Abstract
Background:
One of the most common cancers is skin cancer worldwide. Since incidence and cost of treatment of the cancer are increasing, it is necessary to further investigate to prevent and control this disease. This study aimed to determine skin cancer trend and epidemiology in Iran.
Methods:
This study was done based on existing data. Data used in this study were obtained from a national registry of cancer cases and the Disease Management Center of Ministry of Health in Iran. All cases registered in the country were included during 2004–2008. Incidence rates were reported based on the direct method and standard population of World Health Organization.
Results:
Based on the results of this study, the incidence of skin cancer is rising in Iran and the sex ratio was more in men than women in all provinces. The age-standardized incidence rate (ASR) of skin cancer was highest in males in Semnan, Isfahan, and Hamedan provinces (34.9, 30.80, and 28.84, respectively). The highest ASRs were seen in females in Semnan, Yazd, and Isfahan provinces (26.7, 24.14, and 18.97, respectively). The lowest ASR in male was observed in Sistan and Baluchestan, and in female in Hormozgan provinces.
Conclusions:
The incidence of skin cancer is increasing in the country. Therefore, the plan for the control and prevention of this cancer must be a high priority for health policy makers.
Keywords: Incidence, Iran, skin cancer, trend
INTRODUCTION
Skin cancer is one of the most common cancers in the world, especially in the whites.[1] The cancer includes two types of melanoma and non-melanoma (basal cell carcinoma and squamous cell carcinoma).[2] Monitoring of skin cancer indicates an increase in the incidence of the disease.[1] In the Netherlands, the incidence of cancer has increased 80% from 2000 to 2005,[3] and in Brazil, this rate has reached from 50 new cases in 2000 to 94 cases per 100,000 people in 2006.[4] In Iran, about 15% of all cancer was skin cancer and this disease consider as the most common cancer.[5]
In addition, the financial impact of cancer can significantly affect a community resource. Treatment cost of the cancer goes beyond the 500 million dollars per year in the United States.[6] In Australia in 2010, it is estimated at around 511 million dollars.[7] Although deaths from this of cancer are low, what is more painful than the mortality rate of this type of cancer is emotional and physical suffering from it. Important activities are not done in understanding the etiology and molecular basis of cancer.[8,9]
The most important risk factors for skin cancer are individual, genetic, and environmental factors.[10] Factors such as skin color, eye color, hair color, aging, and sometimes immunodeficiency are considered genetic factors and individual characteristics affecting the risk of skin cancer.[10] Environmental factors are Exposure to ultraviolet solar radiation, decreasing latitude, high intake of alcohol, and consumption of high-fat foods, long-term activities in the outdoors, and cover change.[11,12,13,14]
Although skin cancer is a common cancer, it is one of the most preventable types of cancers.[15] The primary prevention in the earlier stage, the impact will be greater. Considering the high incidence of this cancer in Iran as the most common cancer, and the absence of a comprehensive and systematic study on the trend of the disease, this study aimed to determine skin cancer trend and epidemiology in Iran.
METHODS
This analytic study was done based on longitudinal program in Iran that similar to many countries in the world that have national registry of cancer (NCR) is trying to identify all cases of cancer occurring in Iran from 2004 to 2008. Data used in this study were obtained from a NCR, and Disease Control and Prevention (CDC) of Ministry of Health and Medical Education in Iran for 2004–2008.[16] In 2008 in Iran, there are 30 provinces and 41 Medical Universities. Deputy for the health of each university is responsible for health issues of the population and all health activities are managed by these deputies. All deputies for health have been included in the NCR. Registrar would apply the national registration software, which was developed by CDC. For pathologic centers, without software, the cancer records were gathered manually. The cancer office of CDC should provide techniques and funding supports. The data are transmitted every 3 months, by electronic file and also hard copy of “Cancer Registry Data Collection Form;” this form is comprised of three parts: Part I, regarding patient's identity characteristics in addition to the name of biopsy-taker physician, name of hospital, location of which the biopsy is taken, clinical diagnosis and date of biopsy sent to histological laboratory and demographic information of the patients includes race and residence. Part II includes the most important findings of patient's clinical history. Part III includes preclinical findings. The information includes the primary location of the tumor, date of cancer diagnosis, morphology, and histology and its behavior and diagnosis method. Physicians fill the form of clinical data and the official personnel fill the identity and demographic information. Quality control has been coordinated in five main areas by cancer office of CDC: (i) Regarding completeness of coverage, (ii) completeness of details, (iii) accuracy of data, (iv) accuracy of reports, (v) accuracy of interpretation, and (vi) repeated cases are deleted from national data. Surveillance of pathology is based on the cancer record in several selected provinces to compare it with the present pathology cancer record for a general and complete evaluation and also for the accuracy of the collected data. IARC software provides a way to identify inaccuracies in data coding. Accordance of The International Classification of Diseases for Oncology (ICD-OC: Topography with ICD-OM: Morphology) is done manually and also by considering age and sex groups (pathology file of fatal error has been revised by the Scientific Society of Pathology of Iran and also by two masters in pathology).
