Abstract
Introduction
People with chronic epilepsy (PWE) often make costly but clinically unnecessary emergency department (ED) visits. Offering them and their carers a self-management intervention that improves confidence and ability to manage seizures may lead to fewer visits. As no such intervention currently exists, we describe a project to develop and pilot one.
Methods and analysis
To develop the intervention, an existing group-based seizure management course that has been offered by the Epilepsy Society within the voluntary sector to a broader audience will be adapted. Feedback from PWE, carers and representatives from the main groups caring for PWE will help refine the course so that it addresses the needs of ED attendees. Its behaviour change potential will also be optimised. A pilot randomised controlled trial will then be completed. 80 PWE aged ≥16 who have visited the ED in the prior 12 months on ≥2 occasions, along with one of their family members or friends, will be recruited from three NHS EDs. Dyads will be randomised to receive the intervention or treatment as usual alone. The proposed primary outcome is ED use in the 12 months following randomisation. For the pilot, this will be measured using routine hospital data. Secondary outcomes will be measured by patients and carers completing questionnaires 3, 6 and 12 months postrandomisation. Rates of recruitment, retention and unblinding will be calculated, along with the ED event rate in the control group and an estimate of the intervention's effect on the outcome measures.
Ethics and dissemination
Ethical approval: NRES Committee North West—Liverpool East (Reference number 15/NW/0225). The project's findings will provide robust evidence on the acceptability of seizure management training and on the optimal design of a future definitive trial. The findings will be published in peer-reviewed journals and presented at conferences.
Trial registration number
ISRCTN13 871 327.
Keywords: ACCIDENT & EMERGENCY MEDICINE, EDUCATION & TRAINING (see Medical Education & Training), QUALITATIVE RESEARCH, REHABILITATION MEDICINE, THERAPEUTICS
Strengths and limitations of this study.
This will be the first study to develop and pilot seizure first aid training for people with epilepsy who frequently visit hospital emergency departments (EDs), and their carers.
The intervention will be developed so that it closely aligns with service users' needs and preferences in order to maximise its acceptability and benefit.
Its method of delivery and low cost could mean it holds the potential to be generalisable across the health service and sustainable.
The follow-up period in the pilot randomised controlled trial will be 1 year and the data on the primary outcome measure, namely subsequent ED use, will be collected using objective hospital data.
We expect that the pilot will provide robust estimates to inform the optimal design of a future definitive trial.
Introduction
Emergency hospital use for epilepsy
With a prevalence of up to 1%,1 epilepsy is one of the most common brain disorders in the UK.2 As well as having significant implications for the lives of patients,3 epilepsy also has important societal impacts.4 5 Studies show that one of these is the cost of providing emergency care.6–8
In the UK, one fifth of people with epilepsy (PWE) visit hospital emergency departments (ED) each year for seizures,6–8 with rates being highest in socially deprived areas.9 10 In England in 2012/2013, the cost of providing emergency care for epilepsy was >£56 million.11 One reason it is so high is because half of the PWE visiting EDs are admitted to hospital;8 12–14 indeed, 85% of admissions for epilepsy occur on this unplanned basis.15 Readmissions further drive costs up;16 ≥60% of PWE reattend ED within 12 months.17
Seeking emergency care for epilepsy can be important, even life-saving. However, most ED visits by PWE are clinically unnecessary. The UK-wide National Audits of Seizure Management in Hospitals (NASH)18 19 found that most visits were by people with known rather than new epilepsy and most had experienced uncomplicated seizures. Guidelines are clear that, with the correct training, such seizures can be safely managed by patients and their families within the community.20–22 Factors beyond clinical need have been identified as often being important in determining whether an emergency admission occurs, which most likely explains why so many visits to the ED by people in whom the diagnosis is clear and who have made a full recovery still end in hospital admission.8 23
Reducing unnecessary emergency visits to hospital by PWE has been identified as one way that resource-limited health services can generate savings.24 Reducing emergency visits is also important for service users. ED visits can be inconvenient, distressing and do not typically lead to extra support.12 There may even be iatrogenic harm, such as that associated with unnecessary intravenous cannulations.25
Reasons for emergency hospital use
It has been challenging to know how to reduce emergency visits for epilepsy,26 not least because the reason/s for them were unclear. The association between seizure frequency and ED use had, for example, been found to only be modest in size and seizure type had not proved a robust predictor.6 27–29
However, a recent mixed-methods study has brought clarity to the issue.11 It suggests that what is often key in determining whether someone visits the ED for seizures is not necessarily clinical need, but confidence in seizure management.30 31 Eighty-five adults with epilepsy were prospectively recruited from UK EDs and interviewed. Patients fell into two groups. In the first, there were patients who reported high levels of confidence. Their views closely aligned with seizure first aid guidelines. They had typically visited the ED only once in the previous 12 months.
In contrast, patients in the second group did not feel confident managing seizures and had typically made ≥2 ED visits in the prior year. They feared seizures, including the possibility of death. This led them to call for an ambulance when they believed they were about to have, or had had, a seizure. Despite having diagnosed epilepsy for ∼10 years, they said they had not received sufficient information about epilepsy.
Quantitative results from the project reinforced what patients said. Regression analyses identified that it was a patient's score on a measure of perceived ‘mastery’ over their epilepsy which significantly predicted how many ED visits they made over the subsequent 12-months rather than seizure frequency.29 There was also evidence of poor first aid knowledge. One third of the sample incorrectly stated that it was always necessary to call a doctor or ambulance if a person with epilepsy has a seizure, even if it occurs without complications.17 Only 11% of the wider epilepsy population believe this (S Jarvie. Self perception and psychosocial functioning in people with intractable epilepsy [PhD thesis, Unpublished data]. University of Glasgow, 1993).
