Abstract
Background
Congenital cardiovascular malformations are the most common category of birth defects and responsible for mortality in the first twelve months of life. Critical congenital heart disease (CCHD) will be present in approximately one quarter of these children, which requires catheter or surgery intervention in the first year of life.
Aim
To determine the accuracy of pulse oximetry for detecting clinically unrecognized CCHD in the newborns.
Methods
Pulse oximetry was performed on clinically normal newborns within first 4 hours of life. If screening oxygen saturation (SpO2) was below 90%, echocardiography was then performed. Inclusion criteria: All newborns who were admitted in postnatal ward & NICU. Exclusion criteria: Out born babies and babies with a prenatal diagnosis of duct dependent circulation.
Results
Pulse-oximetric screening was performed on 2110 clinically normal newborns. Low SpO2 (<90%) was found in eight babies seven of them had CCHD, including three neonates with TGA, two with tricuspid atresia, one with tetralogy of fallot and one with transposition of great vessels. A pulse oximetry cut-off value of below 90% for detecting CCHD showed 100% sensitivity, 99.95% specificity, 87.50% positive predictive value, 100% negative predictive value.
Conclusions
Pulse oximetry is safe, feasible and noninvasive, can be used as screening tool for detecting CCHD in clinically normal newborn. If SpO2 is below 90% in clinically normal newborns within 4 hours of birth, urgent echocardiography is suggested to rule out CCHD.
Keywords: Critical, Heart defect, Pulse Oximetry, Newborn, Screening
Introduction
Congenital cardiovascular malformations (CHD) are the most common group of birth defects, occurring in 6 to 8 per 1000 live births and are responsible for most deaths in the first 12 months of life. 1,2 One quarter of these children will have critical congenital heart disease (CCHD), which requires surgery or catheter intervention in the first year of life. 3 Early diagnosis of CHD is important because the delayed diagnosis of CCHD can lead to cardiac failure, cardiovascular collapse and even death. CCHD in the newborn may have low oxygen saturations unrecognized clinically. Pulse oximetry is a well established, exact, noninvasive test for quantification of hypoxemia. Use of this screening method for early detection of CCHD is based on clinically undetectable hypoxemia in potentially life-threatening cases. 3,4 Several studies have documented the lack of sensitivity of routine neonatal examination in detecting CHD. 4-6 Many neonates with CHD have no signs that can be detected by clinical examination. 5,6 Recent studies have reported a high sensitivity and specificity for pulse oximetry for early detection of CHD in newborn babies. 7-10 In developing countries with inadequate medical staff, this method can be very helpful in early detection of CCHD. Our study was designed to find the incidence of clinically unrecognized CCHD by using pulse oximetry in a rural hospital.
Material & Methods
This was a prospective hospital-based study conducted in the Level II Neonatology Unit of Pediatric Department at Acharya Vinoba Bhave Rural Hospital (AVBRH) from April 2012 to January 2013. AVBRH is a 1206 bedded fully equipped teaching Hospital attached to the Medical College with state of the art facilities at Sawangi Meghe, Wardha, India.
Inclusion criteria: All newborns who admitted in postnatal ward & NICU. Exclusion criteria: Out-born babies and those neonates with a prenatal diagnosis of duct dependent circulation by fetal echocardiography. The measurements of SpO2 were performed using a Massimo Single Extraction Technology (SET) handheld pulse oximeter with a neonatal reusable Nellcor SpO2 sensor OXI-A/N probe. For each newborn, SpO2 was measured by a trained social worker on all the four limbs of the newborn within the first 4 hours of life. The probe was held manually to the wrist or palm and to the sole of the foot, following a random order. It usually required 5-6 minutes for all 4 measurements to be performed.