Method for deleting repeated cases: For the lack of any classified National Identification Numbers, the process for deleting the repeated cases was completed by a manual review of the record. After editing data of each province and considering in mind that for deleting of repeated cases, similar cases should also be the same as morphology, topography, identity, and demographic information; deletion of the repeated cases would be done separately in each province and finally in all over country by experienced manual reviewers. In duration of study (2003–2008), the number of cancer case that repetition and delegating from list of all type of cancers was 38,468, 47,217, 55,854, 59,786, 62,040, and 76,159, respectively. Furthermore, between of 25% and 39.5% of patients have defected in coding [Diagram 1]. We consider skin cancer in four types: Basal cell carcinoma, squamous cell carcinoma, malignant melanoma, and basosquamous carcinoma.
Diagram 1.
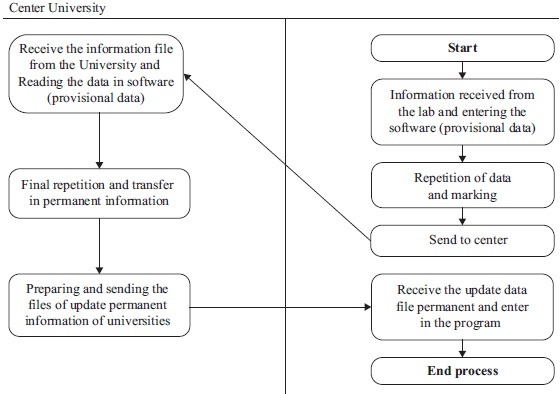
Process of data collection of cancer cause in Iran
Crude (all ages) and age-specific rates per 100,000 person-year for all provinces were calculated. For each province, the average annual age-standardized incidence rate (ASR) per 100,000 person-year was calculated by the direct method using the world standard population.
RESULTS
Findings obtained from the national registry system of cancer showed that the incidence of skin cancer had increasing trend from 2004 to 2008 [Figure 1]. That is, 43,694 cases of skin cancer have been registered in the country. Of the incidence cases, 27,364 cases were male and Sex ratio was 1.67 in these years. The highest incidence rate (9964 cases) was observed in 2008, but the lowest rate (7320 cases) was recorded in 2004 [Table 1].
Figure 1.
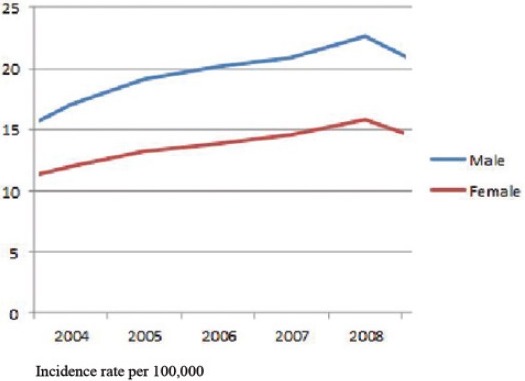
The trend of skin cancer incidence, 2004–2008
Table 1.
