Diabetes affects 22.3 million people in the United States.1 It is a major cause of heart disease and stroke and is the seventh leading cause of death.2 Patients with diabetes are at two to four times greater risk of myocardial infarction (MI) than those without diabetes, and diabetes is the primary reason for renal failure, blindness, and nontraumatic limb amputations.3 Preventive care practices can reduce the development of severe vision loss by 50–60%, reduce foot amputations by 45–85%, and lower blood pressure to reduce proteinuria, a risk factor for developing kidney disease, by ∼ 35%.2 Despite evidence that complications related to diabetes are preventable,4,5 only 52% of individuals with diabetes meet guidelines targeting an A1C of < 7.0%, and only 18% meet combined glycemic, lipid, and blood pressure goals.6
In addition to significant morbidity, diabetes has a substantial financial impact. Medical expenses for people with diabetes are more than two times higher than for those without diabetes.2 Total national health care and related costs for the treatment of all people with diabetes total ∼ $245 billion.1 Complications from diabetes, such as chronic kidney disease, can cost health care organizations $33 billion per year.2 Most diabetes care is provided in the community in the primary care setting,3 and diabetes is the fourth most frequent reason for ambulatory physician visits.7 A gap exists between optimal and actual care, constituting a wide “quality chasm,”8 which underscores the need for innovative approaches to change the current practice of diabetes care. Clinical decision support systems (CDSSs) have been suggested as a viable solution to these pressing issues.9
Clinical Decision Support Systems
CDSSs have been defined as systems providing an automated process for comparing patient-specific characteristics against a computerized knowledge base, with resulting recommendations or reminders presented to providers at the time of clinical decision making.10 Studies have used CDSSs in diabetes management for a variety of purposes, including glycemic control,4,7,11,12 behavioral/attitude changes,4,7,13,14 combined management goals of cardiovascular risk reduction and glycemic control,3,8,9,15–18 and cost-effectiveness.19–22 CDSSs have been shown to improve processes of diabetes care3,4,8,11,14,16,17 and management outcomes.3,7,9,10–12,18
Although CDSSs in diabetes care may improve care processes and delay diabetes complications, most studies in this field do not include cost-effectiveness analyses. Cleveringa et al.19 found that patients in CDSS intervention groups showed slightly more quality-adjusted life years, but with increased total costs incurred for their care, leading to a high cost-effectiveness ratio when compared to control groups. Although cost savings exist, current results suggest that they are modest.19–22
Unless a strategic plan is in place, organizational and health care delivery problems may contribute to the inability to reach current evidence-based goals for optimal chronic disease control.23,24 CDSSs within ambulatory/primary care practices are at the forefront of effective standards-based care within the diabetes population.10 However, more work needs to be performed to determine the effectiveness and sustainability of CDSSs in practice.
Local Problem
Challenges exist to improve quality across the continuum of diabetes-related care. To address these challenges, the American Board of Medical Specialties launched the Improving Performance in Practice (IPIP) initiative in 2005.25 The goal of IPIP is to improve the quality of care in all primary care practices across states. North Carolina was chosen as one of the pilot states to focus on diabetes and asthma. To drive the initiative, collaboration was formed between the N.C. Area Health Education Center and Community Care of North Carolina. This collaborative defined common quality measures tied to national diabetes measures and used a CDSS (Reach My Doctor) to allow rapid-cycle quality techniques to be used.25
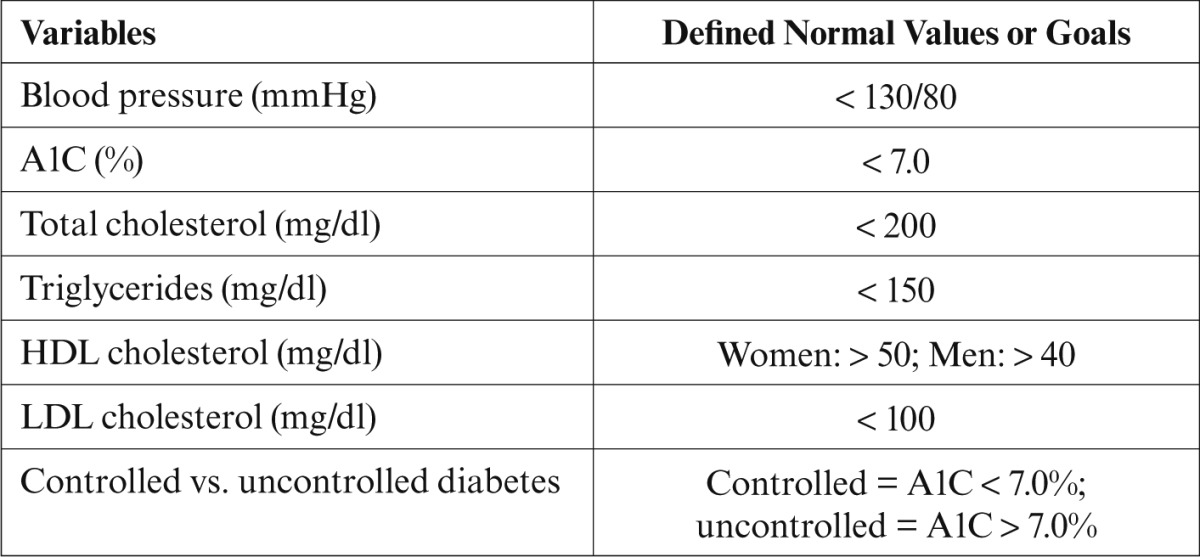
Rapid-cycle improvement is a quality improvement (QI) method that identifies, implements, and measures changes made to improve a process or a system.25 Rapid-cycle improvement implies that changes are made and tested over periods of ≤ 3 months rather than the standard 8–12 months. One commonly used rapid-cycle improvement strategy is the Plan-Do-Study-Act cycle.25 Table 1 summarizes the American Diabetes Association (ADA) treatment recommendations that were used within the CDSS for glycemic, blood pressure, and lipid control for most adults with diabetes.26
Table 1.
