Abstract
Objectives:
It has been repeatedly shown that clozapine is underutilized and there is delayed use of it in clinical practice.
Method:
An online survey was sent to 2771 consultant psychiatrists registered with the Royal College of Psychiatrists in the UK. A total of 243 responded to this survey. The survey elicited their views and experiences in using clozapine as well as to identify what may be the underlying causes for its underutilization.
Results:
Over 75% acknowledged that they had good training in using clozapine and about 56% had clozapine-dedicated service. However, 40.5% preferred to use several other antipsychotics prior to considering clozapine. A third felt it was not safe to start clozapine in the community and 42% had less than five patients on clozapine. Eleven possible reasons for clozapine underutilization were identified including concerns about side effects, patients not wanting to have blood tests and lack of experience or knowledge. Knowledge deficiency in certain aspects of clozapine use were identified, e.g. a third of respondents did not know that the risk of agranulocytosis changes with time, 42.7% did not think that clozapine can reduce substance use, while 20% were not aware of its benefit in reducing suicidal risk.
Conclusions:
Important areas of concern such as managing side effects and deficiency in evidence-based use of clozapine were identified. These can be targeted in training and professional development programme.
Keywords: antipsychotics, clozapine, treatment-resistant schizophrenia
Background
Clozapine was reintroduced in clinical practice worldwide following a seminal study by Kane and colleagues [Kane et al. 1988]. Since then, several other studies [Rosenheck et al. 1997; Lewis et al. 2006; McEvoy et al. 2006], meta-analysis [Davis et al. 2003; Wahlbeck et al. 1999; Essali et al. 2009] and reviews [Agid et al. 2010] have repeatedly shown that clozapine is more efficacious than other antipsychotics in treatment-resistant schizophrenia (TRS). Despite good evidence of efficacy, clozapine is associated with a number of side effects. A review by Safferman and colleagues [Safferman et al. 1991] lists drowsiness or sedation (39%), salivation (31%), tachycardia (25%), dizziness (19%), constipation (14%), nausea and vomiting (11%) as among the commonly reported side effects of clozapine. Other side effects include weight gain, hypotension, sweating, seizures, and dry mouth [Safferman et al. 1991; Kumlien and Lundberg, 2010]. In addition, clozapine has other rare but serious side effects such as agranulocytosis, cardiomyopathies and myocarditis [Killian et al. 1999; Raja, 2011]. There are some suggestions that clozapine’s side-effects profile and the need to undergo regular blood tests are some of the underlying reasons why patients and clinicians are less likely to opt for its use [Nielsen et al. 2010; Raja, 2011; Patel, 2012]. Despite all of the above-mentioned challenges, however, under the current stringent monitoring system which includes regular blood tests, clozapine continues to be administered safely and is well tolerated by many [Agid et al. 2010].
Evidence from a number of studies suggests that clozapine remains underutilized in many parts of the world [Weissman, 2002; Joober and Boksa, 2010]. The reasons for the inadequate use remain speculative and may include the perception of the drug as dangerous medicine [Farooq and Taylor, 2011] or difficulties associated with initiating and maintaining the treatment. A study by Taylor and colleagues [Taylor et al. 2003] showed that on average it took 5 years before patients are started on clozapine in the UK. It was 9.7 years for patients in New Zealand [Wheeler, 2008]. The reasons for delayed use of clozapine remain obscure, and may include several factors related to patients, carers and clinicians. A recent survey by Nielsen and colleagues [Nielsen et al. 2010] on the attitude and knowledge of 137 psychiatrists in Denmark of which only 100 were consultants revealed that some have never prescribed clozapine despite having worked for over 5 years. A total of 64% preferred to use combinations first and 66% felt patients on clozapine were less satisfied. There is no UK based study in peer-reviewed journals that has looked into the attitudes and the practice of consultant psychiatrists regarding the use of clozapine. We aimed to explore their views and their experience on the use of clozapine.
Methodology
We conducted an online survey of consultant psychiatrists (herein addressed as psychiatrists) registered with the faculty of the general adult and community psychiatry of the Royal College of Psychiatrists. Following the approval by the faculty, the College sent the link to the survey through email shot to its members in September 2013, requesting to complete the survey. No follow-up or reminder email was sent. Two weeks after the email, all responses were collected and analysed.
