Abstract
Objective
The aim of this study was to identify chronotypes of medical students at the Federal University of Paraíba (UFPB) and its relationship to quality of sleep, daytime sleepiness, age, sex and season of birth.
Methods
The final sample consisted of 221 students, assessed by four questionnaires: demographic questionnaire, Morningness–Eveningness Questionnaire (MEQ), Pittsburgh Sleep Quality lndex (PSQI) and Epworth Sleepiness Scale (ESS).
Results
There was a statistically significant difference between groups with respect to chronotypes and PSQI score (p<0.0005), but not with excessive daytime sleepiness. A significant negative correlation was found between the scores of MEQ and PSQI (rho=−0.3, p<0.0005), demonstrating that the greater the eveningness, the worse the sleep quality. It was observed that 51.6% of students were classified as indifferent chronotype, 61.5% had poor quality of sleep, while 42.1% had excessive daytime sleepiness. Sex and season at birth did not differ between chronotypes.
Conclusion
These findings demonstrate that the evening chronotype was associated with poor quality of sleep in medical students, but not with increased daytime sleepiness, with potential impairment to their academic performance and quality of life.
Keywords: Chronobiology phenomena, Sleep deprivation, Medical students
1. Introduction
Chronobiology organization constitutes itself as one of the parameters responsible for inter-individuality differences. Three human chronotypes are described: morning (“larks”), evening (“owls”) and indifferent. They are characterized by individual preferences for activity realization during a determined period of the day, with better alertness during morning, evening or without any preference, respectively [1].
Regardless of the individual chronotype, synchronization and regularity of the sleep–wake cycle, is a must. In medical students, this process is modified by various factors, such as curricular load during the entire day, extra-curricular activities, physical and emotional stress, pressure for high academic performance and influence of hospital demands [2,3]. Learning process and humor status are also conditioned by sleep–wake cycle and influenced by the quality and duration of sleep [4]. When compared to normal population, medical students show an average of 6 h of sleep per day, a result that is inferior to the 8 h per day, commonly found in the normal population [2,5].
It is supposed that individual circadian preferences for sleep–wake cycles are, till a certain degree, under genetic and hereditary control [6–10]. Possibly, such association derives from intrinsic properties of the circadian system [11], and it is also believed that diurnal preference as well as the quality of sleep, demonstrate a strong genetic component. A series of studies were conducted to verify the relationship between genes and variables of the circadian rhythm [12]. Environmental influence, on other hand, did show a low correlation with these phenotypes [11].
The main question of this research is: Does chronotype demonstrate association with the quality of sleep and excessive diurnal sleepiness among medical students? The objective of this study was to verify the association of chronotype with quality of sleep and excessive diurnal sleepiness among medical students of the Federal University of Paraiba (UFPB), as well as to evaluate its association with the demographics of the studied population.
2. Methods
2.1. Model of study and sampling
This was an observational cross-sectional study, involving students of the 1st to the 6th year of the graduation course of Medicine at the Federal University of Paraiba (UFPB), campus I, João Pessoa, Paraíba, Brazil. Stratified sample was used, proportionately to the number of students in each year of medical school.
For the calculation of sample size, we used the SPSS SamplePower 3.0 software, through the model of difference between means of two groups. The primary variable, the Pittsburgh Sleep Quality Index (PSQI) score, was utilized as a reference for the calculation and the data were determined from the results of Selvi et al. (2012), who also studied the quality of sleep in relationship to chronotype in a sample of university students [13]. In the referred study, the difference between the mean values for the global score obtained by the application of PQSI in morning and evening groups was of 1.5, being the highest standard deviation of 2.6. It was considered a level of significance of 0.05 for all calculations. To obtain a statistical power of 80%, it was established that the ideal sample size was of 49 students per group. As in the study by Selvi et al. (2012), the approximately proportion of morning, indifferent and evening subjects was of, respectively, 1:2:1; we estimated a similar distribution, with the need for 196 students to obtain a minimum of 49 students per group. We additionally considered 30% more individuals to compensate for possible exclusions and dropouts after the data collection (for example, by means of incomplete filling out of the research instruments) or by refusal to participate in the research, reaching then a total sample of 255 students to apply the research tools.
2.2. Instruments and procedures for data collection
The application of the research instruments was performed in the classroom, self-administered, after 4 weeks of the beginning of the ongoing semester. We handed out the study protocol to all students at the initial approach, containing the four instruments to collect the data and the Term of Informed Consent.
