Abstract
Aims
We assessed and compared the diagnostic accuracy of two sets of diagnostic criteria for headache secondary to temporomandibular disorders (TMD).
Methods
In 373 headache subjects with TMD, a TMD headache reference standard was defined as: self-reported temple headache, consensus diagnosis of painful TMD and replication of the temple headache using TMD-based provocation tests. Revised diagnostic criteria for Headache attributed to TMD were selected using the RPART (recursive partitioning and regression trees) procedure, and refined in half of the data set. Using the remaining half of the data, the diagnostic accuracy of the revised criteria was compared to that of the International Headache Society's International Classification of Headache Diseases (ICHD)-II criteria A to C for Headache or facial pain attributed to temporomandibular joint (TMJ) disorder.
Results
Relative to the TMD headache reference standard, ICHD-II criteria showed sensitivity of 84% and specificity of 33%. The revised criteria for Headache attributed to TMD had sensitivity of 89% with improved specificity of 87% (p < 0.001). These criteria are (1) temple area headache that is changed with jaw movement, function or parafunction and (2) provocation of that headache by temporalis muscle palpation or jaw movement.
Conclusion
Having significantly better specificity than the ICHD-II criteria A to C, the revised criteria are recommended to diagnose headache secondary to TMD.
Keywords: Temporomandibular disorders, diagnostic accuracy, headache, sensitivity and specificity
Introduction
The 2004 publication of the International Classification of Headache Disorders (ICHD-II) was a major advancement for standardizing the classification of primary and secondary headaches for clinical and research purposes (1). Establishing conceptual clarity regarding the necessary characteristics for a headache to be secondary to some other disorder has been challenging. Table 1 lists the 2004 general ICHD-II template for secondary headaches as well as the proposed 2009 revision by Olesen and colleagues (2).
Table I.
Current and proposed diagnostic templates for secondary headache.
| General diagnostic criteria for secondary headaches per ICHD-II (2004) | General diagnostic criteria for secondary headaches proposed by Olesen and colleagues (2009) |
|---|---|
| Diagnostic criteria | Diagnostic criteria |
| A. Headache with one (or more) of the following (listed) characteristics and fulfilling criteria C and D. | A. Headache of any type fulfilling criteria C and D. |
| B. Another disorder known to be able to cause headache has been demonstrated. | B. Another disorder scientifically documented to be able to cause headache has been diagnosed. |
| C. Headache occurs in close temporal relation to the other disorder and/or there is other evidence of a causal relationship. | C. Evidence of causation shown by at least two of the following: |
| 1. Headache has occurred in temporal relation to the onset of the presumed causative disorder. | |
| 2. Headache has occurred or has significantly worsened in temporal relation to worsening of the presumed causative disorder. | |
| D. Headache is greatly reduced or resolves within three months (this may be shorter for some disorders) after successful treatment or spontaneous remission of the causative disorder. | 3. Headache has improved in temporal relation to improvement of the presumed causative disorder. |
| 4. Headache has characteristics typical of the causative disorder. | |
| 5. Other evidence exists of causation. | |
| D. The headache is not better accounted for by another headache diagnosis. |
ICHD-II: International Classification of Headache Diseases, 2nd edition.
One of the secondary headaches represented in the ICHD-II headache taxonomy is (11.7) Headache or facial pain attributed to temporomandibular joint (TMJ) disorder (Table 2). Cross-sectional studies of clinical samples have demonstrated co-morbidity between headache and temporomandibular disorders (TMD). A majority of symptomatic TMD patients have headache (3–5), and it is common for patients with tension-type headache (TTH) and even migraine to also have TMD (6–10). However, longitudinal studies are necessary to clarify the temporal relationship between TMD and headache. One three-year prospective study found that the development of TMD was accompanied by an increase in headache (11), while a two-year prospective study demonstrated that the presence of TMD at baseline predicted the future onset of headache (12). Finally, the results of randomized clinical trials have suggested that interventions influencing the masticatory system have a beneficial effect on headache (13–15).
Table 2.
