Abstract
Background:
Gilles de la Tourette Syndrome (GTS) is a complex neuropsychiatric disorder, characterized by chronic motor and vocal tics, associated in 50–90% of cases with psychiatric comorbidities. Patients with moderate and severe clinical picture are treated with psychotherapy and pharmacological therapy. Deep brain stimulation (DBS) is reserved for pharmacological refractory GTS patients. As GTS tends to improve with time and potentially resolves in the second decade of life, the major concern of DBS in GTS is the age at which the patient undergoes surgical procedure. Some authors suggest performing DBS after 18 years, others after 25 years of age.
Case Description:
We present a 25-year-old patient with GTS, who was aged 17 years and was treated with thalamic DBS. DBS resulted in progressive and sustained improvement of tics and co-morbidities. After 6 years of DBS treatment, it was noted that the clinical improvement was maintained also in OFF stimulation setting, so it was decided to keep it off. After 2 years in off-setting and stable clinical picture the entire DBS device was removed. Six months after DBS device removal the patient remained symptom-free.
Conclusions:
DBS is a therapeutic option reserved for severe and refractory GTS cases. In our opinion DBS might be considered as a temporary application in GTS.
Keywords: Deep brain stimulation, Gilles de la Tourette syndrome, management, timing
INTRODUCTION
Gilles de la Tourette syndrome (GTS) is a chronic neuropsychiatric disorder, characterized by multiple vocal and motor tics.[2] Co-morbidities such as attention deficit hyperactivity disorder (ADHD), obsessive compulsive disorder (OCD), depression and anxiety disorders are present in 50–90% of patients.[8] GTS commences with simple motor tics by the age of 4–6 years, aggravated subsequently by complex motor and simple and complex vocal tics. GTS has a waxing and waning nature, with periods of remission and periods of aggravations. Remission with adult age has been reported.[5] Observational approach with regular follow-ups should be reserved to mild cases without social impairment and interferences with daily activities. In moderate and severe cases with social impairment pharmacological treatments and/or psychotherapeutic treatments should be applied.
CASE REPORT
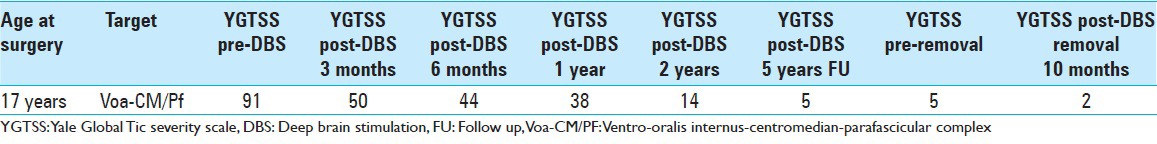
We present a patient with GTS,[10] who at the age of 17 years underwent bilateral deep brain stimulation (DBS) for severe and refractory GTS. The patient history started at the age of 7 with simple motor tics associated with ADHD. Two years later, vocal and complex motor tics appeared. The patient suffered a relevant social impairment with important difficulties in learning and education due to tics and ADHD. Several pharmacological treatments and psychological treatments were tried without any benefit. Three months prior to surgery, the patient developed a severe “status ticcosus” (continuous motor and vocal tics) that obliged him to leave school. His clinical condition did not respond to any treatment. After careful multidisciplinary examination that involved a neurologist, psychiatrist, and a psychotherapist, DBS of the ventro-oralis internus centromedian parafasciular complex (Vo-Cm/Pf) was considered. The Vo-Cm/PF coordinates were 5 mm lateral to the anterior commissure-posterior commissure (AC-PC), 2 mm posterior to the AC-PC midpoint, and at AC-PC (Electrodes Model 3389 Medtronic Minneapolis, MN, USA). The procedure was done following compassionate use. The DBS procedure was uneventful. The patient was evaluated at 1, 3, 6 months, and subsequently every 6 months with progressive improvement in his Yale Global Tic Severity Scale (YGTSS) scores [Table 1]. Twelve months after intervention, his YGTSS had improved by 58.2%. However, 3 years after surgery, the patient started to worsen. Examination revealed that the internal pulse generator (IPG, Kinetra) was discharged. After IPG substitution, the patient's motor and vocal tics improved as evidenced by regular follow-up visits. Three years after IPG replacement, it was noticed that the IPG was turned off once again, but surprisingly this time the patient (now aged 23 years) did not present any aggravation of symptoms. In light of his stable clinical status the patient and his caregivers decided to leave the IPG in OFF state. Close follow-up for 2 years confirmed his stable clinical status in OFF IPG setting. Consequently, together with the patients and his family the decision was taken, to remove the entire DBS device. At the last follow-up visit, that is, 8 months after DBS-device removal, the patient remained clinically stable. Video available at www.surgicalneurologyinternational.com/video/GTS_DBS.wmv.
Table 1.