The following instruments were used: (1) Social-Demographic Questionnaire: gender, date of birth and course semester; (2) Standard Questionnaire for chronotype identification (MEQ); (3) Pittsburgh Sleep Quality Index (PSQI); (4) Epworth Sleepiness Scale (ESS).
The Standard Questionnaire for identifying the chronotypes (Morningness–Eveningness Questionnaire – MEQ) [14] is constituted by 19 auto-evaluating questions for identification of the chronotype and whose global score varies from 16 to 86. Individuals with values below 42 are classified as evening type; those above 58, as morning type and those between 42 and 58, as indifferent type. This questionnaire was translated and adapted for the Portuguese language by the Multidisciplinary Development and Biological Rhythms Group of the University of São Paulo [15].
The Pittsburg Sleep Quality Index (PSQI) [16] is composed of 10 questions to measure the sleep quality of the adult during the month that preceded the interview. This questionnaire is divided into seven areas: quality, latency, duration, sleep habitual efficiency, disturbances, use of medication to sleep and sleep disorders. For each area a score is attributed, varying from 0 (zero) to 3 (three). The final score is obtained from the sum of the scores from the seven areas, varying from 0 to 21, being the better the quality of sleep with the lower score obtained. Scores from 0 to 5 indicate good quality of sleep and from 6 to 21 indicate poor quality of sleep. The questionnaire was translated and adapted for the Portuguese language, whose version demonstrated a degree of confidence of 81% [17].
The Epworth Sleepiness Scale (ESS) is used to evaluate the existence of excessive diurnal sleepiness. Scores above 10 are associated with diurnal sleepiness [18]. Validated for the Portuguese language [17], this scale consists of questions about the probability of sleeping in different situations, such as, for example, watching TV, reading or sitting down, and it attributes points to each one of the evaluated items. Results inferior to 10 points indicate the absence of sleepiness; between 10 and 16 points suggest mild sleepiness; between 16 and 20 points, severe sleepiness.
The research project was approved by the Lauro Wanderley University Hospital׳s Ethics Committee for Research.
2.3. Variables
The main variable of the research was the chronotype. Scores of Quality of Sleep (PSQI), scores of Diurnal Sleepiness (Epworth), gender, age, season of birth (Spring, Summer, Autumn, Winter) and semester in Medical School, were all secondary variables.
To evaluate the possible correlation between chronotype and season of birth, we used the dates for the South Hemisphere: Spring between September 22nd and December 20th; Summer, between December 21st and March 20th; Autumn, between March 21st and June 20th; Winter, between June 21st and September 21st.
2.4. Statistical analysis
We utilized the normality tests of Shapiro–Wilk and Kolmogorov–Smirnov with Lilliefors corrections to verify the normality of the distribution of the quantitative variables, whose results revealed the rejection of the null hypothesis for the PSQI and ESS scores. We considered, then, that the variables did not show normal distribution and, therefore, we applied non-parametric tests for the inferential analysis.
The quantitative variables were analyzed between the 3 groups of chronotypes by the Kruskall–Wallis test. The correlation between variables was determined by Spearman׳s Correlation test and the comparison of the qualitative variables between groups was evaluated by the chi-square test.
The level of significance adopted for all tests was of 5%. For the data analysis we used the statistical software SPSS, version 20.0 (SPSS inc., Chicago, IL).
3. Results
From the 255 applied questionnaires, 34 were excluded from incomplete filling out, and 221 remained for the final sample. From these, 55.7% were male students. The average age was of 22.3±3.8 years.
The mean score for PSQI was of 6.5±2.6 and we observed that 136 (61.5%) demonstrated poor quality of sleep. As for diurnal sleepiness, the mean value for the Epworth Sleepiness Scale was 9.12±3.2 points, showing that 128 students (57.9%) did not demonstrate diurnal sleepiness, 84 (38%) had mild sleepiness, and 9 (4.1%) had intense diurnal sleepiness.
