Abstract
Background:
Although the frequency of self-medication has been well-documented in the public health literature, but no study has examined the relationship between health literacy and self-medication yet. This study was aimed to investigating the relationship between health literacy and self-medication in a community-based study.
Methods:
This cross-sectional study was conducted on 924 adults to survey association between health literacy and self-medication among peoples in Ardabil city in 2014 who were selected using a multi-stage random sampling method. Health literacy was measured by the test of functional health literacy in adults and general health status was measured by the 12-item General Health Questionnaire, and self-reported self-medication (overall, sedative, antibiotic and herbal) in last 3 months was assessed. All statistical analysis was performed using the SPSS version 18 and a P < 0.05 was considered significant.
Results:
The mean age and weight of respondents were 37 years and 74.7 kg, respectively. The prevalence of self-medication was 61.6%, and the percentage of self-administering antibiotics, sedative, and herbal medicines were 40%, 54.4%, and 59.1% in the last 3 months, respectively. Significant relationship was found between of total health literacy and general health status with self-medication. The prevalence of self-medication among participants with poor and very poor self-rated physical and mental health was significantly higher than other participants (P < 0.001).
Conclusions:
Self-medication had a significant relationship with health literacy and health status. Therefore, the design and implementation of training programs are necessary to increase the perception on the risk of self-medication.
Keywords: Health literacy, health status, self-medication
INTRODUCTION
Taking drug is one of the rings of the treatment chain,[1] while self-medication is one of the problems in treatment cycle.[2] Self-medication without prescription is the main problem of the drug culture that, in addition, to disturb the treatment process and incidence of side effects; it imposes huge costs of the drugs.[3]
In this regard, Iran is considered as the country with highly self-medication prevalence. Previous studies showed that drug use does not follow any proper pattern in the country. Efforts done to modify the pattern have not been successful, and the national medical system is still faced with the problem of excessive consumption and self-medication.[4] In addition to the prescription of the drugs by physicians, many people directly refer to pharmacies and prepare and consume various drugs to prevent and treat diseases and possibly strengthen themselves depending on their own diagnosis which is often wrong.[5] Studies also show that the rate of drug prescription is not consistent with the population and the epidemiological status of diseases which may be resulted from self-medication in the community.[6]
Given the increasing prevalence of self-medication in the community and the direct role of individuals in the selection and use of medicines, it is necessary to identify factors influencing the change in behavior to achieve healthy behavior (lack of self-medication) so that individuals can have long-life and relatively healthy and active life.
Although the frequency of self-medication has been well-documented in the public health literature, but no study has examined the relationship between health literacy and self-medication yet. Whereas, evidences showed the association between patient literacy skills and a number of medication-related behaviors and outcomes[7,8] however, Kim et al. findings showed that patients with adequate health literacy performed worse in certain self-management behaviors compared with the limited literacy group.[9]
As far as we know no studies examined relationship between health literacy and self-medication in the community population and this is first study to look specifically at the link between health literacy and self-medication, we feel the data can provide important preliminary evidence on policy makers and health professionals for enhancing health literacy and promoting community knowledge and literacy on self-medication and also on which future studies should be based. Therefore, given that the health literacy can provide useful guides on how to design educational interventions for improving patients’ knowledge and skills,[10] the current study was done with the aim of investigating the relationship between health literacy and self-medication in a community-based study.
METHODS
Study design and participants
This cross-sectional study was conducted to survey association between health literacy and self-medication among peoples in Ardabil city (Ardabil is located in northwest of Iran, near Iran-Azerbaijan border) in 2014 who were selected using a multi-stage random sampling method. Sample size was calculated by the function n = Z2 1−a/2P (1 – P)/d2× deff. The Health Literacy Survey in 2012 regarding health literacy in Iran showed the inadequate health literacy percentage was 76%[11] (P = 0.76). The confidence interval was ±3%, d = 0.03* P = 0.70, α = 0.05, Z1−α/2 = 1.96, deff is design effect, defined as 2 due to cluster sampling. Therefore, the minimum sample size is calculated 950. With considering response rates of the questionnaire 90%, the actual sample size should be at least 1045, in the present study 1100 people were asked to participate that 924 participants completed the study.