ICHD-II (11.7) Diagnostic criteria for Headache or facial pain attributed to temporomandibular joint (TMJ) disorder (2004).
| Diagnostic criteria |
| A. Recurrent pain in one or more regions of the head and/or face fulfilling criteria C and D. |
| B. MRI and/or scintigraphy demonstrate TMJ disorder. |
| C. Evidence that pain can be attributed to the TMJ disorder, based on at least one of the following: |
| 1. Pain is precipitated by jaw movements and/or chewing of hard or tough food. |
| 2. Reduced range of or irregular jaw opening. |
| 3. Noise from one or both joint capsule(s) of one or both TMJs. |
| 4. Tenderness of the joint capsule(s) of one or both TMJs. |
| D. Headache resolves within three months, and does not recur, after successful treatment of the TMJ disorder. |
ICHD-II: International Classification of Headache Diseases, 2nd edition.
A multisite study that we will refer to in this paper as the Validation Project was conducted to assess the validity of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) (16). One of the recommendations from this project was to develop diagnostic criteria for headache secondary to TMD (17). As part of the planned data collection, the Validation Project TMD examiners had recorded, with one exception, all data necessary for the ICHD-II criteria for (11.7) Headache or facial pain attributed to temporomandibular joint (TMJ) disorder. This one exception was for data pertinent to criterion D that requires longitudinal observations (Table 2). Such data could not be collected in the cross-sectional Validation Project. However, this criterion D is no longer proposed in the 2009 revision of the general template for secondary headaches (Table 1) (2).
The purpose of this paper is to contribute toward identifying the most valid diagnostic criteria for headache attributed to TMD. This goal was addressed by the following aims:
-
Aim 1:
To estimate the diagnostic accuracy of criteria A to C of the ICHD-II diagnostic template for Headache or facial pain attributed to temporomandibular joint (TMJ) disorder;
-
Aim 2:
To develop new diagnostic criteria for Headache attributed to TMD and assess the diagnostic accuracy of these criteria.
Methods
Study subjects
The subject sample for this investigation was drawn from the 705 participants in the Validation Project. A complete description is available for the multisite Validation Project, conducted from 2003 to 2006. It includes recruitment methods, inclusion and exclusion criteria, participant demographics and clinical characteristics, as well as notice regarding Institutional Review Board approval (16). Subjects reporting widespread pain were excluded from the analyses in this manuscript (18). A subset of the Validation Project sample was selected for the current investigation consisting of 373 subjects who reported temple headache and were diagnosed with painful TMD. Each subject's temple headache was evaluated according to ICHD-II primary headache criteria.
ICHD-II defines primary TTH using four main criteria: Criterion A requires at least 10 headache episodes in the past year. Criterion B requires headache duration of 30 minutes, or longer. Criterion C defines four qualitative headache characteristics, of which at least two are required. Criterion D requires absence or limited presence of associated symptoms that include nausea, vomiting, photophobia or phonophobia (1). Of the 373 subjects who reported temple headache, there were 141 subjects with insufficient symptoms to meet some, or all, of ICHD-II criteria A, B and C for TTH. These subjects are grouped for analysis in this study as “TTH-like headache.” There were 87 subjects meeting ICHD-II TTH criteria, and 145 subjects classified as “migraine-like headache.” Sixty-one “migraine-like headache” subjects fulfilled TTH criteria except for criterion D due to increased presence of associated symptoms. Nine other subjects did not fully meet ICHD-II criteria for migraine without aura, while 75 had classifiable TTH plus migraine without aura.
TMD headache reference standard
To assess the criterion validity of diagnostic templates, a credible reference standard was needed. In consultation with experts in TMD, orofacial pain and headache, the reference standard for headache secondary to TMD was defined by the following criteria:
Consensus diagnosis of painful TMD including masticatory myofascial pain and/or TMJ arthralgia (19);
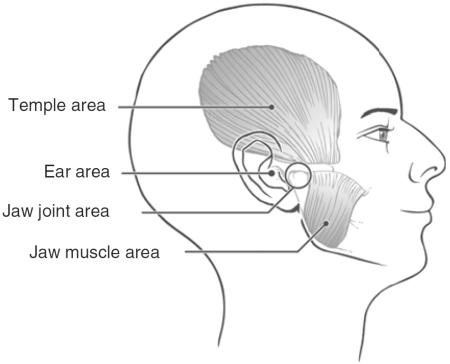
Self-report of headache in the temple area based on a positive response to the question, “In the last year, have you had a headache(s) that included the temple areas of your head, that is, temple area headache(s)?”