A questionnaire was designed to elicit the views and the experiences of practising psychiatrists about the use and barriers in using clozapine. The questionnaire was based on the evidence gathered from literature and experience in clinical practice. The questionnaire was piloted first for clarity, relevance and ease of administration, in a group of 10 local psychiatrists. The questionnaire consisted of three main parts: part one dealt with general demographic information and in which sector they worked, e.g. community mental health team, inpatients or assertive outreach. The second part had open-ended questions asking about the experience and views in using clozapine. Part three had 16 statements that dealt with their experience, knowledge and attitude toward using clozapine in clinical practice. Responders had five options to choose from based on a five-point Likert scale: strongly agree, agree, do not know, disagree and strongly disagree. The questionnaire is available from the authors on request. Data analysis was carried out using SPSS 21 for window. Descriptive statistics were used to describe demographic information and views of the participants. Chi-square test was used to examine association between categorical responses.
Results
The survey was sent to 2771 members, 245 (8.8%) responded within 2 weeks of the survey. Two were excluded for the following reasons; one was a nurse prescriber and the other has worked as a consultant for just a month. The final analysis is based on 243 responses (total responses may not add to 243 in some areas due to differing proportions responding to each question). Table 1 gives a summary of the demographic details of participants and clozapine service characteristics. The majority of respondents were male (n = 141, 58.8%), in the age group 41–50 years (n = 104, 43.5%) and almost half (n = 122, 50.2%) worked as community mental health team (CMHT) psychiatrists. Only as small proportion (n = 28, 11.7%) were in academic posts. On average consultants have been in their current posts for 7.2 years, and have worked as consultant for 11.2 years. Due to functionalization of the teams, the majority (n = 182, 74.9%) had worked in just one sector while 61 (25.1%) worked across several sectors.
Table 1.
Demographics and clozapine service characteristic.
| Description | n (%) |
|---|---|
| Gender | |
| Female | 99 (41.3) |
| Male | 141 (58.8) |
| Academic post | |
| YES | 28 (11.7) |
| NO | 212 (88.3) |
| Age distribution | |
| 31–40 | 59 (24.7) |
| 41–50 | 104 (43.5) |
| 51–60 | 62 (25.9) |
| Over 61 | 14 (5.9) |
| Sector currently working in | |
| Community mental health team | 122 (50.2) |
| Inpatient | 66 (27.2) |
| Crisis/home treatment team | 27 (11.1) |
| Rehabilitation | 25 (10.3) |
| Assertive outreach | 19 (7.8) |
| Early intervention team | 18 (7.4) |
| Forensic | 8 (3.3) |
| Others | 44 (18.1) |
| Working in one sector of mental health | |
| YES | 182 (74.9) |
| NO | 61 (25.1) |
| Have clozapine dedicated service | |
| YES | 130 (56.5) |
| NO | 100 (43.5) |
| Agreed there was a delay in starting clozapine | |
| YES | 184 (80.7) |
| NO | 44 (19.3) |
| Have started clozapine in past 6 months | |
| YES | 144 (65.2) |
| NO | 77 (34.8) |
| Have started clozapine in past 12 months | |
| YES | 113 (67.7) |
| NO | 54 (32.3) |
| Have used clozapine for other conditions | |
| YES | 104 (45.4) |
| NO | 125 (54.6) |
Service characteristics and delay in starting clozapine
A total of 230 responded to the question about having clozapine-dedicated service in their trusts. The majority (n = 130, 56.5%) agreed that they have a dedicated service for patients on clozapine. Most consultants agreed that they have started someone on clozapine either in the last 6 months (n = 144, 65.2%) or during the last 1 year (n = 113, 67.7%). There was no significant association between having a dedicated service for clozapine and consultant starting patients on clozapine in the previous 6 (χ2 = 0.154, d.f. = 1, p = 0.70) or 12 months (χ2 = 0.019, d.f. = 1, p = 0.89).
Figure 1 outlines the average number of patients on clozapine for each consultant. Of the 192 who provided the estimates, 32 (16.7%) had no patients despite having been in their current posts for 7 years, 48 (25%) had between 1–4 patients, an indication that nearly 42% had less than 5 patients on their caseload at the time of the survey. There was association of having less than five patients and working as inpatient (χ2 = 15.33, d.f. = 1, p <0.001) or crisis and home treatment team (HTT) psychiatrist (χ2 = 4.02, d.f. = 1, p < 0.05). There was no association with working as CMHT, assertive outreach team, early intervention service or rehabilitation consultants.
Figure 1.