Multi-stage sampling was employed to collect data. The target population was first stratified into local (urban) and nonlocal (rural) residents, with an equal sample size for each group. Then, based on the principle of balancing samples among factors such as age and occupation, cluster sampling was conducted in six places where local residents gather (including communities, government organizations and other institutions) and six places where nonlocal residents gather (including near the hospitals and shops).
A total of 1,100 adults aged 18 and older were selected and interviewed for participation in the survey. Excluding nonresponders (subjects who refused or could not complete questionnaires), and illiterate subjects (illiterate subjects may feel embarrassed about not being able to read and may be uncomfortable taking the self-administered health literacy test, which requires the respondent to read and answer to health related questions.[12,13] Subjects who had uncorrectable vision and hearing problems and who were cognitively impaired, 924 adults voluntarily completed questionnaires and participated in the survey. The response rate was 84%. On average, the interview took around 35 min to complete. Interviewers trained to data quality assurance, and they completed data collection evaluation.
Procedures, study instrument and variables assessment
Health literacy was measured by the test of functional health literacy in adults (TOFHLA) which was originally designed by Parker et al. for the adult population.[14] The TOFHLA was translated and validated by Javadzade et al. to Persian language.[11] The TOFHLA contains a reading comprehension and numeracy section, and the sum of the two sections yields the TOFHLA score, which ranges from 0 to 100, with higher scores indicating better health literacy.[14] Scores are classified and interpreted as follows: 0–59, inadequate functional health literacy; 60–74, marginal health literacy; 75–100, adequate functional health literacy. The TOFHLA had high internal reliability, in the current study sample; the internal reliability of the scale was 0.82 for numeracy section and 0.9 for reading comprehension section.
Health status was measured by the 12-item General Health Questionnaire (GHQ), GHQ-12 was a shorter 12-item version of GHO, which originally consisted of 60 items with four response categories in each item indicating the severity of psychological distress experienced in past 4 weeks.[15] Its psychometric properties have been validated in Persian language[16,17] and in the present study Cronbach's alpha coefficient was found to be 0.88. Our study used the Lickert scoring method, in which each response categories scored 0, 1, 2, and 3, respectively. The summation of scores from all the 12 questions gave a final result ranging from 0 to 36. Self-rated health status was assessed by asking respondents to self-rate their physical and mental health over the past 6 months on a 5-point Likert scale, ranging from 1 (very poor) to 5 (excellent). Sociodemographic attributes included marital status, age, gender, educational level.
Self-reported self-medication (overall, sedative, antibiotic and herbal) in last 3 months was assessed by two points include yes or no.
Statistical analysis
For descriptive analysis, age was classified into 18–24 years, 25–35 years, 36–45 years, 46–55 years and 56–65 years. Significant differences in HL across self-reported self-medication groups analyzed with using t-test, associations of self-reported self-medication groups with self-rated health status were assessed using the Chi-square test, correlation of self-medication with health literacy and health status was analyzed with using logistic regression analysis. All statistical analysis was performed using the SPSS version 18 and a P < 0.05 was considered significant. Before the interview, the interviewerfirst explained the purpose of the survey, the study participants’ rights, and the confidentiality of study participants. Further, a verbal informed consent was obtained prior to the interview.
RESULTS
The mean age and weight of respondents were 37 years and 74.7 kg, respectively. The majority of respondents were female (61.4%) and married (75.8%). The largest group of respondents (32.1%) had middle school literacy (6–9 years of formal schooling) and the second largest had 9–12 years (high school).
The prevalence of self-medication among studied participants was 61.6%. The percentage of self-administering antibiotics, sedative and herbal medicines were 40, 54.4 and 59.1 in the last 3 months, respectively. The most common reasons for self-medication were previous experience of diseases and high cost of a physician visit 41.9%, 25.6%, respectively.
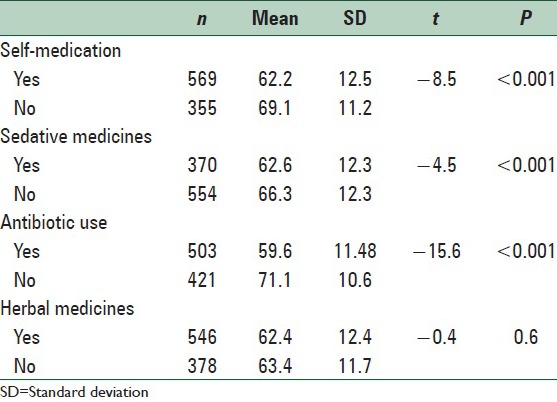
The mean score of total health literacy among the participants who self-medicated was significantly lower than who had not the self-medication. Furthermore, the mean score of total health literacy among the participants who self-medicated sedative and antibiotic medicines were significantly lower than who reported no self-medication [Table 1].