Replication of the subjects' “temple headache” complaint using any one of standard TMD provocation tests listed below.
Based on these criteria, the absence or presence of the reference standard TMD headache was then determined for each of the 373 subjects in the study sample.
The first requirement for the TMD headache reference standard was a valid diagnosis of painful TMD: This was established by two TMD experts at each study site who independently evaluated study participants using a standardized study protocol (16). The clinical tests included questionnaire responses, semi-structured interviews, clinical measurements, and radiographic studies including bilateral TMJ MRI and bilateral TMJ CT, with all imaging interpreted by a calibrated board-certified radiologist. After completion of their independent assessments and diagnoses, the two TMD experts met to establish a consensus diagnosis with the subject still present in order to resolve any differences between the independently recorded diagnoses. For questions that involved radiographic interpretations, the radiologist was available.
The third requirement for the TMD headache reference standard was that standard TMD provocation tests replicated the subject's temple headache. This requirement was also fulfilled by tests independently performed at each study site that consisted of mandibular range of motion (ROM); temporalis muscle palpation; bite tests including biting on a cotton role and clenching the teeth; orthopaedic tests of the TMJ including compression, traction and translation; and static and dynamic orthopaedic jaw tests (16). If pain was reported with any of these provocation tests, the subjects were asked if the pain was “similar or like” their temple headache (i.e., familiar headache).
Validation Project Data for ICHD-II (11.7) Headache or facial pain attributed to temporomandibular joint (TMJ) disorder, criteria A to C
Data for criterion A were based on (1) the presence of head/facial pain in past month and (2) the recurrence of this pain (20). Data to fulfill criterion B were provided by interpretation of the TMJ MRIs and CTs to assess for the presence of any pathology in the TMJs, including disc displacements and degenerative joint disease (16). No scintigraphy was performed since this is an uncommon technique to assess for TMJ pathology. Criterion C1, presence of pain, was addressed using a self-report questionnaire that assessed temple, jaw muscle and TMJ pain changed by jaw activities including jaw movement, function and parafunction. Criterion C2, restriction or irregularity in jaw opening, was met if reduced mouth opening (unassisted or assisted inter-incisal opening) was less than 40 mm after correction for vertical overlap of the incisors, and by assessment for deviations in the opening pattern as viewed from the frontal plane during the exam. Criterion C3, joint noise, was assessed during the examination for any click or crepitus with mandibular ROM. Criterion C4, TMJ tenderness, was addressed by the subject's report of pain in response to digital palpation of the TMJ. Criterion D was not assessed, as explained in the Introduction.
At this point, each subject now had a reference standard TMD headache diagnosis (absent or present) and an ICHD-II (11.7) diagnosis for TMJ-related headache based on criteria A to C.
Data and methods for revised diagnostic model-building
To construct revised diagnostic criteria for Headache attributed to TMD, data for the total subject sample (N=373) were randomly divided into training (N=187) and validation (N=186) data sets. Two steps are described for the revised model-building process: the first involved a computer-program selection of new predictors for the TMD headache reference standard diagnoses, and the second involved investigator-performed refinement of the computer-generated diagnostic template.
For the computer-generated diagnostic template, the TMD headache reference standard diagnoses were set as the dependent (response) variable for a recursive partitioning method called RPART (21). Out of 97 candidate predictors submitted to the RPART procedure, 37 variables were selected as being mathematically associated with this dependent variable, and they were assembled into multiple classification tree models. The RPART program employed 10-fold cross-validation procedures that first divided the training data set into 10 subsets of data. These data were then randomly regrouped into 10 groups, each with 9 of the 10 data subsets, and with a different subset of data excluded from each. A prediction tree for the reference standard headache was then grown within each data group, and the performance of the tree was evaluated within the 10th subset of the data that had been excluded for the growing of the tree.
