Abstract
Background:
The prevalence of hypertension is on the increase in Nigeria. Prehypertension is considered a precursor of hypertension and a predictor of excessive cardiovascular risk. Identifying individuals with prehypertension and initiating effective measures will aid in reducing the incidence and prevalence of hypertension in our environment. The aim of this study was to quantify the magnitude of prehypertension and determine its associations among adults in a representative semi-urban Nigerian population.
Methods:
A cross-sectional study which was carried out in a semi-urban setting in Southeast Nigeria. Blood pressure (BP) was measured using the standard methods. A cardiovascular risk factor screening based on physical characteristics, individual medical, and family history of participants was done.
Results:
There were a total of 389 participants comprising 223 (57.3%) males and 116 (42.7%) females; male:female ratio been 1.9:1. The prevalence of prehypertension and hypertension were 45.5% and 37.8%, respectively. Males were significantly more likely to have prehypertension than females (61% vs. 39% respectively; OR = 1.32, P = 0.03). There was a weak positive significant correlation between age and both systolic (r = 0.16, P < 0.01) and diastolic (r = 0.12, P = 0.02) blood pressures. Up to 72.6% of individuals with prehypertension have abnormal body mass index (BMI). While up to 8.5% of the participants had a family history of cardiovascular disease, 20.3%, and 17.3% had a history of significant intake of alcohol and smoking, respectively.
Conclusions:
The prevalence of prehypertension in the community was high. It was associated with increasing age, male gender, and increasing BMI. Interventions at this stage may aid in stemming the rising prevalence of hypertension in our environment.
Keywords: Body mass index, cardiovascular risk factors, hypertension, Nigeria, obesity, prehypertension
INTRODUCTION
The term prehypertension was first introduced as a blood pressure (BP) category by the Seventh Joint National Committee on prevention, detection, evaluation, and treatment of high BP (JNC-7) in 2003, replacing former categories of “high-normal” and “above-optimal” BP.[1] The rationale for redefining this category was to emphasize the excess risk associated with BP in this range and to focus increased clinical and public health attention on prevention. This report, published in 2003, originally proposed the following classification based upon the average of two or more properly measured readings at each of two or more visits after an initial screen;[1]
Normal BP – systolic <120 mmHg and diastolic <80 mmHg
Prehypertension – systolic 120–139 mmHg or diastolic 80–89 mmHg.
According to JNC-7, prehypertension is not a disease entity, rather it is a reminder to intervene in the patients’ lifestyle immediately in order to prevent its progression to hypertension.[1] These definitions were re-affirmed by he eighth report of the JNC[2] and by the American Society of Hypertension/International Society of Hypertension.[3]
The mechanism of excess risk from prehypertension is presumed to be the same as that from hypertension.[4] It is known that prehypertension is associated with subclinical atherosclerosis, including increased coronary atherosclerosis[5] and increased carotid and brachial intima-media thickness.[6] In addition, prehypertension is associated with oxidized low-density lipoproteins,[6] elevations in the blood level of C-reactive protein,[7,8] tumor necrosis factor,[8] and homocysteine.[8]
Reports from the third National Health and Nutrition Examination Survey (NHANES-III; 1999–2000) in the USA showed that the prevalence of prehypertension is 31%, with no apparent difference by race/ethnicity.[9] Women were less likely to have prehypertension than men (23% vs. 40%).[9] In the same study individuals aged more than 60 years of age were less likely to have prehypertension than younger individuals (24% vs. 34%), probably because the majority of individuals in the older age group (65%) have progressed to clinical hypertension.[9] Like hypertension, prehypertension tends to cluster with other metabolic risk factors such as dyslipidemia and obesity, hence, predisposing affected individuals to the higher risk of cardiovascular diseases. For example, a meta-analysis of approximately 1 million individuals from 61 long-term epidemiological studies demonstrated that for each 20 mmHg increase in systolic BP (SBP) or 10 mmHg increase in diastolic BP (DBP) over 115/75 mmHg, there was a 2-fold increase in mortality associated with coronary artery disease and stroke.[10]
Only a few studies have addressed the magnitude of prehypertension and factors associated with it in Nigerian adults. One of such studies was carried out among adults in the community[11] and the other, among treated diabetic patients in an out-patient clinic;[12] both in Northern Nigeria. Other studies on prehypertension focused mainly on the adolescents.[13,14,15,16,17] We do not know the magnitude of prehypertension among adults in our environment and its determinants/associations. Hence, the aim of this study is to determine the magnitude of prehypertension among adults in a semi-urban Nigerian community. The objectives are to obtain the point prevalence of prehypertension and the magnitude of some cardiovascular risk factors in the community. We also sought to establish an association between BP and these risk factors if any.