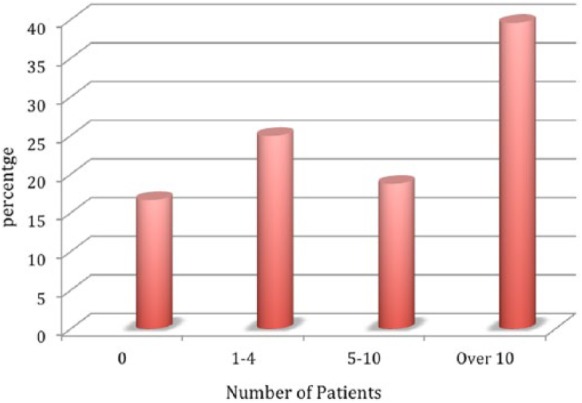
Number of patients on clozapine per consultant.
Out of 228 participants who responded to the question about the possible delay in starting clozapine, 184 (80.7%) agreed that there was a delay in initiating clozapine treatment. Table 2 summarizes what clinicians believed to be the underlying reasons. The frequently mentioned reasons were concerns about side effects including metabolic problems, reluctance to have blood test, knowledge deficiency or lack of experience, the general reluctance among patients to take clozapine, concerns about poor compliance and service fragmentation and poor community support.
Table 2.
Reasons for delayed use of clozapine.
| Frequency | |
|---|---|
| Side effects/metabolic problems | 80 |
| Reluctance to have blood test | 74 |
| Lack of experience/knowledge | 71 |
| Patient/family reluctance to use clozapine | 60 |
| Clinicians concerns about poor compliance | 54 |
| Complex to initiate and manage | 42 |
| Service fragmentation/no community support | 39 |
| Need to admit/bed shortage | 32 |
| Tendency to try other antipsychotics first | 28 |
| Delayed diagnosis/not sure about diagnosis | 12 |
| Negative views of others | 8 |
Some specific issues highlighted as regards to delayed use of clozapine included the need for inpatient admission before starting clozapine; with some trusts insisting that patients must be admitted first. However, for those earmarked for clozapine, most were not acutely ill and hence were not given priority for inpatient beds or even under HTTs. Psychiatrists trying several antipsychotics felt that clozapine was the last resort or were concerned about serious side effects and the drug was perceived to be associated with high risks. Lack of experience/knowledge was attributed to several factors such as frequent job changes, lack of exposure as trainee and inadequate pharmacological knowledge, resulting in overestimation of side effect and not appreciating higher efficacy of clozapine in TRS.
Knowledge and attitude in the use of clozapine
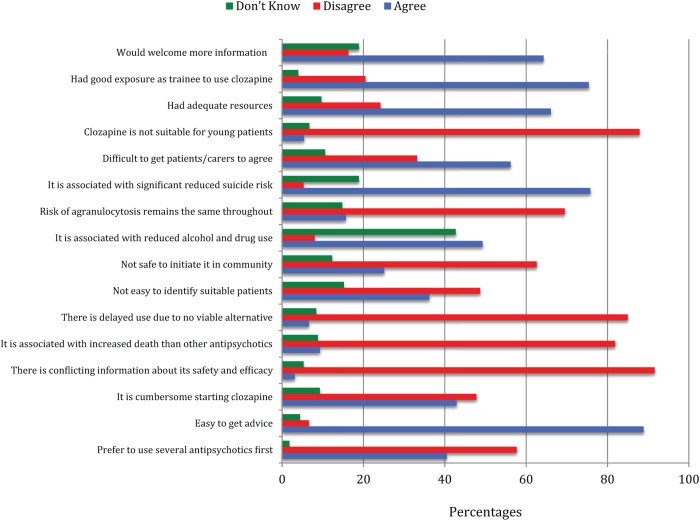
Figure 2 summarizes the findings on the general knowledge and attitude towards clozapine utilization. About three quarters of respondents (n = 169, 75.4%) agreed that they had good exposure in using clozapine as trainees. Nearly 90% agreed that clozapine is suitable for young patients. About a quarter (n = 55, 24.2%) felt that that they lacked adequate resources and 127 (56.2%) agreed that it is difficult to get patients and carers to accept to go on clozapine. Nearly a third either felt that the risk of agranulocytosis remains the same throughout treatment with clozapine or did not know that the risk changes. A significant number, 42.7% did not know that there is some evidence that the use of clozapine may be associated with reduced alcohol and drug use in patients with schizophrenia. Although over 75% were aware that clozapine reduces suicide risk, nearly a fifth (18.9%) did not know. About 40.5% preferred to use several other antipsychotics before considering clozapine. A quarter of consultants (57, 25.1%) felt it was not safe to start clozapine in the community and a further (28, 12.3%) did not know whether it was safe to do so. Over a third of clinicians (36.2%) felt it was not easy to identify suitable patients for clozapine. The initiation of clozapine was acknowledged as being cumbersome by 42.9%.
