In Brief
Ward management of diabetic ketoacidosis (DKA) using subcutaneous insulin in specific patient populations is safe and effective, but insulin administered by continuous infusion has not been analyzed in this setting. This retrospective cohort study utilizing a nursing-driven, continuous infusion insulin calculator demonstrated safe and effective treatment of patients with DKA on medicine wards.
Diabetic ketoacidosis (DKA) is a potentially life-threatening manifestation of type 1 diabetes, the incidence of which has increased from 3.2 to 4.6 cases/10,000 population between 1988 and 2009.1 Fortunately, DKA treatment is very effective; experienced centers have an estimated mortality rate from DKA of < 5%.2 Treatment of DKA focuses on restoring circulatory volume, clearing ketones, stabilizing blood glucose, and managing electrolyte abnormalities.
The costs of DKA treatment are significant, with estimated mean expenses for a single hospitalization ranging from $7,470 to $20,864.3 The annual cost of DKA management to the health care system is in excess of $1 billion and accounts for one of every two dollars spent on the management of type 1 diabetes in adults.2
One potential intervention to decrease these costs is to minimize the use of hospital intensive care units (ICUs) when patients can receive safe and effective care on hospital wards. Expert opinion has provided some guidance for ICU use based on the severity of illness at presentation, but evidence to support such recommendations is minimal.4,5 The American Diabetes Association (ADA) provides limited specific recommendations regarding ICU utilization, whereas a 2011 position statement and care recommendations from the Joint British Diabetes Societies recommend intensive care for patients meeting any of the following criteria: serum ketones > 6 mmol/L, anion gap >16, bicarbonate level < 5 mmol/L, pH < 7.1, potassium < 3.5 mmol/L, Glasgow coma scale < 12, O2 saturation < 92%, systolic blood pressure < 90 mmHg, or pulse > 100 or < 60 bpm.6
Clinical practice with regard to DKA management varies greatly, as described in a 2009 review in the state of New York,7 showing that patients with DKA comprised 0.4% of all hospital admissions, with 52.6% of these patients admitted to ICUs. This study identified patient factors that may lead to ICU admission, including income, insurance provider, teaching status of the hospital, and hospital occupancy, rather than the clinical presentation of the patients. No difference was noted in duration of hospitalization or mortality between ICU and non-ICU management. Previous studies have shown that patients with DKA can be safely and effectively treated with subcutaneous insulin on medicine wards; however, we have not identified any studies of ward treatment of DKA with continuous infusions of insulin.8–12
The Medical University of South Carolina (MUSC) treats a similar percentage of patients on general medicine wards, as seen in the New York study described above,7 using an internally developed, Internet-based, nursing-driven insulin infusion protocol. The safety and efficacy of the MUSC protocol was validated in a population of cardiothoracic surgery patients.13 DKA treatment at MUSC calls for blood glucose to be checked hourly, with a target of 150–200 mg/dl, regardless of the location of treatment. Monitoring treatment safety, both in the ICU and on medicine wards, is crucial because hypoglycemia has been shown to increase mortality among hospitalized patients.14 The goal of this study was to review the overall management of DKA and characterize patients who were safely and effectively treated on general medicine wards compared to patients treated in the ICU.
Research Design and Methods
This retrospective cohort analysis of adult patients treated for DKA at MUSC between 1 June 2011 and 30 September 2012 was approved by the university’s institutional review board.
Patient selection
All patients ≥ 18 years of age who were treated at MUSC during the study period with a diagnosis of DKA or type 1 diabetes with ketosis were included. Type 1 diabetes was confirmed through chart review. Patients with type 2 diabetes, those receiving hemodialysis, and those receiving DKA treatment initiated at another hospital were excluded. The diagnosis of DKA was confirmed by the presence of at least two of the following: elevated anion gap attributable to DKA, serum pH < 7.4, elevated blood glucose, or presence of serum or urine ketones.
Study methods
Baseline characteristics were collected from the time of presentation with DKA. Laboratory values such as the A1C, pH, serum or urine ketones, and serum osmolality were not measured for some hospitalizations; in these instances, no value was included in the analysis. Nominal data were analyzed with a Fisher’s exact test, and continuous data were analyzed using a Student’s t test.