The complexity parameter (CP) used for our investigation was the procedure's default setting of 0.01. The RPART “class” method was specified for the model formula as is indicated for mutually exclusive diagnoses within the response variable. The program selected the best out of the 10 prediction models based on its having the lowest complexity (highest CP) and the lowest cross-validation relative error.
The investigators then refined the best RPART model by eliminating some less statistically influential criteria and evaluating other candidate criteria of interest. All model revision was done in concert with expert opinion and from a review of the current literature. In particular, one candidate variable of interest to be tested was the ICHD-II (11.7) criterion B that requires radiographic evidence for a TMJ disorder. With each model modification, sensitivity and specificity were re-assessed relative to the reference standard. Since this was an exploratory investigation, protection for alpha inflation due to the multiple statistical tests was not required.
Statistical power associated with the study sample
Statistical precision for the Validation Project required sensitivity and specificity estimates to have 95% confidence intervals (CI) with a total width of ≤20 (0–100 scale). For the current study, validity cutoffs for sensitivity and specificity were set a priori at ≥80% with the same precision requirement. Taking sensitivity as an example, its CI half-width is expressed as where p is the estimated sensitivity, and N is the number of participants positive for the reference standard. If both sensitivity and specificity were at 50% where the binomial variance is largest, the minimum sample for required precision is 100 positive and 100 negative diagnoses. The fixed sample of N=373 was considered adequate.
Statistical comparisons
Using contingency tables (chi-square statistic) and the two-independent sample t-test, demographic and socioeconomic variables were compared in subjects who were positive for the TMD headache reference standard versus those who were negative. The McNemar test for correlated data evaluated statistical differences in sensitivity and specificity between the revised criteria and the ICHD-II criteria A to C.
Results
This report compares two diagnostic templates for the diagnosis of headache attributed to TMD: the ICHD-II (11.7) Headache or facial pain attributed to temporomandibular joint (TMJ) disorder criteria A to C, and the final revised diagnostic template for Headache attributed to TMD. Table 3 shows for each of these study templates their frequencies of positive and negative agreement with the TMD headache reference standard.
Table 3.
Agreement of two diagnostic templates with the TMD headache reference standard.
| 1. Diagnostic agreement of the ICHD-II template using criteria A–C | ||||
|---|---|---|---|---|
| TMD headache reference standard |
||||
| Yes | No | Total | ||
|
|
||||
| ICHD-II template | Yes | 63 | 74 | 137 |
| No | 12 | 37 | 49 | |
| Total | 75 | 111 | 186 | |
| 2. Diagnostic agreement of the revised criteria template | ||||
|---|---|---|---|---|
| TMD headache reference standard |
||||
| Yes | No | Total | ||
|
|
||||
| Revised criteria template | Yes | 67 | 14 | 81 |
| No | 8 | 97 | 105 | |
| Total | 75 | 111 | 186 | |
ICHD-II: International Classification of Headache Diseases, 2nd edition; TMD: temporomandibular joint disorder.
Table 4 shows their point estimates for sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and the 95% normal approximation CIs for each point estimate. For informational purposes, these estimates are also indicated separately for each criterion within the templates.
Table 4.
Diagnostic accuracy of two templates designed to diagnose headache attributed to TMD.