Summary of ADA-Recommended Treatment Goals for Most Adults With Diabetes26
The ambulatory care division of New Hanover Regional Medical Center (NHRMC), located in Wilmington, N.C., provides evidence-based primary care to its population of patients with diabetes. However, the NHRMC HIV/Primary Care Clinic identified gaps between the actual care it provided and the optimal care of its patients. Specifically, HIV patient admissions had a higher rate of endocrine disorders than the general NHRMC inpatient population (6.16 vs. 3.28%). Another gap identified was a lack of an effective registry for identifying and evaluating diabetes-related outcome measures. To address these gaps and align the HIV/Primary Care Clinic to NHRMC’s strategic goal of accountable quality care, the clinic joined the IPIP initiative using a CDSS to improve the quality of care provided to its population of patients with diabetes. Other practices participated; however, no evaluation had been made of the CDSS’s impact on the ambulatory care division’s population of patients with diabetes.
Hence, the purpose of this QI project was to evaluate the impact of the CDSS in an ambulatory care setting on outcome measures and the costs of diabetes-related care. To evaluate the alignment of care with NHRMC’s strategic goals, the question asked was, “Does using a CDSS improve ADA outcome measures within the ambulatory care setting?”
Study Methods
This was a retrospective review providing an evaluation arm to assess the effectiveness and costs of a CDSS within NHRMC’s ambulatory care setting. Three practices were evaluated: Coastal Family Medicine Practice, Internal Medicine Practice, and the HIV/Primary Care Clinic. Inclusion criteria included 1) a diagnosis of type 1 or type 2 diabetes, 2) a history of being treated for diabetes within the three ambulatory care practices, and 3) inclusion in the IPIP CDSS database at defined time points.
Ethical Issues
This QI project was approved by the institutional review boards at NHRMC and Duke University in Durham, N.C.
Study Design
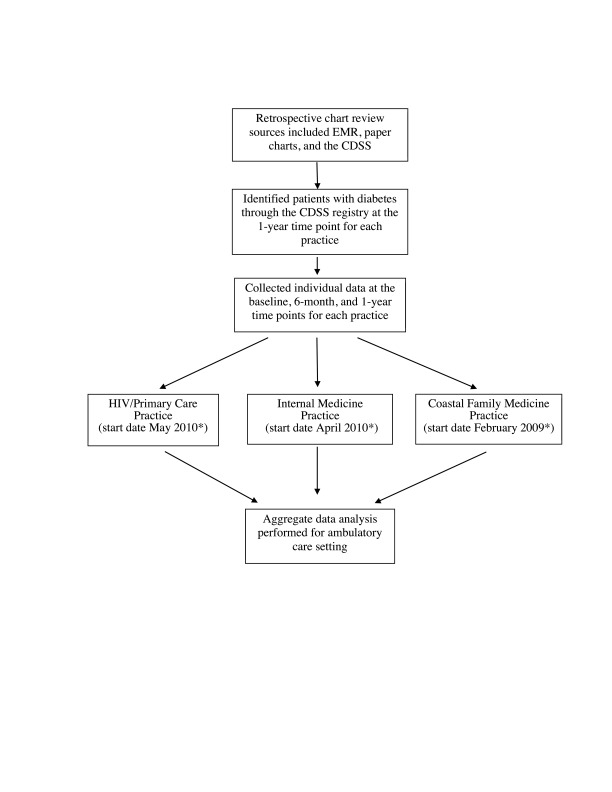
The QI project consisted of a workflow process to evaluate the CDSS’s impact on identified ADA measures (Figure 1). These measures included 1) BMI, 2) systolic and diastolic blood pressure, 3) A1C, 4) lipid levels (total cholesterol, triglycerides, HDL cholesterol, and LDL cholesterol), 5) estimated glomerular filtration rate (GFR), and 6) controlled versus uncontrolled diabetes (controlled = A1C < 7.0%; uncontrolled = A1C > 7.0%).
Figure 1.
Workflow for evaluation arm. *Start date indicates the date the practice started using the CDSS. EMR, electronic medical record.