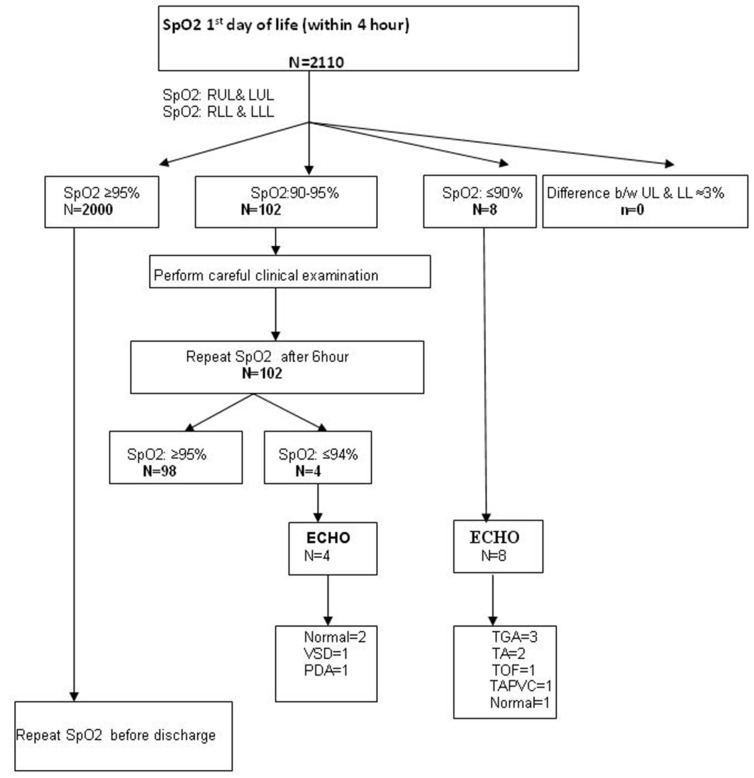
An SpO2 result of ≥95% was considered normal. If the SpO2 difference between the right upper limb and lower limb was ≥3%, then echocardiography was done. If the SpO2 was between 90-94%, clinical examination was performed carefully. If CHD was suspected, the neonate was referred for echocardiography. If no suspicion of CHD was made clinically, then measurement of SpO2 was repeated after 6 hours and echocardiography done if SpO2 persisted ≤95%. When the SpO2 reading was ≤90%, bedside echocardiography was done. For normal babies, a follow-up evaluation (clinical evaluation) was performed at 6 weeks. At this point of evaluation, if the newborn had abnormal cardiac examination including a finding of SpO2 <90%, echocardiography was done. Figure 1 shows the flow chart of the study design.
Figure 1.
Flow chart of the study design.
CCHD is defined as lesions that include cyanotic defects such as tetralogy of Fallot, pulmonary atresia, truncus arteriosus, transposition of the great vessels, total anomalous pulmonary venous return, and tricuspid atresia, as well as left-sided obstructive lesions, including coarctation of the aorta, critical aortic stenosis, interrupted aortic arch, and hypoplastic left heart syndrome. All other heart disease are labelled as non-critical CHD (including patent foramen ovale or ASD <5 mm, PDA <2 mm).
Neonates who developed signs or symptoms suggestive of a cardiac defect were evaluated, including blood pressure, electrocardiogram, chest radiograph, pulse oximetry and echocardiography. An informed consent was obtained from one of the parents (preferably by mother) before initial screening. The study protocol was approved by the ethical committees of the Institute.
The diagnostic accuracy of pulse oximetry was measured by computation of sensitivity, specificity, positive and negative predictive values. STATA 12 software was used for the statistical analysis.
Results
During the study period there were 2110 (Male: 1071; Female: 1039) live born neonates at AVBR Hospital. Oximetry screening was performed on all newborns. There were eight neonates with SpO2< 90%, 102 neonates with SpO2 between 90-95% and 2000 neonates with SpO2 >95%. Seven out of eight neonate with SpO2<90% had CCHD, three neonates had TGA, two had tricuspid atresia, one had tetralogy of Fallot and one had transposition of great vessels.
Out of 102 with SpO2 90-95%, 98 neonates showed normal SpO2 when repeated after 6 hours from the initial measurement. Four still showed low SpO2. Out of these two where detected to have CHD, one with VSD and one with PDA. Table 1 shows the comparison between well and low saturated groups. The mean SpO2 in the first four hour of life in well saturated group (SpO2 ≥ 95%) was 98.1 and 82.5% in the low saturated group (SpO2 ≤ 90%). There were 27 neonates with CHD in this study period, the incidence was 21.85 per 1000 live births and CCHD was 3.33 per 1000. A pulse oximetry cut-off value of below 90% for detecting CCHD showed 100% sensitivity, 99.95% specificity, 87.50% positive predictive value, 100% negative predictive value. A pulse oximetry cut-off value of below 95% showed 100% sensitivity, 95.08% specificity, 6.36% positive predictive value, 100% negative predictive value.
Table 1.
