Abstract
Homelessness among US veterans has been a focus of research for over 3 decades. Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, this is the first systematic review to summarize research on risk factors for homelessness among US veterans and to evaluate the evidence for these risk factors. Thirty-one studies published from 1987 to 2014 were divided into 3 categories: more rigorous studies, less rigorous studies, and studies comparing homeless veterans with homeless nonveterans. The strongest and most consistent risk factors were substance use disorders and mental illness, followed by low income and other income-related factors. There was some evidence that social isolation, adverse childhood experiences, and past incarceration were also important risk factors. Veterans, especially those who served since the advent of the all-volunteer force, were at greater risk for homelessness than other adults. Homeless veterans were generally older, better educated, and more likely to be male, married/have been married, and to have health insurance coverage than other homeless adults. More studies simultaneously addressing premilitary, military, and postmilitary risk factors for veteran homelessness are needed. This review identifies substance use disorders, mental illness, and low income as targets for policies and programs in efforts to end homelessness among veterans.
Keywords: clinical characteristics, homelessness, low income, mental illness, risk factors, substance abuse, veterans
INTRODUCTION
Homelessness among veterans has been of major public concern for over 3 decades. Homelessness among substantial numbers of veterans was first documented after the Civil War (1), but it was not until the early 1980s, a period characterized by high inflation and 2 economic recessions, that veteran homelessness began to be recognized as an important public health problem (2–4). Most recent estimates report that veterans are slightly overrepresented in the US homeless population with veterans constituting 12.3% of all homeless adults in the United States (5) but only 9.7% of the total US population (6).
Homelessness has been defined as not having a “fixed, regular, and adequate nighttime residence” (7, p. 1), and it includes moving frequently between different types of accommodations and staying in homeless shelters and places not meant for human habitation (e.g., vehicles, abandoned buildings). Among the general population, homelessness has been a social, economic, and public health concern in the United States and internationally since the early 1980s (8–10). Some consider homelessness a violation of a basic human right—the right to have access to safe and secure housing (11, 12). Homelessness is also a concern because it is associated with a host of other negative outcomes, including a wide range of serious medical problems (13, 14), mental health and substance abuse problems (10, 15), premature mortality (16, 17), frequent hospitalizations, greater than average costs per hospital stay (18, 19), and incarceration (20, 21).
Veterans constitute a unique segment of the US population because of their service to the nation and, as reflected in their increased access in the years since World War II (22), to special benefits such as VA health care, disability and education benefits, and home-loan guarantees. Veterans may also be more vulnerable to certain health and psychosocial problems than other adults because of their higher exposure to combat-related trauma and geographic dislocation for military deployment (23). The presence of veterans within the general US homeless population is regarded as a point of public shame by many, and public concern for their health and well-being is strong (24, 25). In 2009, Secretary Eric Shinseki of the Department of Veterans Affairs (VA) pledged to end homelessness among veterans in the next 5 years, and since then millions of dollars have been used to fund the creation and expansion of VA services for homeless veterans (26). A growing component of those efforts is a focus on the prevention of homelessness, which involves addressing key risk factors before they result in an episode of homelessness.
Veterans have been overrepresented in the homeless population since at least the late 1980s. Although this disparity has attenuated over time (5), it remains puzzling because homeless veterans are consistently found to be older, better educated, more likely to have married, and more likely to have health coverage than other homeless adults (22). By virtue of their military service, all homeless veterans also have had some employment and a work history. These advantages should put veterans at lower risk for homelessness than other homeless adults, although they appear to be at higher risk among some veteran cohorts, especially those who were recruited after the advent of the all-volunteer force in 1975 (22, 27). No comprehensive models of veteran homelessness have been formulated, but it has been recognized that premilitary, military, and postmilitary factors need to be considered in identifying risk factors for veteran homelessness (28–30).
Several reviews of studies on risk factors for homelessness in the general population have been conducted (31–33), and a broad literature review on homelessness among veterans was recently conducted by the VA's Evidence-Based Synthesis Program (34). However, to our knowledge, there has been no systematic review of risk factors for homelessness specifically among veterans in the published literature. Such a review is important as efforts to address veteran homelessness continue, government funds are directed at prevention efforts, more veterans return from recent conflicts in Iraq and Afghanistan, and the scientific community seeks to understand the body of knowledge amassed from research on the causes of homelessness among veterans.
In this systematic review, we provide a comprehensive examination of the published literature on risk factors of homelessness among US veterans. First, we compiled and categorized existing studies into 3 categories on the basis of the nature and rigor of their research designs: 1) large cohort, case-control, or other more rigorous studies based on recognized designs; 2) less rigorous, cross-sectional, descriptive, specific focus, or other uncontrolled studies; and 3) studies comparing homeless veterans with homeless nonveterans. Second, we summarized the findings of studies in each category and provide a synthesis of distinctively consistent findings across studies. Third, we describe current gaps in knowledge and recommend future areas for research. Fourth, we conclude with a discussion of the implications of these findings for policy and practice.
METHODS
A systematic and exhaustive computerized literature search of PubMed, PsycINFO, Google Scholar, Academic Search Premier, and Web of Science databases was performed by both authors of studies published in English from 1900 to July 2014. Different combinations and iterations of the following key words and medical subject headings were used to search titles and abstracts in each database: homelessness, homeless, veterans, military, risk, risk factors, characteristics, and causes. Boolean operators (e.g., AND, OR) and wildcard symbols (e.g., *) were used (e.g., search string: “homeless veteran*” AND “risk factor*” OR “homeless veteran*” AND “characteristic*”).
Only studies that met the following criteria were included in the review: 1) sampled US veterans; 2) assessed homelessness in the United States; 3) included homelessness as an outcome or dependent variable; and 4) examined variables in relation to homelessness as a main study aim with the intent to identify risk factors orcharacteristics associated with homelessness. A broad definition of homelessness was used to be inclusive of studies, which included the US Housing and Urban Development's (HUD's) definition (35), use of any specialized VA homeless services, or a documented V60.0 clinical code suggesting homelessness according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Veteran status was defined as having ever served in the US military regardless of discharge status.
Studies were excluded if they reported only the effects of a specific intervention (e.g., supported housing) or if they reported only qualitative data. Case reports, published commentaries, and letters to the editor that did not report any quantitative data were also excluded. References from all relevant literature were hand searched and used to identify additional relevant studies. Several experts in the field were contacted to inquire about additional studies or reports that may not have been found in the literature search.
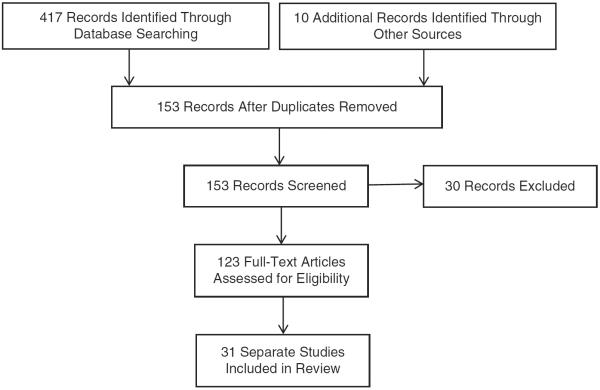
As Figure 1 shows, our search initially yielded a total of 153 individual records, which were screened generally for topic relevance and reporting of quantitative data, resulting in the exclusion of 30 of those records. The remaining 123 records were carefully examined, of which 81 were excluded because they failed to meet inclusion/exclusion criteria, resulting in a total of 32 studies that met criteria. All 32 studies included were peer-reviewed journal articles, except for 4 book chapters and 2 published governmental reports. One report (36) and one study (37) used the same data and reported similar results so they were considered one study, resulting in a total of 31 separate studies included in this review.
Figure 1.
Different phases of the search for risk factors for homelessness among US veterans in studies published from 1900 to 2014.
Our systematic review followed the guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (38). We did not conduct a meta-analysis because a varying array of measures, variables, research designs, and statistical tests were used in these studies that precluded an accurate, balanced, quantitative synthesis of this literature. However, we reported odds ratios or adjusted odds ratios (both denoted as “ORs” for simplicity) and other effect size statistics (e.g., hazard ratios, risk ratios, percentages) when available to provide readers with a sense of the magnitude of the risk factors identified. However, we do caution that these statistics must be understood in the context of each individual study and may not be directly comparable as different research designs, covariates, and measures were used in each study.
For our review, we categorized studies on the basis of the rigor of their research design and provided a narrative synthesis of their findings. We divided the 31 included studies into 3 categories: more rigorously designed studies, less rigorously designed studies, and comparative studies of homeless veterans and homeless nonveterans. One book chapter (39) contained 2 separate analyses so it was divided into 2 categories.
More rigorous studies consisted of studies that used a cohort, case-control, or clearly formulated research design that provided support for causal factors for homelessness (e.g., structural equation modeling estimates of causal relations) (40); used relatively large samples; and evaluated a broad range of sociodemographic, psychosocial, and health measures. These studies were judged to have lower risk for bias because methodologies were clearly described, more representative samples were used, and confounding variables were taken into account.
Less rigorously designed studies consisted of studies that were cross-sectional (i.e., descriptive) or had weaker research designs (e.g., case-control design with no historical controls); had relatively small sample sizes or focused descriptively on particular subgroups of homeless veterans; and utilized a limited number of psychosocial and health measures or focused on a particular domain (e.g., neurological deficits).