The above findings are in keeping with prior evidence. Coping with life in the context of epilepsy requires PWE to learn and adopt specific self-management behaviours to prevent seizures and manage consequences. It is known, however, that PWE typically receive little support from health services in learning to self-manage.32–35 One consequence is that knowledge about epilepsy among patients can be poor, especially in those with low education.36 37
Another important finding from the interviews conducted for the project was that when seizures occurred, responsibility for patient care and the decision to seek emergency care could be delegated to family or friends. When these persons were confident in seizure management and been correctly informed, the patient would visit the ED only under certain circumstances. However, when they were not, they would often seek emergency medical care, regardless of clinical need: One said, “[I was] just worried because I don't know anything about epilepsy… I mean I only know the bad things, I know it can be quite serious… I know you can die… I was so worried I decided just to ring an ambulance…better safe than sorry.”30 This accords with evidence that most seizures leading to the ED appear to occur within patients’ homes and are often witnessed.13 38
Need for seizure first aid training
On the basis of the evidence presented, PWE who frequently visit the ED might benefit from a self-management intervention that improves their own and their informal carers’ confidence and ability in managing seizures and empowers them to be able to tell others from their wider support network about first aid.
No epilepsy self-management intervention is available which focuses on seizure management, or on those attending the ED, and none systematically involves carers.39–41 That such an intervention might improve seizure management skills is, however, supported by the broader literature. Studies on general first aid show that even brief interventions can improve skills in a variety of groups.42–46 Evidence from asthma studies is also important.47–49 Boyd et al47 reviewed 17 randomised controlled trials (RCT) of educational interventions for children (and parents) at risk of asthma-related ED attendances. The interventions led to a 37% reduction in the relative risk of reattendance at the ED and a 21% reduction in subsequent hospital admissions.
Aims
We describe here a project to develop and then pilot a seizure first aid training intervention for PWE who frequently visit the ED and their carers (protocol V.1.1, 31/3/15). This project will be completed in the Merseyside area of North-West England.
Rather than creating an entirely new intervention, it will be developed by adapting a promising seizure management course that already exists to address the needs of PWE visiting the ED. The course titled ‘Epilepsy awareness and seizure management’ has been offered on a small scale within the third sector to people from a variety of backgrounds, including patients, teachers and care home staff by the UK charity, Epilepsy Society. The society has offered the course since 1998 and given us permission to adapt it. It has not been formally evaluated, but aims to increase participants’ confidence in seizure management.
Changes to the existing course will be required since it was developed for delivery to a narrower, fee-paying group. It was not created for delivery within the health service, nor for PWE who visit EDs who can be particularly challenged by epilepsy and may have lower education.9 17 27 36 37 Once adapted, a pilot RCT shall be completed. A pilot is required to address uncertainties about the optimal design of a full RCT.50 These include intervention acceptability, likely effect, as well as participant uptake and retention.
Accordingly, the project's objectives are to:
Optimise the content, delivery and behaviour change potential of the existing course for PWE attending the ED, and their informal carers. The resulting adapted package will be named Seizure First Aid Training.
Conduct a pilot RCT of Seizure First Aid Training versus Treatment As Usual (TAU) alone to estimate likely recruitment, consent and follow-up rates in a future definitive trial.
Test acceptability of randomisation to participants.
Calculate estimates of the annual rate of ED visits in the control group and the likely dispersion parameter to inform the sample size calculation of a future RCT.
Conduct an analysis of the cost of implementing the Seizure First Aid Training programme.
Methods and analysis
Part A: Intervention development (months 1–8)
Design
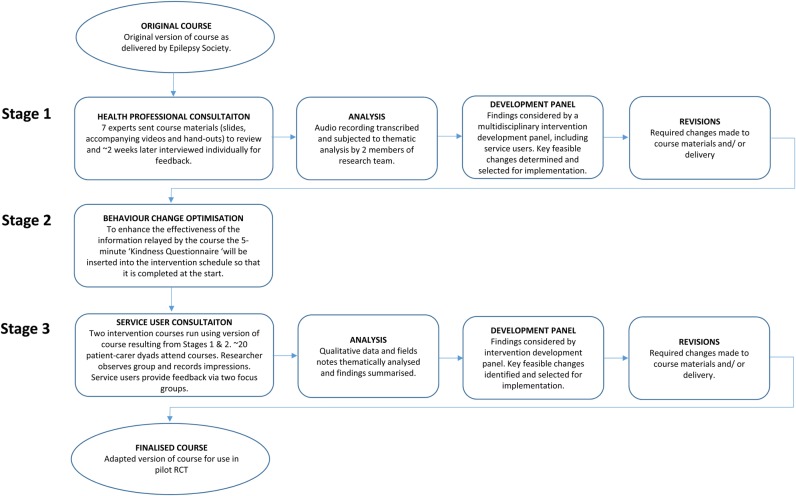
To adapt the existing course, three stages will be completed (figure 1).
Figure 1.
Intervention development process.
Stage 1: Consultation with main professional groups
Leading representatives from the professional groups supporting PWE will review the course materials and be interviewed. Consensus exists on seizure first aid22 and so, where expertise permits, representatives will be asked to identify changes needed to ensure accuracy, as well as suggestions for improvement.
Stage 2: Optimisation of behaviour change potential
A significant component of the intervention consists of providing information about epilepsy, its manifestations and first aid. This will highlight to some participants that their past behaviour conflicts with medical guidance. This could be construed as a threat to self-integrity.51–53 Self-Affirmation theory states that people are motivated to maintain self-integrity.53 Accordingly, threats to the self can be defensively processed (eg, motivated scepticism, unrealistic optimism). To mitigate against this, Reed and Aspinwall's self-affirmation54 ‘Kindness Questionnaire’ will be inserted to the beginning of the intervention. Completing such an exercise is known to reduce resistance to threatening or dissonant information and increase behaviour change.55 56
Stage 3: Consultation with service user representatives
Health professionals and PWE may have different views of support needed.57 For this reason, two courses using the initial adaptation of the course will be run with patient-carer dyads and focus groups will explore users’ views of the intervention, its content, the facilitator, scheduling and acceptability.
Participants
For Stage 1, representatives from neurology, emergency medicine, the ambulance service, nursing, general practice, user groups and health care commissioning based within the UK have been identified, approached and will be asked to provide informed consent. For Stage 3, user groups within the Merseyside area will help identify and recruit dyads. PWE will be eligible to participate if they are aged ≥16 and have visited ED in the past 2 years. The full inclusion/exclusion criteria are in table 1.
Table 1.