Comparison between Well Saturation (≥90%) & Low Saturation (<90%) groups
| Parameter | Well Saturation | Low Saturation (CCHD) |
|---|---|---|
| • Newborns | 2103 | 7 |
| • Mean gestation age | 38.6 Wk | 38.2Wk |
| • Mean body weight | 2.7Kg | 2.3Kg |
| • Mean oxygen saturation of right hand | 99.1 | 86 |
| • Mean oxygen saturation of left hand | 98.5 | 84 |
| • Mean oxygen saturation of right leg | 99.3 | 83 |
| • Mean oxygen saturation of left leg | 98.2 | 85 |
Discussion
CHD are a leading cause of infant deaths in the developed world. Delayed diagnosis of CHD is associated with a worse preoperative condition. 2 In our study the incidence was 21.85 per 1000 live birth which is higher than the previous reported study. 10-17 The incidence CCHD was 3.33 per 1000 live births in our study which is in agreement with a previous study. 8 Brown KL et al 11 reported that 25% of infants with CCHD were not diagnosed with heart disease until after discharge from the nursery. A number of children with CCHD are so severely compromised at presentation that they die before surgical intervention. Screening infants with non-invasive measurement of oxygen saturation has been proposed as an aid for early detection of duct dependent circulation. CCHDs are structural heart defects that often are associated with hypoxia among infants during the newborn period. Infants with CCHDs are at risk for significant morbidity or mortality because there circulation is duct dependent. Vaidyanathan B et al 12 reports a poor sensitivity for pulse oximetry, as well, for detection of CHD. Pulse oximetry was also found to have a low predictive value. This may be due to the fact that only four patients in this study had critical CHD with cyanosis.
The study done by Koppel RI et al 8 reported the effectiveness of pulse oximetry screening for CHD in asymptomatic newborns (sensitivity: 60%; specificity: 99.95%; positive predictive value: 75%; negative predictive value: 99.98%; accuracy: 99.97%). Similarly, de Wahl Granelli A et al1 revealed that systematic screening for CCHD with high accuracy required a new generation oximeter, and comparison of saturation values from the right hand and one foot substantially improves the detection of CCHD (sensitivity: 98.5%; specificity: 96.0%; positive predictive value: 89.0%; negative predictive value: 99.5%). In our study, for detecting CCHD, pulse oximetry (SpO2) cut-off value of below 90% showed 100% sensitivity, 99.95% specificity, 87.50% positive predictive value, 100% negative predictive value.
As CCHD may not be apparent at the time of early discharge examination, post-ductal arterial pulse oximetry screening during the first 24 hours of life has been put forth as the most useful strategy to prevent circulatory collapse or death. 9-13 Previous studies have suggested that performing pulse oximetry on all newborns before hospital discharge is an effective screening tool for detection of CCHD. 14-16 Mostly in institutions, pulse oximetry prior to discharge from the newborn nursery is not performed routinely. And even screening is also not done regularly.
Pulse oximetry is a safe, noninvasive, inexpensive, excellent detection rate and reasonably sensitive test that will detect many cases of CCHD. Earlier diagnosis of CCHD may lead to earlier interventions and improved patient outcomes. 17-19 The limitation of the study is that the number of screened neonates are small and no cases of coarctation of aorta were picked up to validate the difference of oxygen saturation in the right arm and leg. The strengths of the study was that it screened large numbers of newborns to rule out CCHD with the help of cheap, non-invasive, and ubiquitous pulse oximetry devices. The weakness of the study was it would not detect all forms of congenital heart disease, and the inevitable false positives cases.
Conclusion
This study suggested that the pulse oximetry, which is noninvasive and cost-effective, can be used as a screening tool for detecting CCHD in clinically normal newborns. If oxygen saturation is below 90% in clinically normal newborns within first 4 hours of birth, urgent echocardiography is suggested to rule out CCHD. To decrease the false-positive cases, neonatal screening for CCHD should be done after 24 hrs of life. This results in a decreased burden for echocardiography services.
