements were performed with the participants seated after a five minutes rest, and were repeated three times at five minute intervals. For the analysis the mean of the second and third of the three BP measurements was calculated; however, if the difference was larger than 5 mmHg, up to five additional measurements were made, and the last two values were averaged. Body mass index was calculated as weight in kilograms divided by height in meters squared. Cardiovascular risk factors were defined as (7) 1) hypertension; use of antihypertensive medications, systolic blood pressure≥140 mmHg, or diastolic blood pressure≥90 mmHg; 2) diabetes mellitus; use of oral hypoglycemic agents or treatment by insulin injection at the current examination, fasting blood glucose≥126 mg/dL; 3) hypercholesterolemia; use of antihyperlipidemic agents or serum total cholesterol >220 mg/dL. Present illnesses were identified through medical interviews by physicians or survey interviewers. Clinical cardiovascular disease at baseline was defined by any of the following: a history of myocardial infarction, angina, stroke, and congestive heart failure.
Fig. 1. The location of Yangpyeong-gun in northeast of Korea.
Electrocardiographic and echocardiographic examination
A portable ECG machine was used to make 12 lead resting surface ECGs to detect AF, and all ECG records were reviewed by a physician.
AF was defined as disorganized atrial activity without discrete P waves, atrial activation ranging from 350 to 600 beats per minute, and irregularly irregular ventricular response.
The echocardiographic examination consisted of a standard 2-dimensional echocardiogram, including M-mode and Doppler echocardiography Sonos 2500 (Hewlett-Packard Co) during continuous ECG monitoring according to the American Society of Echocardiography guidelines; it was performed by a well-trained cardiologist and all records were reviewed and measured by the same physician. The exclusion criteria for echocardiography were poor acoustic window, dextrocardia, history of open heart surgery, and oblique M-mode interrogation angle >10° on the vertical axis of the left ventricle. Details have been given previously (8). The investigators who performed the echocardiographic measurements and the reviewer were independent observers blinded to participants' characteristics. This study was approved by the research ethics committee of Hanyang University Hospital, and written informed consent was obtained from each participant before the examination.
Statistical analysis
Continuous variables are presented as mean and standard deviation, categorical variables as observed number of participants and percentages. We used an independent t-test after performing Levene's test for equality of variances to compare all continuous variables. Categorical variables were tested with the chi-square and Fisher's exact tests. All parameters with a P value<0.1 resulting from the univariate comparisons were included in a multiple logistic regression model. Another logistic model was used to explore the association between AF and stroke, where the dependent variable was stroke (yes/no) and the independent variables based on previous studies (9) included age, diabetes, hypertension, dyslipidemia, smoking, and drinking. The criterion for inclusion of a variable in the regression model was P<0.05, and that for exclusion was P>0.10. Statistical analysis was performed with SPSS statistical software (SPSS Inc., release 15.0) and statistical significance was assumed at P<0.05. All tests were two-sided.
Ethics statement
The institutional review board of Hanyang University College of Medicine reviewed and approved the protocol of this study (IRB approval number; 2010-R-31). Written informed consent was obtained from each participant before the examination.
RESULTS
Prevalence of a trial fibrillation
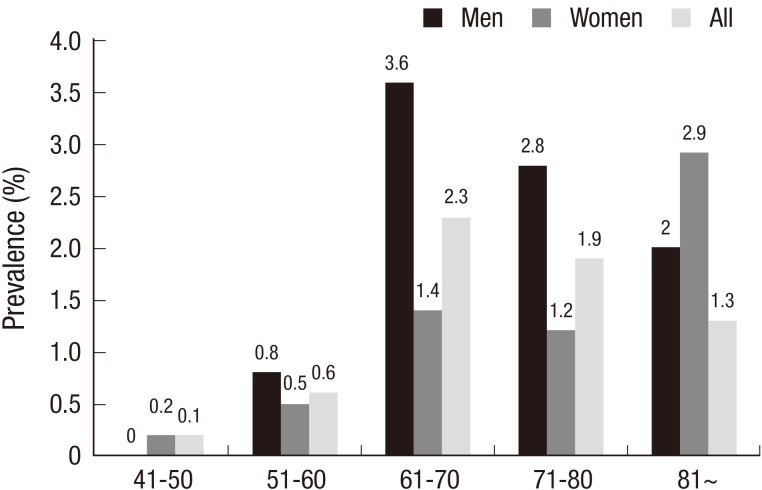
Among the 4,053 survey participants, the crude overall prevalence of AF was 1.3% (n=54). It was higher in men (2.0%) than in women (0.9%), and there was a nonlinear increase with age in both men and women. The crude prevalence was highest between ages 61 and 70 in both genders (3.6% in men, 1.4% in women), and higher in those aged 41 to 70 than below 41 in both genders. The crude prevalence of AF in men was higher than that in women except for the 41-50 age group and those over 81. The crude overall AF prevalence was 0.6% in the 51 to 60 group, 2.3% in the 61 to 70 group, 1.9% in the 71 to 80 group, and 1.3% in those over 81 (Fig. 2). When age was adjusted on the basis of Korean age composition data (2005 National Population Census), the combined age-standardized prevalence of AF in Korea (≥40 yr) was 0.36% (0.45% for men and 0.32% for women).