Table 1.
Mean and SD of health literacy based on self-medication status
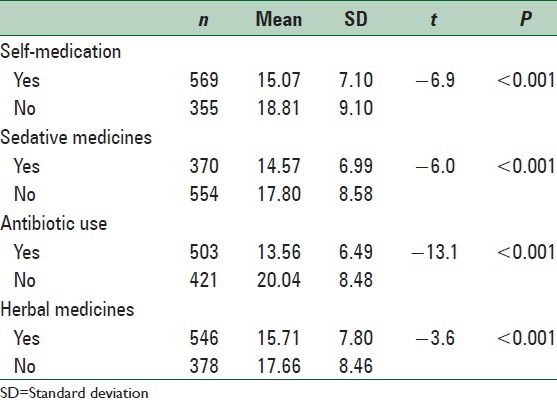
The mean score of total general health status among the participants who self-medicated was significantly lower than who had not the self-medication. Furthermore, the mean score of total general health status among the participants who self-medicated sedative and antibiotic medicines were significantly lower than who reported no self-medication [Table 2].
Table 2.
Mean and SD of general health status based on self-medication status
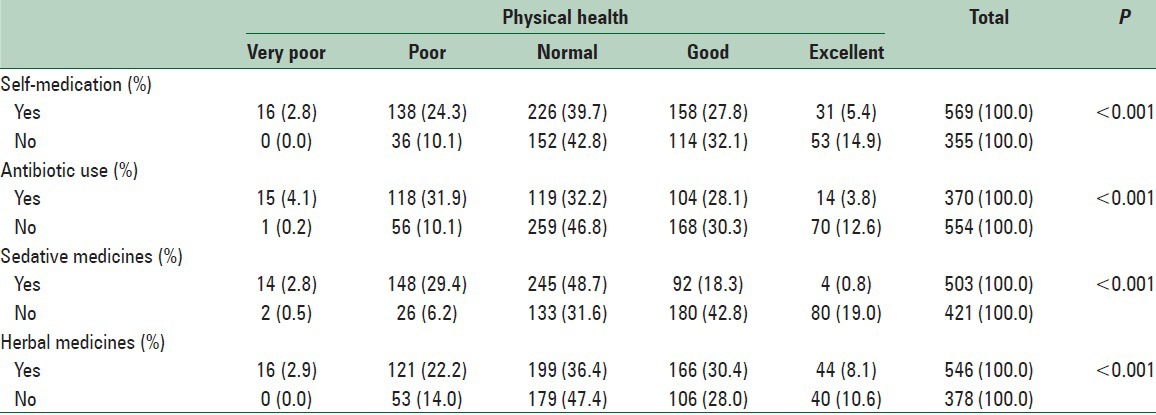
The prevalence of self-medication among participants with poor and very poor self-rated physical health was significantly (P < 0.001) higher and in contrast, good and excellent self-rated physical health was significantly more prevalent in no self-medication group. Furthermore, poor and very poor self-rated physical health was significantly (P < 0.001) more prevalent in participants who self-medicated antibiotic, sedative and herbal medicines [Table 3].
Table 3.