Figure 2.
Knowledge, attitude and experience of using clozapine.
Clozapine’s other indications and untoward effects
A total of 104 (45.4%) out of 229 acknowledged that they have used clozapine to treat other conditions. The frequently mentioned diagnoses were resistant schizoaffective disorders (52 times), difficult to treat bipolar affective disorder (38 times), borderline personality disorder (25 times) and schizophrenia where patients were unable to tolerate other antipsychotics (13 times). Mentioned less than 10 times in decreasing order were psychosis related to parkinsonism, persistent delusional disorder, psychotic depression and severe head injury.
A total of 105 (45.5%) out of 231 respondents acknowledged that their patients had experienced untoward effects while on clozapine. The frequently mentioned undesirable events were myocarditis, constipation, seizure, sudden death, and cardiomyopathy (see Table 3). We observed that there was a significant association of psychiatrists recalling to have started someone on clozapine in the past 6 months and reporting of patients experiencing serious side effects (χ2 = 6.11, d.f. = 1, p < 0.05).
Table 3.
Reported clozapine-related adverse events.
| Frequency | |
|---|---|
| Myocarditis | 21 |
| Cardiomyopathy | 10 |
| Severe tachycardia | 7 |
| Arrhythmias | 4 |
| Hypotension | 8 |
| Sudden death | 16 |
| Constipation | 17 |
| Liver problems | 5 |
| Deep vein thrombosis/pulmonary embolism | 3 |
| Overdose | 4 |
| Toxicity | 4 |
| Seizure | 16 |
Discussion
Consultant psychiatrists play a leading role in starting clozapine. Previous studies have explored the use of clozapine in older adult psychiatrists [Paranthaman and Baldwin, 2006] and a mixed group of clinicians (doctors, nursing staffs and pharmacists) working in one mental health trust [Gee et al. 2013]. To the best of the authors’ knowledge this is the first study to focus on the views of consultant psychiatrists nationwide working with adult patients aged 18–65 on the use of clozapine in practice.
Major limitations of our study include the low response rate, which was understandable as we could only send one email shot, and that data was collected within 2 weeks of the email request. The online surveys have their limitations and a number of reminders are usually required with some incentive to participate. Survey response rates among physicians are generally low and rate as low as 3% are reported [Thomas et al. 2002]. Although overall response rate was low, we were still able to elicit views of 243 consultant psychiatrists, the largest number of respondents in such a study. In addition, we were not in a position to verify what clinicians felt were the reasons for clozapine underutilization. Although our respondents represented all of the major sectors of general adult psychiatry, there may be some limitations in the generalization of our findings given a low response rate. However, more likely than not, our findings reflect the perception and the practise of psychiatrists given the known variability in clozapine prescribing and utilization. Our findings also mirror and extend what has been observed previously [Nielsen et al. 2010; Gee et al. 2013].
Our main findings are as follows: the reasons for clozapine underutilization are multiple, however, a significant number were related to clinicians’ factors. Over half of the consultants worked in a trust that had a dedicated clozapine service, a significant number (42%) had less than five patients on clozapine despite being in the current post for about 7 years. About 80% agreed that there was a delay in starting clozapine. Three quarters of respondents agreed that they had good exposure in using clozapine as a trainee, but there appeared to be significant gaps in knowledge, e.g. about one fifth of respondents did not know that clozapine use is associated with reduced suicidality. Just over a third felt that it was not safe to start patients on clozapine in the community and the same proportion felt that they were unable to identify suitable patients for clozapine treatment and just over 40% preferred to use several other antipsychotics before considering clozapine.
Why there is a delay in using clozapine
This survey observed that clinicians are aware of the delayed use of clozapine and like previous studies, they are aware of its underutilization [Nielsen et al. 2010; Howes et al. 2012]. The cost does not seem to be a barrier now as clozapine has become generic with a significant cost reduction. However, the underutilization appears to have remained [Joober and Boksa, 2010; Farooq and Taylor, 2011].