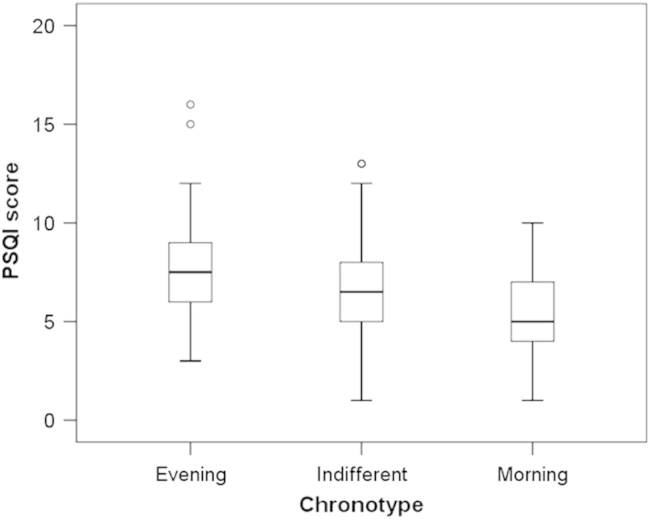
The mean score value to classify the chronotype was of 50.9±11.1. Categorically, 46 students (20.8%) were classified as evening type, 114 (51.6%) as indifferent and 61 (27.6%) as morning types. Table 1 demonstrates that the comparison of the values of the PSQI between the chronotype groups was statistically significant (p<0.0005), with the lowest values for the students with morning chronotype and the highest values for the evening chronotype individuals (Fig. 1). The variables age and diurnal sleepiness were not significant when comparing the chronotype groups.
Fig. 1.
Median values and interquartile range of the Pittsburg Sleep Quality Index (PSQI), according to the chronotypes of medical students from the School of Medicine of the Federal University of Paraiba, João Pessoa, Paraíba, Brazil.
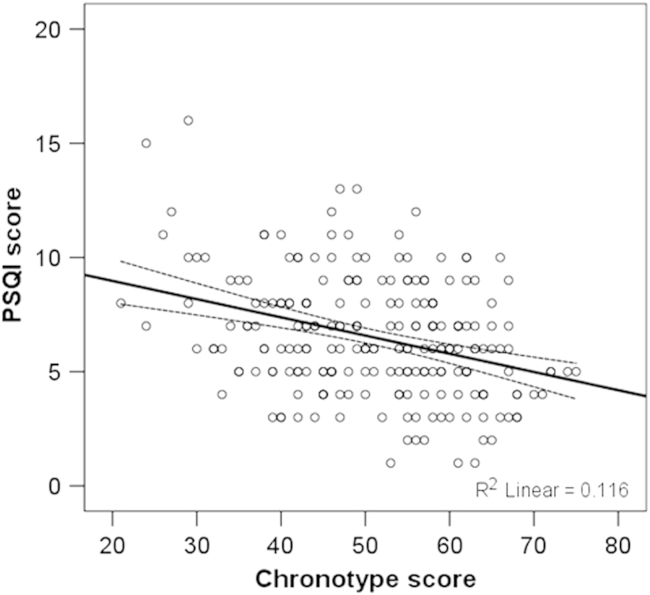
We have observed a significant negative correlation between the scores of the chronotype questionnaire (MEQ) and the quality of sleep (PSQI) (rho=−0.3; p<0.0005) (Fig. 2). The negative correlation suggests that the eveningness – low scores for MEQ – were associated with poor quality of sleep – high scores for PQSI. We have not observed a significant correlation between the scores for MEQ (chronotype) and the ones for ESS (diurnal sleepiness). We did not observe any difference between the evening, indifferent and morning groups in terms of gender and season at birth (Table 2).
Fig. 2.
Linear correlation between the scores of the questionnaire determining the chronotype (MEQ) and the PSQI among the medical students from the School of Medicine of the Federal University of Paraiba, João Pessoa, Paraíba, Brazil.
Table 2.
Distribution of the variables gender and season of birth between chronotypes of medical students from the Federal University of Paraiba, João Pessoa, Paraíba, Brazil.
| Variables |
Groups* |
Total (%) | χ²** | |||
|---|---|---|---|---|---|---|
| Evening (%) | Indifferent (%) | Morning (%) | ||||
| Gender | Male | 29 (63) | 65 (57) | 29 (47.5) | 123 (55.7) | NS |
| Female | 17 (37) | 49 (43) | 32 (52.5) | 98 (44.3) | ||
| Total | 46 (100) | 114 (100) | 61 (100) | 221 (100) | ||
| Season of birth | Spring | 13 (28.3) | 27 (23.7) | 14 (23) | 54 (24.4) | NS |
| Summer | 13 (28.3) | 26 (22.8) | 20 (32.8) | 59 (26.7) | ||
| Autumn | 8 (17.4) | 35 (30.7) | 11 (18) | 54 (24.4) | ||
| Winter | 12 (26.1) | 26 (22.8) | 16 (26.2) | 54 (24.4) | ||
| Total | 46 (100) | 114 (100) | 61 (100) | 221 (100) | ||
Groups determined by the Standard Questionnaire to identify the chronotypes (MEQ).