METHODS
This was a cross-sectional study carried out in Olokoro, a semi-urban community in Umuahia South Local Government Area of Abia state, South-East Nigeria. The community is about 8 km from Umuahia town, the state capital. The inhabitants are predominantly Igbos, mostly Christians, and traders with few civil servants and farmers.
The study population included adults from the age of 18 years and above who presented during the medical screening exercise carried out in the study site in April 2013.
A previous study in Lagos, Nigeria among male footballers[18] showed that 47.3% of the players had prehypertension. The minimum sample size for this study was extrapolated from this value with 95% confidence and an error of margin of 5% using the appropriate formular.[19] This gave a minimum sample size of 383.
Participants who consented to the study were consecutively selected. Consenting adults, 18 years or older were included in the study. Those participants that had a psychiatric illness, who were acutely or chronically ill-looking or manifested hypertensive emergency were excluded from the interview. Furthermore, females who were pregnant or currently menstruating at the time of the study, and participants with symptoms suggestive of urinary tract infection were excluded from the study.
The screening exercise was executed in two stages.
Stage 1 involved recording the sociodemographic data of the participants and taking a brief medical history
Stage 2 involved measurement of BP, anthropometric data collection, treating any diagnosed medical illness and dipstick urine test for protein.
At this stage also, participants with abnormal results were informed and referred to the nearby hospital for follow up.
The BP was measured on the non-dominant arm using a mercury sphygmomanometer (Accoson, England) at heart level using appropriate cuff size. The subjects were allowed to relax for 3–5 min in a sitting position before assessment of BP. Hypertension was defined as a SBP ≥140 mmHg or DBP ≥90 mmHg and/or concomitant use of antihypertensive agents.[1] Two readings were obtained at an interval of 5 min and the average of the two reading recorded. The BP findings were grouped according to the Seventh JNC report on detection, evaluation, and treatment of high BP (JNC-7)[1] report staging of hypertension in which the systolic and diastolic pressures were equally weighted and either of them qualified the patient for a BP group. The JNC-7 guideline described the optimal BP as a SBP <120 and DBP of <80 mmHg. The next category of BP measurements comes under the term prehypertension which includes the range of SBP of 120-139 or diastolic pressure of 80–89 mmHg; either of which qualified the individual as having prehypertension. BP readings equal or greater than a systolic of 140 mmHg and/or diastolic of 90 mmHg were classified as hypertension stage 1 (SBP 140–159 mmHg and/or DBP 90–99 mmHg) or stage 2 for BPs equal or greater than 160 mmHg systolic and/or 100 mmHg diastolic.
Participants were instructed on the modality of collecting mid-stream urine specimen. Thereafter they provided urine samples which were tested using urinary dipstick combi-10 test strips (CHUNGO Pharm, Korea). Significant proteinuria was defined as dipstick positive for a protein of 1+ and above.
Weights were taken using bathroom scale (Hana Weighing Scale, China) after removal of shoes and heavy clothing, while the heights were recorded using stadiometer. The body mass index (BMI) was calculated from the measured weight (in kilograms) and height (in metres) and were categorized as normal (BMI 18-24.9 kg/m2), overweight (BMI = 25–29.9 kg/m2) or obese (BMI ≥ 30 kg/m2) according to the 2000 WHO criteria.[20]
A cardiovascular risk factor screening based on physical characteristics, individual medical, and family history of participants were also done.
Permission for the study was obtained from the local government authority and consent obtained from the participants. Data were consistently recorded on assessment forms administered by 4 assessors who were trained for the study.