| Diagnostic template and criteria | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|
| ICHD-II criteria A–C for TMJ headache | ||||
| A. Recurrent pain in head and/or face | 100 (100–100) | 25 (17–33) | 47 (40–55) | 100 (100–100) |
| B. CT and MRI-disclosed TMJ disorder | 84 (76–92) | 18 (11–25) | 41 (33–49) | 62 (46–79) |
| C. At least one of the following: | 100 (100–100) | 3 (0–6) | 41 (34–48) | 100 (100–100) |
| • Pain with jaw movements | ||||
| • Jaw opening limitation or motion irregularity | ||||
| • Joint capsule noise | ||||
| • Joint capsule tenderness | ||||
| Overall diagnostic validity | 84 (76–92) | 33 (25–42) | 46 (38–54) | 76 (63–88) |
| Revised criteria for headache attributed to TMD | ||||
| Familiar headache to palpation of temporalis muscle | 97 (94–100) | 83 (76–90) | 79 (71–88) | 98 (95–100) |
| Change in headache pain with jaw movements | 92 (86–98) | 52 (43–62) | 57 (48–65) | 91 (83–98) |
| Overall diagnostic validity | 89 (82–96) | 87 (81–94) | 83 (74–91) | 92 (87–97) |
TMD: temporomandibular disorder; ICHD-II: International Classification of Headache Diseases, 2nd edition. PPV: positive predictive value; NPV: negative predictive value; CI: confidence interval; TMJ: temporomandibular joint.
Sensitivity and specificity
The ICHD-II (11.7) criteria A to C were observed to have sensitivity of 84% and specificity of 33%. These estimates had total width of the CI≤17. The individual criteria showed sensitivity of 84–100% with specificity of 3–25%. The revised diagnostic template had sensitivity of 89% and specificity of 87%, with total width of the CIs≤14. When the two revised criteria were evaluated separately, their ranges of sensitivity and specificity were 92–97% and 52–83%, respectively.
New diagnostic template for headache attributed to TMD
The two revised criteria, (1) modification of the temple headache by jaw movement, function or parafunction, and (2) report of familiar headache in the temple with palpation of the temporalis muscle(s) or with mandibular ROM, are used to define criterion C in the recommended diagnostic template seen in Table 5. Adding MRI or CT confirmation of an intra-articular TMJ disorder to this template provided no improvement in its diagnostic accuracy. Sensitivity decreased to 75% and specificity increased to 88%. Additional TMD provocation tests added no new information to that already obtained as a result of using the muscle palpation and ROM tests. When compared to the ICHD-II criteria A to C, the sensitivity of the revised criteria did not differ statistically (p=0.48); however, specificity improved significantly (p<0.001).
Table 5.
Evidence-based diagnostic template for headache attributed to TMD.
| A. Headache of any type fulfilling criteria C and D. |
| B. Painful TMD demonstrated by clinically based diagnostic criteria.a |
| C. Evidence of causation shown by the following: |
| (i) History: Headache in the temple(s) that is changed with jaw movement, function and/or parafunction. |
| AND |
| (ii) Examination: Report of familiar headache in the temple area with: |
| a. Palpation of the temporalis muscle(s),b or |
| b. Range of motion of the jaw. |
| B. The headache is not better accounted for by another headache diagnosis |
A diagnosis of painful TMD (e.g. myofascial pain and TMJ arthralgia) is derived using valid diagnostic criteria (19).
Palpation using 1 kilogram of palpation pressure.
Familiar headache with maximum active opening, maximum passive opening, lateral and/or protrusive movement(s).
TMD: temporomandibular disorders.
Positive and negative predictive values
Table 4 indicates the PPVs for the ICHD-II criteria A to C, and the revised criteria are 46%, and 83%, respectively. NPVs are 76%, and 92%, respectively.
Characterization of the study subjects
Demographic and socioeconomic characteristics of the study sample (N=373) are compared in Table 6. Each subject had temple headache concurrent with painful TMD. The reference standard criteria identified 170 subjects whose temple headache was consistent with Headache attributed to TMD, and 203 subjects whose headache was not related to TMD. There were no statistically significant differences (p≥0.12) between these two groups with regard to gender, age, race, education or income.
Table 6.