Fig. 2. The crude atrial fibrillation prevalence in men, women, and overall groups according to age respectively.
Clinical demographic and echocardiographic parameters
Baseline characteristics and the results of the univariate analysis are presented in Tables 1 and 2. Of the demographic and blood test factors, age, male gender, body mass index, total serum cholesterol, serum uric acid, alanine transaminase, serum creatinine, and adiponectin level were related to AF (Table 1). Among the classical risk factors including smoking and alcohol status, congestive heart failure and ischemic heart disease were also related to AF (Table 2) as were the echocardiographic parameters, systolic and diastolic left ventricular internal dimensions, left atrial (LA) diameter, peak early rapid filling wave velocity (E), and LV ejection fraction (Table 3).
Table 1. Clinical characteristics and blood tests of study participants with and without atrial fibrillation.
| Characteristics | Non-AF cases (n = 3,999) | AF cases (n = 54) | P value |
|---|---|---|---|
| Age | 60.1 ± 11.2 | 67.0 ± 7.7 | < 0.001 |
| Male (%) | 1544 (38.6%) | 32 (59.3%) | 0.002 |
| Body mass index (kg/m2) | 24.5 ± 3.2 | 23.5 ± 3.2 | 0.024 |
| Waist circumference (cm) | 86.1 ± 8.8 | 86.8 ± 8.5 | 0.579 |
| Systolic blood pressure (mmHg) | 124.0 ± 19.6 | 122.9 ± 18.2 | 0.688 |
| Diastolic blood pressure (mmHg) | 79.4 ± 14.7 | 79.8 ± 10.0 | 0.838 |
| Heart rate (beats/min) | 68.4 ± 9.7 | 68.8 ± 12.9 | 0.810 |
| Total serum cholesterol (mg/dL) | 195.7 ± 37.4 | 184.1 ± 34.1 | 0.023 |
| HDL (mg/dL) | 45.6 ± 11.1 | 44.2 ± 11.7 | 0.337 |
| Triglycerides (mg/dL) | 149.0 ± 89.1 | 137.1 ± 64.4 | 0.329 |
| Blood glucose (mg/dL) | 102.7 ± 25.1 | 108.0 ± 26.9 | 0.120 |
| Serum uric acid (mg/dL) | 4.9 ± 1.4 | 5.5 ± 1.8 | 0.012 |
| Aspartate transaminase (U/L) | 26.2 ± 13.0 | 25.9 ± 8.2 | 0.864 |
| Alanine transaminase (U/L) | 23.8 ± 14.1 | 21.0 ± 7.8 | 0.011 |
| Blood urea nitrogen (mg/dL) | 15.1 ± 4.4 | 16.0 ± 4.6 | 0.139 |
| Creatinine (mg/dL) | 0.94 ± 0.21 | 1.02 ± 0.18 | 0.010 |
| C-reactive protein (mg/dL) | 1.60 ± 2.56 | 1.81 ± 2.75 | 0.563 |
| Serum Insulin, fasting (µU/mL) | 10.2 ± 5.3 | 9.5 ± 4.9 | 0.424 |
| Adiponectin (µg/mL) | 8.09 ± 4.81 | 10.13 ± 5.82 | 0.017 |
Data are presented as mean±standard deviations. AF, atrial fibrillation; HDL, high-density lipoprotein.