Eleven factors were identified as important causes of delayed use of clozapine in this survey. The major concerns in the mind of psychiatrists were side effects including metabolic problems. This is understandable, as it appears that a significant number of respondents in this survey had observed serious side effects in their patients. Concerns about side effects of clozapine by clinicians have been highlighted previously as a significant reason for clozapine underutilization [Nielsen et al. 2010]. It is recognized that side effects are a common cause of all antipsychotics discontinuation [Davis et al. 2013]. Clozapine is known to have low extrapyramidal side effects including tardive dyskinesia and low tendency to elevate prolactin. However, it has a number of uncommon but life-threatening side effects such as agranulocytosis, myocarditis and cardiomyopathy. Overestimation of side effects, clinicians’ perception of them and lack of knowledge on how to manage them has been hypothesized as underlying reasons for clinicians’ hesitation in using clozapine [Patel, 2012; Nielsen et al. 2010]. However, with adequate resources and monitoring, a significant number of them can be identified early on and appropriate measures taken to minimize their impact [Young et al. 1998; Miller, 2000; Raja, 2011]. This is demonstrated by a significant change in the incidence of agranulocytosis from 1–2% in mid-1970s prior to blood monitoring to 0.38% after the introduction of monitoring [Honigfeld et al. 1998].
Reluctance to have blood test was the second commonest reason mentioned. The views of patients who refuse to accept clozapine treatment have not been captured systematically and may be different from those who subsequently go on to take clozapine. Interestingly, however, when asked about clozapine and the associated blood test requirement, patients on clozapine appears to have views that are contrary to psychiatrists’ concerns. A survey of patients on clozapine by Taylor and colleagues [Taylor et al. 2000] revealed that majority of patients (64%) on clozapine had a positive view of blood test and viewed it as part of their treatment. A small study that followed patients on clozapine for just over 8 years found that blood test accounted for only 21.4% of discontinuation despite high overall discontinuation rates [Krivoy et al. 2011]. It is also interesting to note that those taking clozapine have been repeatedly shown to have the longest period of medication adherence prior to discontinue their medication [Taylor et al. 2008; McEvoy et al. 2006; Rosenheck et al. 1997; Valenstein et al. 2004]. It may be more helpful in the future to involve patients already on clozapine as expert patients in educating service users who are candidates to start clozapine. Having evidence-based perspective should also help to alleviate the concerns of many clinicians.
Knowledge, attitudes and practice
Lack of knowledge or experience in using clozapine by psychiatrists was the third frequently mentioned reason. Lack of knowledge or experience has been highlighted earlier [Nielsen et al. 2010; Patel, 2012; Farooq and Taylor, 2011]. Despite the fact that a high proportion (75.4%) of our responders indicated that they had a good exposure in the use of clozapine during their training, a significant number of clinicians in our study had less than five patients on clozapine on their caseload. Psychiatrists’ perception was that functionalization has resulted in more service fragmentation. They felt as well that there was lack of community support. Taken together, all of these factors can result in increased ambivalence among clinicians, magnifying clozapine underutilization given the intense monitoring required and the extra work it generates [O’Brien, 2004; De Berardis et al. 2012; Marder and Van Putten, 1988]. Interestingly, we observed that psychiatrists, who worked in the acute wards or crisis and home treatment, the two important areas for clozapine initiation and support in the early phase, were more likely to have less than five patients on clozapine on their caseload.
Deficiency in knowledge in certain aspect of clozapine use was apparent is response to specific questions about clozapine. It is well known, for example, that the risk of agranulocytosis is highest in the first 6 months following clozapine initiation [Munro et al. 1999; Alphs and Anand, 1999; Nielsen et al. 2013], decreasing to levels similar to other antipsychotics after 1 year of treatment. Likewise clozapine is well established in reducing suicidality and substance abuse in patients suffering from schizophrenia. However, a significant proportion of psychiatrists had deficient knowledge in these aspects. Lack of clarity may have a significant implication when information is conveyed to patients and carers and in the choice of the next antipsychotic once two or more have failed.