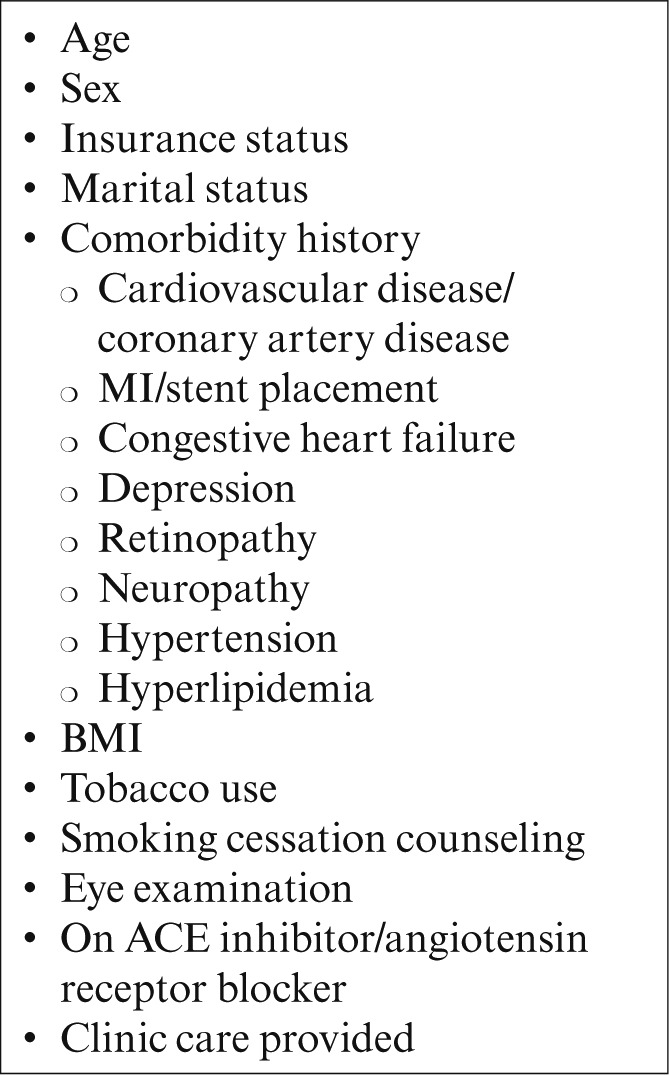
The method of evaluation included a three-step process to collect descriptive and outcome measures for selected variables. This process included 1) collection of individual patient information on identified ADA measures at baseline, 6 months, and 1 year; 2) collection of individual descriptive measures (Table 2); and 3) aggregate analysis of the three practice’s descriptive and outcome measures at baseline, 6 months, and 1 year of CDSS implementation.
Table 2.
Descriptive Measures
Data Analysis
Data were reported as mean ± standard deviation (SD) or frequencies. Variables were compared at baseline, 6-month, and 1-year time intervals with a repeated-measures, mixed-effects model and using proportions for categorical variables. Comparison of categorical variables before and after implementation was completed with McNemar’s test. Data were analyzed using SAS 9.1 (SAS Institute, Cary, N.C.), and all tests were two-tailed. P values < 0.05 were considered significant.
Study Results
Data were collected on 664 patients from three practices within NHRMC’s ambulatory care division, with the majority (67.6%) coming from the Internal Medicine Practice. Twenty-five percent of the population came from Coastal Family Medicine, and 7.4% came from the HIV/Primary Care Clinic. At baseline, the study population was comparable to published national averages for A1C, LDL cholesterol, and blood pressure control from the 2009–2010 National Health and Nutritional Examination Survey.27
Patient Characteristics