Table 2. Relationship between underlying risk factors and prevalence of atrial fibrillation.
| Characteristics | No. (%) of cases | P value | |
|---|---|---|---|
| Non-AF cases (n = 920) | AF cases (n = 23) | ||
| Hypertension | 519 (56) | 10 (44) | 0.217 |
| LVH in ECG | 69 (7.5) | 6 (26.1) | 0.001 |
| Diabetes Mellitus | 169 (18) | 5 (22) | 0.596* |
| Dyslipidemia | 30 (3) | 0 (0) | 1.000* |
| Stroke/TIA | 45 (5) | 0 (0) | 0.621* |
| CHF† | 58† (2) | 4† (11) | 0.005* |
| Ischemic heart disease | 59 (6) | 16 (70) | < 0.001 |
| Smoking‡ | 290‡ (16) | 6‡ (18) | 0.749 |
| Alcohol drinking‡ | 851‡ (47) | 15‡ (46) | 0.835 |
Data are presented as mean±standard deviations or number (percentage).
*Fisher's exact test; †in 3,322 of Non-AF cases and 38 of AF cases; ‡in 1,800 of Non-AF cases and 33 of AF cases. No., number; LVH, left ventricular hypertrophy; TIA, transient ischemic attack.
Table 3. Echocardiographic parameters comparison between the two groups of with and without atrial fibrillation.
| Echocardiographic parameters | Non-AF cases (n = 3,323) | AF cases (n = 39) | P value |
|---|---|---|---|
| IVSs (cm) | 1.41 ± 0.19 | 1.45 ± 0.16 | 0.277 |
| IVSd (cm) | 0.96 ± 0.15 | 0.99 ± 0.14 | 0.264 |
| LVIDs (cm) | 2.96 ± 0.41 | 3.26 ± 0.56 | 0.003 |
| LVIDd (cm) | 4.85 ± 0.47 | 5.05 ± 0.50 | 0.008 |
| LVPWs (cm) | 1.38 ± 0.17 | 1.40 ± 0.15 | 0.503 |
| LVPWd (cm) | 0.87 ± 0.12 | 0.90 ± 0.10 | 0.147 |
| Aortic dimension (cm) | 3.00 ± 0.32 | 3.08 ± 0.35 | 0.133 |
| LA diameter (cm) | 3.20 ± 0.43 | 3.81 ± 0.76 | < 0.001 |
| Peak E (cm/sec) | 70.7 ± 16.6 | 85.9 ± 19.2 | < 0.001 |
| Peak A (cm/sec) | 77.5 ± 17.0 | 85.9 ± 24.1 | 0.086 |
| Deceleration time (msec) | 197.8 ± 32.9 | 188.2 ± 34.0 | 0.317 |
| IVRT (msec) | 77.9 ± 12.6 | 75.2 ± 10.2 | 0.489 |
| LV ejection fraction (%) | 69.6 ± 6.7 | 65.3 ± 9.6 | 0.064 |
Data are presented as mean±standard deviations. AF, atrial fibrillation; IVSs, systolic interventricular septum thickness; IVSd, diastolic interventricular septum thickness; LVIDs, systolic left ventricular internal dimension; LVIDd, diastolic left ventricular internal dimension; LVPWs, systolic left ventricular posterior wall thickness; LVPWd, diastolic left ventricular posterior wall thickness; LA, left atrium; E, early rapid filling wave velocity; A, filling wave during atrial contraction velocity; IVRT, isovolumic relaxation time.
In a multivariate analysis, only ischemic heart disease (P= 0.002), LA diameter (P=0.006), and peak E (P=0.018) were significant risk factors for AF (Table 4).
Table 4. Risk factors for prevalence of atrial fibrillation.