Demographic characteristics of 373 study subjects with TMD and temple headache.
| No headache attributed to TMD N=203 | Headache attributed to TMD N=170 | ||
|---|---|---|---|
|
|
|||
| Characteristic | Number (%) or mean±SD | p value | |
| Gender | 0.24 | ||
| Male | 27 (13.3) | 16 (9.4) | |
| Female | 176 (86.7) | 154 (90.6) | |
| Age (years) | 36.2±12.1 | 36.6±13.1 | 0.73 |
| Race | 0.12 | ||
| White | 185 (91.1) | 162 (95.3) | |
| Nonwhite | 18 (8.9) | 8 (4.7) | |
| Education | 0.19 | ||
| No college | 28 (13.8) | 32 (18.8) | |
| ≥1 year of college | 175 (86.2) | 138 (81.2) | |
| Income per year | 0.74 | ||
| <USD 50,000 | 118 (58.1) | 97 (57.1) | |
| USD 50,000–79,999 | 45 (22.2) | 43 (25.3) | |
| ≥USD 80,000 | 40 (19.7) | 30 (17.6) | |
TMD: temporomandibular disorder; USD: U.S. dollars.
The diagnostic accuracy of the revised criteria for Headache attributed to TMD was assessed in the validation half of the data set (N=186) and observed to be acceptable across the entire spectrum of headache subgroups represented in this study sample. The sensitivity and specificity of these criteria in the TTH-like headache subgroup (N=68) were 93% (95% CI 81–100%) and 91% (95% CI 83–98%), respectively. For the TTH subgroup (N=41), sensitivity was 83% (95% CI 66–100%), with specificity of 83% (95% CI 67–98%). In the migraine-like headache subgroup (N=77), sensitivity was 90% (95% CI 82–99%), and specificity was at 86% (95% CI 74–97%).
Discussion
Comparison of two templates for diagnosis of TMD headache
Relative to the reference standard, the ICHD-II (11.7) criteria showed acceptable sensitivity (84%) but low specificity (33%), resulting in an unacceptable rate of false positive diagnoses (77/111=66.7%, Table 3). The revised diagnostic criteria for Headache attributed to TMD had the highest point estimate for sensitivity at 89%, and showed a significant improvement over the existing ICHD-II (11.7) criteria with specificity of 87%. All these estimates have good precision, with total width of the confidence intervals ≤17. Sensitivity and specificity estimates are theoretically independent of the prevalence of target conditions (22). In contrast, PPV and NPV estimates are affected by the prevalence of study conditions. They are reported here, nevertheless, as further evidence for the relative differences in diagnostic accuracy between the two study templates.
TMD headache reference standard
This reference standard was constructed with elements that support its credibility including consensus-based diagnoses for painful TMD and replication of the subject's headache. Replication of pain has been used successfully to establish reference standards for assessment of pain in other medical classification schemes (19,23–31). We conclude that this reference standard has content and construct validity, given that it was vetted by TMD, orofacial pain and headache experts, and it is consistent with the literature.
Criterion A for headache attributed to TMD
We implemented for this criterion in Table 5 the recommendation by Olesen and colleagues' for “Headache of any type fulfilling criteria C and D” (2). Of the 373 subjects reporting temple headache and painful TMD, the TMD headache reference standard identified 170 subjects with TMD headache and 203 subjects without TMD headache. Primary headaches are, by definition, idiopathic but the evidence presented in this paper demonstrates that some primary headaches may not be idiopathic but rather secondary to TMD. Previous reports of TMD association with primary headache may be explained, at least in part, by the fact that some of these primary headaches could be more correctly diagnosed as secondary headaches attributed to TMD.
In addition, several investigators have observed that multiple types of primary headache can be related to TMD (4–10). In this study, some of the headaches not classifiable for primary headache using ICHD-II criteria were identified as secondary TMD headaches. We note that the proposed diagnostic template for Headache attributed to TMD has sensitivity of 83–93% and specificity 83–91% within each subgroup of the spectrum of headache that includes TTH, TTH-like headache, and migraine-like headache. Thus, this study supports the rationale for criterion A in Table 5 that includes headache of any type fulfilling criteria C and D.
Criterion B for headache attributed to TMD
The diagnoses of painful TMD, now required for criterion B in Table 5, include myofascial pain and TMJ arthralgia. These diagnoses are easily determined using simple, reliable and valid diagnostic criteria (19). We eliminated the original criterion B for ICHDII (11.7) that required imaging to demonstrate a TMJ disorder, as this information did not improve sensitivity and specificity. We emphasize also the lack of causal specificity for this criterion since asymptomatic individuals often have positive imaging findings for TMJ disc displacement and degenerative joint disease (32–35).