Participant inclusion and exclusion criteria
| Study part | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Part A—Intervention development | ||
| Patients |
|
|
| Carers |
|
|
| Part B—Pilot RCT | ||
| Patients |
|
|
| Carers |
|
|
While efforts will be made to maximise the recruitment of patient-carer dyads, patient participants will be permitted to take part without a carer. Carers will not, however, be able to take part in this part of the project without a patient partner having at least consented to take part in the study. Up to 90% of PWE can identify an informal carer.58
ED, emergency department PWE, people with chronic epilepsy; RCT, randomised controlled trial.
Intervention in its current form
The existing course lasts 3 h. It is delivered to groups of 10–20 people by an educational facilitator. It covers eight topics (table 2) and emphasises how most seizures are self-limiting. It seeks to provide participants with a practical understanding of when seizures do, and do not, require emergency treatment.
Table 2.
Topics covered by existing version of a seizure first aid training course
| Topic | Details |
|---|---|
| 1. | What is epilepsy? Myths and truths about epilepsy are discussed, and a simple explanation is provided of what happens in the brain to produce seizures |
| 2. | Different causes of epilepsy and seizure triggers |
| 3. | Diagnosis: important diagnostic tools are discussed |
| 4. | Detailed discussion of seizure types, their effects, and how to manage each of them, including when to call an ambulance and demonstration of the recovery position. This includes video clips showing different types of seizures, with PWE and health professionals discussing them |
| 5. | Status epilepticus |
| 6. | Treatments: medication and side effects |
| 7. | Risk management and support needs |
| 8. | Sources of further information: addresses of organisations offering assistance and information |
Course materials include standardised slides, videos and an information pack. The pack provides participants with a permanent record, as well as space for notes to promote active processing. Participants are encouraged to share experiences and ask questions. The course consists of a number of components and so is a complex intervention.50
Facilitators typically have a nursing or social care background, experience of working with PWE and follow a local Epilepsy Society training programme in order to deliver the course.
As well as holding the potential to increase seizure management confidence and lead to fewer unnecessary ED visits, further justification for adapting this particular course is that its delivery method could be generalisable. Specialist epilepsy nurses and physiologists have been asked to deliver broader self-management interventions.39 59 Such staff are, however, not widely available.8 60 61 The epilepsy voluntary sector is particularly well developed,26 62 63 and so commissioning third sector organisations to deliver seizure-management training could help avoid shortfalls. The Epilepsy Society, for example, currently has a bank of 12 educational facilitators located around England able to deliver its courses, and it already has a role in providing information materials for hospital clinics. The model could also be financially sustainable, with the Epilepsy Society charging only £40 to attend its course.
Another reason for adapting this particular course is that its content and format broadly align with service users’ preferences, thus increasing its likely acceptability. Studies show that PWE tend to want short, face-to-face self-management courses, and for them to be delivered by persons with knowledge or experience of epilepsy.64–68
Part B: Pilot RCT (months 9–38)
Design
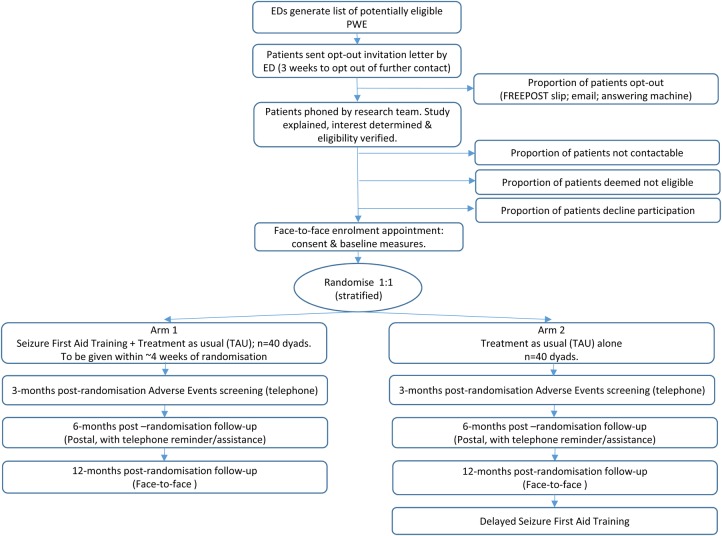
Using the adapted seizure management course, a multicentre, external pilot RCT will be completed with PWE aged ≥16 years who have visited the ED in the prior 12 months for epilepsy on ≥2 occasions, along with one of their family members or friends who have an informal caring role. Patients and carers will be followed up for 12 months. The participants and data flow in the study are shown in figure 2.
Figure 2.
Design of the pilot trial phase of the project. ED, emergency department PWE, people with chronic epilepsy.
Participants
The EDs of three Merseyside NHS hospitals have been recruited to identify potential participants. They serve a population of ∼830 000 people, within which the prevalence of adult epilepsy is 0.98%.69 This population features high levels of social deprivation70 71 and rates of emergency admissions for epilepsy that are among the highest.9
To identify eligible patients, the EDs will complete searches of their electronic attendance records for persons with a presentation/discharge code in the prior 12 months that is indicative of epilepsy. The eligibility criteria are provided by table 2.
Invitation letters from the local consultant will be sent to all ostensibly eligible patients. Those not opting out of further contact within 3 weeks will be phoned by the research team which will confirm interest, verify eligibility and, if applicable, arrange an initial meeting. At that meeting, consent will be obtained and baseline data collected from the patient and their nominated family member or friend.
Randomisation and concealment
Computer-generated randomisation of patient-carer dyads will be completed remotely by the Clinical Trials Research Centre (CTU) at the University of Liverpool following consent and completion of the baseline measures. The unit of randomisation will be the individual participant and randomisation will be 1:1 between the intervention and the control groups, stratified by factors which at this stage will not be disclosed to prevent treatment prediction.
The results of the allocation will be concealed from the trial statistician and researchers responsible for consent and data collection. A study administrator will liaise with patients (and carers) to arrange attendance at the intervention. Participants will be asked not to inform the research team of their treatment allocation and we shall test the success of blinding.