Frequency, CIR, and ASR-based of sex and year
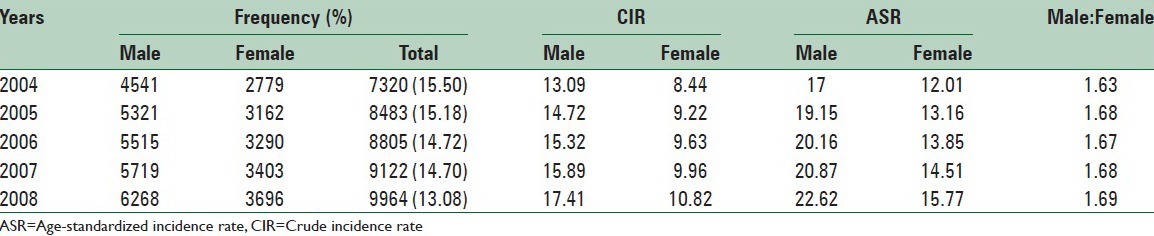
The age-specific rate in men increased from 17 in 2004 to 22.62 in 2008. The highest and lowest incidence rate in men observed in 2004 and 2008, respectively. The trend of skin cancer incidence in man was increasing; on an average, it grew by 07.06% annually. In women, this rate also elevated from 12.01 in 2004 to 15.77 in 2008 per 100,000 people. The maximum and minimum incidence rates were 17.77 and 12.01 per 100,000 people, respectively in 2008 and 2004. Furthermore, in women trend of skin cancer incidence was increasing; on an average, it grew by 06.59% annually. The highest and lowest sex ratios were 1.69 and 1.63, respectively in 2008 and 2004 [Table 1 and Figure 1].
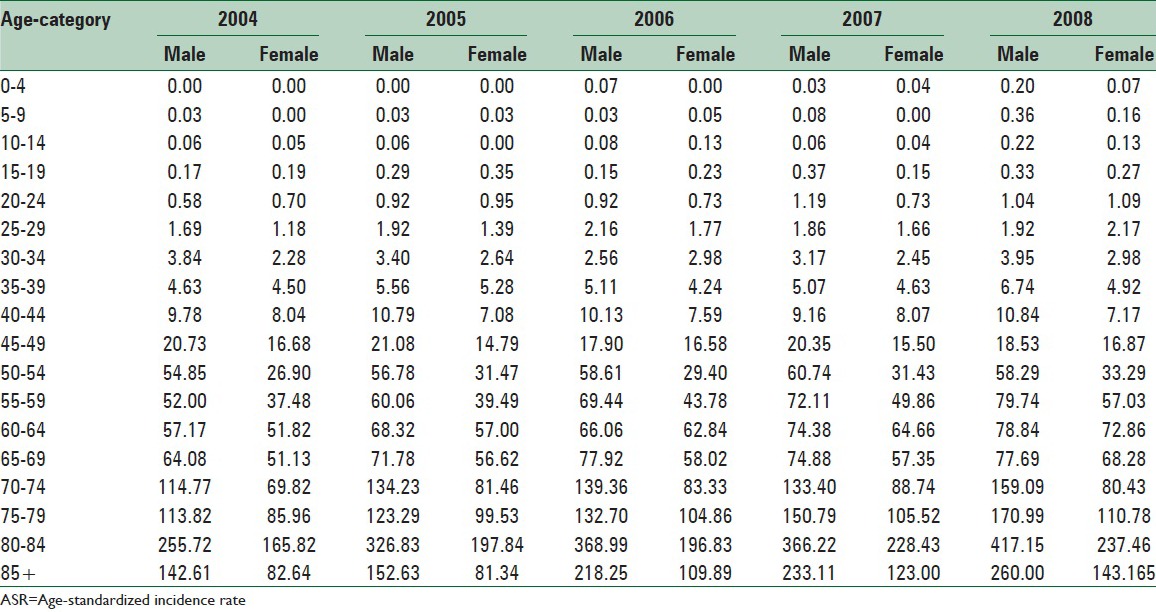
In this study, the age-specific rate was different in age groups so that as age rises, the incidence of skin cancer in men and women was increased, and the highest rate was observed at 80–84 years but it decreased at above 85 years. Furthermore, the age-specific rate in overall has rising trends from 2004 to 2008 [Table 2].
Table 2.