Self-rated physical health and self-medication in participants
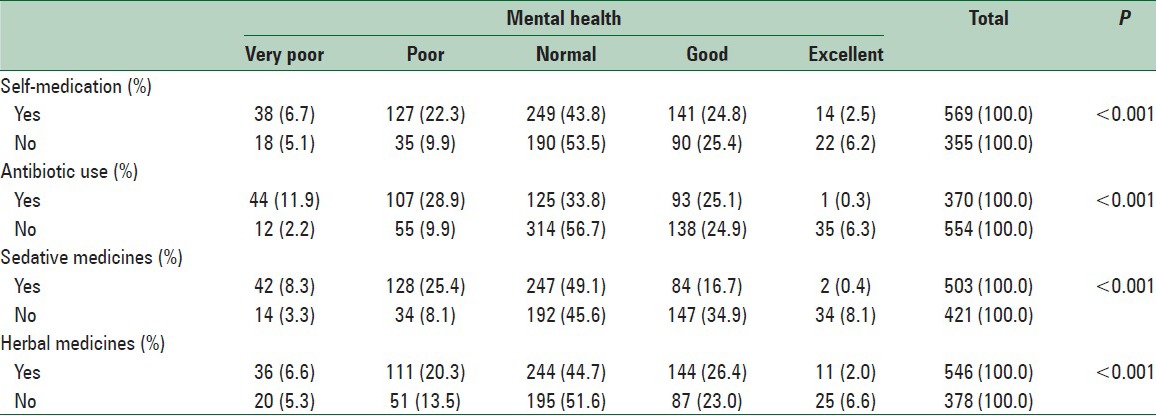
The prevalence of self-medication among participants with poor and very poor self-rated mental health was significantly (P < 0.001) higher and in contrast, good and excellent self-rated mental health was significantly more prevalent in no self-medication group. Furthermore, poor and very poor self-rated mental health was significantly (P < 0.001) more prevalent in participants who self-medicated antibiotic, sedative and herbal medicines [Table 4].
Table 4.
Self-perceived mental health and self-medication in participants
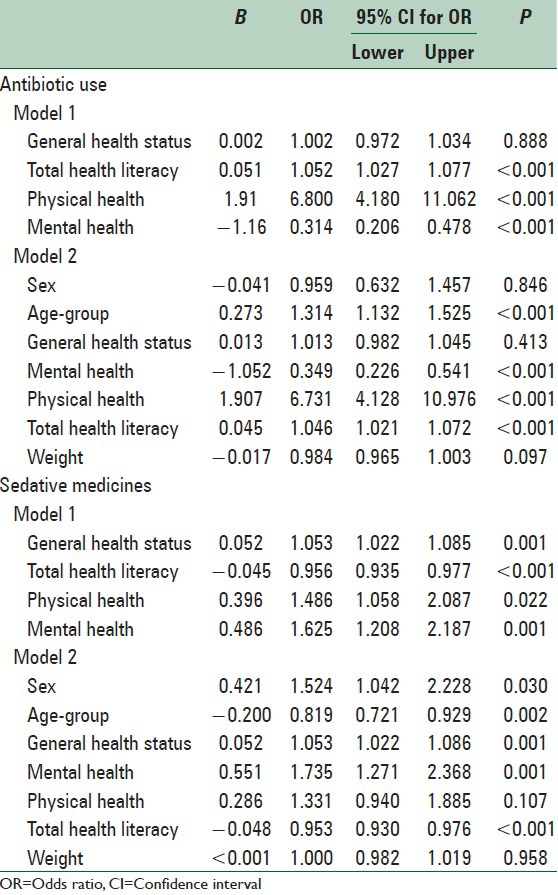
Logistic regression analysis was conducted for predictability of health status and health literacy variables on self-medication. An enter model building procedure was conducted and according to the results as showed in Table 5, the general health status, perceived mental health, perceived physical health and health literacy variables were selected more influential predictor on antibiotic medicines use and perceived mental and physical health and health literacy variables were selected more influential predictor on sedative medicines self-medication. After adjusting for potentially confounding covariates such as age, sex and weight, the general health status, perceived mental health, perceived physical health and health literacy variables were selected more influential predictor on antibiotic and sedative medicines self-medication.
Table 5.
The correlation self-medication with health literacy and health status using logistic regression analysis
DISCUSSION
Results showed that the prevalence of self-medication is alarmingly high. The prevalence of self-medication among studied participants was 61.6%. Some higher rates were reported, in another Iranian study, 76.6% of the students had used analgesics in self-medication in the previous 3 months in a study was conducted in Iran,[18] 91% of migraine patients used self-medication; acetaminophen and codeine were the most common[19] and some lower rates reported 35.4% of the participants had self-medication[20] The results indicated that 35.4% of the respondents had practiced self-medication past 2 weeks.[21] The percentage of self-medicated antibiotics, sedative and herbal medicines was 40, 54.4 and 59.1 in the last 3 months, respectively. In similar study by Ilhan et al. the percentage of self-administering antibiotics was 19.1% in the last 12 months[22] in another study 48.1% of the study population had used antibiotics without a prescription within 1-month.[23] This variation could be partly due to the differences in study design and studied samples. Regarding the growing global resistance for antibiotic and documented health issues related to inappropriate use of such drugs, our findings approve emergency of legal regulation in this issue.