Comparative studies consisted entirely of studies that compared veterans with nonveterans on risk factors and characteristics associated with homelessness. These studies mostly used a cross-sectional research design, with a few exceptions (e.g., one longitudinal and one case-control design study).
RESULTS
More rigorous studies
A total of 7 studies were identified that were based on data collected between 1986 and 2011 (arranged by date of data in Table 1). Of these 7 studies, 3 were case-control studies, 3 were cohort studies, and 1 was a study that used a structural equation modeling analysis of cross-sectional data. These studies differed in their sample frames, partly based on when the studies were conducted. For example, one study sampled Vietnameraveterans(28),while 3 studies exclusively sampled Iraq and Afghanistan era veterans (36, 41, 42). It is notable that all of the studies exclusively or predominantly sampled male veterans given the predominance of males in the veteran population, except for one study that exclusively sampled female veterans (43). All of the studies used large population-based samples, except the study focused on female veterans and another study that examined subsequent homelessness among veterans who had obtained supported housing (44).
Table 1.
More Rigorous Published Studies on Risk Factors for Veteran Homelessness, 1994–2013
| First Author, Year (Reference No.) | Design | Data Source | Total No. | No. of Homeless | Sampling Frame | Study Period | Identified Risk Factors |
|---|---|---|---|---|---|---|---|
| Rosenheck, 1994 (28) | Cross-sectional study using structural equation modeling | National Vietnam Veterans Readjustment Study | 1,460 | 123 | Male Vietnam veterans | 1986–1987 | Four premilitary factors included year of birth (total effect = 0.10), childhood physical or sexual abuse (total effect = 0.10), other childhood trauma (total effect = 0.07), and foster care (total effect = 0.06). Four postmilitary factors included psychiatric disorders (total effect = 0.08), substance abuse (total effect = 0.06), being unmarried (total effect = 0.14), and low levels of social support 1 year after military discharge (total effect = 0.30). |
| O'Connell, 2008 (44) | Retrospective cohort study | Randomized controlled trial of the HUD–VASH Program | 392 | 172 subsequently homeless | Formerly homeless veterans in supported housing | 1992–1995 | Drug use upon entry into housing (RR = 12.33) and a diagnosis of PTSD (RR= 1.85) were predictive of subsequent homelessness. |
| Washington, 2010 (43) | Matched case-control study | Local survey data | 198 | 33 | Female veterans | 2005–2006 | Being unemployed (OR = 13.1), disabled (OR = 12.5), in fair or poor health (OR = 3.2), unmarried (OR = 0.1), having less than a college education (OR = 0.2), and screening positive for post-traumatic stress disorder (OR = 4.9). |
| VA Office of Inspector General, 2012 (36); Metraux, 2013 (37) | Population-based retrospective cohort study | Administrative data from VA and DoD maintained by the Office of Inspector General | 310,685 | 5,574 | Iraq and Afghanistan era veterans | 2005–2006 | Lower military pay grade (HR = 0.13–0.43), diagnosed mental illness in the military, especially psychotic disorders (HR = 1.57–4.22) and substance use disorders (HR = 1.85–2.72), traumatic brain injury (HR = 1.20–1.64), problematic military discharges (HR = 1.79–8.18), service in OEF/OIF (HR = 1.34), and active duty vs. reserves (HR = 0.74–1.34). |
| Blackstock, 2012 (42) | Population-based case-control study | Administrative data from VA | 445,319 | 7,431 | OEF/OIFVA service users | 2001–2009 | Age, 18–35 years (HR = 1.51–1.66), black (HR = 2.53), unmarried (HR = 1.32), high school education or lower (HR = 1.76), urban location (HR = 0.77), enlisted vs. military officer (HR = 2.66), VA service connection (HR = 1.45–2.35), and nearly all mental health diagnoses, especially substance use disorders and schizophrenia (HR = 1.17–3.38). |
| Edens, 2011 (45) | Population-based case-control study | Administrative data from VA | 1,120,424 | 109,056 | VA mental health service users | 2008–2009 | Diagnoses of alcohol and drug use disorders (OR = 2.0–3.3), schizophrenia (OR = 1.1), bipolar disorder (OR = 1.0), pathological gambling (OR = 2.4), personality disorders (OR = 1.6), male, urban-dwelling (OR = 0.3–0.5), lower income (OR = 0.3–0.8), age, 40–49 years (OR = 1.7), and being black (OR = 1.4). |
| Protective characteristics were VA service connection (OR = 0.3), age, ≥65 years (OR = 0.2–0.6), and service in OEF/OIF (OR = 0.4). | |||||||
| Elbogen, 2013 (41) | Retrospective cohort study | National Postdeployment Adjustment Baseline and Follow-up Survey | 1,090 | 39 | Iraq and Afghanistan era veterans | 2009–2011 | Criminal history (OR = 2.65), mental health diagnosis (OR = 2.59), income level (OR = 0.30), and money mismanagement (OR = 4.09). |
Abbreviations: DoD, Department of Defense; HR, hazard ratio; HUD–VASH, Housing and Urban Development–Veterans Affairs Supportive Housing Program; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OR, odds ratio; PTSD, post-traumatic stress disorder; RR, risk ratio; VA, Department of Veterans Affairs.
Of the 7 studies, the most consistent risk factors for homelessness identified by all studies were substance abuse and mental health problems. This was found in all 3 cohort studies (36, 41, 44), which provide support that these problems preceded homelessness. Substance abuse problems appeared to be the risk factor with the greatest magnitude of effect. Three of the 4 studies that included assessment of psychotic disorders (i.e., schizophrenia) also particularly identified psychotic disorders as a major risk factor (36, 42, 45). Post-traumatic stress disorder (PTSD) was a risk factor, but it was found to be of the same magnitude as other mental health disorders. One study did find that PTSD specifically increased a veteran's risk for returning to homelessness, but only after supported housing had led to an initial exit from being homeless (44).
Another consistent finding was that 6 of the 7 studies identified low income/poverty and income-related variables, such as military pay grade and unemployment, as risk factors for homelessness. Presumably all of the homeless veterans in these studies were poor and lacked financial resources for housing. One of these studies found that VA service connection, which is a VA source of disability compensation income, was protective against homelessness (45). Another of these studies further found that money mismanagement was a larger risk factor than income and mental health problems (7).
Three studies also suggested that lack of social support was a risk factor for homelessness. One study found that post-military social isolation after returning from the Vietnam theater had direct effects on homelessness (28), and 2 other studies identified unmarried status as a risk factor (42, 43).
There were mixed findings regarding whether service in Operation Enduring Freedom (OEF)/Operation Iraqi Freedom (OIF) increased risk for homelessness, which most likely reflected differences in the choice of comparison groups. Although one study found that OEF/OIF service was protective against homelessness when examined among a comprehensive sample of VA service users, even after adjustment for age (6), another study found that OEF/OIF war-zone service moderately increased the risk for homelessness when examined among only Iraq and Afghanistan era veterans (37). Therefore, it seems that, among veterans of all service eras, OEF/OIF war-zone service does not stand as a risk factor, but it does among veterans who have served since September 11, 2001.
Several potentially important risk factors that were identified and measured in only single studies were adverse childhood events (e.g., childhood abuse, foster care) (28) and criminal history (41).
Less rigorous studies
A total of 9 less rigorous studies were identified on the basis of data collected from 1993 to 2013 (arranged by date of data in Table 2). Seven of the studies were cross-sectional studies, and the remaining 2 were small case-control studies. These studies, although not having as rigorous research designs, as comprehensive measures, or ability to infer directionality of associations, largely supported the findings of the “more rigorous” studies. All 3 of the studies that examined substance abuse and mental health problems found that they increased the risk for homelessness (21, 46, 47), supporting findings from the more rigorously designed studies. Although no studies examined psychotic disorders specifically, one separate study examined PTSD specifically and found that veterans with PTSD were not at greater risk for homelessness than veterans with other mental health diagnoses (39), consistent with findings from the more rigorous studies. Moreover, veterans with combat exposure appeared to be at lower risk for homelessness than those without combat exposure (39). It is noteworthy that only a small number of studies actually examined mental disorders as a risk factor, because many studies sampled homeless veterans with mental illness exclusively (29, 39, 47, 48). Moreover, income level/poverty was not examined specifically as a risk factor in these studies because, almost by definition, homeless veterans in these studies were poor and impoverished. A few other less rigorous studies provide further evidence for findings of the more rigorous studies. Childhood problems were found to be weakly associated with more extensive periods of homelessness (49), providing evidence that premilitary factors increase the risk for homelessness found in a more rigorous study (28). OEF/OIF veterans were generally not found to be at higher risk for homelessness compared with veterans of other eras (50), similar to findings reported in one more rigorous study (45). The presence of neurological deficits was also found to be a potential risk factor (48), which accords with a more rigorous study that found that traumatic brain injury increases the risk for homelessness among recent non-OEF/OIF male veterans (37). Specific to the veteran population, problematic military discharges were found to be a risk factor for homelessness (29) as found in a more rigorous study (37).
Table 2.