The general reluctance of patients and families to start clozapine was another frequently mentioned reason. Psychiatrists pointed out about the importance of patient choice and the need for self-determination. However, this has been challenged given the effect of TRS on the patient outcomes and service utilization [Patel, 2012; Hermes and Rosenheck, 2012]. Conservative estimates indicate that TRS adds more than US$34 billion in annual direct medical costs in the USA [Kennedy et al. 2013]. It was observed in the phase II CATIE study that if left to patients and their clinicians only 31.2% of eligible patients were allocated to the clozapine treatment arm and most were men with severe symptoms and having increased service utilization [Hermes and Rosenheck, 2012]. A recent Report of the National Audit of Schizophrenia (NAS) in the UK [Royal College of Psychiatry, 2012] also noted that 43% of patient with TRS were not on clozapine and no reason was documented. Decision-making process in medicine is complex and several factors are involved on both parties including knowledge of the drug of interest, side effects and efficacy, experience, preference and values and the level of communication between clinician and the patient [Mistler and Drake, 2008]. The observation by Whiskey and colleagues [Whiskey et al. 2003] that clinicians with a long history of using clozapine had a large number of patients on clozapine and also had the lowest discontinuation rates is interesting and demands that clozapine service provision be re-examined again in the light of current mounting evidences. Our survey noted that negative views of other healthcare professionals might have undesirable influence on both the treating doctor and the patient.
Over a third of respondents felt that it was not easy to identify suitable patients to start clozapine despite the clear National Institute for Health and Care Excellence (NICE) guidelines on the subject. Previous studies have shown that clinicians are aware of the NICE guidance and the definition of treatment resistance [Nielsen et al. 2010]. However, despite this, consultants still seem to wants to try several antipsychotics before considering clozapine. Over 40% of respondents in our survey said they would do this before considering clozapine. A higher proportion (two thirds) was reported by Nielsen and colleagues [Nielsen et al. 2010].
Implications of the study
Out of the 11 identified possible reasons for delayed clozapine use, at least 7 if not more can be directly or indirectly attributed to psychiatrists’ knowledge, attitudes or local practices for starting clozapine. Following the introduction of clozapine, it was part of license agreement and mandatory for inpatient admission before clozapine was initiated. This is no longer a requirement; for example NICE (2014) guidelines do not recommend admission as a prerequisite for starting clozapine. Over the years through research observations and experiences, clozapine can be started safely in the community with the support of the community teams such as the HTT [O’Brien, 2004]. Frequent visits and the frequent monitoring of blood pressure, temperature and pulse at least twice daily in the community is seen as added burden given the limited resources and makes clozapine a less preferred drug [O’Brien, 2004]. It is appreciated that there will always be a need to start clozapine as inpatient in some patients especially where the risk of relapse is high when clozapine is being titrated, and where there is concern about physical health problems [De Berardis et al. 2012; Nielsen et al. 2013]. Over a third of clinicians either felt it was not safe to start clozapine in the community or did not know that they could do so. Evidence-based local protocols should be able to address this issue.
Having clozapine-dedicated services need to be seriously considered given the plight of patients with schizophrenia ‘a forgotten illness’ [The Schizophrenia Commission, 2012]. Lessons can be learnt from our medical colleagues who have specialists with specific experience or interest in dealing with specific conditions, e.g. diabetes (diabetologist) and rheumatic disease (rheumatologists). Services based on a similar model need to be considered to improve the uptake and early use of clozapine and possibly the outcome of TRS given the complexity of clozapine initiation and monitoring, the concerns about life-threatening side effects, the high attrition rate and the lack of best alternative when patients with TRS fail to use clozapine.
A major implication of the study is that the education needs of the practicing psychiatrists are identified and addressed. It is also interesting to know that over 63% of psychiatrist would welcome receiving more information on clozapine. Considering that increasingly psychiatric services in the UK are focused on the complex cases and work in subspecialty-type setting it is important that the educational needs for management of TRS becomes a priority both in training and continued professional development. Our study identifies some important areas, such as managing side effects, current evidence regarding use of clozapine and identification of treatment resistance at an early stage, which should be targeted in training and professional development programme by organizations such as the BAP (British Association of Psychopharmacology) and The Royal College of Psychiatrists.
Acknowledgments
We would like to thank BCPFT for approving this study, the faculty of the general adult and community psychiatry of the Royal College of Psychiatrists for allowing us to conduct this survey. We would like to thank all colleagues who took time from their busy timetable to respond to this survey.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: TET has attended meeting sponsored by Lilly and Otsuka. SF has received funding to attend meetings and honoraria from Novartis. No pharmaceutical companies had any role in designing or conducting this survey.
Contributor Information
Tongeji E. Tungaraza, Choice Lifestyles LTD, Birmingham B17 8LL, UK
Saeed Farooq, Black Country NHS Foundation Trust and Staffordshire University, UK.