Interventions
Intervention arm: seizure first aid training (+TAU)
The intervention's exact content will be determined in Part A of the project. It is anticipated, however, that it will continue to last ∼3 h, with no additional booster sessions, and be delivered to groups of ∼10 patient-carer dyads by local Epilepsy Society educational facilitators. Courses will be delivered within educational rooms at the local hospitals from where recruitment occurred. Both patients and carers will be expected to participate actively in the course. Participants will each be provided with an information pack. These will include copies of the course material, certificates of attendance, epilepsy identification cards, wallet sized first aid instruction cards and contact details for further information.
Control arm: TAU only
The active intervention will be compared to TAU alone by the PWE's normal care team. No restrictions will be placed on the services TAU participants can access.
In the UK, there is no accepted care for those with established epilepsy who have visited an ED.26 All PWE are, however, expected to have a medical review of their epilepsy at least yearly by a generalist or specialist. When seizures are not controlled or treatment fails, it is expected that a patient will be referred to secondary or tertiary services.26 The UK's NASH showed that EDs initiate referral to neurology for only a third of PWE attending the ED.18 19
Delayed access to the Seizure First Aid Training for control participants is being used as a recruitment/retention incentive. These courses will be run once all retained patient and carer participants from both arms have completed their final follow-up assessments. The TAU group will only contribute outcomes to the trial data set under the TAU condition.
Outcomes and outcome measures
Primary
The proposed primary outcome measure for a future definitive trial is the number of epilepsy-related ED visits made over the 12 months following randomisation by patient participants. This will be measured in the pilot using routinely collected hospital data. The NHS’s Hospital Episode Statistics system provides a record of an individual's use of all EDs in England and data will be extracted from it to provide information on individual participants’ use of the ED at baseline and over follow-up. While this system is increasing in sophistication, it does not currently have a code to indicate visits related specifically to epilepsy. However, in order to increase specificity and provide a more reasonable estimate of such visits, we shall utilise a broader code that does exist within the system so as to identify only visits related to a central nervous system condition (excluding stroke).
Secondary
Over the course of the trial, patient and carer participants will be required to each complete three sets of questionnaires (table 3) either in a face-to-face interview with a research worker (at baseline and at 12-month follow-up) or through the post (at 6-month follow-up). To encourage continued participation, we will offer each participant a £10 voucher on completion of each assessment.86
Table 3.
Self-reported secondary outcome measures by assessment and participant type
| Outcome | Participants | Measure | Items (n) | Baseline | 6-month | 12-month |
|---|---|---|---|---|---|---|
| Knowledge and fear of seizures | Patients; carers | Epilepsy Knowledge and Management Questionnaire—Fears subscale72 | 5 | ✓ | – | ✓ |
| Knowledge of what to do when faced with a seizure | Patients; carers | Items from Thinking About Epilepsy Questionnaire73 | 3 | ✓ | – | ✓ |
| Confidence managing seizures/epilepsy | Patients; carers | Epilepsy Mastery Scale74 (P); Parents Response to Child Illness Scale—Condition Management subscale75(C) | 6 | ✓ | ✓ | ✓ |
| Quality of life | Patients | Quality of Life in Epilepsy Scale-3176 | 31 | ✓ | ✓ | ✓ |
| Distress | Patients; carers | Hospital Anxiety and Depression Scale77 | 14 | ✓ | – | ✓ |
| Seizure control | Patients | At baseline, Thapar's Seizure Frequency Scale for the prior 12 months.78At follow-up, patients will be asked for number of seizures (of any type) since the last assessment and dates of the first and most recent* | 1 | ✓ | ✓ | ✓ |
| Felt Stigma | Patients; carers | Stigma of Epilepsy Scale79 80 | 3 | ✓ | – | ✓ |
| Burden | Carers | Zarit Caregiver Burden Inventory81 | 22 | ✓ | ✓ | ✓ |
| Activation | Patients; carers | Patient Activation Measure82 | 13 | ✓ | – | ✓ |
| Health economics | Patients | Client Service Receipt Inventory83 and EQ-5D 84 | 13 | ✓ | – | ✓ |
| Feedback on trial participation | Patients; carers | Adapted from Magpie Trial85 | 3 | – | – | ✓ |
*To assist patients to be able to provide this information, they will be offered a seizure diary at their baseline appointment.
Secondary measures will be based on participant self-report and be used to help estimate whether the intervention leads to changes including improved quality of life, confidence managing seizures, knowledge of seizure first aid, as well as reductions in fear of seizures. Patient participants will also be asked to self-report on their service use, including of ED and ambulances. A full list of the measures to be used is provided in table 3.
Participants will be requested to complete the measures prior to randomisation and then 6 and 12 months postrandomisation. Baseline and 12 month follow-up measures will be collected in face-to-face sessions by a research worker, blind to treatment allocation. Estimated completion time is 1 h. An abbreviated assessment will occur at 6 months. For it, participants will be posted a set of questionnaires for completion.
Statistical analysis
Since this is a pilot RCT, a formal power calculation is not appropriate; the study will not be powered to detect a clinically meaningful difference in the primary outcome between the treatment groups. Rather, we aim to generate the following: estimates of eligibility, consent, recruitment and retention rates and speed of recruitment; and estimates of completion rates of study assessment tools and rates of unblinding. To accurately inform a sample size calculation for a future definitive trial, estimates of the ED event rate and dispersion parameter will also be provided, along with summary statistics measuring the effect of the intervention on the primary and secondary outcome measures and the precision of such estimates.
Forty patients in each treatment arm will provide the above estimates with adequate precision. In particular, with a sample size of 80, we will be able to estimate an overall dropout rate of 25% (approximate rate experienced by similar studies11 39 40) to within a 95% CI of ±10% and a participation rate of 20% from an assumed 400 patients to within a 95% CI of ±4%. Assuming that the ED data at 12 months is not available for 25% of patients, outcome data from 60 patients would still allow robust estimation of the ED rate and dispersion parameter.87 88
Minimising bias
PWE will attend the course outside of their routine clinic appointments and we do not expect transfer of intervention-related knowledge (and therefore contamination of the TAU group) between those in the intervention and control arms at a single site. Bias will be further minimised by restricting access to and availability of the intervention materials. When participants are asked to self-report on their service use, we shall also ask those in the control group whether they accessed any elements of the intervention.