The ASR according to age group and gender
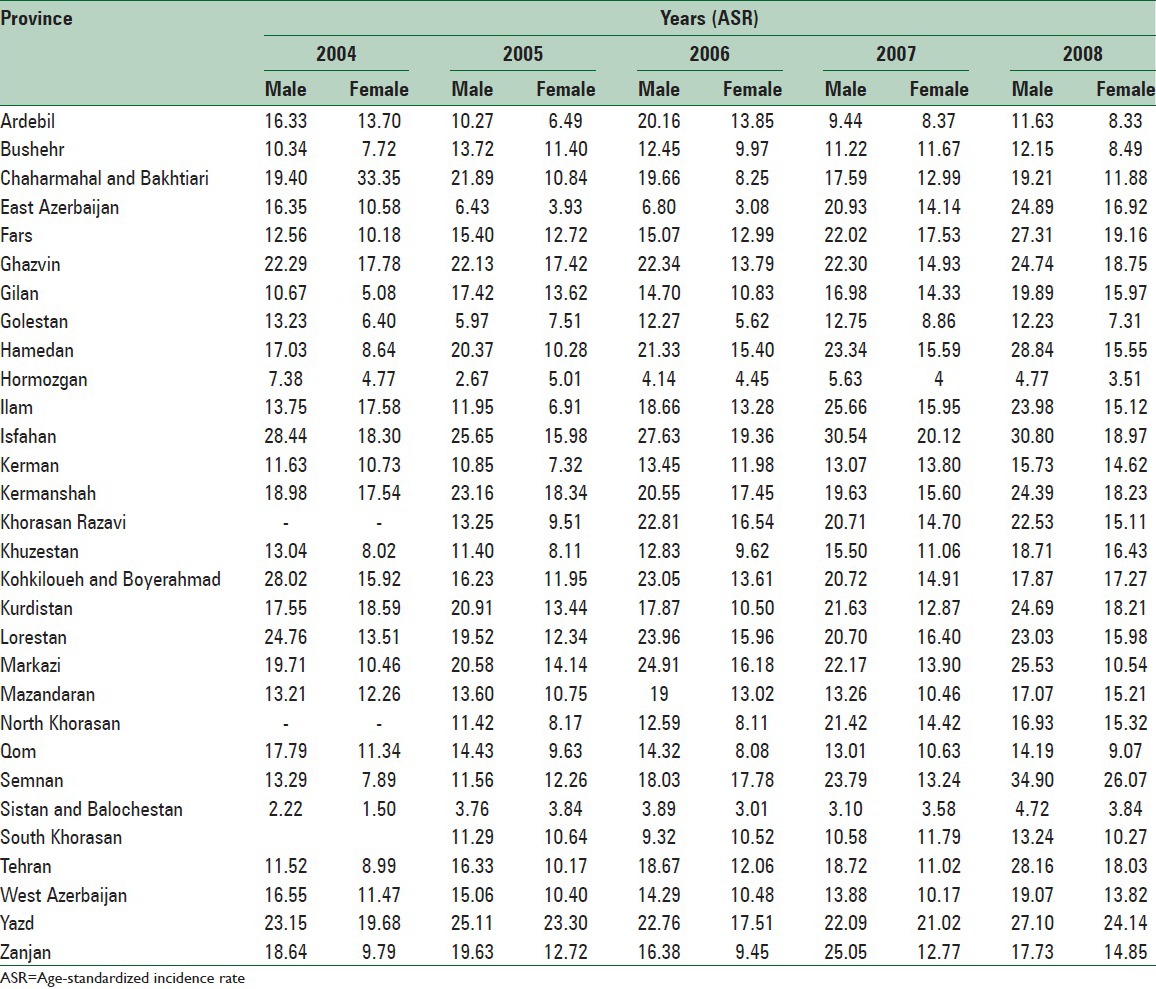
In 2008, the age-specific rate of skin cancer was highest in males in Semnan, Isfahan, and Hamedan provinces (34.9, 30.80, and 28.84, respectively). The highest ASRs were seen in females in Semnan, Yazd, and Isfahan provinces (26.7, 24.14, and 18.97, respectively). The lowest ASR in male was observed in Sistan and Baluchestan, and in female in Hormozgan provinces [Table 3].
Table 3.
Trend of ASR in Iranian province from 2004 to 2008
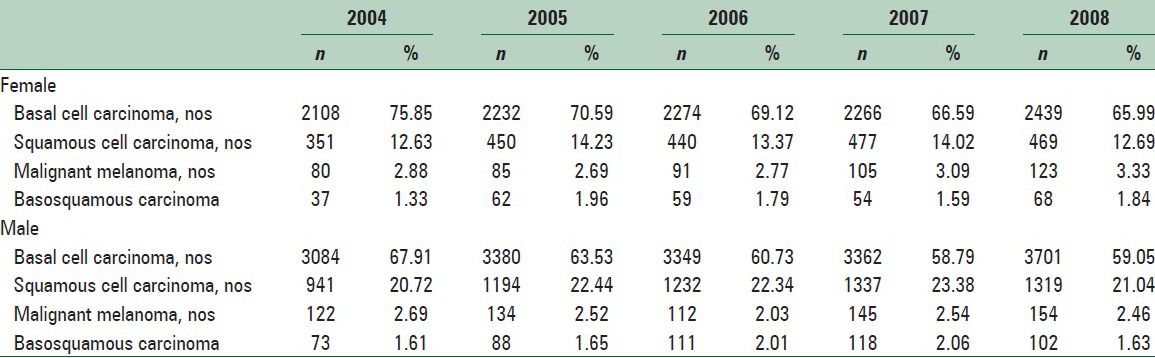
Basal cell carcinoma, squamous cell carcinoma, malignant melanoma, and basosquamous carcinoma in two gender have a rising trend in study duration, so in male Basosquamous carcinoma has maximum rising in annually incidence average 16.75% and minimum basal cell carcinoma with 03.14% and in female Squamous cell carcinoma has maximum rising in annually incidence average 08% and minimum in basal cell carcinoma with 04% [Table 4].