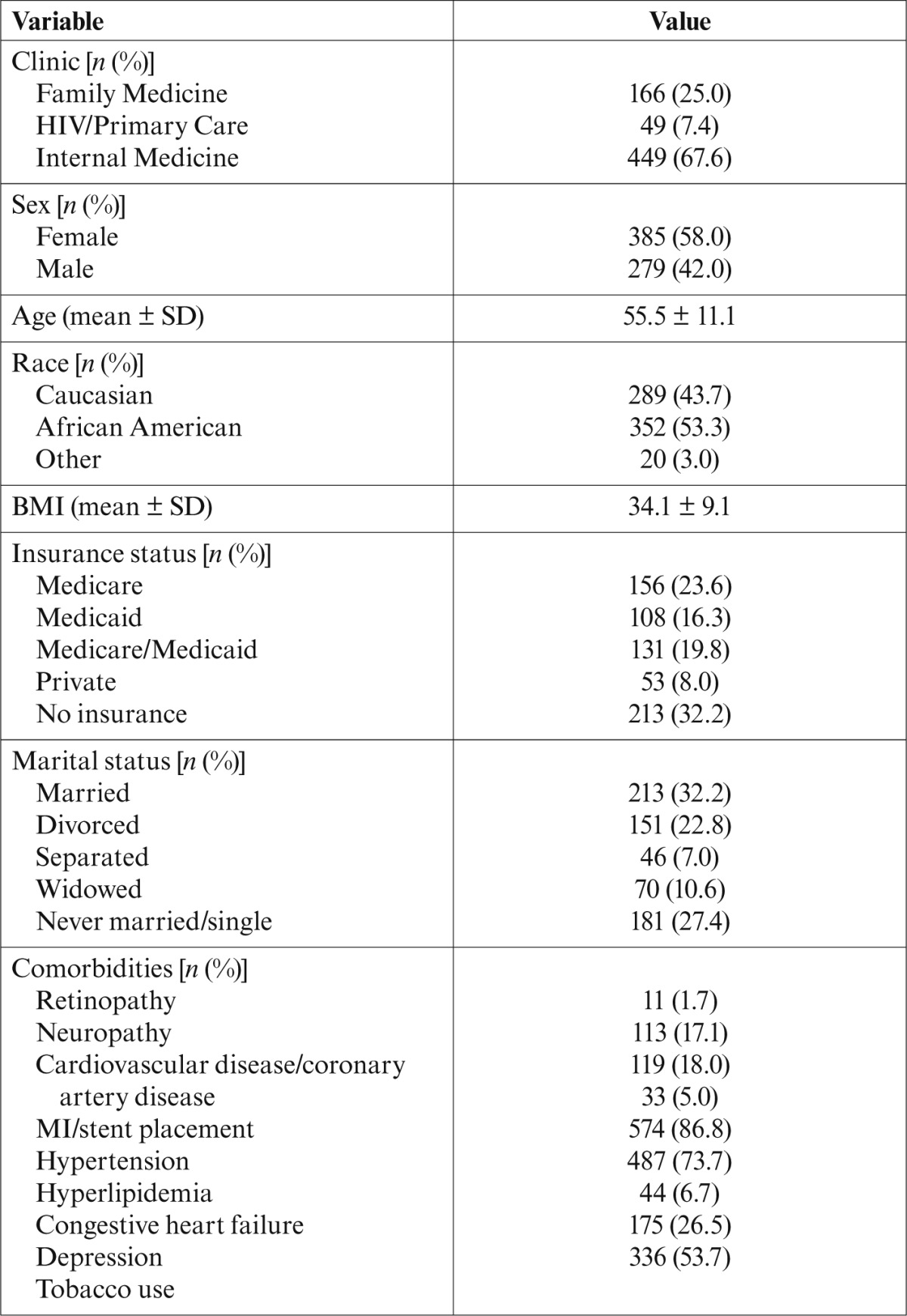
Patient characteristics are summarized in Table 3. Slightly more than half of the patients were female (57.7%) and African American (53.3%). The average age was 55.5 ± 11 years, with a mean BMI of 34.1 ± 9.1 kg/m2. Baseline BMI fell within the World Health Organization (WHO) obese class I.28 The majority of patients were married (32.2%) and uninsured (32.2%), and only 8.0% had private insurance. The most common comorbidities reported were hypertension (86.8%) and hyperlipidemia (73.68%). Tobacco use was reported in 53.7% of the patient population.
Table 3.
Patient Characteristics
Measured Variables
Table 4 compares selected variables to the 2013 ADA management guidelines. Patients’ clinical characteristics did not differ significantly from before implementation to 1 year after implementation, although there was a nonsignificant reduction of 2 percentage points in those with an estimated GFR ≤ 60 ml/min/m2 (14.1 to 12.7%, P = 0.4748) after 1 year (Table 5). There were also no significant differences in measurements taken at 6 months, although there was a nonsignificant 20-mg/dl reduction in triglycerides (178.8 ± 233.1 to 159.7 ± 178.9 mg/dl, P = 0.4472). Smoking cessation counseling was performed for 100% of the patient population. Eighty-eight percent (87.9%) of the population were taking either ACE inhibitors or angiotensin receptor blockers, and 81.5% of the population received a retinal screening, which exceeds the Agency for Healthcare Research and Quality (AHRQ) national average of 66.7%.29 WHO considers individuals