Alghanim study showed that respondents with poor health status were more likely to practice self-medication.[21] The results of this study showed that respondents with very poor and poor self-reported health status were more likely to practice self-medication than those who reported their health conditions good or excellent. This finding in consistent with other similar studies.[24,25]
It is evidenced that people with low health literacy understand health information less well[26] and in A meta-analysis conducted by Berkman et al. finding from 96 peer reviewed papers on health literacy showed that low health literacy was consistently associated with greater use of emergency care, poorer ability to demonstrate taking medications appropriately and with poorer overall health status.[27]
Evidences showed that self-medication occurred in an attempt to resolve health problems,[21] so, the decision process of self-medication depends on individual knowledge, perceptions and health-related behaviors and purchasing and using of over-the-counter medicines influenced by these factors.[28]
Self-medication is considered as a major issue of communities for their side effects, risks, mortality and its huge costs in drug budgets of governments, insurance companies, and general population.[4] Thus, the identification and analysis of reasons for self-medication are very important among various groups of community. One of these reasons is the low level of health literacy.
In his study, Sahebi et al. stated that among patients referred to Tabriz Pharmacies, analgesics and antibiotics had the highest rates of drug consumption for self-medication.[29]
On the importance of health literacy in self-medication behaviors of people, studies conducted on its reasons can be pointed out. The reasons for self-medication reported in previous studies may pertain to inadequate health literacy. In this regard, several factors such as lack of enough time,[30] symptomatic treatment by physicians and assuming unimportant problem by patients,[1] not considering serious illness and fear of treatment,[31] symptomatic treatment of diseases, not considering important disease and expensive visits,[32] having experience in the treatment of diseases, lack of accurate information on the effects of drugs and lack of confidence in physicians’ practices[14] in various studies and lack of need to referring to physician in the study by Corbally had been the most important reasons for self-medication among participants.[33]
Logistic regression analysis showed that the general health status, perceived mental and physical health and health literacy variables were more influential predictor on self-medication, this result was is consistent with Carrasco-Garrido et al.,[34] Sawyer et al.[35] and Turunen et al.[36] studies. Previous studies had shown that people with poor perception of health status are more likely to use analgesic medication. However, no studies were examined relationship between self-medication and health literacy.
The issues outlined in the results and discussion of our study also point to the necessity that the theme of self-medication and health literacy should be present in the education of future nursing professionals, who must have sound knowledge about fundamental aspects for the practice of care for another, not only regarding adverse events, medication interactions, or importance of adherence to the therapeutic regimen, among others; but also skills in the preparation and implementation of educational nursing programs on responsible self-medication.
Thus, the present study showed a significant difference between those who are involved in self-medication and those who did not report self-medication; however, given the lack of information on this issue, further studies are needed to prove the relationship.
LIMITATIONS
The present study suffers from some limitations such as collecting data through questionnaire. In this regard, it should be noted that in studies using questionnaire to collect data, it is assumed that the respondent states correct and true information; however, the questionnaire may not be completed honestly by the respondents. Another limitation of this study was to collect information in the spring and summer. It is recommended to consider this in future studies. It is also suggested that considering the nature of self-medication, presence or absence of difference in the prevalence and type of medicines used in different seasons be studied.
Study strength
The optimal number of samples and collecting information from the community are considered as the study strengths. To the best knowledge of the researchers, this study is the first one which assesses the relationship between health literacy and self-medication in the community.
CONCLUSIONS
Self-medication, especially antibiotics use had a high prevalence in the studied community and had significant relationship with health literacy and health status Therefore, the design and implementation of training programs are necessary to increase the perception on the risk of self-medication among various groups.