Table 4.
The frequency and percent of occurrence of skin cancer in Iran from 2004 to 2008
DISCUSSION
The findings indicated that the incidence of skin cancer was increasing. The trend was observed in all provinces. The highest incidence rate of skin cancer was in males in Semnan, Isfahan, and Hamedan provinces. The highest incidence rates were seen in females in Semnan, Yazd, and Isfahan provinces. The lowest ASR in male was observed in Sistan and Baluchestan, and in female in Hormozgan provinces the incidence of the disease was more in all provinces in men than women. There was a direct association between skin cancer and age so that the incidence of skin cancer was increased as age rises.
The results of this study showed that, during the period 2003 through 2008, the trend of skin cancer incidence in Iran was increasing; on an average, it grew by 07.22% annually, extensive amount of this growing was certainly related to the enhancement of the registry and reporting system. In addition, the low incidence rate of cancer in 2004 was not due to the fact that few cancer cases occurred, but rather owing to the incomplete registration of cancer cases at the beginning of the cancer registry program. Iranian national reports of cancer registry showed that the average annual percentage change for standardized incidence rate in all cancer was 9.6% in males and 10.6% in females during 2003–2008,[16] Other studies also confirmed the increasing trend of the cancer.[17] In addition this reason, various other factors may be effective in rising trend of incidence skin cancer in Iran. These factors include climate changes, environmental factors, promoting awareness, and advances in diagnosis.[13,14,22,23,24,25] The most important etiologic agent of all types of skin cancer is ultraviolet radiation.[26]
As the approach the equator, melanoma and non-melanoma cancers have linearly increased.[26] In other words, skin cancer is twice when latitude reduced nearly 10°. It revealed the increasing incidence of skin cancer in different races.[26] el Khwsky et al. expressed a relation between skin color and sun exposure. The incidence of skin cancer in people who have had excessive exposure to sunlight than other people was 4.8 times. In most seasons of the year, the intense radiation of the sun and lack of using suitable protection for outdoor in Iran can probably lead to high incidence of the disease.[27]
According to rising life expectancy and the mean age of population in our country, increasing the incidence of skin cancer, especially in the older age, may be justifiable. Other studies, similar our study, showed as age increases, the incidence of cancer will increase.[20,28]
Another research also determined that high incidence of the cancer in men than women.[28] In our study, such a result was observed in all provinces.
Daily activities in outdoor and sunny environments or contact with the carcinogen can be main factors cause to the high rate of the cancer in males.[29,30] It recommended that in the area that age-specific rate is higher than the national average, appropriate studies to identify environmental, cultural, biological and so, designed to identify the factors affecting the occurrence of the disease in these areas.
Strengths and limitations
Though the study well assessed incidence and age-specific rates of skin cancer based on the area, type of disease, age, and sex groups in Iran from 2004 to 2008, that given the extent of the time and place of the study, can have valuable results. However, it should be stated that the cancer registry system in Iran is still not fully and equally in all area and sometimes the differences in the quality and coverage of data is observed. Furthermore, in this study, despite the continued increase in the incidence of disease with rising the age, the disease in the age group 85 years, and elders is less than the previous age group, a possible reason was reduce in physician meeting in this age group for skin problem and reduce skin cancer diagnosis. In addition, we observed that provinces with the highest incidence rates in males were different from those where the highest rates of female cancers but with note to my study design; we can’t determent cause of this different.