Statistical significance by the chi-square test for the difference between the groups.
4. Discussion
The results suggest that there is a significant relationship between the chronotype and the quality of sleep in the medical students evaluated, corroborating the research hypothesis. The evening-type individuals showed worse quality of sleep when compared with the morning and indifferent types in the sample of this study. These findings are compatible with the data from the literature. Recently, Selvi et al. (2012), in a study involving 264 university students between 17 and 26 years of age, also identified the relationship between the evening-type chronotype and the poor quality of sleep [13]. Similar results were also evidentiated in other studies [9,11,19,20,21].
During the last decades, researchers have dedicated themselves to investigate the genetic and molecular basis related to the human patterns of morningness and eveningness [6,22–25]. The quality of sleep has also been the target of similar studies [11,26–29]. After clinical evidences of the association between these 2 phenotypic variables (also observed in the present study), an important question arose: would the chronotype and quality of sleep have some genetic correlation between each other?
In this study, we have verified a high prevalence of poor quality of sleep among medical students, corroborating previous researches also conducted with PSQI in medical students, with prevalences of 46 to 58% [5,30]. Bàez et al. (2005) found an even higher prevalence (82%) among medical students from a Colombian University [31]. In Peru, Mayor et al. (2008) found a very similar frequency, of 59.2% [32].
There are several evidences that the medical students constitute a population with higher vulnerability to sleep–wake disturbances. In most part, this vulnerability to sleep disorders might be explained by the presence of a full time curricular load with high demand for study, disrespecting the morningness–eveningness equilibrium among these individuals [2,33].
Another important finding is related to the presence of excessive diurnal sleepiness (EDS) in this group of individuals which, although elevated, did not demonstrate significant association to the chronotype. The prevalence of EDS found in our study (42.1%) was higher than the average for the general Brazilian population, which varies from 0.3% to 13.3% [34]. This finding corroborates with other studies, as Mayor et al. (2008) and Rosales et al. (2007), who found sleepiness averages of 39.2% and 34%, respectively [5,32]. Danda et al. (2005) found the presence of ESD in 39.3% of the medical students at the University in Pernambuco (Brazil), a prevalence very close to the one obtained in the present study [35].
In France, Tailard et al. (1999) evaluated the association between the chronotype and excessive diurnal sleepiness by the Epworth Sleepiness Scale in a population of 617 individuals between the ages of 17 and 80 years of age [36]. Differently from our study, Taillard el al. verified a significant association between morningness and lesser diurnal sleepiness. In a study comprising Brazilian medical students, Hidalgo et al. (2003) also investigated the association between chronotype and DES, using the same research instruments, observing similar results to the ones from our study, or in other words, the absence of correlation between chronotype and DES [37]. The fact that our study, as well as Higalgo et al. (2003) have been conducted in a more homogenous population as far as age was concerned (young adults), in comparison to the one used by Tailard et al. (1999), might have influenced the different results. On other hand, Giannotti et al. (2002) and Vardar et al. (2008) also described higher complaint of diurnal sleepiness among individuals with eveningness chronotype [21,38].
In the present study, we did not verify a statistically significant relationship between gender and chronotype, although we did observe a higher proportion of morningness-type individuals of the female gender (32.7% vs. 23.6%), meanwhile a higher percentage of males were of the eveningness-type chronotype (26.6% vs. 17.3%). Lehnkering and Siegmund (2006) verified the influence of gender among the chronotype distribution. Males, in the previously mentioned study, were significantly more eveningness-type than the females [39].
Adan and Natale (2002), in a study conducted in Barcelona involving 2135 individuals with age between 17 and 30 years, verified association between the male gender and eveningness [40]. In the same year, in Brazil, Hidalgo et al. (2003) investigated 318 individuals of the same age, obtaining the same findings – males more evening-types and females more morning-types [37]. Other studies reinforced the fact that women are more morning-types than men [11,41–46]. On other hand, the results obtained in our study are compatible with the findings of Selvi et al. (2012) who, in a similar sample, of 264 university students between the ages of 17 and 26 years of age, did not find a significant association between gender and chronotype [13].
We also did not observe a significant relationship between chronotype and age, in accordance to the results of Selvi et al. (2012) [13]. Other studies, however, point out to associations between age and chronotype [38,47,48]. Carrier et al. (1997) verified that, with increasing age, people tend to morningness [49]. In adolescence, there are indications that women, as well as men, tend to be more evening-type [50].