Implications and recommendations
The results of our study showed that self-medication rate was high, and health literacy rate was low, therefore these results indicate a serious crisis in the public health and our society, which can impose expensive costs to society and the healthcare system. Hence, health and national policy makers might increase funding for research and actions into social and health interventions in various health and healthcare settings to improve health literacy. Furthermore, health care systems and medical universities should have more attention for health literacy skills and health professions education and training programs, particularly programs that train professionals in the fields of direct patient interaction. As well as, with regard to the findings of this study, the followings are recommended:
To provide appropriate, systematic and widespread educational programs on the serious complications of self-medication among different social groups; to monitor the pharmacies in order not to sell antibiotic and seductive medicines without prescription; to pay particular attention to obstacles on referring patients to physicians and to receive medicines under the supervision of doctors and to eliminate obstacles such as insurance of medical care and prevention
ACKNOWLEDGEMENTS
This is a part of larger study with number 9209. The authors are grateful to the Ardabil University of Medical Sciences Research Review Board for the financial support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tavakooli R. Effect of important variables; economic, social and cultural on self-medication. Med Daneshvar. 2001;8:9–12. [Google Scholar]
- 2.Karimy M, Heidarnia A, Ghofrani F. Factors influencing self-medication among elderly urban centers in Zarandieh based on Health Belief Model. Arak Univ Med Sci J. 2011;14:70–8. [Google Scholar]
- 3.Sanaei MD, Sobhani A. Pattern of drug consumption and its changes during the first trimester of pregnancy. J Qazvin Univ Med Sci. 2002;20:55–61. [Google Scholar]
- 4.Davati A, Jafari F, Samadpoor M, Tabar K. Survey of medication in ageing of Tehran city. J Med Counc Islam Repub Iran. 2008;25:450–6. [Google Scholar]
- 5.Kamat VR, Nichter M. Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Soc Sci Med. 1998;47:779–94. doi: 10.1016/s0277-9536(98)00134-8. [DOI] [PubMed] [Google Scholar]
- 6.Masoudi-Alavi N, Izadi F, Ebadi A, Hajbagheri A. Self treatment experience in diabetes mellitus type 2. Iran J Endocrinol Metab. 2009;10:581–8. [Google Scholar]
- 7.Bailey SC, Oramasionwu CU, Wolf MS. Rethinking adherence: A health literacy-informed model of medication self-management. J Health Commun. 2013;18(Suppl 1):20–30. doi: 10.1080/10810730.2013.825672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: A systematic review of the literature. J Gen Intern Med. 2004;19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. 2004;27:2980–2. doi: 10.2337/diacare.27.12.2980. [DOI] [PubMed] [Google Scholar]
- 10.Pignone M, DeWalt DA, Sheridan S, Berkman N, Lohr KN. Interventions to improve health outcomes for patients with low literacy. A systematic review. J Gen Intern Med. 2005;20:185–92. doi: 10.1111/j.1525-1497.2005.40208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Javadzade SH, Sharifirad G, Radjati F, Mostafavi F, Reisi M, Hasanzade A. Relationship between health literacy, health status, and healthy behaviors among older adults in Isfahan, Iran. J Educ Health Promot. 2012;1:31. doi: 10.4103/2277-9531.100160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolf MS, Williams MV, Parker RM, Parikh NS, Nowlan AW, Baker DW. Patients’ shame and attitudes toward discussing the results of literacy screening. J Health Commun. 2007;12:721–32. doi: 10.1080/10810730701672173. [DOI] [PubMed] [Google Scholar]
- 13.Lee SY, Tsai TI, Tsai YW, Kuo KN. Health literacy, health status, and healthcare utilization of Taiwanese adults: Results from a national survey. BMC Public Health. 2010;10:614. doi: 10.1186/1471-2458-10-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 15.Bloomington, Minnesota, USA: StatPac, Inc; [Last accessed on 2009 Aug 06]. General Health Questionnaire. Available from: http://www.webpoll.org/psych/ghq12.htm . [Google Scholar]