Less Rigorous Published Studies on Risk Factors for Veteran Homelessness, 1997–2014
| First Author, Year (Reference No.) | Design | Data Source | Total No. | No. of Homeless | Sampling Frame | Study Period | Identified Risk Factors |
|---|---|---|---|---|---|---|---|
| Rosenheck, 1997 (39) | Case-control study | VA's Homeless Chronically Mentally Ill veterans program, 1987 Third Survey of Veterans, a 1990 national survey of VA outpatient mental health clinic users, and the NVVRS | 98,371 | 34,711 | Homeless veterans engaged in VA services | 1986–1992 | Military combat exposure was associated with lower likelihood for homelessness (OR = 0.48–0.85). PTSD was not associated with greater likelihood for homelessness among veterans with other mental health diagnoses (OR = 0.41–0.96). |
| Wenzel, 1993 (46) | Cross-sectional study on duration of lifetime homelessness | Domiciliary care for homeless veterans in Los Angeles | 343 | 343 | Homeless veterans enrolled in a VA domiciliary care program | 1988–1992 | Being white and having a longer period of recent homelessness, a greater number of homeless episodes, a poorer employment history, greater mental and substance use problems, and weaker social support were associated with longer term homelessness. |
| Douyon, 1998 (48) | Cross-sectional study | Assessment battery on homeless VA inpatient service users | 53 | 33 | Homeless veterans enrolled in acute inpatient care | Unknown | Neurological deficits (frontoparietal, cerebellar, and frontal lobe functions). |
| Gamache, 2000 (29) | Case-control study | ACCESS evaluation and the NVVRS | 1,676 from NVVRS; 616 from ACCESS | 616 | Homeless male veterans with mental illness | 1995–1998 for ACCESS | 6.8% of homeless veterans with mental illness had either a bad conduct or dishonorable discharge. |
| 1986–1988 for NVVRS | The relative risk for homelessness among veterans who served in the Vietnam era and had a bad conduct or dishonorable discharge is 9.9 times as great as among veterans without such discharges. | ||||||
| Tsai, 2013 (49) | Cross-sectional study on severity of homelessness | National data from the HUD–VASH Program | 1,161 | 1,161 | Homeless veterans enrolled in VA-supported housing | 1992–2003 | Conduct disorder behaviors (Cohen's d = 0.16–1.13), family instability during childhood (d = 0.47–1.43), and childhood abuse (d = 0.05–0.40) were each weakly associated with lifetime homeless episodes. |
| Mares, 2004 (47) | Cross-sectional study on perceived military risk for homelessness | Therapeutic Employment Place and Support Program evaluation | 631 | 631 | Homeless veterans enrolled in VA vocational rehabilitation | 2001–2003 | 31% of sample reported that military service increased their risk for becoming homeless. |
| Perceived risk factors included substance abuse and health problems in the military, inadequate preparation for civilian employment, loss of structured lifestyle after military, weakened social connections, and interrupted education. | |||||||
| Younger age at military discharge, greater childhood problems, and less social support were associated with more rapid homelessness after military discharge. | |||||||
| van den Berk-Clark, 2013 (51) | Cross-sectional study | VA-funded specialized transitional living programs | 59 | 33 chronically and 26 acutely homeless | Homeless elderly veterans in Los Angeles | 2003–2005 | Chronically homeless veterans were less educated and had a smaller social network, particularly for “instrumental support” than acutely homeless veterans. |
| Kasprow, 2011 (50) | Population-based cross-sectional study | VA administrative data and “VetPop 2007” | 18,997,936 | 73,740 | OEF/OIF veterans who had contact with the VA homeless services | 2001–2007 | OEF/OIF veterans were seen in VA homeless programs at a lower rate in all age categories than other veterans (OR = 0.09–0.69), except for veterans less than 25 years of age (OR = 2.22). |
| Tsai, 2014 (21) | Cross-sectional study | Administrative data from the VA's HCRV Program | 30,348 | 9,201 | Incarcerated veterans in state or federal prisons | 2007–2011 | Rate of lifetime homelessness among incarcerated veterans is 5 times the rate in the general population (30% vs. 6%). |
| Incarcerated veterans with homeless histories reported more mental health and substance abuse problems, especially drug abuse/dependence (OR = 1.55–1.984), more times arrested in their lifetime (OR = 1.01–1.02), and were more likely to be incarcerated for a nonviolent offense than other incarcerated veterans (OR = 1.44–1.60). |
Abbreviations: ACCESS, Access to Community Care and Effective Services and Supports; HCRV, Health Care for Reentry Veterans Program; HUD–VASH, Housing and Urban Development–Veterans Affairs Supportive Housing Program; NVVRS, National Vietnam Veterans Readjustment Study; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OR, odds ratio; PTSD, post-traumatic stress disorder; VA, Department of Veterans Affairs.
Consistent with 3 more rigorous studies suggesting that the effects of social isolation increased the risk for homelessness (28, 42, 43), 2 less rigorous studies also reported that weaker social support was associated with a longer duration of lifetime homelessness (46) and more chronic homelessness (51). A third less rigorous study reported that veterans themselves attributed weakened social connections to their increased risk for homelessness (47).
A strong association was found between incarceration and homelessness in veterans in one less rigorous study (21). Although the directionality of this relation is unclear, it is generally supportive of criminal history's being a risk factor for homelessness as reported in a more rigorous study (41).
Comparative studies of homeless veterans and homeless nonveterans
A total of 15 studies were identified that compared risk factors and characteristics of homeless veterans and homeless nonveterans. Collectively, these studies were based on data collected from 1983 to 2010, which include some of the earliest studies in this review (arranged by date of data in Table 3). Most of the studies were cross-sectional, except for 6 studies that had case-control design components (27, 39, 52–55) and 1 study that used observational longitudinal data (56).
Table 3.
Comparative Published Studies of Homeless Veterans and Other Homeless Adults, 1987–2013
| First Author, Year (Reference No.) | Design | Data Source | Location | Total No.a | No. of Veterans | Sampling Frame | Study Period | Findings |
|---|---|---|---|---|---|---|---|---|
| Robertson. 1987 (1)b |
Cross-sectional study | Surveys of shelter users | Los Angeles and Boston |
635 | 246 | Homeless male adults in Los Angeles and Boston |
1983–1985 | Veterans were older, better educated, more likely to be white, more likely to have married, and more likely to be receiving some type of government assistance than nonveterans. Veterans also had higher rates of psychiatric hospitalization and more physical health problems, and they were more likely to identify substance abuse as a reason for their homelessness, although they were less likely to be street drug users than nonveterans. |
| Roth, 1992 (58) |
Cross-sectional study | State-wide survey of homeless adults |
Ohio | 790 | 305 | Homeless male adults in Ohio |
1984 | Veterans were older, more likely to be white, better educated, more likely to have been married, to have been in jail, to have alcohol problems, and to use shelters than nonveterans. |
| Rosenheck, 1994 (52) |
Population-based case-control and cross-sectional study |
Urban Institute's 1987 national survey of homeless service users, 3 city surveys, and the 1987 Current Population Survey |
City-wide surveys were in Los Angeles, Baltimore, and Chicago |
2,223 | 916 | Homeless male adults |
1985–1987 | Veterans were at higher risk than nonveterans, especially striking among white men aged 20–34 years, post-Vietnam era or later (OR = 4.76). |
| Among white men and black men, homeless veterans were more educated and more likely to be married than their nonveteran counterparts. There was little difference in mental and substance use disorders, except in those aged 20–34 years in which white veterans had higher rates of mental and substance use disorders than nonveterans, and black veterans had higher rates of substance use disorders. | ||||||||
| Rosenheck, 1993 (60) |
Population-based cross-sectional study |
Urban Institute's 1987 national survey of homeless service users and 2 city surveys in 1986 |
City-wide surveys were in Los Angeles and Chicago |
1,991 | 793 | Homeless male adults |
1986–1987 | Veterans were older, more educated, more likely to have married, and more likely to be white than nonveterans. |
| No consistent difference in physical or mental health between veterans and nonveterans. | ||||||||
| Rosenheck, 1997 (39)c |
Population-based case-control study |
Four community homeless surveys and nationally conducted between 1986 and 1988, as well as the 1987 Current Population Survey |
Baltimore, Los Angeles, and Chicago |
2,223 | 915 | Homeless adults | 1986–1987 | Only veterans of the post-Vietnam generation (OR = 3.95) and in the generation between the Korea and Vietnam eras (OR = 1.75) had a greater risk than nonveterans in those age cohorts. |
| Winkleby, 1993 (59) |
Cross-sectional study | Survey of 3 National Guard armories offering free shelter to adults without children |
California | 1,008 | 423 | Single homeless shelter users in California |
1989–1990 | Veterans entered homelessness at later ages and were older, more highly educated, more likely to be separated/divorced, and less likely to be Hispanic than nonveterans. Veterans were also more likely to have physical and mental disorders and to report excessive alcohol use than nonveterans. |
| Tessler, 2002 (61) |
Cross-sectional study | ACCESS program evaluation |
9 states | 4,488 | 1,252 | Homeless male adults |
1994–1998 | Veterans were older (OR = 0.58), better educated (OR = 1.16), less likely to have married (OR = 0.49), more likely to be working for pay (OR = 1.02), more likely black (OR = 1.3), less likely to be Hispanic (OR = 0.53), and were homeless for longer (OR = 1.17) than nonveterans. |
| Veterans also reported fewer symptoms of conduct disorder in childhood (OR = 0.91) but were more likely to report alcohol abuse/dependence in adulthood (OR = 1.56). | ||||||||
| Gamache, 2003 (53) |
Population-based case-control study and cross-sectional study |
ACCESS program evaluation, NSHAPC, and the 1996 Current Population Survey |
9 states | 3,490 | 143 | Homeless women with mental illness |
1994–1998 | Female veterans were more likely to be homeless than female adults in the general population (OR = 3.58) and the low-income population (OR = 4.39). |
| Female veterans were less likely to report misconduct or family instability during childhood and were more educated, more likely to be married, and more likely recently employed than female nonveterans. | ||||||||
| Gamache, 2001 (27) |
Population-based case-control study |
NSHAPC and the 1996 Current Population Survey |
National | 1,841 | 602 | Homeless male adults |