Statistical analysis
The Statistical Package for Social Sciences (SSPS Inc., Chicago, IL, USA) version 20.0 statistical software was used for data analysis. For continuous variables, mean values, and standard deviations were calculated and the means compared using independent sample t-test. Categorical variables were compared using the Chi-squares. Cross-tabulation was used to analyze the relationship between the BMI, grades of BP (SBP and DBP), and proteinuria in the respondents. Correlation analysis was used to assess the relationship between age and BP (SBP and DBP) in respondents. All tests were two-tailed with P < 0.05 taken as statistically significant.
RESULTS
There were a total of 389 participants comprised 223 (57.3%) males and 116 (42.7%) females; male:female ratio been 2:1. There were more traders (44%) and farmers (27%) than other occupational groups [Table 1]. Majority of the participants (88%) had received one form of formal education [Figure 1].
Table 1.
Sociodemographic characteristics of the participants
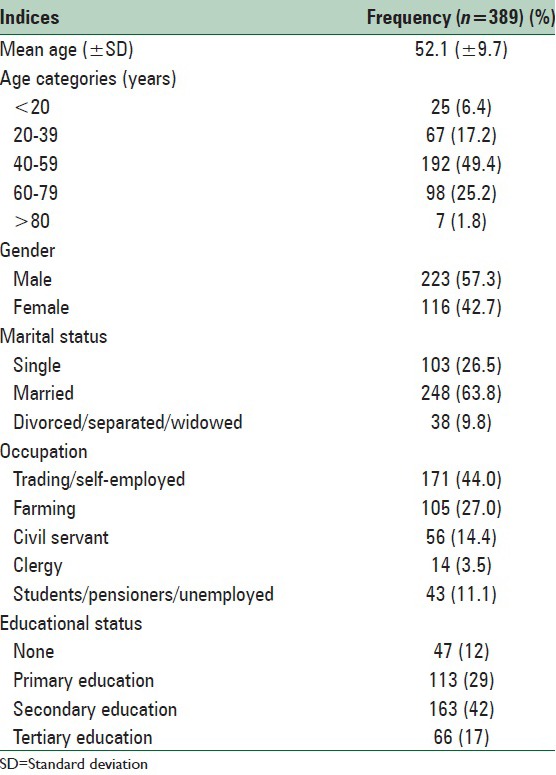
Figure 1.
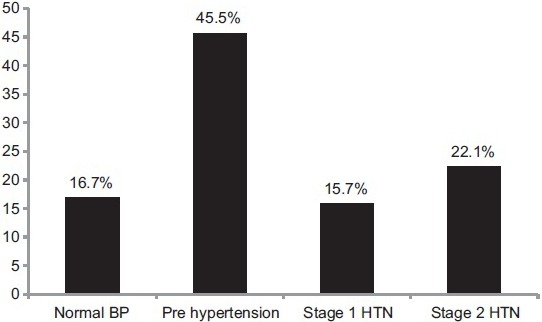
Distribution of Blood pressure among the participants, HTN = Hypertension
The distribution of the participants according to BP category is as shown in Figure 1. The prevalence of prehypertension in this study is 45.5%. Males were significantly more likely to have prehypertension than females (61% vs. 39% respectively; odds ratio [OR] = 1.32, P = 0.03).
The prevalence of hypertension in this study was 37.8%. The mean SBP was 141.8 ± 19.3 mmHg, while mean DBP was 80 ± 12.4 mmHg. There was a weak positive significant correlation between age and both SBP (r = 0.16, P < 0.01) and DBP (r = 0.12, P = 0.02).
The mean BMI was 27.3 ± 3.6 mmHg and its distribution among the different BP categories is shown in Table 2. There was a weak positive significant correlation between BMI and DBP (r = 0.43, P = 0.01). The distribution of some cardiovascular risk factors is as illustrated in Figure 2.
Table 2.