YGTSS pre-DBS and post-DBS
DISCUSSION
In the late 1990s, Vandewalle et al. applied the first stereotactic bilateral DBS for refractory GTS targeting the Vo-Cm/Pf complex.[11] This approach was based on previous experience by Hassler and Dickmann lesioning the thalamus.[4] The thalamus was selected as prime target as a thalamic over-activity was thought to be the pathophysiological basis of GTS.[1] For 41 GTS patients treated since 1999 with thalamic DBS a significant mean YGTSS decrease of 58% (standard deviation [SD] =15) was reported.[9] Several guidelines have been published for DBS in GTS. One of the main decisive topics in these guidelines is the age of inclusion. The European guideline[7] suggest that DBS should be reserved to patients older than 18 years, while the American guidelines suggest 25 years as the age limit for DBS.[6] The age limit of 25 years is related to the observation that in some patients GTS resolves spontaneously in the second decade of life. On one hand we approve this line of reasoning, but on the other hand we have to consider that the time period between 15 and 25 years is a critical part of the life of a young adult for educational, professional and social reasons. Consequently patients with severe GTS in this age range (15–25 years) have decisively lower chances to optimize their quality of life. In our opinion, severely and refractory patients younger than 18 years old should be screened and evaluated as potential candidates for DBS. Our proposal of a temporary application of DBS in GTS is based on the observation that the patient did not present any worsening of his clinical status even after a prolonged period without stimulation. For this reason we did not substitute the IPG and arrived gradually to the decision to remove the entire DBS device. The likelihood of temporary DBS application is especially given for GTS as some patients experience a complete cure or at least a clinical amelioration in young adulthood. Before DBS, our patient was not able to confront the challenges of school and had to leave without qualification. After DBS he had an optimal professional formation and social insertion in the most crucial period of his young adult life.
CONCLUSION
DBS is experimental in GTS and unfortunately large clinical trials remain rare in DBS, whatever its indication. This has several reasons, as the important financial aspects of a complex surgical intervention, the difficulties to standardize the procedure and the strict eligibility criteria for DBS, foremost for subjects per definition refractory to conventional treatment. The publication of every case, favorable and unfavorable outcomes,[3] becomes therefore still more imperative, in order to gather important information to evaluate, despite the known limitations of class IV studies, the efficacy of DBS.
DBS application needs to be weighted against the severity of the disease and its co-morbidies, for which no other therapeutic means are available.
SUPPLEMENTAL VIDEO INFORMATION
Pre-DBS, at 9 months post-DBS, 1 year DBS off
Pertinent translations:
9 months post-DBS:
MP (Mauro Porta): How are you Simone?
Patient: I feel much better now.
MP: When did you have the implantation of the pacemaker?
Patient: Last year in April.
MP: And now you do not have any more tics?
Patient: No, not now anymore.
MP: Also no vocal tics?
Patient: No, no.
MP: So, you feel fine.
Patient: Yes.
At one year DBS off the patient is saying that he benefited much from DBS and that he could also take the driving license, thanks to it. He works now as an electrician.
Video Available on: www.surgicalneurologyint.com
Footnotes
Contributor Information
Edvin Zekaj, Email: ezekaj@yahoo.com.
Christian Saleh, Email: chs12us75010@yahoo.com.
Mauro Porta, Email: mauroportamilano@gmail.com.
Domenico Servello, Email: servello@libero.it.
REFERENCES
- 1.Ackermans L, Neuner I, Temel Y, Duits A, Kuhn J, Visser-Vandewalle V. Thalamic deep brain stimulation for tourette syndrome. Behav Neurol. 2013;27:133–8. doi: 10.3233/BEN-120301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.4th ed. Washington, DC: 2000. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. text revision. [Google Scholar]
- 3.Dueck A, Wolters A, Wunsch K, Bohne-Suraj S, Mueller JU, Haessler F, et al. Deep brain stimulation of globus pallidus internus in a 16-year-old boy with severe tourette syndrome and mental retardation. Neuropediatrics. 2009;40:239–42. doi: 10.1055/s-0030-1247519. [DOI] [PubMed] [Google Scholar]
- 4.Hassler R, Dieckmann G. Stereotaxic treatment of tics and inarticulate cries or coprolalia considered as motor obsessional phenomena in gilles de la tourette's disease. Rev Neurol. 1970;123:89–100. [PubMed] [Google Scholar]
- 5.Leckman JF, Zhang H, Vitale A, Lahnin F, Lynch K, Bondi C, et al. Course of tic severity in tourette syndrome: The first two decades. Pediatrics. 1998;102:14–9. doi: 10.1542/peds.102.1.14. [DOI] [PubMed] [Google Scholar]
- 6.Mink JW, Walkup J, Frey KA, Como P, Cath D, Delong MR, et al. Patient selection and assessment recommendations for deep brain stimulation in tourette syndrome. Mov Disord. 2006;21:1831–8. doi: 10.1002/mds.21039. [DOI] [PubMed] [Google Scholar]
- 7.Muller-Vahl KR, Cath DC, Cavanna AE, Dehning S, Porta M, Robertson MM, et al. European clinical guidelines for tourette syndrome and other tic disorders.Part IV: Deep brain stimulation. Eur Child Adolesc Psychiatry. 2011;20:209–17. doi: 10.1007/s00787-011-0166-4. [DOI] [PubMed] [Google Scholar]
- 8.Robertson MM. Gilles de la tourette syndrome: The complexities of phenotype and treatment. Br J Hosp Med. 2011;72:100–7. doi: 10.12968/hmed.2011.72.2.100. [DOI] [PubMed] [Google Scholar]
- 9.Saleh C, Gonzalez V, Cif L, Coubes P. Deep brain stimulation of the globus pallidus internus and gilles de la tourette syndrome: Toward multiple networks modulation. Surg Neurol Int. 2012;3:S127–42. doi: 10.4103/2152-7806.95424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Servello D, Sassi M, Brambilla A, Defendi S, Porta M. Long-term, post-deep brain stimulation management of a series of 36 patients affected with refractory gilles de la tourette syndrome. Neuromodulation. 2010;13:187–94. doi: 10.1111/j.1525-1403.2009.00253.x. [DOI] [PubMed] [Google Scholar]
- 11.Vandewalle V, van der Linden C, Groenewegen HJ, Caemaert J. Stereotactic treatment of gilles de la tourette syndrome by high frequency stimulation of thalamus. Lancet. 1999;353:724. doi: 10.1016/s0140-6736(98)05964-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