References
- 1. de Wahl Granelli A, Mellander M, Sunnegårdh J, Sandberg K, Ostman-Smith I. Screening for duct-dependant congenital heart disease with pulse oximetry: a critical evaluation of strategies to maximize sensitivity. Acta Paediatr 2005;94:1590–6. [DOI] [PubMed] [Google Scholar]
- 2. Riede FT, Worner C, Dahnert I, Mockel A, Kostelka M, Schneider P. Effectiveness of neonatal pulse oximetry screening for detection of critical congenital heart disease in daily clinical routine - results from a prospective mulicenter study. Eur J Pediatr. 2010;169:975-981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren CN. Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis. Health Technol Assess 2005;9:1–168. [DOI] [PubMed] [Google Scholar]
- 4. Meberg A, Otterstad JE, Frøland G, Hals J, Sörland SJ. Early clinical screening for congenital heart disease: the cases we miss. Cardiol Young 1999;9:169–74. [DOI] [PubMed] [Google Scholar]
- 5. Arlettaz R, Bauschatz AS, Mönkhoff M, Essers B, Bauersfeld U. The contribution of pulse oximetry to the early detection of congenital heart disease in newborns. Eur J Pediatr 2006;165:94–8. [DOI] [PubMed] [Google Scholar]
- 6. Bakr AF, Habib HS. Combining pulse oximetry and clinical examination in screening for congenital heart disease. Pediatr Cardiol 2005;26:832–5. [DOI] [PubMed] [Google Scholar]
- 7. Ewer AK, Middleton LJ, Furmston AT, Bhoyar A, Daniels JP, Thangaratinam S, et al. Pulse oximetry screening for congenital heart defects in newborn infants: a test accuracy study. Lancet. 2011. August 27;378(9793):785-94. [DOI] [PubMed] [Google Scholar]
- 8. Koppel RI, Druschel CM, Carter T, Goldberg BE, Mehta PN, Talwar R, Bierman FZ. Effectiveness of pulse oximetry screening for congenital heart disease in asymptomatic newborns. Pediatrics. 2003;111:451–455. [DOI] [PubMed] [Google Scholar]
- 9. Thangaratinam S, Daniels J, Ewer AK, Zamora J, Khan KS. Accuracy of pulse oximetry in screening for congenital heart disease in asymptomatic newborns: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2007. May;92(3):F176-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hoke TR, Donohue PK, Bawa PK, Mitchell RD, Pathak A, Rowe PC, Byrne BJ. Oxygen saturation as a screening test for critical congenital heart disease: a preliminary study. Pediatr Cardiol. 2002;23: 403– 409. [DOI] [PubMed] [Google Scholar]
- 11. Brown KL, Ridout DA, Hoskote A, Verhulst L, Ricci M, Bull C. Delayed diagnosis of congenital heart disease worsens preoperative condition and outcome of surgery in neonates. Heart. 2006;92: 1298 –1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vaidyanathan B, Sathish G, Mohanan ST, Sundaram KR, Warrier KK, Kumar RK. Clinical Screening for Congenital Heart Disease at Birth: A Prospective Study in a Community Hospital in Kerala. Indian Pediatr 2011;48: 25-30 [DOI] [PubMed] [Google Scholar]
- 13. Granelli AD, Wennergren M, Sandberg K, Mellander M, Bejlum C, Inganäs L et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39,821 newborns. BMJ. 2009;338:a3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Richmond S, Reay G, Abu Harb M. Routine pulse oximetry in the asymptomatic newborn. Arch Dis Child Fetal Neonatal Ed. 2002;87: 83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reich JD, Miller S, Brogdon B, Casatelli J, Gompf TC, Huhta JC, Sullivan K. The use of pulse oximetry to detect congenital heart disease. J Pediatr. 2003;142:268–272.73. [DOI] [PubMed] [Google Scholar]
- 16. Rosati E, Chitano G, Dipaola L, De Felice C, Latini G. Indications and limitations for a neonatal pulse oximetry screening of critical congenital heart disease. J Perinat Med. 2005;33:455–457. [DOI] [PubMed] [Google Scholar]
- 17. Richmond S, Wren C. Early diagnosis of congenital heart disease. Semin Neonatal. 2001;6:27–35. [DOI] [PubMed] [Google Scholar]
- 18. Mahle WT, Newburger JW, Matherne GP, Smith FC, Hoke TR, Koppel R, Gidding SS, Beekman RH Role of pulse oximetry in examining newborns for congenital heart disease: a scientific statement from the AHA and AAP. Pediatrics. 2009;124:823–836. [DOI] [PubMed] [Google Scholar]
- 19. Ruangritnamchai C, Bunjapamai W, Pongpanich B. Pulse oximetry screening for clinically unrecognized critical congenital heart disease in the newborns. Images Paediatr Cardiol 2007;30:10-15 [PMC free article] [PubMed] [Google Scholar]