The Internet-based intravenous (IV) insulin infusion calculator (IVIIC) used in this institution employs a multiplier, which is a surrogate for insulin sensitivity based on the current and previous glucose values.15 The units of insulin to be infused per hour is calculated based on (current glucose – 60 mg/dl) × [multiplier]. For DKA, the multiplier is set at 0.01 initially.13,15
Study outcomes
The primary effectiveness outcome was the time to closure of the anion gap and percentage of blood glucose readings within a goal range of 150–200 mg/dl while on insulin infusion. The goal range of 150–200 mg/dl was previously established based on expert opinion at MUSC, with consideration for the glucose targets for initial DKA treatment published in ADA guidelines.16 Duration of hospitalization was calculated from the time of admission to the time of discharge, which excluded emergency department care before admission.
Secondary safety outcomes included the incidence of hypoglycemia, both while on insulin infusion and after conversion to subcutaneous insulin, and the incidence of re-opening of the anion gap. Hypoglycemia was characterized as mild for glucose values 60–69 mg/dl, moderate for glucose values of 40–59 mg/dl, and severe for glucose values < 40 mg/dl. Overall rates of hypoglycemia were based on a blood glucose value < 70 mg/dl. Conversion to subcutaneous insulin was analyzed for appropriate overlap of 2 hours before discontinuation of IV insulin infusion.
Study Results
One hundred and twenty-three admissions coded as DKA were screened, of which 52 were excluded for either type 2 diabetes (n = 33), hemodialysis (n = 4), initiation of treatment at another hospital (n = 9), or not meeting diagnostic criteria for DKA (n = 6). Of the remaining cases, 40 were treated on the general medicine wards and 31 were treated in the ICU.
Patients were generally 25–35 years of age, with a median A1C of 11.9% (Table 1). Patients in the ICU had higher admission blood glucose and lower bicarbonate levels (Table 2). A total of 1,526 blood glucose readings were obtained, including 781 from patients initially treated in the ICU and 745 from patients treated on medicine wards (Table 3). There was no difference between ICU and ward patients in the frequency of values above, within, or below goal. The incidence of hypoglycemia while on insulin infusion was 12.9 and 12.5% in the ICU and medicine wards, respectively, and all cases of severe hypoglycemia (blood glucose < 40 mg/dl) occurred in the ICU (Figure 1).
Table 1.
Baseline Characteristics (n = 71)
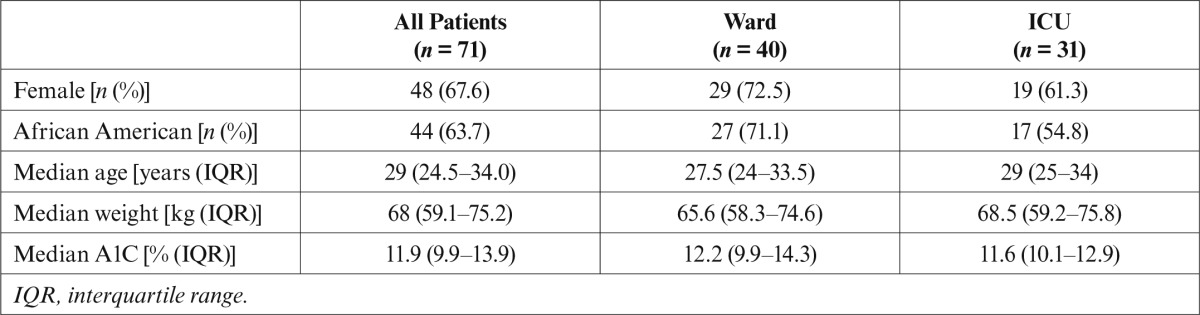
Table 2.