Discussion
Ethics and oversight
Monitoring by an independent Study Steering Committee (SSC) will help to ensure that the rights, safety and well-being of the participants are the most important considerations. Compliance with Good Clinical Practice and scientific integrity will be managed by the study management team through regular and ad hoc meetings. Guidelines from the project's funder indicates that a Data Monitoring and Ethics Committee is not required (http://www.nets.nihr.ac.uk/__data/assets/…/ssc-and-dmec-checklist-june13.doc).
Patients’ experience of unexpected serious adverse events (SAE) within the trial phase will be monitored by asking them to complete a standardised SAE checklist. Patients will be asked to complete it by phone at 3 and 6 months postrandomisation, and in person at the 12-month follow-up appointment. A neurologist will assess unexpected SAEs, and the approving ethics committee and sponsor will be informed within 15 days of any SAEs that are judged to be related to participation. Given the population, the following will not be deemed as unexpected SAEs: epileptic seizures with or without injury; visits to the ED where the stay lasts <24 h; side effects of antiepileptic medication; or diagnosis of a comorbid psychiatric condition.
For the trial phase, the CTU will provide regular reports on data quality to ensure the integrity of randomisation, to monitor the level of missing data and the timeliness of data entry and to check for illogical or inconsistent data. Data collection procedures will be monitored and source data verification against the paper data collection forms undertaken at regular intervals.
Recruitment for studies involving serial assessments can be low. Owing to the social impact of epilepsy and its comorbidity, recruitment of PWE can also be challenging.89 For the project, only patients and carers providing signed, informed consent will be able to participate. However, to maximise uptake, we shall utilise an ‘opt out’ method of inviting patients, rather than the traditional ‘opt in’ approach. Specifically, a letter, signed by the ED consultant, will be sent to all ostensibly eligible individuals explaining the study and inviting them to participate. Persons will be informed that unless they opt out (by email, telephone or using a FREEPOST response slip) within 3 weeks, it will be taken that they are interested in being telephoned by the research team with further information.
The approach is ethically justifiable.90 It significantly increases participation rates,91 reduces the likelihood of a biased sample of participants being recruited,92 and is more cost-effective compared to an ‘opt in’ approach.93 We are currently using a version of the opt-out approach for another trial with PWE and the approach has proved largely acceptable.59
Dissemination
Despite the demonstrated need, there has been inadequate attention given to implementing and evaluating interventions to increase seizure management confidence in PWE who visit ED and their informal carers. We have described a study that will develop such an intervention for use within the UK health service. The trial phase aims to provide design information for a future definitive trial and quantitative estimates of the impact of the intervention on patients in terms of its clinical and cost-effectiveness. We will use the findings to inform the development of a future definitive RCT, with the ultimate goal of reducing clinically unnecessary ED use and improving the well-being of PWE who visit ED and their carers.
Acknowledgments
The authors would like to thank the Epilepsy Society for the role that they will have in this project and NHS England for their support with the trial phase. They would like to express appreciation for the contributions from people with epilepsy and their family members and friends who will participate in this study. The study sponsor is the University of Liverpool (reference: UoL001108; sponsor@liv.ac.uk).
Footnotes
Contributors: AJN and LR conceived of the study and designed it together with AGM, CT-S, DH, MM and SG. CT-S planned the statistical analysis. AJN wrote the manuscript, with revisions being made by LR, AGM, CT-S, DAH, MM and SG. All authors read and approved the final manuscript.
Funding: This project is being funded by the National Institute for Health Research's Health Services and Delivery Research (HS&DR) Programme (project number 14/19/09). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the University of Liverpool, the HS&DR programme, the NIHR, the NHS or the Department of Health.
Competing interests: None declared.
Ethics approval: NRES Committee North West—Liverpool East, reference number 15/NW/0225.
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
Data sharing statement: No additional data are available.
Study status: The study is currently in the intervention development phase. The results of the project will be available in 2018.
References
- 1.Ridsdale L, Charlton J, Ashworth M et al. . Epilepsy mortality and risk factors for death in epilepsy: a population-based study. Br J Gen Pract 2011;61:e271–8. 10.3399/bjgp11X572463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacDonald BK, Cockerell OC, Sander JW et al. . The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain 2000;123:665–76. 10.1093/brain/123.4.665 [DOI] [PubMed] [Google Scholar]
- 3. ILAE/IBE/WHO Global Campaign Against Epilepsy (2010). Epilepsy in the WHO European region: Fostering epilepsy care in Europe. Stichting Epilepsie Instellingen: Hoofddorp. [Google Scholar]
- 4.Organization WH. The global burden of disease: 2004 Update. Geneva: WHO, 2008. [Google Scholar]
- 5.Pugliatti M, Beghi E, Forsgren L et al. . Estimating the cost of epilepsy in Europe: a review with economic modeling. Epilepsia 2007;48:2224–33. [DOI] [PubMed] [Google Scholar]
- 6.Jacoby A, Buck D, Baker G et al. . Uptake and costs of care for epilepsy: findings from a U.K. regional study. Epilepsia 1998;39:776–86. 10.1111/j.1528-1157.1998.tb01164.x [DOI] [PubMed] [Google Scholar]
- 7.Hart YM, Shorvon SD. The nature of epilepsy in the general population. II. Medical care. Epilepsy Res 1995;21:51–8. 10.1016/0920-1211(95)00008-X [DOI] [PubMed] [Google Scholar]
- 8.Kitson A, Shorvon S. Clinical Standards Advisory Group. Services for patients with epilepsy: a report of a CSAG Committee. London: Department of Health, 2000. [Google Scholar]
- 9. NHS Right Care. The NHS atlas of variation in healthcare. 2010. www.rightcare.nhs.uk/atlas/qipp_nhsAtlas-LOW_261110c.pdf. [DOI] [PubMed]
- 10.Shohet C, Yelloly J, Bingham P et al. . The association between the quality of epilepsy management in primary care, general practice population deprivation status and epilepsy-related emergency hospitalisations. Seizure 2007;16:351–5. 10.1016/j.seizure.2007.02.005 [DOI] [PubMed] [Google Scholar]
- 11.Ridsdale L, McCrone P, Morgan M et al. . Can an epilepsy nurse specialist-led self-management intervention reduce attendance at emergency departments and promote well-being for people with severe epilepsy? A non-randomised trial with a nested qualitative phase. Health Services and Delivery Research; 2013;1 10.3310/hsdr01090 [DOI] [PubMed] [Google Scholar]
- 12.Dixon PA, Kirkham JJ, Marson AG et al. . National Audit of Seizure management in Hospitals (NASH): results of the national audit of adult epilepsy in the UK. BMJ Open 2015;5:e007325 10.1136/bmjopen-2014-007325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reuber M, Hattingh L, Goulding PJ. Epileptological emergencies in accident and emergency: a survey at St James's university hospital, Leeds. Seizure 2000;9:216–20. 10.1053/seiz.2000.0386 [DOI] [PubMed] [Google Scholar]
- 14.Ryan J, Nash S, Lyndon J. Epilepsy in the accident and emergency department—developing a code of safe practice for adult patients. South East and South West Thames Accident and Emergency Specialty Sub-committees. J Accid Emerg Med 1998;15:237–43. 10.1136/emj.15.4.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruce M, Griffiths C, Brock A. Trends in mortality and hospital admissions associated with epilepsy in England and Wales during the 1990s. Health Stat Q 2004;21:23–9. [PubMed] [Google Scholar]
- 16.Whiston S, Coyle B, Chappel D. Health needs assessment for long term neurological conditions in North East England. Stockton on Tees: North East Public Health Observatory, 2009. [Google Scholar]
- 17.Noble AJ, Goldstein LH, Seed P et al. . Characteristics of people with epilepsy who attend emergency departments: prospective study of metropolitan hospital attendees. Epilepsia 2012;53:1820–8. 10.1111/j.1528-1167.2012.03586.x [DOI] [PubMed] [Google Scholar]
- 18.Pearson M, Marson T, Dixon P et al. . National Audit of Seizure Management in Hospitals: St Elsewhere's Clinical Report. 2012.