CONCLUSIONS
The incidence of skin cancer is increasing in the country. Therefore, the plan for the control and prevention of this disease must be a high priority for health policy makers. Our findings were obtained from the descriptive study on the incidence trend of the disease in recent years and it is recommended that analytical studies should be conducted to obtain a causal relationship and solve problems related to the disease.
ACKNOWLEDGEMENTS
Hereby we appreciate of the cooperation of all employees involved in data collection in the country, especially in NCR, and CDC of the ministry of Health and Medical Education.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Horsham C, Auster J, Sendall MC, Stoneham M, Youl P, Crane P, et al. Interventions to decrease skin cancer risk in outdoor workers: Update to a 2007 systematic review. BMC Res Notes. 2014;7:10. doi: 10.1186/1756-0500-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166:1069–80. doi: 10.1111/j.1365-2133.2012.10830.x. [DOI] [PubMed] [Google Scholar]
- 3.Almahroos M, Kurban AK. Ultraviolet carcinogenesis in nonmelanoma skin cancer. Part I: Incidence rates in relation to geographic locations and in migrant populations. Skinmed. 2004;3:29–35. doi: 10.1111/j.1540-9740.2004.02331.x. [DOI] [PubMed] [Google Scholar]
- 4.Nunes DH, Back L, Vieira e Silva R, Medeiros Vde S. Incidence of squamous cell carcinoma of the skin in the city of Tubarao (SC) – Brazil in the years 2000, 2003, and 2006. An Bras Dermatol. 2009;84:482–8. doi: 10.1590/s0365-05962009000500006. [DOI] [PubMed] [Google Scholar]
- 5.Keyghobadi N, Rafiemanesh H, Mohammadian-Hafshejani A, Enayatrad M, Salehiniya H. Epidemiology and trend of cancers in the province of Kerman: southeast of Iran. Asian Pacific journal of cancer prevention: APJCP. 2015;16:1409–13. doi: 10.7314/apjcp.2015.16.4.1409. [DOI] [PubMed] [Google Scholar]
- 6.Rigel DS. Cutaneous ultraviolet exposure and its relationship to the development of skin cancer. J Am Acad Dermatol. 2008;58:S129–32. doi: 10.1016/j.jaad.2007.04.034. [DOI] [PubMed] [Google Scholar]
- 7.Fransen M, Karahalios A, Sharma N, English DR, Giles GG, Sinclair RD. Non-melanoma skin cancer in Australia. Med J Aust. 2012;197:565–8. doi: 10.5694/mja12.10654. [DOI] [PubMed] [Google Scholar]
- 8.Shariatzadeh SM, Hamta A, Soleimani Mehranjani M, Rasooli Z. Determination of chromosomal changes in DMBA-induced skin cancer in SD rat strains. J Arak Univ Med Sci. 2009;12:73–87. [Google Scholar]
- 9.Eide MJ, Krajenta R, Johnson D, Long JJ, Jacobsen G, Asgari MM, et al. Identification of patients with nonmelanoma skin cancer using health maintenance organization claims data. Am J Epidemiol. 2010;171:123–8. doi: 10.1093/aje/kwp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song F, Qureshi AA, Gao X, Li T, Han J. Smoking and risk of skin cancer: A prospective analysis and a meta-analysis. Int J Epidemiol. 2012;41:1694–705. doi: 10.1093/ije/dys146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whiteman DC, Pavan WJ, Bastian BC. The melanomas: A synthesis of epidemiological, clinical, histopathological, genetic, and biological aspects, supporting distinct subtypes, causal pathways, and cells of origin. Pigment Cell Melanoma Res. 2011;24:879–97. doi: 10.1111/j.1755-148X.2011.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Le Marchand L, Saltzman BS, Hankin JH, Wilkens LR, Franke AA, Morris SJ, et al. Sun exposure, diet, and melanoma in Hawaii Caucasians. Am J Epidemiol. 2006;164:232–45. doi: 10.1093/aje/kwj115. [DOI] [PubMed] [Google Scholar]
- 13.Ibiebele TI, van der Pols JC, Hughes MC, Marks GC, Williams GM, Green AC. Dietary pattern in association with squamous cell carcinoma of the skin:A prospective study. Am J Clin Nutr. 2007;85:1401–8. doi: 10.1093/ajcn/85.5.1401. [DOI] [PubMed] [Google Scholar]