to be at normal weight with a BMI of < 25 kg/m2.28 Unfortunately, less than one-fourth (23.1%) of the patient population met this goal. However, 94.3% of patients received at least one A1C measurement in the course of 1 year (AHRQ’s national average is 79.4%), and 70% of the population had an A1C measured at least twice in 1 year, again exceeding AHRQ’s national average of 61.1%. There was a significant difference in guideline adherence to the HDL cholesterol recommendation in women 6 months after implementation compared to before and 1 year after implementation (P = 0.0022). Combined A1C, LDL cholesterol, and blood pressure targets were achieved in 24.4% at baseline, 33.6% at 6 months, and 26.7% at 1 year after CDSS implementation.
Table 4.
Clinical Guidelines
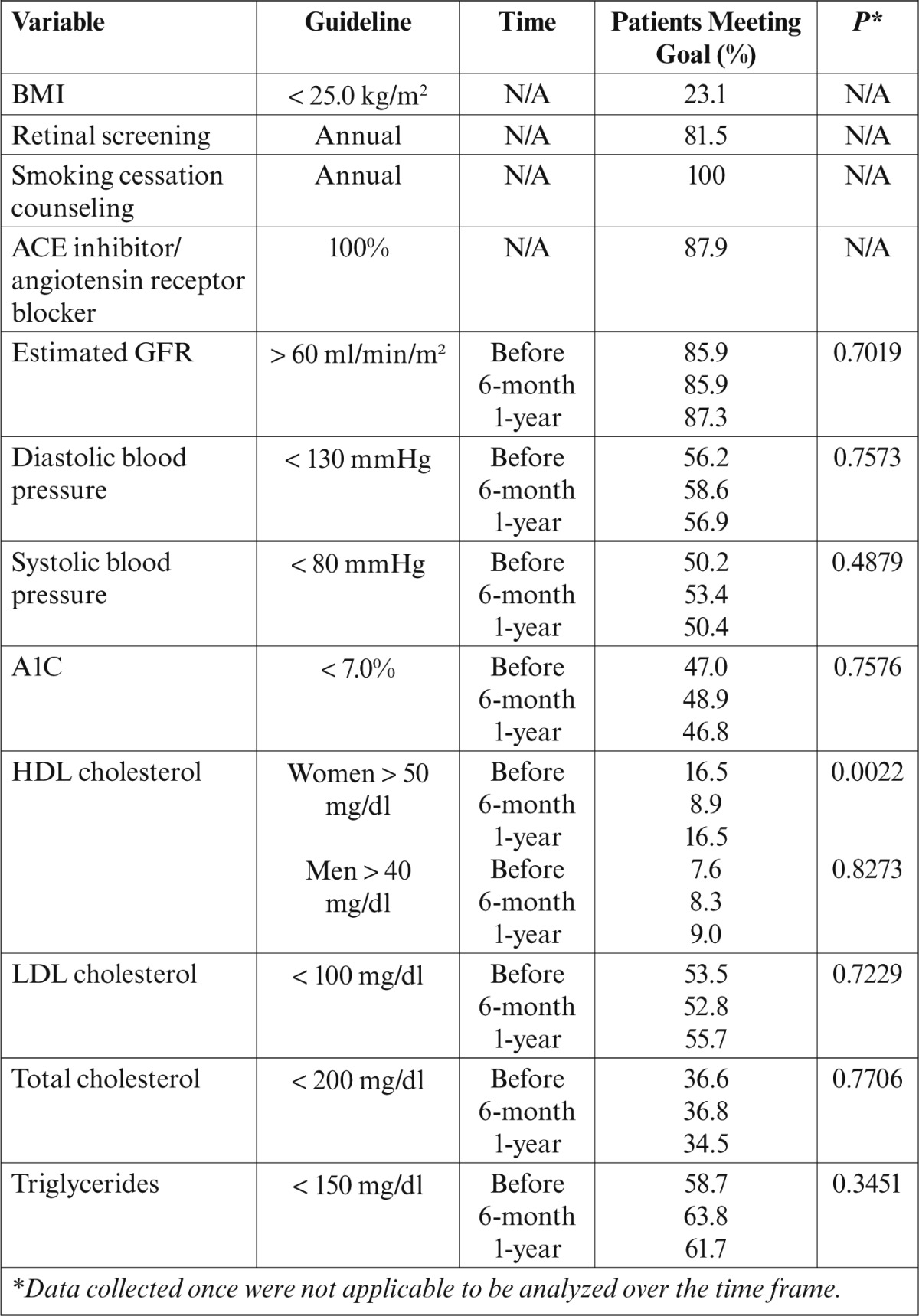
Table 5.
Clinical Characteristics Before and After Implementation
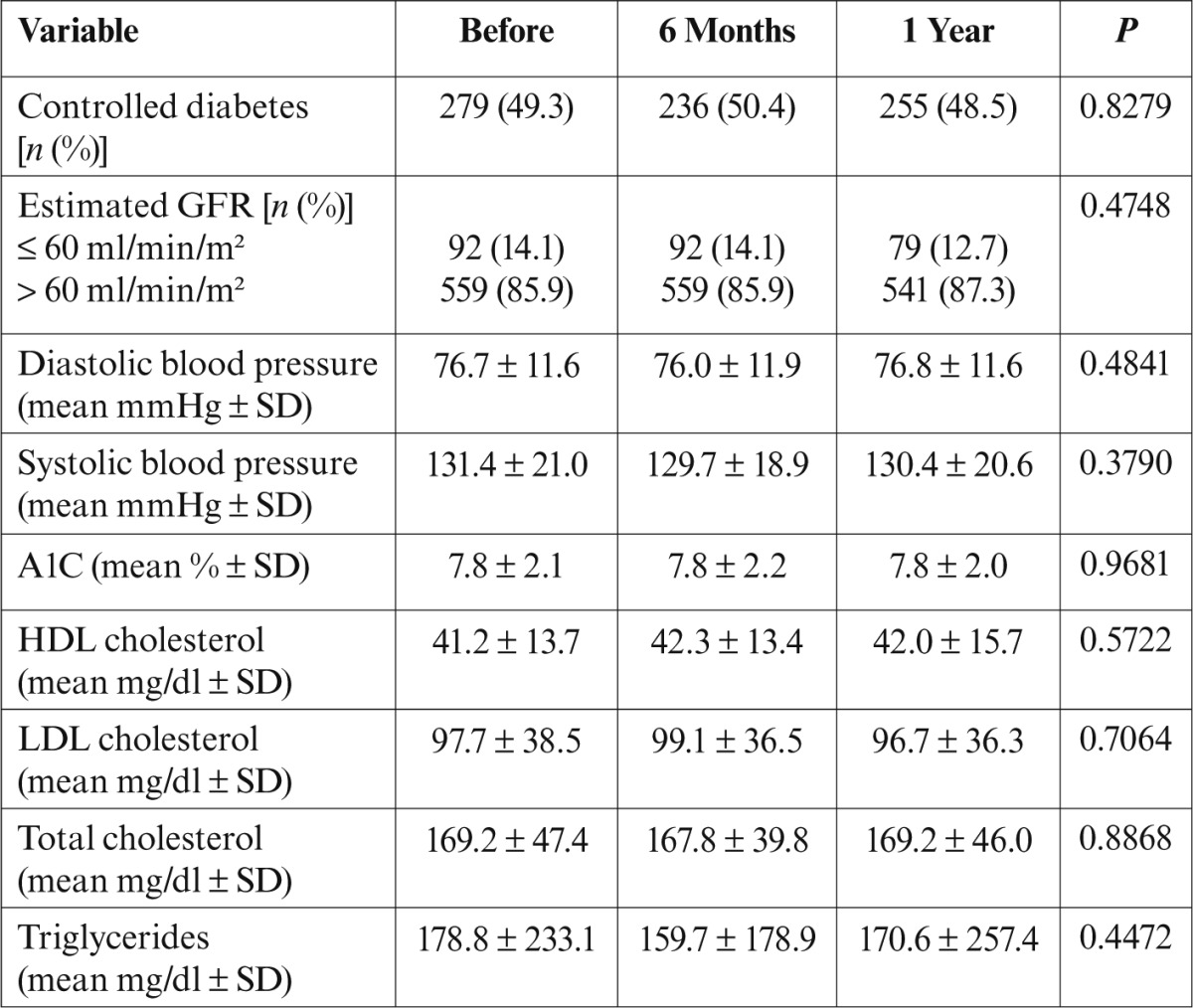
Glycemic Control
To evaluate patients’ glycemic control, this study used the 2013 ADA Standards of Medical Care guidelines26 to compare controlled and uncontrolled diabetes. Findings are summarized in Table 5. Of the 664 patients from all clinics, 234 (35%) had a baseline and 1-year A1C value. Of those 234 patients, 170 (72.7%) had controlled diabetes (A1C < 7%), whereas the A1C values of 64 (27.4%) were in the uncontrolled range. Conversely, 52 (22.4%) with uncontrolled values at baseline attained control, whereas 180 (77.6%) continued to have uncontrolled A1C values. An average A1C value of 7.8% was consistent throughout each time period.