| Variables | Odds ratio | (95% CI) | P value |
|---|---|---|---|
| Age (≥ 65) | 2.17 | (0.47, 10.07) | 0.320 |
| Male gender | 1.06 | (0.13, 9.01) | 0.956 |
| Body mass index (per kg/m2) | 0.76 | (0.57, 1.01) | 0.058 |
| LV ejection fraction (per %) | 0.92 | (0.84, 1.02) | 0.104 |
| Peak E (per cm/sec) | 1.05 | (1.01, 1.09) | 0.018 |
| LA diameter (per cm) | 6.59 | (1.72, 25.22) | 0.006 |
| Uric acid (per mg/dL) | 1.37 | (0.81, 2.34) | 0.243 |
| Creatinine (per mg/dL) | 0.03 | (0.01, 14.79) | 0.263 |
| Alanine transaminase (per U/L) | 1.00 | (0.95, 1.06) | 0.914 |
| Total cholesterol (per mg/dL) | 0.99 | (0.98, 1.01) | 0.413 |
| Adiponectin (per mg/dL) | 1.00 | (1.00, 1.00) | 0.878 |
| Ischemic heart disease | 9.73 | (2.30, 41.22) | 0.002 |
CI, confidence interval; LV, left ventricle; E, early rapid filling wave velocity; LA, left atrium.
Interestingly, in a multivariate analysis for stroke risk factors, neither age, gender, AF, diabetes, hypertension, hyperlipidemia, smoking, or drinking status were related to stroke events.
DISCUSSION
This present study is the first to investigate the prevalence of AF in a relatively healthy population group in a rural area of Korea and to include echocardiographic data in the analysis. This study is different from previous Korean study (7) in that the participants were relatively healthy population group who lives in rural area compared to previous study group in which all participants were over 40 and live in cities of Gyeongsangnam-do. And present study included echocardiographic data which was not included in previous Korean and other country studies. This inclusion criteria may have caused selection bias because all participants were asymptomatic disease-free population. This may be obstacle to our accurate analysis. We observed an AF prevalence of 1.3% for participants aged between 21 and 88. This figure is higher than in a previous Korean study in which all participants were over 40. The mean age of participants enrolled in the present study was 60.2±11.2, higher than in the previous study. AF is increasing all over the world, probably due to the aging of populations, and possibly related to exposure to risk factors. AF increased with age in this study, and depended on gender and ethnicity as in nearly all previous studies (4,10). Thus AF was higher in men (11,12) and increased with age in both men and women (13,14). The methods used to diagnose AF, such as 12-lead resting ECGs and review of medical records may influence the observed frequency of AF. Because we used one 12-lead resting ECG examination for all participants, we might miss some paroxysmal AF events, and this is a limitation of our study.
Interestingly, hypertension was not significantly associated with AF in our study. Hypertension is not always found to be a risk factor for AF in cross-sectional study despite its major contribution to AF in longitudinal studies. Moreover, anti-hypertensive medications such as angiotensin-receptor blockers, which are prescribed for patients with hypertension, are a mainstay of up-stream therapy to prevent AF nowadays, and may weaken the relationship between hypertension and AF. We also found no significant association between smoking and drinking and AF, unlike previous studies (15,16). This difference may be due to the cross-sectional design of our study and the different ethnicities of the participants.
The increase in the prevalence of ischemic heart disease (17,18,19) may contribute to an increase in AF. Ischemic heart disease was a significant risk factor for AF in our multivariate analysis.
In our univariate analysis, serum uric acid, alanine transaminase, serum creatinine, and adiponectin were related to AF, as in previous studies (20,21,22,23). Serum uric acid promotes inflammatory reactions by activating pro-inflammatory cytokines or by stimulating the rennin-angiotensin system. Much epidemiological evidence indicates that high levels of uric acid are associated with cardiovascular disease. Therefore, we suggest that uric acid promotes AF event by causing oxidative stress (20).
In previous retrospective studies of the relationship between AF and kidney dysfunction, AF was detected in 27% of patients with chronic kidney disease. This frequency was 3 to 15 times higher than in the Framingham population (24,25) and some authors have suggested that the effect on AF is attributable to inflammatory changes due to the reduced glomerular filtration rate (22).
The exact mechanism connecting adiponectin and AF is unclear. Adiponectin has anti-inflammatory, antihypertrophic, and atherogenic effects (26). Several clinical studies (27,28) and a cross-sectional study have shown that high concentrations of adiponectin are associated with AF (29). However, adiponectin was not a risk factor for AF in our multivariate analysis, and nor was the inflammatory marker, C-reactive protein. This could be due to the difference between our relatively healthy rural cohort and the participants in previous studies.
Our study is noteworthy in that we collected echocardiographic data on the participants to examine the relationships of this data with AF. To the best of our knowledge, no previous studies have done this in Asian population. We found that in univariate analysis, systolic and diastolic LVID, LA diameter, and peak E velocity differed significantly between the participants with and without AF. However in the multiple logistic regression model, only LA diameter and peak E velocity were risk factors for AF.