Cross-tabulation showing distribution of BMI among the BP categories
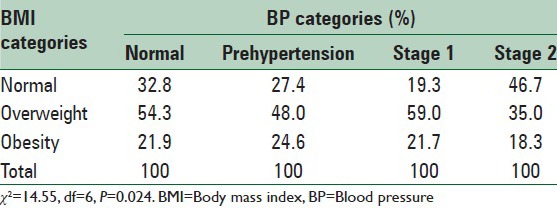
Figure 2.
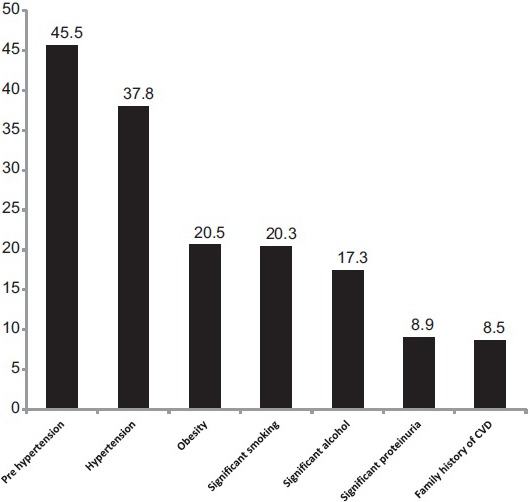
Distribution of prehypertension and some cardiovascular risk factors among the participants, CVD = Cardiovascular disease
DISCUSSION
The main findings of this study were that majority of participants were traders/self-employed and farmers and most had received some form of education. There was a high prevalence of prehypertension, more common among males, the younger age group, smokers, and participants with overweight.
The prevalence of prehypertension among the participants in this study was 45.5%. This is comparable to the prevalence of 47.3% obtained among male football players in Lagos, Nigeria.[21] However, It is higher than 31% reported in the NHANES among non-institutionalized adults in the USA,[9]34.3% reported from Indonesia,[22] and 28.8% among young people in South-Eastern Nigeria.[23] This higher value may be because majority of the participants in our study were traders and artisans [Table 1]. Ulasi et al. had earlier reported a high prevalence of high BP among traders in Nigeria.[24] This is because they sit in one place to conduct their businesses (sedentary lifestyle) and may not have regular exercise. In addition, they spend most of the day at the market and depend on food vendors for most of their meals. The typical local meal of the community consists mainly of root crops of yam and processed cassava. These have been shown to have naturally low sodium and mineral content.[25] Hence, they are often salt-laden during preparation to improve the taste. All these are possible risk factors for high BP in traders. The high prevalence of prehypertension obtained in this study is worrisome and calls for urgent attention. Proper intervention at this stage would help in controlling the pandemic of hypertension.
In this study, males were found to be more likely to have prehypertension than females. This is also in line with earlier observations[9,26] and may be due to the cardiovascular protective effect of the female hormones during premenopause. This may also be due to differences in health seeking behavior; as females are more likely than men to present to the hospital for various health related issues including antenatal visits, family planning, and well woman clinics.[27,28] All these are opportunities for casual BP checks and institution of corrective measures as necessary.
Advancing age is by far the strongest independent risk factor for cardiovascular disease risk in multiple risk factor algorithms.[29] Above the age of 60 years, individuals with prehypertension are more likely to have progressed to hypertension.[9] Hence, prehypertension is more common in lower age groups.[9] Our study corroborates this finding as majority of the participants with prehypertension (61%) were <60 years.
The prevalence of obesity in this study is similar to earlier reports of obesity prevalence among adult Nigerians.[30] The findings of our study suggest that although other factors might be responsible for a raised DBP, about 20% of such increase is accounted for by increasing BMI.
Smoking is a strong independent risk factor for cardiovascular disease.[29] Smoking causes an immediate increase in BP and heart rate that persists for more than 15 min after one cigarette.[31] People who smoke show higher ambulatory BP levels than non-smokers.[31] More than 20% of individuals with prehypertension in our study were a current smoker. This calls for urgent attention to initiate smoking cessation therapy in these individuals to prevent future adverse cardiovascular outcomes.