- 19.Pearson M, Marson T, Dixon P et al. . National Audit of Seizure Management in Hospitals: St Elsewhere's Clinical Report. 2014.
- 20.National Society for Epilepsy. When to dial 999. Secondary When to dial 999 2012. http://www.epilepsysociety.org.uk/AboutEpilepsy/Firstaid/Whentodial999
- 21.British Epilepsy Association. What to do when someone has a seizure. Secondary What to do when someone has a seizure 2013. https://www.epilepsy.org.uk/info/firstaid
- 22.NHS Choices. What to do if someone has a seizure (fit). Secondary What to do if someone has a seizure (fit) 2013. http://www.nhs.uk/Livewell/Epilepsy/Pages/Ifyouseeaseizure.aspx
- 23.O'Cathain A, Knowles E, Turner J et al. . Explaining variation in emergency admissions: a mixed-methods study of emergency and urgent care systems. Health Serv Del Res 2014;2(48). [PubMed] [Google Scholar]
- 24. Department of Health. The NHS Outcomes Framework 2013/14. 2012. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213055/121109-NHS-Outcomes-Framework-2013-14.pdf.
- 25.Limm EI, Fang X, Dendle C et al. . Half of all peripheral intravenous lines in an Australian tertiary emergency department are unused: pain with no gain? Ann Emerg Med 2013;62:521–5. 10.1016/j.annemergmed.2013.02.022 [DOI] [PubMed] [Google Scholar]
- 26.National Institute for Health and Care Excellence. The epilepsies: the diagnosis and management of the epilepsies in adults and children in primary and secondary care. NICE clinical guideline 137, 2012.
- 27.Bautista RE, Glen ET, Wludyka PS et al. . Factors associated with utilization of healthcare resources among epilepsy patients. Epilepsy Res 2008;79:120–9. 10.1016/j.eplepsyres.2008.01.003 [DOI] [PubMed] [Google Scholar]
- 28.Cramer JA, Blum D, Fanning K et al. . The impact of comorbid depression on health resource utilization in a community sample of people with epilepsy. Epilepsy Behav 2004;5:337–42. 10.1016/j.yebeh.2004.01.010 [DOI] [PubMed] [Google Scholar]
- 29.Noble AJ, McCrone P, Seed PT et al. . Clinical- and cost-effectiveness of a nurse led self-management intervention to reduce emergency visits by people with epilepsy. PLoS ONE 2014;9:e90789 10.1371/journal.pone.0090789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ridsdale L, Virdi C, Noble A et al. . Explanations given by people with epilepsy for using emergency medical services: a qualitative study. Epilepsy Behav 2012;25:529–33. 10.1016/j.yebeh.2012.09.034 [DOI] [PubMed] [Google Scholar]
- 31.Noble AJ, Morgan M, Virdi C et al. . A nurse-led self-management intervention for people who attend emergency departments with epilepsy: the patients’ view. J Neurol 2013;260:1022–30. 10.1007/s00415-012-6749-2 [DOI] [PubMed] [Google Scholar]
- 32.Gilliam F, Penovich PE, Eagan CA et al. . Conversations between community-based neurologists and patients with epilepsy: results of an observational linguistic study. Epilepsy Behav 2009;16: 315–20. 10.1016/j.yebeh.2009.07.039 [DOI] [PubMed] [Google Scholar]
- 33.Jain P, Patterson VH, Morrow JI. What people with epilepsy want from a hospital clinic. Seizure 1993;2:75–8. 10.1016/S1059-1311(05)80106-2 [DOI] [PubMed] [Google Scholar]
- 34.Goldstein LH, Minchin L, Stubbs P et al. . Are what people know about their epilepsy and what they want from an epilepsy service related? Seizure 1997;6:435–42. 10.1016/S1059-1311(97)80017-9 [DOI] [PubMed] [Google Scholar]
- 35.Ridsdale L, Morgan M, O'Connor C. Promoting self-care in epilepsy: the views of patients on the advice they had received from specialists, family doctors and an epilepsy nurse. Patient Educ Couns 1999;37:43–7. 10.1016/S0738-3991(98)00094-9 [DOI] [PubMed] [Google Scholar]
- 36.Ridsdale L, Kwan I, Cryer C. The effect of a special nurse on patients’ knowledge of epilepsy and their emotional state. Epilepsy Evaluation Care Group. Br J Gen Pract 1999;49:285–9. [PMC free article] [PubMed] [Google Scholar]
- 37.Ridsdale L, Kwan I, Cryer C. Newly diagnosed epilepsy: can nurse specialists help? A randomized controlled trial. Epilepsy Care Evaluation Group. Epilepsia 2000;41:1014–19. [DOI] [PubMed] [Google Scholar]
- 38.Hunt N, Touquet VL. Known epileptic patients brought to the accident and emergency department. J R Coll Gen Pract 1986;36:224–5. [PMC free article] [PubMed] [Google Scholar]
- 39.Bradley PM, Lindsay B. Care delivery and self-management strategies for adults with epilepsy. Cochrane Database Syst Rev 2008;(1):CD006244 10.1002/14651858.CD006244.pub2 [DOI] [PubMed] [Google Scholar]
- 40.Ramaratnam S, Baker GA, Goldstein LH. Psychological treatments for epilepsy. Cochrane Database Syst Rev 2008;(3):CD002029 10.1002/14651858.CD002029.pub3 [DOI] [PubMed] [Google Scholar]
- 41.Lindsay B, Bradley PM. Care delivery and self-management strategies for children with epilepsy. Cochrane Database Syst Rev 2010;(12):CD006245 10.1002/14651858.CD006245.pub2 [DOI] [PubMed] [Google Scholar]
- 42.Pelinka LE, Thierbach AR, Reuter S et al. . Bystander trauma care—effect of the level of training. Resuscitation 2004;61:289–96. 10.1016/j.resuscitation.2004.01.012 [DOI] [PubMed] [Google Scholar]
- 43.Murad MK, Husum H. Trained lay first responders reduce trauma mortality: a controlled study of rural trauma in Iraq. Prehosp Disaster Med 2010;25:533–9. [DOI] [PubMed] [Google Scholar]