1996 | White veterans and black veterans under the age of 55 years (post-Vietnam era or later) had a greater risk than nonveterans (OR = 1.01–3.95). |
| Tessler, 2003 (57) |
Cross-sectional study | NSHAPC | National | 1,691 | 570 | Homeless male adults who used homeless services |
1996 | Veterans less than 45 years of age (early years of the all-volunteer force) were more likely to be homeless for longer than 6 months than other adults (OR = 2.48), but veterans 45 years or older were less likely and had fewer risk factors. |
| Compared with other homeless adults less than 45 years of age, homeless veterans were less often white, less likely to have an employment history, more likely to be divorced/separated, more likely to have drug problems, and more likely to have used inpatient mental health services, but they had a higher level of education and were likely to have been in foster care. | ||||||||
| O'Toole, 2003 (62) |
Cross-sectional study | Survey in unsheltered enclaves, emergency shelters, and transitional housing or single-room occupancy dwellings |
Pittsburgh and Philadelphia |
425 | 127 | Homeless male adults in Pittsburgh and Philadelphia |
1997 | Veterans were significantly older, better educated, and more likely to have health insurance (including VA coverage) than nonveterans. |
| Veterans were more likely to report a chronic medical condition (66.1% vs. 55.4%), especially hepatitis or cirrhosis (18.9% vs. 7.0%) than nonveterans and to have more than 1 mental health condition (33.1% vs. 22.2%), especially post-traumatic stress disorder (18.1% vs. 8.1%). | ||||||||
| Tsai, 2012 (56) |
Observational longitudinal study |
Collaborative Initiative to Help End Chronic Homelessness Program evaluation |
9 states | 550 | 162 | Chronically homeless adults |
2004–2009 | Veterans were older, more likely to be in the Vietnam era age group, to be male, and to have a higher education than nonveterans. |
| There were no differences between veterans and nonveterans on housing or clinical outcomes over 1 year. | ||||||||
| Fargo, 2012 (55) |
Case-control study | HMIS and the American Community Survey |
National | 130,554 | 10,726 | Homeless adults in the community |
2008 | Veterans were at greater risk for homelessness compared with other homeless adults in the general population (RR = 1.3) and in the poverty population (RR = 2.1). For veterans and nonveterans, being black (OR = 2.18.45–5.49) and men aged between 45 and 54 years were at higher risk (OR = 1.85– 2.65). |
| HUD and VA, 2010 (54) |
Case-control study | Point-in-Time data from HUD and HMIS |
National | 1,257,927 | 144,842 | All sheltered homeless adults |
2010 | Veterans who were female, individuals (as opposed to families), from racial/ethnic minority groups, and aged 18– 30 years were at greater risk than nonveterans. |
| Montgomery, 2013 (65) |
Cross-sectional study | Washington State Behavioral Risk Factor Surveillance System |
Washington State |
2,313,988 | 293,707 | Veterans and other adults with any history of homelessness |
2010 | The association between adverse childhood experiences and adult homelessness was greater for nonveterans than veterans (OR = 1.67 vs. 1.42). |
Abbreviations: ACCESS, Access to Community Care and Effective Services and Supports; HMIS, Homeless Management Information System; HUD, Department of Housing and Urban Development; NSHAPC, National Survey of Homeless Assistance Providers and Clients; OR, odds ratio; RR, risk ratio; VA, Department of Veterans Affairs.
Total sample size of homeless adults (not including nonhomeless adults).
Surveys of Boston were conducted by Schutt in 1985 and 1986 (111, 112) but described by Robertson (1).
This book chapter was also cited in Table 1.
All of the case-control studies found a greater risk for homelessness among veterans compared with nonveterans, including other adults in the general population and specifically in low-income populations, although there were substantial differences between age strata representing different eras of military service (27, 52). These studies further found particular subgroups of veterans who were at particularly greater risk than nonveterans. Male post-Vietnam era veterans, that is, those who served in the early years of the all-volunteer force, appeared to be at particularly greater risk for homelessness than other male adults in the same age cohort, while veterans who served during World War II or the Korean War era were at lower risk for homelessness than nonveterans. As one study suggested (57), this may be due to a “social selection” effect. Many of the men who volunteered to serve in the military during this time may have been escaping poor economic conditions and lacked family support. Two other case-control studies, conducted on data collected over a decade apart, both found that female veterans were particularly at greater risk than other women (53, 54). These findings suggest the substantial risk for homelessness among female veterans regardless of service era, perhaps because they have never been subject to a military draft and thus have always been volunteers susceptible to social selection effects (53).
The remaining cross-sectional studies were focused mainly on comparing sociodemographic and health characteristics between homeless veterans and homeless nonveterans (1, 55, 57–62). Some consistent differences in sociodemographic characteristics were found as homeless veterans were older, better educated, and more likely to be male, to be or to have been married, and to have health coverage (often through the VA). However, there were some mixed findings about race differences, which may reflect when the data were collected and the era in which the veterans under study served. Several of the earlier studies found that homeless veterans were more likely to be white than were homeless nonveterans (1, 58, 60), but fewer race/ethnic differences were found in more recent studies as the veteran population has become more racially/ethnically diverse and some studies found the reverse to be true with homeless veterans more likely to be nonwhite (54, 55, 57, 61).
A high prevalence of physical, mental health, and substance abuse problems was found among both homeless veterans and homeless nonveterans, but there were inconsistent findings when they were compared. For example, 4 studies found that homeless veterans were more likely to have substance abuse problems (57–59, 61), but 4 other studies found little to no difference in mental health or substance abuse problems (52, 53, 56, 60). Additionally, 3 studies found that homeless veterans had more physical health problems than homeless nonveterans (59, 62, 63), which may partly reflect their greater age, while 2 other studies found no significant differences in physical health (60, 64). Studies that have found greater physical health problems among homeless veterans reported that they were more likely to report a physical injury or medical problem that contributed to their homelessness (59) and to have 2 or more chronic medical conditions, including hypertension, hepatitis/cirrhosis, diabetes, and heart disease (62).
Finally, 2 studies suggested that adverse childhood experiences are less of a risk factor for homelessness for veterans than for nonveterans. One study found that homeless veterans reported fewer conduct disorder behaviors in childhood than did homeless nonveterans (61), and another study found that the association between adverse childhood experiences and adult homelessness was attenuated in veterans (65).
DISCUSSION
This systematic review provides an examination of data on risk factors for veteran homelessness spanning over 2 decades. Several consistent risk factors were found across both more rigorous and less rigorous studies. Probably the strongest risk factors identified, other than the pervasive risk factor of extreme poverty that plagues virtually all homeless people, were substance use disorders and mental illness. In particular, psychotic disorders such as schizophrenia and alcohol and drug use disorders were found to be associated with homelessness. This is consistent with research on homelessness in the general population, where schizophrenia and bipolar disorder have been found to have the greatest impact on risk for homelessness at the individual level, and substance abuse has been found to have the greatest impact at the population level (31).
It is noteworthy that PTSD, which is more prevalent in the veteran population than the general population, was not a particularly important risk factor relative to other mental disorders. Similarly, combat exposure, at least among Vietnam era veterans, was not found to be associated with increased risk for homelessness, perhaps, in part, because such veterans are more likely to receive VA compensation, pension, and health benefits. OEF/OIF war-zone veterans were not at greater risk for homelessness when compared with veterans of other eras, but they were at greater risk compared with non-OEF/OIF theater veterans of the same era (i.e., military service after September 11, 2001). There may be various reasons for this. OEF/OIF veterans likely have higher overall rates of mental disorders and substance abuse problems compared with their non-OEF/OIF counterparts because of their exposure to war-zone stress (66, 67). OEF/OIF veterans are also more likely to experience traumatic brain injury and other neurological problems, which may be risk factors for homelessness as found in several studies reported in this review (37, 48). Some veterans have never been deployed or served in a war zone, whereas OEF/OIF war-zone veterans have all been separated from family and friends for some time. This may have led to deterioration in social support networks after military service, which is another risk factor for homelessness identified in several of the studies considered in this review (28, 46, 47). Some of these factors may have been less salient during the Vietnam War because of different methods of warfare, conscription, stigma, and screening of mental health problems at the time. It is also possible that rates of homelessness among Vietnam veterans were much higher in the years immediately following their return from overseas than they have been in recent decades when homelessness among veterans has been subject to more extensive research. Homelessness was virtually unstudied at that time so data on the Vietnam cohort in the years immediately following their war-zone service are not available.
As mentioned above, another robust risk factor was low income and income-related variables, such as military pay grade and unemployment. This finding was not surprising as homeless individuals, almost by definition, are impoverished and deprived of economic resources. Additionally, many studies of homeless adults in the general population have identified low income and unemployment as common antecedents of homelessness (31). For veterans, access to a VA service-connected disability payment was found to be a protective factor against homelessness, which suggests that it is one way to prevent homelessness. Besides the amount of income veterans receive, one study in this review reported that money mismanagement of income is also a risk factor (41).