- 14.Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer – The role of sunlight. Adv Exp Med Biol. 2008;624:89–103. doi: 10.1007/978-0-387-77574-6_8. [DOI] [PubMed] [Google Scholar]
- 15.Reynolds KD, Buller DB, Yaroch AL, Maloy JA, Cutter GR. Mediation of a middle school skin cancer prevention program. Health Psychol. 2006;25:616–25. doi: 10.1037/0278-6133.25.5.616. [DOI] [PubMed] [Google Scholar]
- 16.Goya M. Iranian Annual Cancer Registration Report 2005/2006. Ministry of Health and Medical Education, Health Deputy. Center for Disease Control and Prevention. 2007 [Google Scholar]
- 17.AIRTUM Working Group. Italian cancer figures, report 2009: Cancer trend (1998-2005) Epidemiol Prev. 2009;33:1–168. [PubMed] [Google Scholar]
- 18.de Vries E, van de Poll-Franse LV, Louwman WJ, de Gruijl FR, Coebergh JW. Predictions of skin cancer incidence in the Netherlands up to 2015. Br J Dermatol. 2005;152:481–8. doi: 10.1111/j.1365-2133.2005.06386.x. [DOI] [PubMed] [Google Scholar]
- 19.Stang A, Pukkala E, Sankila R, Söderman B, Hakulinen T. Time trend analysis of the skin melanoma incidence of Finland from 1953 through 2003 including 16,414 cases. Int J Cancer. 2006;119:380–4. doi: 10.1002/ijc.21836. [DOI] [PubMed] [Google Scholar]
- 20.Hussain SK, Sundquist J, Hemminki K. Incidence trends of squamous cell and rare skin cancers in the Swedish national cancer registry point to calendar year and age-dependent increases. J Invest Dermatol. 2010;130:1323–8. doi: 10.1038/jid.2009.426. [DOI] [PubMed] [Google Scholar]
- 21.Birch-Johansen F, Jensen A, Mortensen L, Olesen AB, Kjær SK. Trends in the incidence of nonmelanoma skin cancer in Denmark 1978-2007: Rapid incidence increase among young Danish women. Int J Cancer. 2010;127:2190–8. doi: 10.1002/ijc.25411. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy WH. The Australian experience in sun protection and screening for melanoma. J Surg Oncol. 2004;86:236–45. doi: 10.1002/jso.20086. [DOI] [PubMed] [Google Scholar]
- 23.Abarca JF, Casiccia CC. Skin cancer and ultraviolet-B radiation under the Antarctic ozone hole: Southern Chile, 1987-2000. Photodermatol Photoimmunol Photomed. 2002;18:294–302. doi: 10.1034/j.1600-0781.2002.02782.x. [DOI] [PubMed] [Google Scholar]
- 24.Bulliard JL, Panizzon RG, Levi F. Melanoma prevention in Switzerland: Where do we stand? Rev Med Suisse. 2006;2:1122–5. [PubMed] [Google Scholar]
- 25.Moan J, Dahlback A. The relationship between skin cancers, solar radiation and ozone depletion. Br J Cancer. 1992;65:916–21. doi: 10.1038/bjc.1992.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wakeford R. The cancer epidemiology of radiation. Oncogene. 2004;23:6404–28. doi: 10.1038/sj.onc.1207896. [DOI] [PubMed] [Google Scholar]
- 27.el Khwsky F, Bedwani R, D’Avanzo B, Assaad S, el Shafei Ali A, Mokhtar S, et al. Risk factors for non-melanomatous skin cancer in Alexandria, Egypt. Int J Cancer. 1994;56:375–8. doi: 10.1002/ijc.2910560314. [DOI] [PubMed] [Google Scholar]
- 28.Richmond-Sinclair NM, Pandeya N, Ware RS, Neale RE, Williams GM, van der Pols JC, et al. Incidence of basal cell carcinoma multiplicity and detailed anatomic distribution: Longitudinal study of an Australian population. J Invest Dermatol. 2009;129:323–8. doi: 10.1038/jid.2008.234. [DOI] [PubMed] [Google Scholar]
- 29.Mackie RM, Quinin AG. Non-melanoma skin cancer and other epidermal skin tumors. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7th ed. Oxford: Blackwell Science Publication; 2004. pp. 36.1–36.50. [Google Scholar]
- 30.Grossman D, Leffell D. Wolff K, Goldsmith K, Katz S, Gilchrest B, Paller A, Leffell D. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: McGraw-Hill; 2008. Squamous cell carcinoma; pp. 1028–36. [Google Scholar]