Reference
- Agid O., Foussias G., Singh S., Remington G. (2010) Where to position clozapine: re-examining the evidence. Can J Psychiatry 55: 677– 684. [DOI] [PubMed] [Google Scholar]
- Alphs L., Anand R. (1999) Clozapine: the commitment to patient safety. J Clin Psychiatry 60(Suppl. 12): 39–42. [PubMed] [Google Scholar]
- Davis J., Chen N., Glick I. (2003) A meta-analysis of the efficacy of second- generation antipsychotics. Arch Gen Psychiatry 60: 553–564. [DOI] [PubMed] [Google Scholar]
- Davis M., Fuller M., Strauss M., Konicki P., Jaskiw G. (2013) Discontinuation of clozapine: a 15-year naturalistic retrospective study of 320 patients. Acta Psychiatr Scand. DOI: 10.1111/acps.12233. [DOI] [PubMed] [Google Scholar]
- De Berardis D., Serroni N., Campanella D., Olivieri L., Ferri F., Carano A., et al. (2012) Update on the adverse effects of clozapine: focus on myocarditis. Curr Drug Saf 7: 55–62. [DOI] [PubMed] [Google Scholar]
- Essali A., Al-Haj Haasan N., Li C., Rathbone J. (2009) Clozapine versus typical neuroleptic medication for schizophrenia. Cochrane Database Syst Rev 1: CD000059 DOI: 10.1002/14651858.CD000059.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq S., Taylor M. (2011) Clozapine: dangerous orphan or neglected friend? Br J Psychiatry 198: 247–249. [DOI] [PubMed] [Google Scholar]
- Gee S., Vergunst F., Howes O., Taylor D. (2013) Practitioner attitudes to clozapine initiation. Acta Psychiatr Scand. DOI: 10.1111/acps.12193. [DOI] [PubMed] [Google Scholar]
- Hermes E., Rosenheck R. (2012) Choice of randomization to clozapine versus other second generation antipsychotics in the CATIE schizophrenia trial. J Psychopharmacol 26: 1194–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honigfeld G., Arellano F., Seth Bianchini A., Schein J. (1998) Reducing clozapine-related morbidity and mortality: 5 years of experience with the Clozaril National Registry. J Clin Psychiatry 59(Suppl. 3): 3–7. [PubMed] [Google Scholar]
- Howes O., Vergunst F., Gee S., McGuire P., Kapur S., Taylor D. (2012) Adherence to treatment guidelines in clinical practice: study of antipsychotic treatment prior to clozapine initiation. Br J Psychiatry 1: 481–485. [DOI] [PubMed] [Google Scholar]
- Joober R., Boksa P. (2010) Clozapine: a distinct, poorly understood and under-used molecule. J Psychiatry Neurosci 35: 147–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane J., Honigfeld G., Singer J., Meltzer H. (1988) Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45: 789–796. [DOI] [PubMed] [Google Scholar]
- Kennedy J., Altar C., Taylor D., Degtiar I., Hornberger J. (2014) The social and economic burden of treatment-resistant schizophrenia: a systematic literature review. Int Clin Psychopharmacol 29: 63–76. [DOI] [PubMed] [Google Scholar]
- Killian J., Kerr K., Lawrence C., Celermajer D. (1999) Myocarditis and cardiomyopathy associated with clozapine. Lancet 354: 1841–1845. [DOI] [PubMed] [Google Scholar]
- Krivoy A., Malka L., Fischel T., Weizman A., Valevski A. (2011) Predictors of clozapine discontinuation in patients with schizophrenia. Int Clin Psychopharmacol 26: 311–315. [DOI] [PubMed] [Google Scholar]
- Kumlien E., Lundberg P. (2010) Seizure risk associated with neuroactive drugs: data from the WHO adverse drug reactions database. Seizure 19: 69–73. [DOI] [PubMed] [Google Scholar]
- Lewis S., Barnes T., Davies L., Murray R., Dunn G., Hayhurst K., et al. (2006) Randomized controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull 32: 715–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marder S., Van Putten T. (1988) Who should receive clozapine? Arch Gen Psychiatry 45: 865–867. [DOI] [PubMed] [Google Scholar]
- McEvoy J., Lieberman J., Stroup T. (2006) Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry 163: 600–610. [DOI] [PubMed] [Google Scholar]
- Miller D. (2000) Review and management of clozapine side effects. J Clin Psychiatry 61(Suppl. 8): 14–17. [PubMed] [Google Scholar]