There was no significant association between chronotype and the season of birth (Spring, Summer, Autumn, Winter) of the participants of the present study. These results corroborate with the study of Takao et al. (2009), in Japan, conducted with 1156 university students, demonstrating that the season of the year at birth did not influence the diurnal preferences among that population, suggesting possible ethnical interferences [51]. Our results contradicts the study conducted in the south of Brazil, with 648 university students, on which it was verified an association between the season of birth and the circadian typology [52]. In the referred study, the individuals born during spring/summer were associated with eveningness, and the ones born during autumn/winter, were associated with morningness. Researches conducted in Italy, Spain and Canada have also evidentiated associations between chronotype and the season of the year at birth in a sample constituted by adolescents [53,54]. Besides the genetic differences associated with these ethnics, other factors might be implicated on the genesis of dissociation between the chronotype and the season of the year at birth among the Asian population, as the presence of a minor photosensitivity [55] and cultural differences related with the care of children [50,56].
It is known, however, that the four seasons of the year are much better defined in areas of medium latitudes (30–60° in relation to the line of the Equator), as exemplified by Europe, Japan and the United States. On other hand, on low latitudes, from 0° to 30°, such as the case of the location of this study (07°06′55″ S), the seasons of the year are not well defined. Such observation might make it difficult to associate chronotype with this variable [57]. Brazil is almost in its totality situated in low latitudes, going from approximately 5°16′ N latitude, to 33°45′ S latitude. This way, the south region of the country demonstrates characteristics that are closer to the regions of medium latitude, with seasons of the year much better defined [57].
5. Conclusions
The chronotype demonstrated significant association with the quality of sleep, in such a way that evening-type individuals showed worse quality of sleep in comparison to the morning-type ones as well as indifferent ones. There was a high prevalence of poor quality of sleep and excessive diurnal sleepiness among the medical students, although the diurnal sleepiness did not correlate with the chronotypes, as well as age, gender and season of the year at birth.
It is important to point out as a limitation to this study the use of a restricted age range, which resulted in the restriction for the analysis of the association between age and chronotype.
We suggest other studies about the theme, amplifying the evidences toward the association between chronotypes and characteristics related to sleep and other demographic variables, to facilitate a meta-analysis study which comes to elucidate the still divergent issues present in the literature.
From the observation of the impact of circadian biology among the medical students, it might be a better way to plan their daily activities, in accordance to their chronotypes, benefiting not only their academic performance, but as well, their quality of life.
Conflict of interest
No funding source.
Table 1.
Distribution of age, quality of sleep and diurnal sleepiness, according to chronotype among medical students of the Federal University of Paraiba, João Pessoa, Paraíba, Brazil.
| Variables | Groupb | N | Mean | SD | p |
|---|---|---|---|---|---|
| Age | Evening | 46 | 22.0 | 2.7 | NS |
| Indifferent | 114 | 22.2 | 3.2 | ||
| Morning | 61 | 22.8 | 5.2 | ||
| PSQI | Evening | 46 | 7.6 | 2.8 | <0.0005* |
| Indifferent | 114 | 6.63 | 2.5 | ||
| Morning | 61 | 5.43 | 2.2 | ||
| Epworth | Evening | 46 | 9.1 | 3.7 | NS |
| Indifferent | 114 | 9.1 | 2.8 | ||
| Morning | 61 | 9.2 | 3.6 | ||
p<0.05.
Groups determined by the Standard Questionnaire for the identification of chronotypes (MEQ); N: group size; SD: standard deviation; p: statistical significance for the Kruskall–Wallis test; NS: Non-significant; PSQI: Pittsburg Sleep Quality Index; Epworth: Epworth Sleepiness Scale.
Footnotes
Peer review under responsibility of Brazilian Association of Sleep.