There was also a significant relationship between insurance status and glycemic control. Specifically, trends suggest that those with Medicare and Medicaid have higher rates of controlled diabetes (55%) than those with private (50%) or no insurance (41%).
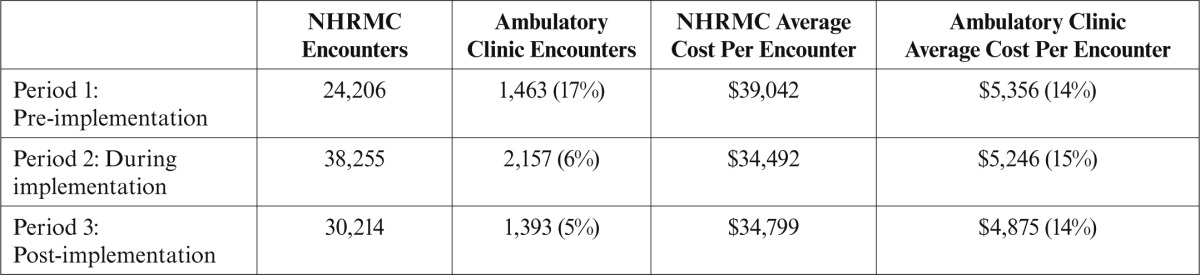
Costs of Care
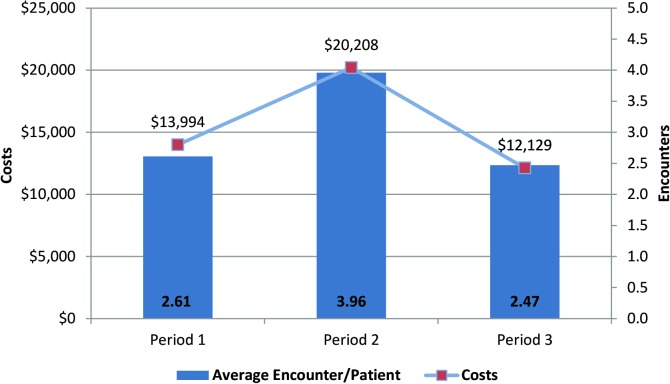
Figure 2 examines Emergency Department and inpatient utilization and costs during three time periods: Period 1 was 1 year before CDSS implementation, Period 2 was the year during implementation of the CDSS, and Period 3 was 1 year after the CDSS implementation. Patient Emergency Department and inpatient encounters were significantly higher in Period 2 than in Periods 1 or 3 (P = 0.0026). Likewise, Emergency Department and inpatient costs were significantly higher in Period 2 (P < 0.0001) compared to Periods 1 or 3.
Figure 2.
NHRMC ambulatory patient population’s Emergency Department/inpatient utilization and costs.
Discussion
This QI project provided an evaluation of the impact of a CDSS within an ambulatory care setting. Although not statistically significant, this study demonstrated that utilization of a CDSS improved diabetes care processes, had a modest effect on diabetes management, and provided a foundation for potential cost savings to the organization.
Within health care settings, barriers exist in making transformations of care a reality. Previous studies have shown that providers adhere to quality measures for chronic illness care only 50% of the time.30 This project demonstrated adherence to ADA 2013 standards of care that far exceeded AHRQ national averages.29
Numerous studies have shown the importance of combined glycemic, lipid, and blood pressure control in helping to prevent both macro- and microvascular complications of diabetes.4,5,16,31 Although not statistically significant, within 1 year, this study noted a 2-percentage-point increase in the number of patients achieving combined glycemic, lipid, and blood pressure control (24.4 to 26.7%). This finding may be helpful when targeting the study’s population with hypertension (86.8%) and hyperlipidemia (73.7%) to prevent complications associated with diabetes.
Seventy-seven percent of the project population was on antihypertensive therapy. A systematic review32 that evaluated the effectiveness of lowering blood pressure in preventing recurrent vascular events in patients with previous stroke or ischemic attack found that those on antihypertensive treatment were 24% less likely to have a stroke, 21% less likely to have an MI, and 21% less likely to have any kind of vascular event. Similarly, 18% of the project population had a stroke diagnosis, suggesting that their risk for additional vascular events was reduced.