- 44.Kano M, Siegel JM, Bourque LB. First-aid training and capabilities of the lay public: a potential alternative source of emergency medical assistance following a natural disaster. Disasters 2005;29:58–74. 10.1111/j.0361-3666.2005.00274.x [DOI] [PubMed] [Google Scholar]
- 45.Plant N, Taylor K. How best to teach CPR to schoolchildren: a systematic review. Resuscitation 2013;84:415–21. 10.1016/j.resuscitation.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 46.Oliver E, Cooper J, McKinney D. Can first aid training encourage individuals’ propensity to act in an emergency situation? A pilot study. Emerg Med J 2014;31:518–20. 10.1136/emermed-2012-202191 [DOI] [PubMed] [Google Scholar]
- 47.Boyd M, Lasserson TJ, McKean MC et al. . Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009;(2):CD001290 10.1002/14651858.CD001290.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gibson PG, Powell H, Coughlan J et al. . Limited (information only) patient education programs for adults with asthma. Cochrane Database Syst Rev 2002(2):CD001005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tapp S, Lasserson TJ, Rowe B. Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007;(3):CD003000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Craig P, Dieppe P, Macintyre S et al. . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baumeister RF. Self-regulation and ego-threat: motivated cognition, self-deception, and destruction in goal setting. In: Gollwitzer PM, Bargh JA, eds. The psychology of action: linking cognition and motivation to behavior. New York: Guilford Press, 1996: 27–47. [Google Scholar]
- 52.Schüz N, Schüz B, Eid M. When risk communication backfires: randomized controlled trial on self-affirmation and reactance to personalized risk feedback in high-risk individuals. Health Psychol 2013;32:561–70. 10.1037/a0029887 [DOI] [PubMed] [Google Scholar]
- 53.Steele CM. The psychology of self-affirmation: sustaining the integrity of the self. In: Berkowitz L, ed. Advances in experimental social psychology. New York: Academic Press, 1988:261–302. [Google Scholar]
- 54.Reed MB, Aspinwall LG. Self-affirmation reduces biased processing of health-risk information. Motiv Emotion 1998;22:99–132. 10.1023/A:1021463221281 [DOI] [Google Scholar]
- 55.Cohen GL, Sherman DK. The psychology of change: self-affirmation and social psychological intervention. Annu Rev Psychol 2014;65:333–71. 10.1146/annurev-psych-010213-115137 [DOI] [PubMed] [Google Scholar]
- 56.Epton T, Harris PR. Self-affirmation promotes health behavior change. Health Psychol 2008;27:746–52. 10.1037/0278-6133.27.6.746 [DOI] [PubMed] [Google Scholar]
- 57.Johnson EC, Fraser RT, Miller JW et al. . A comparison of epilepsy self-management needs: Provider and patient perspectives. Epilepsy Behav 2012;25:150–5. 10.1016/j.yebeh.2012.07.020 [DOI] [PubMed] [Google Scholar]
- 58.Walker ER, Bamps Y, Burdett A et al. . Social support for self-management behaviors among people with epilepsy: a content analysis of the WebEase program. Epilepsy Behav 2012;23:285–90. 10.1016/j.yebeh.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 59.Kralj-Hans I, Goldstein LH, Noble AJ et al. . Self-Management education for adults with poorly controlled epILEpsy (SMILE (UK)): a randomised controlled trial protocol. BMC Neurol 2014;14:69 10.1186/1471-2377-14-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Epilepsy Action. A critical time for epilepsy in England. A study of epilepsy service provision in England Leeds. British Epilepsy Association, 2013. [Google Scholar]
- 61.Epilepsy Action. Best care: the value of epilepsy specialist nurses. Leeds: British Epilepsy Association, 2010. [Google Scholar]
- 62.Brown SW, Besag FMC. United Kingdom. In: Engel J, Pedley TA, eds. Epilepsy: a comprehensive textbook. Philadelphia: Lippincott, Williams & Wilkins, 2008:2915–20. [Google Scholar]
- 63.Dua T, de Boer HM, Prilipko LL et al. . Epilepsy Care in the World: results of an ILAE/IBE/WHO Global Campaign Against Epilepsy survey. Epilepsia 2006;47:1225–31. 10.1111/j.1528-1167.2006.00595.x [DOI] [PubMed] [Google Scholar]
- 64.Fraser RT, Johnson EK, Miller JW et al. . Managing epilepsy well: self-management needs assessment. Epilepsy Behav 2011;20:291–8. 10.1016/j.yebeh.2010.10.010 [DOI] [PubMed] [Google Scholar]
- 65.Choi-Kwon S, Yoon SM, Choi MR et al. . The difference in perceptions of educational need between epilepsy patients and medical personnel. Epilepsia 2001;42:785–9. 10.1046/j.1528-1157.2001.42100.x [DOI] [PubMed] [Google Scholar]
- 66.Elliott JO, Shneker BF. A health literacy assessment of the epilepsy.com website. Seizure 2009;18:434–9. 10.1016/j.seizure.2009.04.003 [DOI] [PubMed] [Google Scholar]
- 67.Pramuka M, Hendrickson R, Van Cott AC. Survey results of Internet and computer usage in veterans with epilepsy. Epilepsy Behav 2010;17:366–8. 10.1016/j.yebeh.2009.11.016 [DOI] [PubMed] [Google Scholar]
- 68.Kendall S, Thompson D, Couldridge L. The information needs of carers of adults diagnosed with epilepsy. Seizure 2004;13:499–508. 10.1016/j.seizure.2003.12.003 [DOI] [PubMed] [Google Scholar]
- 69. Health & Social Care Information Centre. Quality and Outcomes Framework (QOF) for April 2012-March 2013, England. 2013. http://www.hscic.gov.uk/catalogue/PUB12262.