References
- 1.Urbán R., Magyaródi T., Rigó A. Morningness–eveningness chronotypes and health-impairing behaviors in adolescents. Chronobiol Int. 2011;28(3):238–247. doi: 10.3109/07420528.2010.549599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cardoso H.C., Bueno F.C.C., Mata J.C., Alves A.P.R., Jochims I., I.H.R.V. Filho. Avaliação da qualidade do sono em estudantes de Medicina. Rev Bras Educ Med. 2009;33(3):349–355. [Google Scholar]
- 3.Pilcher J.J., Huffcutt A.I. Effects of sleep deprivation on performance: a meta-analysis. SLEEP. 1996;19:318–326. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- 4.Valentinuzzi V.S., Araujo J.F. Los ritmos biológicos y el aprendizaje. Ingenierías. 2008;11:41–46. [Google Scholar]
- 5.Rosales E., Egoavil M., La Cruz C., Rey C.J. Somnolencia y calidad del sueño en estudiantes de medicina de una universidad peruana. An Fac Med Lima. 2007;68:150–158. [Google Scholar]
- 6.Archer S.N., Robilliard D.L., Skene D.J., Smits M., Williams A., Arendt J. A length polymorphism in the circadian clock gene Per3 is linked to delayed sleep phase syndrome and extreme diurnal preference. SLEEP. 2003;26:413–415. doi: 10.1093/sleep/26.4.413. [DOI] [PubMed] [Google Scholar]
- 7.Drennan S.J., Kripke D.F., Kelsoe J., Gillin J.C. Morningness/eveningness is heritable. Soc Neurosci Abstr. 1992;18:196. [Google Scholar]
- 8.Hur Y., Bouchard T.J., Lykken D.T. Genetic and environmental influence on morningness–eveningness. Pers Individ Differ. 1998;25:917–925. [Google Scholar]
- 9.Koskenvuo M., Hublin C., Partinen M., Heikkila K., Kaprio J. Heritability of diurnal type: a nationwide study of 8753 adult twin pairs. J Sleep Res. 2007;16:156–162. doi: 10.1111/j.1365-2869.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 10.Vink J.M., Groot A.S., Kerkhof G.A., Boomsma D.I. Genetic analysis of morningness and eveningness. Chronobiol Int. 2001;18:809–822. doi: 10.1081/cbi-100107516. [DOI] [PubMed] [Google Scholar]
- 11.Barclay N.L., Eley T.C., Buysse D.J., Archer S.N., Gregory A.M. Diurnal preference and sleep quality: same genes? A study of young adult twins. Chronobiol Int. 2010;27:278–296. doi: 10.3109/07420521003663801. [DOI] [PubMed] [Google Scholar]
- 12.Allebrandt K.V., Roenneberg T. The search for circadian components in humans: new perspectives for association studies. Braz J Med Biol Res. 2008;41:716–721. doi: 10.1590/s0100-879x2008000800013. [DOI] [PubMed] [Google Scholar]
- 13.Selvi Y., Aydin A., Gulec M., Boysan M., Besiroglu L., Ozdemir P.G. Comparison of dream anxiety and subjective sleep quality between chronotypes. Sleep Biol Rhythms. 2012;10:14–22. [Google Scholar]
- 14.Horne J.A., Östberg O. A self-assessment questionnaire to determine morningness–eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 15.Benedito-Silva A.A., Menna-Barreto L., Marques N., Tenreiro S. Self-assessment questionnaire for the determination of morningness–eveningness types in Brazil. Prog Clin Biol Res. 1990;314(b):89–98. [PubMed] [Google Scholar]
- 16.Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. J Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 17.Bertolazi A.N., Fagondes S.C., Hoff L.S., Dartora E.G., Perin C., Schonwald S.V. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. 2011;2:70–75. doi: 10.1016/j.sleep.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigues R.N.D., Viegas C.A.A., Silva A.A.A.A., Tavafres P. Daytime sleepiness and academic performance in medical students. Arq Neuropsiquiatr. 2002;60(1):6–11. doi: 10.1590/s0004-282x2002000100002. [DOI] [PubMed] [Google Scholar]
- 19.Megdal S.P., Schernhammer E.S. Correlates for poor sleepers in a Los Angeles high school. Sleep Med. 2007;9:60–63. doi: 10.1016/j.sleep.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Shiihara Y., Nakajima M., Miyazaki Y., Nakamiya T., Miyamoto M., Takahashi S. Evaluation of sleep using ambulatory skin potential recording: differences between morning and evening type. Psychiatry Clin Neurosci. 1998;52:167–168. doi: 10.1111/j.1440-1819.1998.tb01010.x. [DOI] [PubMed] [Google Scholar]