This study has some limitations which deserve mentioning. Firstly, the participants were not selected randomly but consecutively and only those who presented for the screening exercise. This may have introduced some selection bias in the study. Furthermore, the responses elucidated in terms of smoking, alcohol, and family history of cardiovascular diseases could not be validated as we would have if we had embarked on an audit of practices. However, this would have been difficult, cumbersome and expensive.
CONCLUSIONS
The magnitude of prehypertension is high in this semi-urban community of southern Nigeria. Male sex, younger age, and increasing BMI were significantly associated with prehypertension. The proportion of individuals with hypertension, obesity, and history of significant intake of smoking and alcohol is equally high. This calls for urgent attention from health care providers, policymakers, and the general public.
RECOMMENDATION
We must act now. Interventions to control prehypertension should be instituted at the point of diagnosis. For most patients, this consists of lifestyle modifications that lower BP. Lifestyle modifications include the dietary approach to stop hypertension plan, reduced sodium intake, weight loss, regular physical activity, moderation of alcohol intake, and cessation of smoking.[1,32]
The JNC-7 report recommends drug treatment “if a trial of lifestyle modification fails to reduce BP to 130/80 mmHg or less” in patients with either diabetes mellitus or chronic kidney disease[1] implying that prehypertension in these clinical subgroups should be treated pharmacologically.
These interventions, if properly applied will go a long way in reducing the number of individuals that eventually develop hypertension; hence aid in the fight against the hypertension pandemic.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 3.Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3–15. doi: 10.1097/HJH.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 4.Svetkey LP. Management of prehypertension. Hypertension. 2005;45:1056–61. doi: 10.1161/01.HYP.0000167152.98618.4b. [DOI] [PubMed] [Google Scholar]
- 5.Washio M, Tokunaga S, Yoshimasu K, Kodama H, Liu Y, Sasazuki S, et al. Role of prehypertension in the development of coronary atherosclerosis in Japan. J Epidemiol. 2004;14:57–62. doi: 10.2188/jea.14.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toikka JO, Laine H, Ahotupa M, Haapanen A, Viikari JS, Hartiala JJ, et al. Increased arterial intima-media thickness and in vivo LDL oxidation in young men with borderline hypertension. Hypertension. 2000;36:929–33. doi: 10.1161/01.hyp.36.6.929. [DOI] [PubMed] [Google Scholar]
- 7.King DE, Egan BM, Mainous AG, 3rd, Geesey ME. Elevation of C-reactive protein in people with prehypertension. J Clin Hypertens (Greenwich) 2004;6:562–8. doi: 10.1111/j.1524-6175.2004.03577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chrysohoou C, Pitsavos C, Panagiotakos DB, Skoumas J, Stefanadis C. Association between prehypertension status and inflammatory markers related to atherosclerotic disease: The ATTICA Study. Am J Hypertens. 2004;17:568–73. doi: 10.1016/j.amjhyper.2004.03.675. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: New challenges of the old problem. Arch Intern Med. 2004;164:2126–34. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- 10.Robinson SC, Brucer M. Range of normal blood pressure: A statistical and clinical study of 11,383 persons. Arch Intern Med. 1939;64:409–44. [Google Scholar]
- 11.Isezuo SA, Sabir AA, Ohwovorilole AE, Fasanmade OA. Prevalence, associated factors and relationship between prehypertension and hypertension: A study of two ethnic African populations in Northern Nigeria. J Hum Hypertens. 2011;25:224–30. doi: 10.1038/jhh.2010.56. [DOI] [PubMed] [Google Scholar]
- 12.Nwankwo E, Ene A, Nwankwo B. Prevalence of prehypertension, hypertension and high body mass index in newly presenting diabetics in sub-Saharan Africa. Internet J Trop Med. 2007;5:1. [Google Scholar]