In fact, researchers working in some non-VA programs have developed money management services to help homeless adults manage their money (68), and the popular Housing First model of supported housing generally encourages clients to participate in money management and/or to have representative payees to ensure that their rent is paid (69). Within the VA, researchers have developed interventions to teach veterans with addictive disorders money management skills and to offer them voluntary representative payees (70, 71), but these interventions have not yet been specifically tested or adapted for homeless veterans.
A third risk factor concerns a difficult construct to measure, which is deficient social support. Several studies indicated that lack of support from family and friends, weak social support networks, and social isolation are related to veteran homelessness. It is not clear whether veterans are particularly susceptible to this risk factor given the nature of military service (e.g., deployments and transfers, on-base housing), but the beneficial and protective effects of social support on stress, health, and overall functioning are well documented in the general population (72, 73), as well as in the veteran population (74, 75). Therefore, it is reasonable to theorize that the interruption of such support by military service can have deleterious effects and be associated with increased social isolation and, thus, homeless risk among veterans. However, further study with stronger research designs and comprehensive measures of social support is needed to determine the magnitude of this risk factor exactly.
Two other risk factors not commonly studied but appearing to be moderate risk factors—incarceration and adverse childhood experiences—deserve mention. Incarceration can lead to residential displacement, limited employment prospects, stigma, and disrupted personal relationships, which can ultimately increase risk for homelessness. It has been suggested that the general increase in homelessness in the United States during the 1980s was more related to mass incarceration secondary to the war on drugs than to deinstitutionalization of patients in state mental hospitals (76). Adverse childhood experiences and other premilitary factors may also set a pathway toward poverty and homelessness. Several studies have found that many homeless veterans report childhood behavioral problems, family instability, placement in foster care, and childhood trauma and abuse (28, 49, 65), and these early childhood problems have also been documented among the general, nonveteran homeless population as well (77, 78). More recently, a large survey study found that men with military experience since the advent of the all-volunteer force had a higher prevalence of a range of adverse childhood events than adults without such experience (79), consistent with our findings of greater risk for homelessness among veterans of the all-volunteer force. However, more rigorous studies are needed to conclusively label these premilitary factors as well as incarceration as independent risk factors for homelessness among veterans and to understand the mechanisms behind their association with homelessness.
Although race and gender were not found to be substantial risk factors for homelessness among veterans, it is important to recognize that many homeless veterans are demographically different from other homeless adults. Comparative studies with nonveterans have shown consistently that veterans were at greater risk for homelessness and that homeless veterans were more likely to be male, to be better educated, and to be or have been married than homeless nonveterans. Certain groups of veterans may be at particularly greater risk for homelessness compared with their nonveteran counterparts, including male veterans who served during the early years of the all-volunteer force in the later 1970s and female veterans.
In many ways, the major risk factors for homelessness identified for veterans are similar to those that have been identified for adults in the general population. However, this finding does not suggest that all the risk factors are the same, as we did find some unique risk factors for veterans. Comparative studies between homeless veterans and nonveterans pointed to additional questions that future studies should seek to answer. Our review highlights these gaps in the research literature, which we suggest as important areas for future research.
Recommendations for future research
First, more rigorously designed studies are needed. We could find no prospective cohort or experimental studies, which admittedly could be prohibitively expensive or infeasible. As homelessness is a relatively rare event, large sample sizes would be needed, and there would be ethical concerns with random assignment. However, more retrospective cohort studies as well as case-control studies could be conducted. Also lacking are studies that utilize structured diagnostic assessments and comprehensive measures of sociodemographic, health, and psychosocial characteristics. Most existing studies used self-report measures assessing a few select domains. Future studies using measures that have been psychometrically tested and validated on homeless populations and are objective and/or corroborated by other data are needed. We did not conduct a meta-analytical review of risk factors because of the variety of different measures, research designs, samples, and statistical analyses used across studies. For that reason, we also could not definitively comment on the relative magnitude of different risk factors compared with each other. It may be worthwhile for future studies to use more standard methodologies so that meta-analyses may be possible.
Second, more studies are needed on certain subgroups of veterans, such as female veterans and veteran families. Nearly all studies in this review predominantly or exclusively sampled the male veteran, and all focused on veterans as single adults (rather than families). However, the demographics of the veteran population are changing, as more female and racial/ethnically diverse veterans enlist (80, 81). Consequently, there is concern about the increasing number of homeless female veterans (54, 82), their rates of sexual trauma (83), and the welfare of their children and families (54, 82). Further research is needed on risk factors within these special subgroups.
Third, the pathways by which veterans become homeless and the specific role of military service in that process remain unclear. For example, one study found that mental illness diagnosed during the military predicted homelessness within 2 years after military discharge (37), while another study observed an average of 14 years between military discharge and the first episode of homelessness (47). Postdeployment social isolation and the possible disruptive effect of military service on relationships with family, friends, and other loved ones need to be studied in far more detail as they may be remedial features in pathways to veteran homelessness. Many veterans would not have become homeless if there were other people in their lives who could have offered emotional or instrumental support (e.g., money, place to stay).
Some studies have also gone beyond identifying specific risk factors to identifying constellations of factors or risk pro-files of homeless veterans (64). More detailed studies on the individual and synergistic effects of risk factors, mechanisms, and their time course are needed to elucidate these pathways to allow eventual development of a comprehensive model of the causes of veteran homelessness. With the exception of one model formulated 2 decades ago (28), there has not been much progress in developing comprehensive explanatory models for homelessness. Additionally, further work is needed to elucidate the interrelations between premilitary, military, and post-military factors to determine which ones are independent, addictive, or mitigative in increasing homeless risk.
A fourth area for future study is in understanding the differences in characteristics and risk factors between homeless veterans and homeless nonveterans. It appears that veterans of certain age cohorts appear to be at particularly greater risk for homelessness than nonveterans of the same age. Nonetheless, the paradox of certain cohorts of veterans being at greater risk despite being better off socioeconomically than nonveterans and being eligible for various health-care services and benefits through the VA needs to be further examined. Future research should address why veterans in some age cohorts differ or don't differ from nonveterans of similar age in their background and life experiences that may make them susceptible to homelessness, as this remains a question in the literature.
Finally, this review did not specifically identify risk factors that were modifiable or amenable to interventions, as there has been a paucity of research in this area. Future studies, however, should investigate which risk factors are most amenable to change and how to change them, information which will be important for ongoing prevention efforts. This review also focused on only individual risk factors, that is, micro-level factors, but did not examine system or institutional risk factors, that is, macro-level factors related to veteran homelessness. There may be factors, such as the dynamics of rental markets in areas with large populations of veterans, that put the veteran population or segments of the population at risk for homelessness beyond the effect of individual characteristics.
Implications for policy and practice
Policies and practices focused on assisting veterans to address the risk factors identified in this review should be supported. The VA's commitment to end veteran homelessness by 2015 depends on its ability not only to house veterans who are currently homeless but also to prevent veterans from becoming homeless in the future. Recent governmental reports have announced a decline in veteran homelessness (84), which may at least partly be due to the increased funding and development of VA homeless services. However, this apparent progress will likely need continued public attention and government support beyond 2015 to maintain reductions in veteran homelessness.
Homeless prevention efforts must be geared toward screening for the identified risk factors and ameliorating them, to the extent possible. The VA has recently implemented a 2-item homeless screening instrument at all facilities to identify veterans who are homeless or at risk of being homeless (85). This screener should be utilized to help target prevention interventions directly at those most vulnerable. Additionally, the Supportive Services for Veterans and Families (SSVF) Program was created in 2012 to prevent homelessness among veterans at imminent risk. The Supportive Services for Veterans and Families Program offers competitive grants to community-based organizations that can rapidly re-house homeless and at-risk veterans through time-limited case management, temporary financial assistance for moving expenses or rental fees, landlord mediation services, and other supportive services. Although not yet a well-defined program model, the Supportive Services for Veterans and Families Program holds promise in addressing many of the identified risk factors for veteran homelessness (86).
One main implication that can be drawn from our review is the crucial importance of connecting homeless and at-risk veterans with needed services and benefits. Access to mental health treatment, disability benefits, other income supports, and social services can help to prevent initial or subsequent episodes of homelessness. The VA, the largest integrated health-care network in the United States, offers an invaluable resource and a safety net for low-income and disabled veterans with multiple complex needs (25, 87). Outreach to homeless and at-risk veterans eligible for VA care should be encouraged. Both veterans who are eligible and ineligible for VA care may become eligible for various medical, mental health, and social services outside the VA system as well. As the Affordable Care Act is implemented, hundreds of thousands of low-income and homeless veterans will be eligible for Medicaid in states that implement the Medicaid expansion (88–91) and/or have new affordable coverage options through the state-based health insurance exchanges that will be required to cover mental health and substance abuse services on par with medical services (92, 93).
The findings of the review also support the use of supported housing as a direct response to homelessness. Permanent supported housing, which typically provides subsidized housing and case management services, has become one of the dominant service models for homeless adults, including veterans (94–97). Supported housing can help homeless veterans overcome their lack of income to pay for rent and provide linkages to mental health treatment that, as this review showed, are both factors strongly associated with homelessness. The VA's supported housing program, the Housing and Urban Development–Veterans Affairs Supportive Housing (HUD–VASH) Program, has been one of the centerpieces of the VA's plan to end homelessness among veterans (26). Although the HUD–VASH Program has been able to show substantial improvements in housing outcomes (94), less improvement has been observed in mental health, substance abuse, and quality-of-life outcomes. For example, some studies have found that many HUD–VASH clients continue to use substances after being housed (98, 99) and that there are few improvements in psychiatric symptoms (100). These findings are important to consider because these factors may lead to a return to homelessness, as one of the studies in this review found (44). The HUD–VASH Program has officially adopted the Housing First model, which provides immediate access to subsidized housing with no requirements for mental health or substance abuse treatment. The Housing First model has shown great success in housing high-needs populations outside the VA (101, 102), but it has not yet been formally evaluated in the HUD–VASH Program.