- 21.Vardar E., Vardar S.A., Molla T., Kaynak C., Ersoz E. Psychological symptoms and sleep quality in young subjects with different circadian preferences. Biol Rhythm Res. 2008;39:493–500. [Google Scholar]
- 22.Carpen J.D., von Schantz M., Smits M., Skene D.J., Archer S.N. A silent polymorphism in the PER1 gene associates with extreme diurnal preference in humans. J Hum Genet. 2006;51:1122–1125. doi: 10.1007/s10038-006-0060-y. [DOI] [PubMed] [Google Scholar]
- 23.Dijk D., Lockley S.W. Functional genomics of sleep and circadian rhythm invited review: integration of human sleep–wake regulation and circadian rhythmicity. J Appl Physiol. 2002;92:852–862. doi: 10.1152/japplphysiol.00924.2001. [DOI] [PubMed] [Google Scholar]
- 24.Katzenberg D., Young T., Finn L., Lin L., King D.P., Takahashi J.S. A CLOCK polymorphism associated with human diurnal preference. SLEEP. 1998;21:569–576. doi: 10.1093/sleep/21.6.569. [DOI] [PubMed] [Google Scholar]
- 25.Lee H.J., Paik J.W., Kang S.G., Lim S.W., Kim L. Allelic variants interaction of clock gene and gprotein beta 3 subunit gene with diurnal preference. Chronobiol Int. 2007;24:589–597. doi: 10.1080/07420520701534632. [DOI] [PubMed] [Google Scholar]
- 26.Brummett B.H., Krystal A.D., Ashley-Koch A., Kuhn C.M., Zuchner S., Siegler I.C. Sleep quality varies as a function of 5-HTTLPR genotype and stress. Psychosom Med. 2007;69:621–624. doi: 10.1097/PSY.0b013e31814b8de6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heath A.C., Kendler K.S., Eaves L.J., Martin N.G. Evidence for genetic influences on sleep disturbance and sleep pattern in twins. SLEEP. 1990;13:318–335. doi: 10.1093/sleep/13.4.318. [DOI] [PubMed] [Google Scholar]
- 28.Partinen M., Kaprio J., Koskenvuo M., Putoken P., Langinvainio H. Genetic and environmental determination of human sleep. SLEEP. 1983;6:179–185. doi: 10.1093/sleep/6.3.179. [DOI] [PubMed] [Google Scholar]
- 29.Serretti A., Benedetti F., Mandelli L., Lorenzi C., Pirovano A., Colombo C. Genetic dissection of psychopathological symptoms: insomnia in mood disorders and CLOCK gene polymorphism. Am J Med Genet B Neuropsychiatr Genet. 2003;121B:35–38. doi: 10.1002/ajmg.b.20053. [DOI] [PubMed] [Google Scholar]
- 30.Brain M., Rey de Castro J. Calidad de sueño en estudiantes de medicina. A propósito de un estudio transversal aplicando la versión colombiana de cuestionario de Pittsburgh. Póster presentado a la XV Reunión Anual de la Asociación Ibérica de Patología del Sueño. Vitoria-Gasteiz, España. Vigilia-Sueño; 2006;18:54-5.
- 31.Báez G.F., Flores N.N., González T.P., Horrisberger H.S. Calidad del sueño en estudiantes de medicina. Rev Posgrado VIa Cátedra Med. 2005;141:14–17. [Google Scholar]
- 32.Mayor E.R., Rojas T.E.M., Dávila C.C.C., Mujica J.R.C. Somnolencia y calidad de sueño en estudiantes de medicina durante las prácticas hospitalarias y vacaciones. Acta Med Peru. 2008;25:4. [Google Scholar]
- 33.Schneider M.L.M. Universidade Federal do Rio Grande do Sul; Rio Grande do Sul: 2009. Estudo do cronotipo em estudantes universitários de turno integral e sua influência na qualidade do sono. (sonolência diurna e no humor. [thesis]) [Google Scholar]
- 34.Souza J.C., Magna L.A., Aiache S., Magna N.S. Sonolência excessiva diurna na população geral de um município brasileiro. J Bras Psiquiatr. 2008;57:34–37. [Google Scholar]
- 35.Danda G.J.N., Ferreira G.R., Azenha M., Souza K.F.R., Bastos O. Padrão do ciclo sono-vigília e sonolência excessiva diurna em estudantes de medicina. J Bras Psiquiatr. 2005;54:102–106. [Google Scholar]
- 36.Taillard J., Philip P., Bioulac B. Morningness/eveningness and the need for sleep. J Sleep Res. 1999;8:291–295. doi: 10.1046/j.1365-2869.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- 37.Hidalgo M.P.L., De Souza C.M., Zanette C.B., Nunes P.V. Association of daytime sleepiness and the morningness/eveningness dimension in young adult subjects in Brazil. Psychol Rep. 2003;93:427–434. doi: 10.2466/pr0.2003.93.2.427. [DOI] [PubMed] [Google Scholar]