- 13.McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640-4–644.e1. doi: 10.1016/j.jpeds.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 14.Ujunwa FA, Ikefuna AN, Nwokocha AR, Chinawa JM. Hypertension and prehypertension among adolescents in secondary schools in Enugu, South East Nigeria. Ital J Pediatr. 2013;39:70. doi: 10.1186/1824-7288-39-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong B, Jin XJ, Su YL, Xiao L, Cai QF, Zou HF, et al. Epidemiological survey on pre-hypertension and hypertension prevalence among adolescents aged 11 to 17 years in Shanghai. Zhonghua Xin Xue Guan Bing Za Zhi. 2012;40:427–31. [PubMed] [Google Scholar]
- 16.Odey F, Anah M, Ansa V, Ogbeche J, Meremikwu M, Ekanem E. Pre-hypertension and hypertension in apparently healthy adolescents in Calabar, Nigeria. Glob J Community Med. 2009;2:13–20. [Google Scholar]
- 17.Oyewole OO, Oritogun KS. Pre-hypertension and hypertension in adolescence: How much does it occur in a Nigerian community? West Afr J Med. 2012;31:71–5. [PubMed] [Google Scholar]
- 18.Owoeye OB, Olawale OA, Tella BA, Ajuluchukwu JN, Akinbo SR. Prevalence of hypertension and pre-hypertension in male adolescent football: A cross-sectional cohort study of Nigerian Players. Am J Hypertens Res. 2013;1:26–8. [Google Scholar]
- 19.Araoye MO. Ilorin: Nathadex Publication; 2004. Research Methodology with Statistics for Health and Social Sciences. [Google Scholar]
- 20.Geneva, Switzerland: World Health Organization; 1997. World Health Organization. Report of a WHO Consultation on Obesity. Obesity Preventing and Managing the Global Epidemic. [PubMed] [Google Scholar]
- 21.Owoeye OBA, Olawale OA, Tella BA, Ajuluchukwu JN, Akinbo SRA. Prevalence of hypertension and pre-hypertension in male adolescent football: A cross-sectional cohort study of Nigerian Players. Am J Hypertens Res. 2013;1:26–8. [Google Scholar]
- 22.Felix FW, Lucyana AS, Nadya RV, Barus GA, Pradana CE. Prehypertension and hypertension among young Indonesian adults at a primary health care in a rural area. Med J Indones. 2013;22:39–45. [Google Scholar]
- 23.Nwazor FO, Oputa SC. Blood pressure pattern among young people in South-Eastern Nigeria: A cross-sectional survey. Ebonyi Med J. 2012;11:1–6. [Google Scholar]
- 24.Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in Enugu, Nigeria. Int J Hypertens 2011. 2011 doi: 10.4061/2011/869675. 869675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oluyemi EA, Akinlua AA, Adenuga AA, Adebajo MB. Mineral contents os some commonly consumed Nigerian foods. Eur J Sci Res. 2005;6:11–5. [Google Scholar]
- 26.Coresh J, Wei GL, McQuillan G, Brancati FL, Levey AS, Jones C, et al. Prevalence of high blood pressure and elevated serum creatinine level in the United States: Findings from the third National Health and Nutrition Examination Survey (1988-1994) Arch Intern Med. 2001;161:1207–16. doi: 10.1001/archinte.161.9.1207. [DOI] [PubMed] [Google Scholar]
- 27.Akinkugbe OO. Lagos: Federal Ministry of Health; 1997. Non communicable disease in Nigeria: Final Report of National Survey. [Google Scholar]
- 28.Omemu VO, Okojie OH, Omemu CE. Awareness of high blood pressure status, treatment and control in a rural community in Edo state. Niger J Clin Pract. 2007;10:208–12. [PubMed] [Google Scholar]
- 29.Wald NJ, Simmonds M, Morris JK. Screening for future cardiovascular disease using age alone compared with multiple risk factors and age. PLoS One. 2011;6:e18742. doi: 10.1371/journal.pone.0018742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chukwuonye II, Chuku A, John C, Ohagwu KA, Imoh ME, Isa SE, et al. Prevalence of overweight and obesity in adult Nigerians-a systematic review. Diabetes Metab Syndr Obes. 2013;6:43–7. doi: 10.2147/DMSO.S38626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31:1281–357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 32.Okwuonu CG, Emmanuel CI, Ojimadu NE. Perception and practice of lifestyle modification in the treatment of hypertension among hypertensives in South-East Nigeria. Int J Med Biomed Res. 2014;3:121–31. [Google Scholar]