Similarly, there may also be a need for greater attention to the social and community integration of veterans after they obtain supported housing. Supported housing improves housing outcomes, but it seems to have little effect on social integration (103, 104). Thus, if homeless veterans are socially isolated before supported housing, as our review suggests, then they may remain lonely and isolated after obtaining housing, which may put them at risk for subsequent homelessness. Additional interventions may be needed. For example, elements of one service model called the Critical Time Intervention (105) may hold potential in helping homeless individuals engage in their communities and develop natural support systems. Peer support and other social support interventions (106–108) may also help homeless or formerly homeless veterans expand their social support networks and integrate into their communities.
Finally, this review provides some support for 2 VA homeless programs recently created to help justice-involved veterans, namely, the Health Care for Re-entry Veterans (HCRV) and the Veterans Justice Outreach (VJO) programs. The Health Care for Re-entry Veterans Program helps recently incarcerated veterans to re-enter the community (109), while the Veterans Justice Outreach Program diverts recently arrested veterans to treatment rather than incarceration (110). These programs, created under the umbrella of VA homeless services, address the link between incarceration and homelessness, as well as connecting at-risk veterans with mental health and social services. Thus, in essence, these programs demonstrate how risk factors for homelessness can be addressed through policy and practice.
Conclusions
Male and female veterans have been found to be at greater risk for homelessness than their nonveteran counterparts, although the disparity has declined over time and is most prominent among veterans of the all-volunteer force. Veterans appear to have many of the same major risk factors for homelessness as other adults, with the strongest and most consistent ones being substance abuse, severe mental illness, and low income. However, several risk factors unique to veterans have been identified in the literature, including problematic military discharges, low military pay grade, and social isolation after military discharge. Combat exposure and PTSD do not seem to playa distinctivelystrong role in veteran homelessness, perhaps because veterans have special access to VA services designed to meet their medical, mental health, and financial needs.
There have been few studies with strong research designs on this topic. No prospective cohort studies or experimental studies could be found, although several rigorous retrospective cohort and case-control studies have been conducted. Further study is needed to understand the exact pathways to veteran homelessness, including comprehensive models that consider premilitary, military, and postmilitary events and experiences. Special homeless veteran subgroups, such as women and families, also require additional comprehensive study. Veterans have been recognized as an especially deserving group throughout American history and have been provided with a unique health and social welfare safety net. The puzzle of why some of them, albeit a relatively small proportion, remain at risk for homelessness is a public health problem that needs to be better understood so veteran homelessness can eventually be ended.
ACKNOWLEDGMENTS
This work was supported by the Department of Veterans Affairs Health Services Research and Development Service (CDA 10-212).
Abbreviations
- HUD
Department of Housing and Urban Development
- OEF
Operation Enduring Freedom
- OIF
Operation Iraqi Freedom
- PTSD
post-traumatic stress disorder
- VA
Department of Veterans Affairs
- VASH
Veterans Affairs Supportive Housing
Footnotes
The views presented here are those of the authors alone and do not represent the position of any state or federal agency or of the US Government.
Conflict of interest: none declared.
REFERENCES
- 1.Robertson MJ. Homeless veterans: an emerging problem? In: Bingham RD, Green RE, White SB, editors. The Homeless in Contemporary Society. Sage Publications; Newbury Park, CA: 1987. pp. 64–81. [Google Scholar]
- 2.Lewin T. New York Times. Dec 30, 1987. Nation's homeless veterans battle a new foe: defeatism; p. A10. [Google Scholar]
- 3.Wright JD. The worthy and unworthy homeless. Society. 1988;25(5):64–69. [Google Scholar]
- 4.Rosenheck R, Leda C, Gallup P, et al. Initial assessment data from a 43-site program for homeless chronic mentally ill veterans. Hosp Community Psychiatry. 1989;40(9):937–942. doi: 10.1176/ps.40.9.937. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Housing and Urban Development . The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1, Point-in-Time Estimates of Homelessness. US Department of Housing and Urban Development; Washington, DC: 2013. [Google Scholar]
- 6.US Department of Veterans Affairs . Profile of veterans 2011. US Department of Veterans Affairs; Washington, DC: [Accessed January 28, 2014]. 2013. http://www.va.gov/VETDATA/docs/SpecialReports/Profile_of_Veterans_2011.pdf. [Google Scholar]
- 7.McKinney-Vento Homeless Assistance Act as amended by S.896 The Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act of 2009, 42 USC 11302 §103. 2009. [Google Scholar]
- 8.Springer S. Homelessness: a proposal for a global definition and classification. Habitat Int. 2000;24(4):475–484. [Google Scholar]
- 9.Toro PA. Toward an international understanding of homelessness. J Soc Issues. 2007;63(3):461–481. [Google Scholar]
- 10.Fazel S, Khosla V, Doll H, et al. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United Nations General Assembly [Accessed September 29, 2014];International Covenant on Economic, Social and Cultural Rights, article 11. Adopted by General Assembly resolution 2200A (XXI) of December 16, 1966. Entry into force. 1976 Jan 3; http://www.refworld.org/docid/3ae6b36c0.html.
- 12.United Nations General Assembly . Universal Declaration of Human Rights, article 25.1. United Nations; Paris, France: 1948. [Google Scholar]
- 13.Hwang SW. Homelessness and health. Can Med Assoc J. 2001;164(2):229–233. [PMC free article] [PubMed] [Google Scholar]
- 14.Schanzer B, Dominguez B, Shrout PE, et al. Homelessness, health status, and health care use. Am J Public Health. 2007;97(3):464–469. doi: 10.2105/AJPH.2005.076190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370–376. doi: 10.1176/appi.ajp.162.2.370. [DOI] [PubMed] [Google Scholar]
- 16.O'Connell JJ. Premature Mortality in Homeless Population: A Review of the Literature. National Health Care for the Homeless Council, Inc; Nashville, TN: 2005. [Google Scholar]
- 17.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304–309. doi: 10.1056/NEJM199408043310506. [DOI] [PubMed] [Google Scholar]
- 18.Salit SA, Kuhn EM, Hartz AJ, et al. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740. doi: 10.1056/NEJM199806113382406. [DOI] [PubMed] [Google Scholar]
- 19.Gladwell M. The New Yorker. Feb 13, 2006. Million-dollar Murray; p. 96. [Google Scholar]
- 20.McGuire J. Closing a front door to homelessness among veterans. J Prim Prev. 2007;28(3–4):389–400. doi: 10.1007/s10935-007-0091-y. [DOI] [PubMed] [Google Scholar]
- 21.Tsai J, Rosenheck RA, Kasprow WJ, et al. Homelessness in a national sample of incarcerated veterans in state and federal prisons. Adm Policy Ment Health. 2014;41(3):360–367. doi: 10.1007/s10488-013-0483-7. [DOI] [PubMed] [Google Scholar]
- 22.Rosenheck RA, Leda C, Frisman LK, et al. Homeless veterans. In: Baumohl J, editor. Homelessness in America. Oryx Press; Phoenix, AZ: 1996. pp. 97–108. [Google Scholar]
- 23.Perl L. Veterans and Homelessness. Congressional Research Service; Washington, DC: 2011. [Google Scholar]
- 24.Donovan S, Shinseki EK. Homelessness is a public health issue. Am J Public Health. 2013;103(suppl 2):S180. doi: 10.2105/AJPH.2013.301727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carrillo EV, Costello JJ, Yoon Ra C. Homelessness among veterans. In: Rubin A, Weiss EL, Coll JE, editors. Handbook of Military Social Work. John Wiley & Sons; Hoboken, NJ: 2012. pp. 247–269. [Google Scholar]
- 26.US Department of Veterans Affairs . Secretary Shinseki details plan to end homelessness for veterans. Office of Public and Intergovernmental Affairs; Washington, DC: 2009. [Google Scholar]
- 27.Gamache G, Rosenheck R, Tessler R. The proportion of veterans among homeless men: a decade later. Soc Psychiatry Psychiatr Epidemiol. 2001;36(10):481–485. doi: 10.1007/s001270170012. [DOI] [PubMed] [Google Scholar]
- 28.Rosenheck R, Fontana A. A model of homelessness among male veterans of the Vietnam War generation. Am J Psychiatry. 1994;151(3):421–427. doi: 10.1176/ajp.151.3.421. [DOI] [PubMed] [Google Scholar]
- 29.Gamache G, Rosenheck R, Tessler R. Military discharge status of homeless veterans with mental illness. Mil Med. 2000;165(11):803–808. [PubMed] [Google Scholar]