- 16.Montazeri A, Harirchi AM, Shariati M, Garmaroudi G, Ebadi M, Fateh A. The 12-item General Health Questionnaire (GHQ-12): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:66. doi: 10.1186/1477-7525-1-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mofidi N, Ghazinour M, Araste M, Jacobsson L, Richter J. General mental health, quality of life and suicide-related attitudes among Kurdish people in Iran. Int J Soc Psychiatry. 2008;54:457–68. doi: 10.1177/0020764008091663. [DOI] [PubMed] [Google Scholar]
- 18.Sarahroodi S, Maleki-Jamshid A, Sawalha AF, Mikaili P, Safaeian L. Pattern of self-medication with analgesics among Iranian University students in central Iran. J Family Community Med. 2012;19:125–9. doi: 10.4103/2230-8229.98302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sedighi B, Ghaderi-Sohi S, Emami S. Evaluation of self-medication prevalence, diagnosis and prescription in migraine in Kerman, Iran. Saudi Med J. 2006;27:377–80. [PubMed] [Google Scholar]
- 20.Jalilian F, Hazavehei SM, Vahidinia AA, Jalilian M, Moghimbeigi A. Prevalence and Related Factors for Choosing Self-Medication among Pharmacies Visitors Based on Health Belief Model in Hamadan Province, West of Iran. J Res Health Sci. 2013;13:81–5. [PubMed] [Google Scholar]
- 21.Alghanim SA. Self-medication practice among patients in a public health care system. East Mediterr Health J. 2011;17:409–16. [PubMed] [Google Scholar]
- 22.Ilhan MN, Durukan E, Ilhan SO, Aksakal FN, Ozkan S, Bumin MA. Self-medication with antibiotics: questionnaire survey among primary care center attendants. Pharmacoepidemiol Drug Saf. 2009;18:1150–7. doi: 10.1002/pds.1829. [DOI] [PubMed] [Google Scholar]
- 23.Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005;8:326–31. [PubMed] [Google Scholar]
- 24.Fuentes Albarrán K, Villa Zapata L. Analysis and quantification of self-medication patterns of customers in community pharmacies in southern Chile. Pharm World Sci. 2008;30:863–8. doi: 10.1007/s11096-008-9241-4. [DOI] [PubMed] [Google Scholar]
- 25.Balbuena FR, Aranda AB, Figueras A. Self-medication in older urban mexicans: An observational, descriptive, cross-sectional study. Drugs Aging. 2009;26:51–60. doi: 10.2165/0002512-200926010-00004. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine. Health Literacy: A Prescription to End Confusion. 2004. [Last accessed on 2014 Aug 08]. Available from: http://www.iom.edu/CMS/3775/3827/19723.aspx .
- 27.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 28.Calamusa A, Di Marzio A, Cristofani R, Arrighetti P, Santaniello V, Alfani S, et al. Factors that influence Italian consumers’ understanding of over-the-counter medicines and risk perception. Patient Educ Couns. 2012;87:395–401. doi: 10.1016/j.pec.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Sahebi L, Seidy A, Amini S, Mousakhani M. Self-medication status among referring patients to Tabriz pharmacies. Pharm Sci. 2009;14:174–81. [Google Scholar]
- 30.Nejad MK, Far MR, Heidari M, Dastjerdi ER. Determination of the most prevalent reasons for requesting drugs without prescription in Kerman pharmacies. J Babol Univ Med Sci. 1999;1:32–7. [Google Scholar]
- 31.Mulder AA, Boerma RP, Barogui Y, Zinsou C, Johnson RC, Gbovi J, et al. Healthcare seeking behaviour for Buruli ulcer in Benin: A model to capture therapy choice of patients and healthy community members. R Soc Trop Med Hyg. 2008;102:912–20. doi: 10.1016/j.trstmh.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 32.James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15:270–5. doi: 10.1159/000092989. [DOI] [PubMed] [Google Scholar]
- 33.Corbally MA, Gallagher P. Accessible yet not accessed?. A literature review exploring factors which may prevent patients taking over the counter analgesia prior to attending Accident and Emergency. Accid Emerg Nurs. 2006;14:78–82. doi: 10.1016/j.aaen.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Carrasco-Garrido P, de Andrés AL, Barrera VH, Jiménez-Trujillo I, Fernandez-de-Las-Peñas C, Palacios-Ceña D, et al. Predictive factors of self-medicated analgesic use in Spanish adults: A cross-sectional national study. BMC Pharmacol Toxicol. 2014;15:36. doi: 10.1186/2050-6511-15-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sawyer P, Bodner EV, Ritchie CS, Allman RM. Pain and pain medication use in community-dwelling older adults. Am J Geriatr Pharmacother. 2006;4:316–24. doi: 10.1016/j.amjopharm.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 36.Turunen JH, Mäntyselkä PT, Kumpusalo EA, Ahonen RS. Frequent analgesic use at population level: Prevalence and patterns of use. Pain. 2005;115:374–81. doi: 10.1016/j.pain.2005.03.013. [DOI] [PubMed] [Google Scholar]