Admission Laboratory Values (median [IQR])
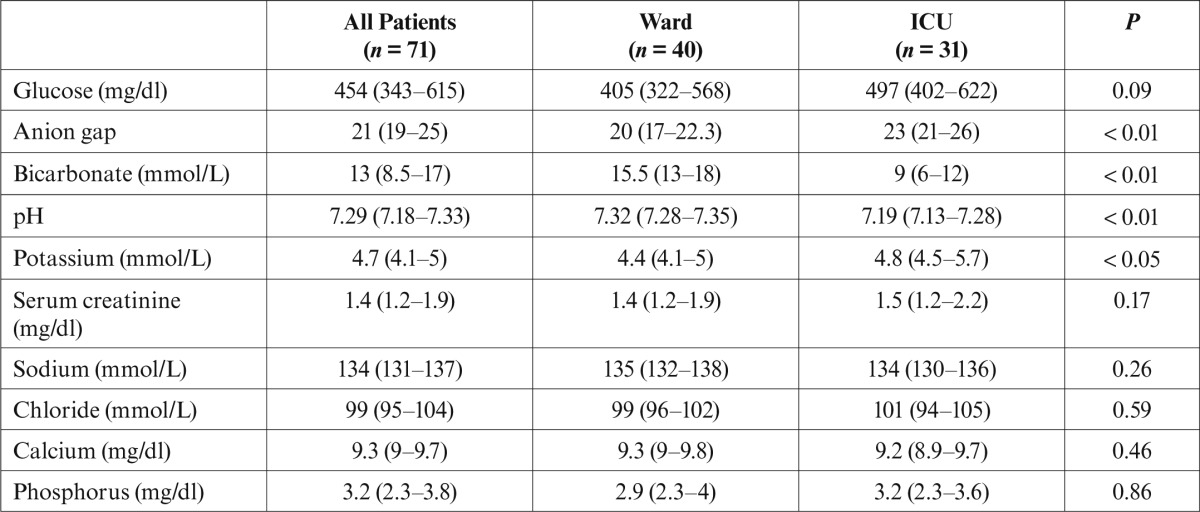
Table 3.
Clinical Outcomes
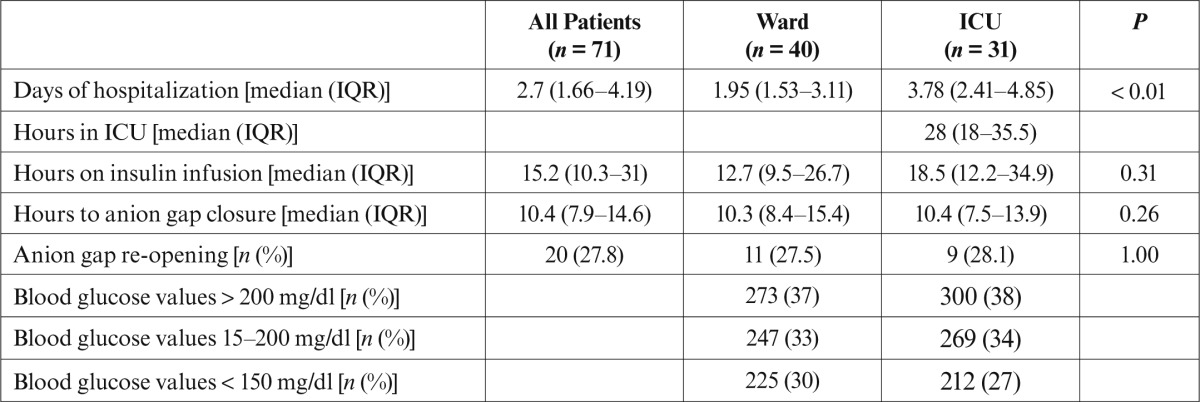
Figure 1.
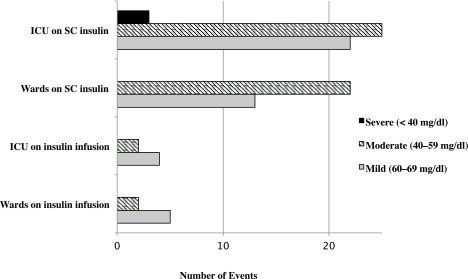
Hypoglycemic events. SC, subcutaneous.
The average time to documented anion gap closure was just over 10 hours regardless of the level of care. Patients in the ICU tended to stay on insulin infusions longer than those on the wards (18.5 vs. 12.7 hours, respectively), but this was not statistically significant. ICU patients had a significantly longer duration of hospitalization (3.78 vs. 1.95 days; P < 0.05). The increased duration was not accounted for by ICU length of stay, which was a median of 28 hours before transfer to the wards. An appropriate 2-hour overlap during the conversion of IV insulin to subcutaneous insulin occurred in 71% and 59% of patients treated in the ICU and medicine wards, respectively. One patient died during hospitalization because of complications of a small bowel obstruction days after resolution of DKA.
Discussion
ICU utilization was slightly lower at our institution than the overall rates previously published by Gershengorn et al.7 The authors noted that academic medical centers had a lower incidence of ICU utilization but did not specify the rates.
This study found that the patients treated on medicine wards had rates of hypoglycemia similar to those of patients treated in an ICU on IV insulin. Previous studies limited the amount of time during which hypoglycemia screening occurred, whereas this analysis encompassed the entire hospitalization; therefore, the ability to compare hypoglycemia incidence rates was limited.