Several limitations to this study should be discussed. First, we failed to detect a significant association between AF and stoke. This result may be due to the relatively low number of participants diagnosed with strokes. Second, we made a single ECG recording for each participant and diagnosed AF based on this single recording. Therefore, we may have missed paroxysmal AF events in some participants, and this may have led us to underestimate the true prevalence of AF. Third, we collected and analyzed more echocardiographic participants (3,362) data than questionnaire (943) data. This may lead to missing data bias.
In conclusion, the crude prevalence of AF in a healthy population in a rural area of Korea is 1.3% overall, and tend to increase with age. Ischemic heart disease, peak E velocity, and LA diameter are independent risk factors for AF, whereas age, hypertension, and stroke are not.
Footnotes
DISCLOSURE: The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and coordination of the study: Park HC, Shin J. Design of ethical issues: all authors. Acquisition of data: Park HC, Kim MK, Choi BY. Data review: Park HC, Choi BY. Statistical analysis: Park HC, Shin J. Manuscript preparation: Park HC, Shin J. Revision of manuscript: Park HC, Park JK and Shin J. Manuscript approval: all authors.
Supplementary Material
Diagram of enrollment
References
- 1.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 2.Stefansdottir H, Aspelund T, Gudnason V, Arnar DO. Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. Europace. 2011;13:1110–1117. doi: 10.1093/europace/eur132. [DOI] [PubMed] [Google Scholar]
- 3.Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994-1998: analysis of data from the general practice research database. Heart. 2001;86:284–288. doi: 10.1136/heart.86.3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 5.Ohsawa M, Okayama A, Sakata K, Kato K, Itai K, Onoda T, Ueshima H. Rapid increase in estimated number of persons with atrial fibrillation in Japan: an analysis from national surveys on cardiovascular diseases in 1980, 1990 and 2000. J Epidemiol. 2005;15:194–196. doi: 10.2188/jea.15.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yap KB, Ng TP, Ong HY. Low prevalence of atrial fibrillation in community-dwelling Chinese aged 55 years or older in Singapore: a population-based study. J Electrocardiol. 2008;41:94–98. doi: 10.1016/j.jelectrocard.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Jeong JH. Prevalence of and risk factors for atrial fibrillation in Korean adults older than 40 years. J Korean Med Sci. 2005;20:26–30. doi: 10.3346/jkms.2005.20.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim YH, Kim YM, Shin J, Lee CH, Kim JH, Kim MK, Choi BY. Association of heart rate and left ventricular structure in a rural population in Korea. Clin Exp Hypertens. 2014;36:165–172. doi: 10.3109/10641963.2013.804540. [DOI] [PubMed] [Google Scholar]
- 9.Nicol MB, Thrift AG. Knowledge of risk factors and warning signs of stroke. Vasc Health Risk Manag. 2005;1:137–147. doi: 10.2147/vhrm.1.2.137.64085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schnabel RB, Wilde S, Wild PS, Munzel T, Blankenberg S. Atrial fibrillation: its prevalence and risk factor profile in the German general population. Dtsch Arztebl Int. 2012;109:293–299. doi: 10.3238/arztebl.2012.0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy NF, Simpson CR, Jhund PS, Stewart S, Kirkpatrick M, Chalmers J, MacIntyre K, McMurray JJ. A national survey of the prevalence, incidence, primary care burden and treatment of atrial fibrillation in Scotland. Heart. 2007;93:606–612. doi: 10.1136/hrt.2006.107573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, Stijnen T, Lip GY, Witteman JC. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27:949–953. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- 13.Langenberg M, Hellemons BS, van Ree JW, Vermeer F, Lodder J, Schouten HJ, Knottnerus JA. Atrial fibrillation in elderly patients: prevalence and comorbidity in general practice. BMJ. 1996;313:1534. doi: 10.1136/bmj.313.7071.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wheeldon NM, Tayler DI, Anagnostou E, Cook D, Wales C, Oakley GD. Screening for atrial fibrillation in primary care. Heart. 1998;79:50–55. doi: 10.1136/hrt.79.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Djoussé L, Levy D, Benjamin EJ, Blease SJ, Russ A, Larson MG, Massaro JM, D'Agostino RB, Wolf PA, Ellison RC. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am J Cardiol. 2004;93:710–713. doi: 10.1016/j.amjcard.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995;155:469–473. [PubMed] [Google Scholar]