- 70. Department of Health. Health Profile 2012 Liverpool. 2012. www.apho.org.uk/resource/view.aspx?RID=117032.
- 71. Department of Health. Health Profile 2012 Wirral. 2012. www.apho.org.uk/resource/item.aspx?RID=117035.
- 72.Mittan R. Fear of seizures. In: Whitman S, Hermann B, eds. Psychopathology in epilepsy: social dimensions. New York: Oxford University Press, 1986:90–121. [Google Scholar]
- 73.Martiniuk AL, Speechley KN, Secco M et al. . Development and psyhometric properties of the Thinking about Epilepsy questionnaire assesing children's knowledge and attitudes about epilepsy. Epilepsy Behav 2007;10:595–603. 10.1016/j.yebeh.2007.01.011 [DOI] [PubMed] [Google Scholar]
- 74.Wagner AK, Keller SD, Kosinski M et al. . Advances in methods for assessing the impact of epilepsy and antiepileptic drug therapy on patients’ health-related quality of life. Qual Life Res 1995;4:115–34. 10.1007/BF01833606 [DOI] [PubMed] [Google Scholar]
- 75.Shore CP, Austin JK, Dunn DW. Maternal adaptation to a child's epilepsy. Epilepsy Behav 2004;5:557–68. 10.1016/j.yebeh.2004.04.015 [DOI] [PubMed] [Google Scholar]
- 76.Cramer JA, Perrine K, Devinsky O et al. . Development and cross-cultural translations of a 31-item quality of life in epilepsy inventory. Epilepsia 1998;39:81–8. 10.1111/j.1528-1157.1998.tb01278.x [DOI] [PubMed] [Google Scholar]
- 77.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 78.Thapar A, Kerr M, Harold G. Stress, anxiety, depression, and epilepsy: investigating the relationship between psychological factors and seizures. Epilepsy Behav 2009;14:134–40. 10.1016/j.yebeh.2008.09.004 [DOI] [PubMed] [Google Scholar]
- 79.Jacoby A. Felt versus enacted stigma: a concept revisited: evidence from a study of people with epilepsy in remission. Soc Sci Med 1994;38:269–74. 10.1016/0277-9536(94)90396-4 [DOI] [PubMed] [Google Scholar]
- 80.Taylor J, Baker GA, Jacoby A. Levels of epilepsy stigma in an incident population and associated factors. Epilepsy Behav 2011;21:255–60. 10.1016/j.yebeh.2011.04.002 [DOI] [PubMed] [Google Scholar]
- 81.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649–55. 10.1093/geront/20.6.649 [DOI] [PubMed] [Google Scholar]
- 82.Hibbard JH, Mahoney ER, Stockard J et al. . Development and Testing of a Short Form of the Patient Activation Measure. Health Serv Res 2005;40:1918–30. 10.1111/j.1475-6773.2005.00438.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Beecham J, Knapp M. Costing psychiatric interventions. In: Thornicroft G, Brewin C, Wing J, eds. Measuring mental health needs. London: Gaskell, 1992:163–83. [Google Scholar]
- 84.Williams A. The role of the EUROQOL instrument in QALY calculations. York: Centre for Health Economics, University of York, 1995. [Google Scholar]
- 85.Smyth RM, Duley L, Jacoby A et al. . Women's experiences of participating in the Magpie Trial: a postal survey in the United Kingdom. Birth 2009;36:220–9. 10.1111/j.1523-536X.2009.00326.x [DOI] [PubMed] [Google Scholar]
- 86.Brueton VC, Tierney J, Stenning S et al. . Strategies to improve retention in randomised trials. Cochrane Database Syst Rev 2013;12:MR000032 10.1002/14651858.MR000032.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012;65:301–8. 10.1016/j.jclinepi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- 88.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287–91. 10.1002/pst.185 [DOI] [Google Scholar]
- 89.Noble AJ, Goldstein LH, Seed P et al. . The characteristics of emergency attendees for epilepsy in London hospitals. World Congress of Neurology; Morocco, 2011. [Google Scholar]
- 90.Vellinga A, Cormican M, Hanahoe B et al. . Opt-out as an acceptable method of obtaining consent in medical research: a short report. BMC Med Res Methodol 2011;11:40 10.1186/1471-2288-11-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Travena L, Irwig L, Barratt A. Impact of privacy legislation on the number and characteristics of people who are recruited for research: a randomised controlled trial. J Med Ethics 2006;8:477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Junghans C, Feder G, Hemingway H et al. . Recruiting patients to medical research: double blind randomised trial of “opt-in” versus “opt-out” strategies. BMJ 2005;331:940 10.1136/bmj.38583.625613.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schroy PC III, Glick JT, Robinson P et al. . A cost-effectiveness analysis of subject recruitment strategies in the HIPAA era: results from a colorectal cancer screening adherence trial. Clin Trials 2009;6:597–609. 10.1177/1740774509346703 [DOI] [PubMed] [Google Scholar]