Nonetheless, we observed a lower incidence than Fusco et al.,17 despite counting each event separately. Similarly, a study by Bull et al.18 found that ∼ 19% of patients had hypoglycemia (defined as < 70 mg/dl). Two studies analyzing the use of subcutaneous insulin for DKA on medicine wards found rates of hypoglycemia closer to 5% but used a lower threshold for hypoglycemia (< 60 mg/dl).9,10 The incidence of hypoglycemia after conversion to subcutaneous insulin was slightly higher than what was found in a study by Umpierrez et al.,11 which documented a range of 15–41% depending on the type of insulin to which patients were converted.
The incidence rates of severe hypoglycemia in the ICU were generally the result of conversion to subcutaneous insulin doses with varying nutritional supplementation during the hospitalization. In the ICU, other confounding variables such as concomitant illness, medications causing elevated glucose levels leading to additional insulin administration, or aggressive dosing of correction insulin, cannot be ruled out as potential reasons for severe hypoglycemia. Similarly, feeding patients and not providing prandial insulin coverage while using the IVIIC may over-treat hyperglycemia, leading to subsequent hypoglycemia. Other previously identified risk factors for hypoglycemia in the ICU that were not evaluated in this study include continuous renal replacement therapy with bicarbonate replacement, sepsis with inotropic support, and octreotide therapy.19 Because glucose samples are often measured from a central line in our ICU, peripheral vasoconstriction is not a likely contributor. Taken together, these findings support the safety of treating DKA on the wards, with the caveat that glucose values must be measured hourly.
DKA resolution was similar to previously published studies of patients in an ICU even though many of our patients were treated on the wards.18 Of note, the lower initial bicarbonate level and increased anion gap in ICU patients may reflect a greater severity of illness. This is supported by the higher potassium levels, which may indicate greater degrees of dehydration. Admitting these more severely ill patients to the ICU is consistent with previously published recommendations.5,6 However, the safe and effective ward management of DKA in patients who have less severe illness supports previously published opinions on the practice of stratifying patients to conserve resources.20
Another interesting outcome was the shorter duration of hospitalization for patients treated on medicine wards, despite the fact that all other outcomes were not significantly different. Two previous studies discussing DKA treatment with subcutaneous insulin on medicine wards had baseline characteristics that were fairly similar but slightly higher initial blood glucose and lower bicarbonate levels.9,10 These patients treated with subcutaneous insulin had a longer length of hospitalization, ranging from 3.4 to 4 days, than those treated on the wards in our study.9,10 Although the greater severity of illness of ICU patients may account for some of the increased length of stay, most patients in both groups were transitioned to subcutaneous insulin during the first 24 hours after admission. Because handoffs pose a significant challenge in patient care, exploring the impact of transition from the ICU to the ward on length of stay for DKA patients may be warranted.21
In total, the results of this study support the safe and effective care of patients with DKA on general medicine wards. This may allow ICU beds to remain available for patients with other illnesses and potentially improve outcomes for those patients. Furthermore, it could limit the number of transitions of care and reduce the costs of treating DKA.
The significant limitation to this study is its inability to evaluate fluid resuscitation because of variances in documentation among the emergency department, ICU, and wards. The ADA and European guidelines both note that appropriate fluid resuscitation is imperative for appropriate DKA treatment. Nonetheless, the rapid resolution of DKA, which was similar to previous reports, in conjunction with short hospital length of stay, suggests that fluid resuscitation was likely adequate.
An additional limitation of the study includes its retrospective design and lack of laboratory values for all patients. Although the ADA recommends using pH as a marker of DKA resolution, six patients did not have an initial pH value, and the majority of patients only had one pH level reported during the course of their hospitalization. This lack of data limits comparisons with previously published studies that used this marker for DKA resolution.17,18
Conclusion
The results of this study show that patients with characteristics such as those described in Table 2 can be safely and effectively treated for DKA on medicine wards using an IVIIC with outcomes similar to those treated in an ICU. In addition to improving bed management issues in the ICU and reducing the number of transitions in care, the treatment of these patients on medicine wards may have a significant financial impact on the health care system. Attribution of a decreased length of stay to transitions in care warrants further study.