- 38.Giannotti F., Cortesi F., Sebastiani T., Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–199. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 39.Lehnkering H., Strauss A., Wegner B., Siegmund R. Actigraphic investigations on the activityrest behavior of right- and left-handed students. Chronobiol Int. 2006;23:593–605. doi: 10.1080/07420520600724094. [DOI] [PubMed] [Google Scholar]
- 40.Adan A., Natale V. Gender diferences in morningness–eveningness preference. Chronobiol Int. 2002;19:709–720. doi: 10.1081/cbi-120005390. [DOI] [PubMed] [Google Scholar]
- 41.Gaina A., Sekine M., Kanayama H., Takashi Y., Hu L.Z., Sengoku K. Morning–evening preference: sleep pattern spectrum and lifestyle habits among Japanese junior high school pupils. Chronobiol Int. 2006;23:607–621. doi: 10.1080/07420520600650646. [DOI] [PubMed] [Google Scholar]
- 42.Harada T., Inoue M. Do majoring subjects affect the morningness-eveningness preference by students? J Human Ergol. 1999;28:49–53. [PubMed] [Google Scholar]
- 43.Ishihara K., Miyake S., Miyasita A., Miyata Y. Comparisons of sleep-wake habits of morning and evening types in Japanese worker sample. J Hum Ergol. 1988;17:111–118. [PubMed] [Google Scholar]
- 44.Mongrain V., Paquet J., Dumont M. Contribution of the photoperiod at birth to the association between season of birth and diurnal preference. Neurosci Lett. 2006;406:113–116. doi: 10.1016/j.neulet.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 45.Natale V., Adan A., Chotaic J. Further results on the association between morningness–eveningness preference and the season of birth in human adults. Neuropsychobiology. 2002;46:209–214. doi: 10.1159/000067803. [DOI] [PubMed] [Google Scholar]
- 46.Steele M.T., McNamara R.M., Smith-Coggins R., Watson W.A. Morningness–eveningness preferences of emergency medicine residents are skewed toward eveningness. Acad Emerg Med. 1997;4:699–705. doi: 10.1111/j.1553-2712.1997.tb03763.x. [DOI] [PubMed] [Google Scholar]
- 47.Achari K.V., Pati A.K. Morningness–eveningness preference in Indian school students as function of gender, age and habitat. Biol Rhythm Res. 2007;38:1–8. [Google Scholar]
- 48.Paine S.J., Gander P.H., Travier N. The epidemiology of morningness/eveningness: influence of age, gender, ethnicity, and socioeconomic factors in adults (30–49 years) J Biol Rhythms. 2006;21:68–76. doi: 10.1177/0748730405283154. [DOI] [PubMed] [Google Scholar]
- 49.Carrier J., Monk T.H., Buysse D.J., Kupfer D.J. Sleep and morningness-eveningness in the ‘‘middle’’ years of life (20–59 y) J Sleep Res. 1997;6:230–237. doi: 10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- 50.Randler C., Diaz-Morales J.F. Morningness in German and Spanish students: a comparative study. Eur J. Pers. 2007;21:419–427. [Google Scholar]
- 51.Takao M., Kurachi Tatsuo, Kato Hikaru. Photoperiod at birth does not modulate the diurnal preference in asian population. Chronobiol Int. 2009;26:1470–1477. doi: 10.3109/07420520903385606. [DOI] [PubMed] [Google Scholar]
- 52.Alam M.F., Tomasi E., Lima M.S., Areas R., Menna-Barreto L. Caracterização e distribuição de cronotipos no sul do Brasil: diferenças de gênero e estação de nascimento. J Bras Psiquiatr. 2008;57:83–90. [Google Scholar]
- 53.Natale V., Adan A., Fabbri M. Season of birth, gender, and social–cultural effects on sleep timing preferences in humans. SLEEP. 2009;32:423–426. doi: 10.1093/sleep/32.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Caci H., Robert P., Dossios C., Boyer P. L’e´chelle de matinalite´ pour enfants et adolescents: Proprie´te´s psychome´triques et effet du mois de naissance. [Morningness–eveningness for children scale: psychometric properties and month of birth effect.] Encephale. 2005;31:56–64. doi: 10.1016/s0013-7006(05)82372-3. [DOI] [PubMed] [Google Scholar]
- 55.White T., Terman M. Effect of iris pigmentation and latitude on chronotype and sleep timing. Chronobiol Int. 2003;20:1193–1195. [Google Scholar]
- 56.Randler C. In sync with the family: children and partners influence the sleep–wake circadian rhythm and social habits of women. Chronobiol Int. 2009;26:510–525. doi: 10.1080/07420520902821101. [DOI] [PubMed] [Google Scholar]
- 57.Ross J.L.S. São Paulo; Edusp: 2005. Geografia do Brasil. [Google Scholar]