Modifying risk factors can also reduce complications associated with diabetes. A recent study33 demonstrated that controlling for certain variables (blood pressure, cholesterol, BMI, tobacco use, A1C, and exercise) could reduce cardiovascular deaths by one-fourth and mortality by one-half. Additionally, Pirie et al.34 suggested that females who quit smoking by the age of 40 years could eliminate 90% of the excess mortality caused by smoking. Although 53.7% of this study population used tobacco, 100% of those using tobacco were counseled in smoking cessation, which highlights the CDSS’s effectiveness in identifying and educating those at risk for smoking complications.
Chronic disease management in general, and diabetes management in particular, continue to challenge and financially burden the health care system.35 A recent study estimated that total costs of diagnosed diabetes have increased by 41% (from $174 billion in 2007 to $245 billion in 2012), accounting for more than one in five health care dollars in the United States.1 Diabetes-associated complications such as amputations can also increase costs by ∼ $3 billion/year ($38,077 per amputation).36 Strategies to improve diabetes health care in a cost-effective manner could include risk factor modification. For example, Medicare can save $11 billion with each 10% improvement in predialysis care.2
Total Emergency Department and inpatient utilization and costs in this QI evaluation of a CDSS implementation are detailed in Table 6. Although emergency and inpatient use and cost-effectiveness were not controlled for a priori, it was observed that there was an increase in the frequency of encounters during CDSS implementation. Overall, however, the proportion of encounters and cost by NHRMC’s ambulatory care patients (in relation to the total patient volume) demonstrated a decrease in emergency and inpatient encounters, both during and after CDSS implementation. Although these observations must be interpreted with caution, they may suggest that more frequent monitoring in the ambulatory setting identified acute issues more readily and that better preventive care strategies may have limited the need for extensive acute care services in the implementation and post-implementation phases. Similar findings suggest that cost savings in emergency and inpatient settings can be realized using a CDSS in diabetes-related care.19–22,37 Although the average national costs of diabetes-related complications far exceed costs associated with primary preventive care measures,38 future work is needed to determine the relationship between CDSS implementation and cost-effectiveness.
Table 6.
NHRMC and Ambulatory Care Clinics: Total Emergency/Inpatient Care Encounters and Associated Costs
Limitations of this study included its retrospective design, separate systems for data entry, lack of cost-effectiveness analysis showing quality-adjusted life-year data, and the varying time frames for implementation of the CDSS within each practice. The aim, however, was to evaluate the impact of a CDSS within an ambulatory care setting. CDSSs provide a viable option to help close the gap between actual and optimal care and to potentially reduce costs through risk factor modification in diabetes-related care.
Conclusion
The CDSS evaluation within the setting described demonstrated improved diabetes care processes, modest effects on management, and potential savings for NHRMC. As a result, this project aligned with NHRMC’s strategic goal to provide high-value, accountable care to the community. Establishing a foundation for potential savings within the NHRMC despite a lack of historical evaluations, this study suggests that risk factor modification can help reduce diabetes complications and the costs of diabetes care. Additionally, the ambulatory care division’s involvement with the IPIP initiative will continue to support QI initiatives geared toward improving diabetes care.
Recognizing the importance of collaboration within community settings can sustain QI across the continuum of diabetes care. CDSS integration into an electronic health record can improve the quality of care by helping to identify subpopulations for disease management, identify patients who might be lost to care, and improve awareness of hospital utilization patterns. In addition, using a CDSS within the setting described allowed for the identification of risk factors, treatment of acute issues, and establishment of preventive care measures, which are accountable-care concerns for all health care organizations.
REFERENCES
- 1.American Diabetes Association : The economic costs of diabetes: is it time for a new treatment paradigm? Diabetes Care 36:775–776, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention National diabetes fact sheet,2011 Available from http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed 11 November 2013 [Google Scholar]
- 3.Holbrook AH, Thabane L, Keshavjee K, Dolovich L, Bernstein B, Chan D, Gerstein H: Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ 181:37–44, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pimazoni-Netto A, Rodbard D, Zanella MT: Rapid improvement of glycemic control in type 2 diabetes using weekly intensive multifactorial interventions: structured glucose monitoring, patient education, and adjustment of therapy: a randomized controlled trial. Diabetes Technol Ther 13:1–8, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaran V, Rushakoff RJ, Owens DK: Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta regression analysis. JAMA 296:427–440, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC: The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care 36:2271–2279, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A: Welldoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther 10:160–168, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Meigs JB, Cagliero E, Dubey A, Murphy-Sheehy P, Gildesgame C, Chueh H, Nathan DM: A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project. Diabetes Care 26:750–757, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Grant RW, Cagliero E, Sullivan CM, Dubey AK, Estey GA, Weil EM, Meigs JB: A controlled trial of population management. Diabetes Care 27:2299–2305, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Bryan C, Boren SA: The use and effectiveness of electronic clinical decision support tools in the ambulatory/primary care setting: a systematic review of the literature. Inform Prim Care 16:79–91, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Augstein P, Vogt L, Kohnert K, Freyse E, Heinke P, Salzsieder E: Outpatient assessment of Karlsburg diabetes management system-based decision support. Diabetes Care 30:1704–1708, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Levetan CS, Dawn KR, Robbins DC, Ratner RE: Impact of computer-generated personalized goals on HbA1c. Diabetes Care 25:2–8, 2002 [DOI] [PubMed] [Google Scholar]