- 30.Hamilton AB, Poza I, Washington DL. “Homelessness and trauma go hand-in-hand”: pathways to homelessness among women veterans. Women's Health Issues. 2011;21(4):S203–S209. doi: 10.1016/j.whi.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Susser E, Moore R, Link B. Risk factors for homelessness. Epidemiol Rev. 1993;15(2):546–556. doi: 10.1093/oxfordjournals.epirev.a036133. [DOI] [PubMed] [Google Scholar]
- 32.Byrne T, Montgomery AE, Dichter ME. Homelessness among female veterans: a systematic review of the literature. Women Health. 2013;53(6):572–596. doi: 10.1080/03630242.2013.817504. [DOI] [PubMed] [Google Scholar]
- 33.Edidin JP, Ganim Z, Hunter SJ, et al. The mental and physical health of homeless youth: a literature review. Child Psychiatry Hum Dev. 2012;43(3):354–375. doi: 10.1007/s10578-011-0270-1. [DOI] [PubMed] [Google Scholar]
- 34.Balshem H, Christensen V, Tuepker A. A Critical Review of the Literature Regarding Homelessness Among Veterans. Department of Veterans Affairs; Washington, DC: 2011. [PubMed] [Google Scholar]
- 35.US Department of Housing and Urban Development Homeless emergency assistance and rapid transition to housing: defining “homeless.”. Fed Regist. 2011;76(233):75994–76019. [Google Scholar]
- 36.US Department of Veterans Affairs . Homeless Incidence and Risk Factors for Becoming Homeless in Veterans. Office of Inspector General; Washington, DC: 2012. GPO no. 11-03428-173. [Google Scholar]
- 37.Metraux S, Clegg LX, Daigh JD, et al. Risk factors for becoming homeless among a cohort of veterans who served in the era of the Iraq and Afghanistan conflicts. Am J Public Health. 2013;103(suppl 2):S255–S261. doi: 10.2105/AJPH.2013.301432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 39.Rosenheck RA, Frisman L, Fontana A, et al. Combat exposure and posttraumatic stress disorder among homeless veterans of three wars. In: Ursano RJ, Fullerton CS, editors. Posttraumatic Stress Disorder: Acute and Long-term Responses to Trauma and Disaster. American Psychiatric Press, Inc; Washington, DC: 1997. pp. 191–207. [Google Scholar]
- 40.Bullock HE, Harlow LL, Mulaik SA. Causation issues in structural equation modeling research. Struct Equ Modeling. 1994;1(3):253–267. [Google Scholar]
- 41.Elbogen EB, Sullivan CP, Wolfe J, et al. Homelessness and money mismanagement in Iraq and Afghanistan veterans. Am J Public Health. 2013;103(suppl 2):S248–S254. doi: 10.2105/AJPH.2013.301335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Blackstock OJ, Haskell SG, Brandt CA, et al. Gender and the use of Veterans Health Administration homeless services programs among Iraq/Afghanistan veterans. Med Care. 2012;50(4):347–352. doi: 10.1097/MLR.0b013e318245a738. [DOI] [PubMed] [Google Scholar]
- 43.Washington DL, Yano EM, McGuire J, et al. Risk factors for homelessness among women veterans. J Health Care Poor Underserved. 2010;21(1):81–91. doi: 10.1353/hpu.0.0237. [DOI] [PubMed] [Google Scholar]
- 44.O'Connell MJ, Kasprow W, Rosenheck RA. Rates and risk factors for homelessness after successful housing in a sample of formerly homeless veterans. Psychiatr Serv. 2008;59(3):268–275. doi: 10.1176/ps.2008.59.3.268. [DOI] [PubMed] [Google Scholar]
- 45.Edens EL, Kasprow W, Tsai J, et al. Association of substance use and VA service-connected disability benefits with risk of homelessness among veterans. Am J Addict. 2011;20(5):412–419. doi: 10.1111/j.1521-0391.2011.00166.x. [DOI] [PubMed] [Google Scholar]
- 46.Wenzel SL, Gelberg L, Bakhtiar L, et al. Indicators of chronic homelessness among veterans. Hosp Community Psychiatry. 1993;44(12):1172–1176. doi: 10.1176/ps.44.12.1172. [DOI] [PubMed] [Google Scholar]
- 47.Mares AS, Rosenheck RA. Perceived relationship between military service and homelessness among homeless veterans with mental illness. J Nerv Ment Dis. 2004;192(10):715–719. doi: 10.1097/01.nmd.0000142022.08830.f4. [DOI] [PubMed] [Google Scholar]
- 48.Douyon R, Guzman P, Romain G, et al. Subtle neurological deficits and psychopathological findings in substance-abusing homeless and non-homeless veterans. J Neuropsychiatry Clin Neurosci. 1998;10(2):210–215. doi: 10.1176/jnp.10.2.210. [DOI] [PubMed] [Google Scholar]
- 49.Tsai J, Rosenheck RA. Conduct disorder behaviors, childhood family instability, and childhood abuse as predictors of severity of adult homelessness among American veterans. Soc Psychiatry Psychiatr Epidemiol. 2013;48(3):477–486. doi: 10.1007/s00127-012-0551-4. [DOI] [PubMed] [Google Scholar]
- 50.Kasprow WJ, Rosenheck RA. Beyond words: homeless veterans who served in Iraq and Afghanistan. In: Kelly D, Howe-Barksdale S, Gitelson D, editors. Treating Young Veterans: Promoting Resilience Through Practice and Advocacy. Springer Publishing Company; New York, NY: 2011. pp. 125–134. [Google Scholar]
- 51.van den Berk-Clark C, McGuire J. Elderly homeless veterans in Los Angeles: chronicity and precipitants of homelessness. Am J Public Health. 2013;103(suppl 2):S232–S238. doi: 10.2105/AJPH.2013.301309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosenheck R, Frisman L, Chung AM. The proportion of veterans among homeless men. Am J Public Health. 1994;84(3):466–469. doi: 10.2105/ajph.84.3.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gamache G, Rosenheck R, Tessler R. Overrepresentation of women veterans among homeless women. Am J Public Health. 2003;93(7):1132–1136. doi: 10.2105/ajph.93.7.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.US Department of Housing and Urban Development. US Department of Veterans Affairs . Veteran Homelessness: A Supplemental Report to the 2009 Annual Homeless Assessment Report to Congress. US Department of Housing and Urban Development and the US Department of Veterans Affairs; Washington, DC: 2010. [Google Scholar]
- 55.Fargo J, Metraux S, Byrne T, et al. Prevalence and risk of homelessness among US veterans. Prev Chronic Dis. 2012;9:E45. [PMC free article] [PubMed] [Google Scholar]
- 56.Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27–31. doi: 10.7205/milmed-d-11-00128. [DOI] [PubMed] [Google Scholar]
- 57.Tessler R, Rosenheck R, Gamanche G. Homeless veterans of the mil-volunteer force: a social selection perspective. Armed Forces Soc. 2003;29(4):509–524. [Google Scholar]
- 58.Roth D. Homeless veterans: comparisons with other homeless men. In: Robertson MJ, Greenblatt M, editors. Homelessness: A National Perspective. Springer Science+ Business Media New York; New York, NY: 1992. pp. 213–219. [Google Scholar]
- 59.Winkleby MA, Fleshin D. Physical, addictive, and psychiatric disorders among homeless veterans and nonveterans. Public Health Rep. 1993;108(1):30–36. [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenheck R, Koegel P. Characteristics of veterans and nonveterans in three samples of homeless men. Hosp Community Psychiatry. 1993;44(9):858–863. doi: 10.1176/ps.44.9.858. [DOI] [PubMed] [Google Scholar]
- 61.Tessler R, Rosenheck R, Gamache G. Comparison of homeless veterans with other homeless men in a large clinical outreach program. Psychiatr Q. 2002;73(2):109–119. doi: 10.1023/a:1015051610515. [DOI] [PubMed] [Google Scholar]
- 62.O'Toole TP, Conde-Martel A, Gibbon JL, et al. Health care of homeless veterans: why are some individuals falling through the safety net? J Gen Intern Med. 2003;18(11):929–933. doi: 10.1046/j.1525-1497.2003.21209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Robertson MJ, Zlotnick C. Homeless adults: a special population in public alcohol treatment programs. Contemp Drug Probl. 1993;20(3):499–520. [Google Scholar]
- 64.Tsai J, Kasprow WJ, Rosenheck RA. Latent homeless risk profiles of a national sample of homeless veterans and their relation to program referral and admission patterns. Am J Public Health. 2013;103(suppl 2):S239–S247. doi: 10.2105/AJPH.2013.301322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Montgomery AE, Cutuli JJ, Evans-Chase M, et al. Relationship among adverse childhood experiences, history of active military service, and adult outcomes: homelessness, mental health, and physical health. Am J Public Health. 2013;103(suppl 2):S262–S268. doi: 10.2105/AJPH.2013.301474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 67.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq and Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 68.Stoner MR. Money management services for the homeless mentally ill. Hosp Community Psychiatry. 1989;40(7):751–753. doi: 10.1176/ps.40.7.751. [DOI] [PubMed] [Google Scholar]
- 69.Tsemberis S, Eisenberg RF. Pathways to housing: supported housing for street-dwelling homeless individuals with psychiatric disabilities. Psychiatr Serv. 2000;51(4):487–493. doi: 10.1176/appi.ps.51.4.487. [DOI] [PubMed] [Google Scholar]
- 70.Rosen MI, Carroll KM, Stefanovics E, et al. A randomized controlled trial of a money management-based substance use intervention. Psychiatr Serv. 2009;60(4):498–504. doi: 10.1176/appi.ps.60.4.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rosen MI, Bailey M, Rosenheck RR. Alcohol & drug abuse: principles of money management as a therapy for addiction. Psychiatr Serv. 2003;54(2):171–173. doi: 10.1176/appi.ps.54.2.171. [DOI] [PubMed] [Google Scholar]