REFERENCES
- 1.Centers for Disease Control and Prevention : Age-adjusted hospital discharge rates for diabetic ketoacidosis as first-listed diagnosis per 10,000 population, United States, 1988–2009 [article online]. Available from http://www.cdc.gov/diabetes/statistics/dkafirst/fig7.htm. Accessed 15 May 2013
- 2.Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM: Hyperglycemic crises in diabetes. Diabetes Care 27 (Suppl. 1):S94–S102, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Maldonado MR, Chong ER, Oehl MA, Balasubramanyam A: Economic impact of diabetic ketoacidosis in a multiethnic indigent population: analysis of costs based on the precipitating cause. Diabetes Care 26:1265–1269, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Savage MW: Management of diabetic ketoacidosis. Clin Med 11:154–156, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marinac JS, Mesa L: Using a severity of illness scoring system to assess intensive care unit admissions for diabetic ketoacidosis. Crit Care Med 28:2238–2241, 2000 [DOI] [PubMed] [Google Scholar]
- 6.Savage MW, Dhatariya KK, Kilvert A, Rayman G, Rees JA, Courtney CH, Hilton L, Dyer PH, Hamersley MS: Joint British diabetes societies guideline for the management of diabetic ketoacidosis. Diabet Med 28:508–515, 2011 [DOI] [PubMed] [Google Scholar]
- 7.Gershengorn HB, Iwashyna TJ, Cooke CR, Scales DC, Kahn JM, Wunsch H: Variation in use of intensive care for adults with diabetic ketoacidosis. Crit Care Med 40:2009–2015, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kitabchi AE, Umpierrez GE, Fisher JN, Murphy MB, Stentz FB: Thirty years of personal experience in hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. J Clin Endocrinol Metab 93:1541–1552, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Umpierrez GE, Cuervo R, Karabell A, Latif K, Freire AX, Kitabchi AE: Treatment of diabetic ketoacidosis with subcutaneous insulin aspart. Diabetes Care 27:1873–1878, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Umpierrez GE, Latif K, Stoever J, Cuervo R, Park L, Freire AX, Kitabchi AE: Efficacy of subcutaneous insulin lispro versus continuous intravenous regular insulin for the treatment of patients with diabetic ketoacidosis. Am J Med 117:291–296, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Umpierrez GE, Jones S, Smiley D, Mulligan P, Keyler T, Temponi A, Semakula C, Umpierrez D, Peng L, Ceron M, Robalino G: Insulin analogs versus human insulin in the treatment of patients with diabetic ketoacidosis. Diabetes Care 32:1164–1169, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karoli R, Fatima J, Salman T, Sandhu S, Shankar R: Managing diabetic ketoacidosis in non-intensive care unit setting: role of insulin analogs. Indian J Pharmacol 43:398–401, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hermayer KL, Neal DE, Hushion TV, Irving MG, Arnold PC, Kozlowski L, Stroud MR, Kerr FB, Kratz JM: Outcomes of a cardiothoracic intensive care web-based online intravenous insulin infusion calculator study at a medial university hospital. Diabetes Technol Ther 9:523–534, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Garg R, Hurwitz S, Turchin A, Trivedi A: Hypoglycemia, with or without insulin therapy, is associated with increased mortality among hospitalized patients. Diabetes Care 36:1107–1110, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hermayer KL, Cawley P, Arnold P, Sutton A, Crudup J, Kozlowski L, Hushion TV, Sheakley ML, Epps JA, Weil RP, Carter RE: Impact of improvement efforts on glycemic control and hypoglycemia at a university medical center. J Hosp Med 4:331–339, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN: Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32:1335–1342, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fusco N, Gonzales J, Yeung SYA: Evaluation of the treatment of diabetic ketoacidosis in the medical intensive care unit. J Health Syst Pharm Residents 1:1–6, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Bull SV, Douglas IS, Foster M, Albert RK: Mandatory protocol for treating adult patients with diabetic ketoacidosis decreases intensive care unit and hospital lengths of stay: results of a nonrandomized trial. Crit Care Med 35:41–46, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Mechanick JI, Handelsman Y, Bloomgarden ZT: Hypoglycemia in the intensive care unit. Curr Opin Clin Nutr Metab Care 10:193–196, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Barski L, Kezerle L, Zeller L, Zektser M, Jotkowitz A: New approaches to the use of insulin in patients with diabetic ketoacidosis. Eur J Intern Med 24:213–216, 2013 [DOI] [PubMed] [Google Scholar]
- 21.Abraham J, Nguyen V, Almoosa KF, Patel B, Patel VL: Falling through the cracks: information breakdowns in critical care handoff communication. AMIA Annu Symp Proc 2011:28–37, 2011 [PMC free article] [PubMed] [Google Scholar]