- 13.Christian JG, Bessesen DH, Byers TE, Christian KK, Goldstein MG, Bock BC: Clinic-based support to help overweight patients with type 2 diabetes increase physical activity and lose weight. Arch Intern Med 168:141–146, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Sequist TD, Gandhi TK, Karson AS, Fiskio JM, Bugbee D, Sperling M, Bates DW: A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. J Am Med Inform Assoc 12:431–437, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cleveringa FG, Gorter KJ, Van Den Donk M, Rutten GE: Combined task delegation, computerized decision support, and feedback improve cardiovascular risk for type 2 diabetic patients: a cluster randomized trial in primary care. Diabetes Care 31:2273–2275, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ilag LL, Martin CL, Tabael BP, Isaman DJ, Burke R, Greene DA, Herman WH: Improving diabetes processes of care in managed care. Diabetes Care 26:2722–2727, 2003 [DOI] [PubMed] [Google Scholar]
- 17.O’Connor P, Crain AL, Rush WA, Sperl-Hillen JM, Gutenkauf JJ, Duncan JE: Impact of an electronic medical record on diabetes quality of care. Ann Fam Med 3:300–306, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peterson KA, Radosevich DM, O’Connor PJ, Nyman JA, Prineas RJ, Smith SA, Hannan PJ: Improving diabetic care in practice. Diabetes Care 31:2238–2243, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cleveringa FG, Welsing PM, Van Den Donk M, Gorier KJ, Niessen LW, Rutten GE, Redekop WK: Cost-effectiveness of the diabetes care protocol, a multifaceted computerized decision support diabetes management intervention that reduces cardiovascular risk. Diabetes Care 33:258–263, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feldman PH, Murtaugh CM, Pezzin LE, McDonald MV, Peng TR: Just-in-time evidence-based e-mail ‘reminders’ in home health care: impact on patient outcomes. Health Ser Res 40:865–885, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plaza V, Cobos A, Ignacio-Garcia JM, Molina J, Bergonon S, Garcia-Alonso F, Grupo AI: Cost-effectiveness of an intervention based on Global INitiative for Asthma (GINA) recommendations using a computerized clinical decision support system: a physicians randomized trial. Med Clin (Barc) 126:201–206, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Tierney WM, Overhage JM, Murray MD, Harris LE, Zhou XH, Eckert G, Wolinsky FD: Effects of computerized guidelines for managing heart disease in primary care. J Gen Intern Med 18:967–976, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oxman AD, Thomson MA, Davis DA, Gaynes RB: No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ 153:1423–1431, 1995 [PMC free article] [PubMed] [Google Scholar]
- 24.Peterson KA, Vinicor F: Strategies to improve diabetes care delivery. J Fam Pract 47:55–62, 1998 [PubMed] [Google Scholar]
- 25.Newton WP, Lefebvre A, Donahue KE, Bacon T, Dobson A: Infrastructure for large-scale quality-improvement projects: early lessons from North Carolina Improving Performance in Practice J Contin Educ Health Prof 30:106–113, 2010 [DOI] [PubMed] [Google Scholar]
- 26.American Diabetes Association : Standards of medical care in diabetes—2013. Diabetes Care 36 (Suppl. 1):S4–S10, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics : The NHANES 2009–2010 Dietary Interviewers Procedure Manual. Hyattsville, Md, National Center for Health Statistics; Available from http://www.cdc.gov/nchs/about/major/nhanes/currentnhanes.htm. Accessed 13 October 2013 [Google Scholar]
- 28.World Health Organization : Obesity and overweight: fact sheet. Geneva, Switzerland, World Health Organization, 2013. Available from http://www.who.int/mediacentre/factsheets/fs311/en Accessed 18 October 2013 [Google Scholar]
- 29.Agency for Healthcare Research and Quality : Diabetes care quality improvement: resource guide. National Health Care Quality Report, 2003. Available from http://archive.ahrq.gov/qual/nhqr03/nhqr03.htm. Accessed 28 August 2013 [Google Scholar]
- 30.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofano A, Kern E: The quality of health care delivered to adults in the United States. N Engl J Med 348:2635–2645, 2003 [DOI] [PubMed] [Google Scholar]
- 31.Satlin MJ, Hoover DR, Glesby MJ: Glycemic control in HIV-infected patients with diabetes mellitus and rates of meeting American Diabetes Association management guidelines. AIDS Patient Care STDS 25:5–12, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rashid P, Leonardi-Bee T, Bath P: Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke 34:2741–2748, 2003 [DOI] [PubMed] [Google Scholar]
- 33.Yang Q, Cogswell ME, Flanders WD, Yong Y, Zhang Z, Loustalot F, Gillespie C, Merute R, Hu FB: Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 28:1278–1283, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pirie K, Reeves GK, Green J, Beral J, Million Women Study Collaborators: The 21st Century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381:13–141, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meyer AA, Donahue KE, Batish S, Gentry T, Adams A, Brown A, Baumann M: Patient care outcomes of the SEAHEC Improving Performance in Practice (IPIP) experience. J Am Board Fam Med 26:16–23, 2013 [DOI] [PubMed] [Google Scholar]
- 36.Amputee Coalition : Fact sheet: diabetes and lower extremity amputations. Available from www.amputee-coalition.org/fact_sheets/diabetes_leamp.html. Accessed 14 September 2013
- 37.Fireman B, Bartlett J, Selby J: Can disease management reduce health care costs by improving quality? Health Aff (Millwood) 23:63–75, 2004 [DOI] [PubMed] [Google Scholar]
- 38.American Diabetes Association : Economic costs of diabetes in the U.S. in 2012. Diabetes Care 36:1033–1046, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]