- 72.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 73.Uchino BN. Social Support and Physical Health: Understanding the Health Consequences of Relationships. Yale University Press; New Haven, CT: 2004. [Google Scholar]
- 74.Tsai J, Harpaz-Rotem I, Pietrzak RH, et al. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry. 2012;75(2):133–149. doi: 10.1521/psyc.2012.75.2.135. [DOI] [PubMed] [Google Scholar]
- 75.Pietrzak RH, Johnson DC, Goldstein MB, et al. Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: the role of resilience, unit support, and postdeployment social support. J Affect Disord. 2010;120(1–3):188–192. doi: 10.1016/j.jad.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 76.O'Flaherty B. Making Room: The Economics of Homelessness. Harvard University Press; Cambridge, MA: 1998. [Google Scholar]
- 77.Koegel P, Melamid E, Burnam MA. Childhood risk factors for homelessness among homeless adults. Am J Public Health. 1995;85(12):1642–1649. doi: 10.2105/ajph.85.12.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roos LE, Mota N, Afifi TO, et al. Relationship between adverse childhood experiences and homelessness and the impact of axis I and II disorders. Am J Public Health. 2013;103(suppl 2):S275–S281. doi: 10.2105/AJPH.2013.301323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Blosnich JR, Dichter ME, Cerulli C, et al. Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry. 2014;71(9):1041–1048. doi: 10.1001/jamapsychiatry.2014.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Goldzweig CL, Balekian TM, Rolón C, et al. The state of women veterans' health research. Results of a systematic literature review. J Gen Intern Med. 2006;21(suppl 3):S82–S92. doi: 10.1111/j.1525-1497.2006.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.National Center for Veterans Analysis and Statistics . Veteran population projections: FY2010 to FY2040. US Department of Veterans Affairs; Washington, DC: [Accessed February 15, 2014]. 2013. http://www.va.gov/VETDATA/docs/Quickfacts/Population_slideshow.pdf. [Google Scholar]
- 82.Tsai J, Kasprow WJ, Kane V, et al. National comparison of literally homeless male and female VA service users: entry characteristics, clinical needs, and service patterns. Women's Health Issues. 2014;24(1):e29–e35. doi: 10.1016/j.whi.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 83.Tsai J, Rosenheck RA, Decker SE, et al. Trauma experience among homeless female veterans: correlates and impact on housing, clinical, and psychosocial outcomes. J Trauma Stress. 2012;25(6):624–632. doi: 10.1002/jts.21750. [DOI] [PubMed] [Google Scholar]
- 84.US Department of Veterans Affairs . VA and HUD announce twenty-four percent reduction in veterans' homelessness since 2010. US Department of Veterans Affairs; Washington, DC: [Accessed July 6, 2014]. 2013. http://www.va.gov/opa/pressrel/pressrelease.cfm? id=2499. [Google Scholar]
- 85.Montgomery AE, Fargo JD, Byrne TH, et al. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210–S211. doi: 10.2105/AJPH.2013.301398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.US Department of Veterans Affairs . Supportive Services for Veteran Families (SSVF) FY 2013 Annual Report. US Department of Veterans Affairs; Washington, DC: 2014. [Google Scholar]
- 87.Wilson NJ, Kizer KW. The VA health care system: an unrecognized national safety net. Health Aff (Millwood) 1997;16(4):200–204. doi: 10.1377/hlthaff.16.4.200. [DOI] [PubMed] [Google Scholar]
- 88.Tsai J, Rosenheck RA. Homeless and nonhomeless VA service users likely eligible for Medicaid expansion. J Rehabil Res Dev. 2014;51(5):675–684. doi: 10.1682/JRRD.2013.10.0225. [DOI] [PubMed] [Google Scholar]
- 89.Tsai J, Rosenheck R. Uninsured veterans who will need to obtain insurance coverage under the patient protection and affordable care act. Am J Public Health. 2014;104(3):e57–e62. doi: 10.2105/AJPH.2013.301791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tsai J, Kasprow WJ, Culhane D, et al. Homeless veterans who will become eligible for Medicaid under the Affordable Care Act. Psychiatr Serv. doi: 10.1176/appi.ps.201500377. In press. [DOI] [PubMed] [Google Scholar]
- 91.Haley JM, Kenney GM. Uninsured Veterans and Family Members: State and National Estimates of Expanded Medicaid Eligibility Under the ACA. Urban Institute; Washington, DC: 2013. [Google Scholar]
- 92.Tsai J, Pilver C, Hoff RA. Potential mental health needs of U.S. residents under different provisions of the Affordable Care Act. J Clin Psychiatry. doi: 10.4088/JCP.13m08885. In press. [DOI] [PubMed] [Google Scholar]
- 93.Beronio K, Po R, Skopec L, et al. Affordable Care Act Expands Mental Health and Substance Use Disorder Benefits and Federal Parity Protections for 62 Million Americans. US Department of Health and Human Services; Washington, DC: 2013. [Google Scholar]
- 94.Rosenheck R, Kasprow W, Frisman L, et al. Cost-effectiveness of supported housing for homeless persons with mental illness. Arch Gen Psychiatry. 2003;60(9):940–951. doi: 10.1001/archpsyc.60.9.940. [DOI] [PubMed] [Google Scholar]
- 95.Rog DJ. The evidence on supported housing. Psychiatr Rehabil J. 2004;27(4):334–344. doi: 10.2975/27.2004.334.344. [DOI] [PubMed] [Google Scholar]
- 96.Ridgway P, Zipple AM. The paradigm shift in residential services: from the linear continuum to supported housing approaches. Psychosoc Rehabil J. 1990;13(4):20–31. [Google Scholar]
- 97.O'Connell M, Kasprow W, Rosenheck RA. National dissemination of supported housing in the VA: model adherence versus model modification. Psychiatr Rehabil J. 2010;33(4):308–319. doi: 10.2975/33.4.2010.308.319. [DOI] [PubMed] [Google Scholar]
- 98.Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455–460. doi: 10.1016/j.addbeh.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 99.Westermeyer J, Lee K. Residential placement for veterans with addiction: American Society of Addiction Medicine criteria vs. a veterans homeless program. J Nerv Ment Dis. 2013;201(7):567–571. doi: 10.1097/NMD.0b013e3182982d1a. [DOI] [PubMed] [Google Scholar]
- 100.Cheng AL, Lin H, Kasprow W, et al. Impact of supported housing on clinical outcomes: analysis of a randomized trial using multiple imputation technique. J Nerv Ment Dis. 2007;195(1):83–88. doi: 10.1097/01.nmd.0000252313.49043.f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tsemberis S. From streets to homes: an innovative approach to supported housing for homeless adults with psychiatric disabilities. J Community Psychol. 1999;27(2):225–241. [Google Scholar]
- 102.Tsemberis S, Kent D, Respress C. Housing stability and recovery among chronically homeless persons with co-occuring disorders in Washington, DC. Am J Public Health. 2012;102(1):13–16. doi: 10.2105/AJPH.2011.300320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tsai J, Mares AS, Rosenheck RA. Does housing chronically homeless adults lead to social integration? Psychiatr Serv. 2012;63(5):427–434. doi: 10.1176/appi.ps.201100047. [DOI] [PubMed] [Google Scholar]
- 104.Yanos PT, Stefancic A, Tsemberis S. Objective community integration of mental health consumers living in supported housing and of others in the community. Psychiatr Serv. 2012;63(5):438–444. doi: 10.1176/appi.ps.201100397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Herman D, Conover S, Felix A, et al. Critical time intervention: an empirically supported model for preventing homelessness in high risk groups. J Prim Prev. 2007;28(3–4):295–312. doi: 10.1007/s10935-007-0099-3. [DOI] [PubMed] [Google Scholar]
- 106.Tsai J, Rosenheck RA. Outcomes of a group intensive peer-support model of case management for supported housing. Psychiatr Serv. 2012;63(12):1186–1194. doi: 10.1176/appi.ps.201200100. [DOI] [PubMed] [Google Scholar]
- 107.Fisk D, Frey J. Employing people with psychiatric disabilities to engage homeless individuals through supported socialization: the Buddies Project. Psychiatr Rehabil J. 2002;26(2):191–196. doi: 10.2975/26.2002.191.196. [DOI] [PubMed] [Google Scholar]
- 108.Hogan BE, Linden W, Najarian B. Social support interventions: do they work? Clin Psychol Rev. 2002;22(3):381–440. doi: 10.1016/s0272-7358(01)00102-7. [DOI] [PubMed] [Google Scholar]
- 109.Tsai J, Rosenheck RA, Kasprow WJ, et al. Risk of incarceration and other characteristics of Iraq and Afghanistan era veterans in state and federal prisons. Psychiatr Serv. 2013;64(1):36–43. doi: 10.1176/appi.ps.201200188. [DOI] [PubMed] [Google Scholar]
- 110.Blue-Howells JH, Clark SC, van den Berk-Clark C, et al. The U.S. Department of Veterans Affairs Veterans Justice Programs and the sequential intercept model: case examples in national dissemination of intervention for justice-involved veterans. Psychol Serv. 2013;10(1):48–53. doi: 10.1037/a0029652. [DOI] [PubMed] [Google Scholar]
- 111.Schutt RK. Boston's Homeless: Their Backgrounds, Problems, and Needs. University of Massachusetts; Boston, MA: 1985. [Google Scholar]
- 112.Schutt RK. A Short Report on Homeless Veterans: A Supplement to Homeless in Boston in 1985. University of Massachusetts; Boston, MA: 1986. [Google Scholar]