- 17.Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, Wang CH, Heiss G. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339:861–867. doi: 10.1056/NEJM199809243391301. [DOI] [PubMed] [Google Scholar]
- 18.Brønnum-Hansen H, Jørgensen T, Davidsen M, Madsen M, Osler M, Gerdes LU, Schroll M. Survival and cause of death after myocardial infarction: the Danish MONICA study. J Clin Epidemiol. 2001;54:1244–1250. doi: 10.1016/s0895-4356(01)00405-x. [DOI] [PubMed] [Google Scholar]
- 19.Capewell S, Livingston BM, MacIntyre K, Chalmers JW, Boyd J, Finlayson A, Redpath A, Pell JP, Evans CJ, McMurray JJ. Trends in case-fatality in 117 718 patients admitted with acute myocardial infarction in Scotland. Eur Heart J. 2000;21:1833–1840. doi: 10.1053/euhj.2000.2318. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Uejima T, Oikawa Y, Koike A, Nagashima K, Kirigaya H, et al. Gender-specific relationship between serum uric acid level and atrial fibrillation prevalence. Circ J. 2012;76:607–611. doi: 10.1253/circj.cj-11-1111. [DOI] [PubMed] [Google Scholar]
- 21.Sinner MF, Wang N, Fox CS, Fontes JD, Rienstra M, Magnani JW, Vasan RS, Calderwood AH, Pencina M, Sullivan LM, et al. Relation of circulating liver transaminase concentrations to risk of new-onset atrial fibrillation. Am J Cardiol. 2013;111:219–224. doi: 10.1016/j.amjcard.2012.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iguchi Y, Kimura K, Kobayashi K, Aoki J, Terasawa Y, Sakai K, Uemura J, Shibazaki K. Relation of atrial fibrillation to glomerular filtration rate. Am J Cardiol. 2008;102:1056–1059. doi: 10.1016/j.amjcard.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 23.Rienstra M, Sun JX, Lubitz SA, Frankel DS, Vasan RS, Levy D, Magnani JW, Sullivan LM, Meigs JB, Ellinor PT, et al. Plasma resistin, adiponectin, and risk of incident atrial fibrillation: the Framingham Offspring Study. Am Heart J. 2012;163:119–124.e1. doi: 10.1016/j.ahj.2011.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–844. [PubMed] [Google Scholar]
- 25.Genovesi S, Pogliani D, Faini A, Valsecchi MG, Riva A, Stefani F, Acquistapace I, Stella A, Bonforte G, DeVecchi A, et al. Prevalence of atrial fibrillation and associated factors in a population of long-term hemodialysis patients. Am J Kidney Dis. 2005;46:897–902. doi: 10.1053/j.ajkd.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 26.Karmazyn M, Purdham DM, Rajapurohitam V, Zeidan A. Signalling mechanisms underlying the metabolic and other effects of adipokines on the heart. Cardiovasc Res. 2008;79:279–286. doi: 10.1093/cvr/cvn115. [DOI] [PubMed] [Google Scholar]
- 27.Ouchi N, Kihara S, Funahashi T, Nakamura T, Nishida M, Kumada M, Okamoto Y, Ohashi K, Nagaretani H, Kishida K, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation. 2003;107:671–674. doi: 10.1161/01.cir.0000055188.83694.b3. [DOI] [PubMed] [Google Scholar]
- 28.Weikert C, Westphal S, Berger K, Dierkes J, Möhlig M, Spranger J, Rimm EB, Willich SN, Boeing H, Pischon T. Plasma resistin levels and risk of myocardial infarction and ischemic stroke. J Clin Endocrinol Metab. 2008;93:2647–2653. doi: 10.1210/jc.2007-2735. [DOI] [PubMed] [Google Scholar]
- 29.Shimano M, Shibata R, Tsuji Y, Kamiya H, Uchikawa T, Harata S, Muto M, Ouchi N, Inden Y, Murohara T. Circulating adiponectin levels in patients with atrial fibrillation. Circ J. 2008;72:1120–1124. doi: 10.1253/circj.72.1120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagram of enrollment