- Mistler L., Drake R. (2008) Shared decision making in antipsychotic management. J Psychiatr Pract 14: 333–344. [DOI] [PubMed] [Google Scholar]
- Munro J., O’Sullivan D., Andrews C., Arana A., Mortimer A., Kerwin R. (1999) Active monitoring of 12,760 clozapine recipients in the UK and Ireland. Beyond pharmacovigilance. Br J Psychiatry 175: 576–580. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2014) Psychosis and Schizophrenia in Adults: Treatment and Management. CG178. London: National Institute for Health and Care Excellence. [Google Scholar]
- Nielsen J., Correll C., Manu P., Kane J. (2013) Termination of clozapine treatment due to medical reasons: when is it warranted and how can it be avoided? J Clin Psychiatry 74: 603–613. [DOI] [PubMed] [Google Scholar]
- Nielsen J., Dahm M., Lublin H., Taylor D., et al. (2010) Psychiatrists’ attitude towards and knowledge of clozapine treatment. J Psychopharmacol 24: 965–971 [DOI] [PubMed] [Google Scholar]
- O’Brien A. (2004) Starting clozapine in the community: a UK perspective. CNS Drugs 18: 845–852. [DOI] [PubMed] [Google Scholar]
- Paranthaman R., Baldwin R. (2006) Survey of clozapine use by consultant old age psychiatrists. Psychiatric Bull 30: 410–412. [Google Scholar]
- Patel M. (2012) Clinician hesitation prior to clozapine initiation: is it justifiable? Br J Psychiatry 201: 425–427. [DOI] [PubMed] [Google Scholar]
- Raja M. (2011) Clozapine safety, 35 years later. Curr Drug Saf 6: 164–184. [DOI] [PubMed] [Google Scholar]
- Rosenheck R., Cramer J., Xu W. (1997) Comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. N Engl J Med. 337:809–815. [DOI] [PubMed] [Google Scholar]
- Royal College of Psychiatrists (2012) Report of the National Audit of Schizophrenia (NAS) 2012. London: Healthcare Quality Improvement Partnership. [Google Scholar]
- Safferman A., Lieberman J., Kane J., Szymanski S., Kinon B. (1991) Update on the clinical efficacy and side effects of clozapine. Schizophr Bull 17: 247–261. [DOI] [PubMed] [Google Scholar]
- Taylor D., Shapland L., Laverick G., et al. (2000) Clozapine - a survey of patient perceptions. Psychiatric Bull 24: 450–452. [Google Scholar]
- Taylor D., Young C., Paton C. (2003) Prior antipsychotic prescribing in patients currently receiving clozapine: a case note review. J Clin Psychiatry 64: 30–34. [DOI] [PubMed] [Google Scholar]
- Taylor M., Shajahan P., Lawrie S. (2008) Comparing the use and discontinuation of antipsychotics in clinical practice: an observational study. J Clin Psychiatry 69: 240–245. [DOI] [PubMed] [Google Scholar]
- The Schizophrenia Commission (2012) The Abandoned Illness: A Report from the Schizophrenia Commission. London: Rethink Mental Illness. [Google Scholar]
- Thomas M., Rogers R., Maclean R. (2002) Collecting data from physicians via Web-based surveys: recommendations for improving response rates. Internet J Med Informat 1: N1. [Google Scholar]
- Valenstein M., Blow F., Copeland L., McCarthy J., Zeber J., Gillon L., et al. (2004) Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophr Bull 30: 255–264. [DOI] [PubMed] [Google Scholar]
- Wahlbeck K., Cheine M., Essali A., Adams C. (1999) Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 156: 990–999. [DOI] [PubMed] [Google Scholar]
- Weissman E. (2002). Antipsychotic prescribing practices in the Veterans Healthcare Administration—New York metropolitan region. Schizophr Bull 28: 31–42. [DOI] [PubMed] [Google Scholar]
- Wheeler A. (2008) Treatment pathway and patterns of clozapine prescribing for schizophrenia in New Zealand. Ann Pharmacother 42: 852–860. [DOI] [PubMed] [Google Scholar]
- Whiskey E., Wykes T., Duncan-McConnell D., Haworth E., Walsh N., Hastilow S. (2003) Continuation of clozapine treatment: practice makes perfect. Psychiatric Bull 27: 211–213. [Google Scholar]
- Young C., Bowers M., Jr, Mazure C. (1998) Management of the adverse effects of clozapine. Schizophr Bull 24: 381–390. [DOI] [PubMed] [Google Scholar]