Criterion C for headache attributed to TMD
To fulfil criterion C in Table 5 for evidence of causation, one history item and one of two clinical findings must be positive. The history item requires that the headache is made better or worse with jaw movement, function or parafunction, all hallmarks of a painful TMD. This characteristic is nearly identical to criterion C1 in the original ICHD-II (11.7). Parafunctional habits, such as clenching of the teeth, may cause trauma to the masticatory system and can result in pain (36,37).
The clinical evidence of causation is met when familiar temple headache is provoked by palpation of the temporalis muscle or by mandibular ROM. These same tests are part of validated diagnostic criteria for painful TMD due to jaw muscle pain (e.g. myofascial pain) and jaw joint pain (e.g. TMJ arthralgia) (19). Together, these two criteria meet the requirement for secondary headaches, that is, that the “ … headache (is) to have characteristics of the presumed causative disorder” (2). This information should encourage clinicians to palpate the pericranial muscles, a clinical test that has been lamented as being “ … a valuable but underused physical examination technique for detection of TTH” (38).
Nomenclature for diagnostic criteria for headache attributed to TMD
We propose a change from “TMJ” to “TMD” in any attribution given to diagnostic criteria for headache that is attributed to TMD. “TMD” is accepted as the collective term for musculoskeletal conditions affecting the masticatory system that includes both the TMJ and the masticatory muscles (39,40).
Strengths of the study
Data for two of the three criteria required for the TMD headache reference standard were collected using incontrovertible methods. The TMD diagnoses collected for criterion B, and the replication of familiar headache for criterion C were all obtained using independent examinations followed by consensus methodology to ensure against misclassification. In addition, standardized specifications were used for all examination tests such as the pressure of 1 kilogram for the muscle palpation tests. All operational definitions are available that were used to assess the criteria for the ICHD-II Headache or facial pain attributed to temporomandibular joint (TMJ) disorder as well as the revised criteria for Headache attributed to TMD (41).
Limitations of the study
Since the Validation Project was designed to assess the reliability and criterion validity of the Research Diagnostic Criteria for Temporomandibular Disorders, a comprehensive headache history was taken, but headache diaries were not used, and complete physical and neurologic examinations were not performed. Some of the 203 subjects with non-TMD headache may have had a primary headache that could not be classified by the ICHD-II criteria used in this study. Secondly, primary headaches, including migraine and the combination of migraine and TTH, have been associated with TMD (6–10,42). Therefore, the diagnostic accuracy of the revised criteria should be assessed in a specialized tertiary headache center. Thirdly, subjects reporting widespread pain were excluded from the current study sample. Future research is needed to determine whether pain conditions such as widespread pain have an effect on the accuracy of the recommended diagnostic template in Table 5, Headache attributed to TMD. Finally, future research should determine if the validity of this diagnostic instrument would improve with the addition of the temporal criteria proposed by Olesen and colleagues (2).
Conclusions
The revised diagnostic template for Headache attributed to TMD provides a valid, standardized and practical tool for clinicians to improve diagnosis of their TMD headache patients and for researchers to reduce mis-classification of their study subjects.
Acknowledgements
The authors would like to thank Dr Vladimir Leon-Salazar for his valuable contribution during the elaboration and finishing of this manuscript.
Funding This work was supported by the NIH/NIDCR (grant no. U01-DE1333).
Appendix
Figure provided to the subject in this study ©
Specific questions used for Headache attributed to TMD:
In the last year*, have you had a headache(s) that included the TEMPLE AREA(S) of your head, that is, temple area headaches(s).
- In the last 30 days*, did the following activities change any headache (that is, make it better or make it worse) in your temple area on either side? (yes or no answer)
- Chewing hard or tough food
- Opening your mouth or moving your jaw forward or to the side
- Jaw habits such as holding teeth together, clenching/grinding or chewing gum.
- Other jaw activities such as talking, kissing or yawning
Specifications for the clinical exam are on the International RDC-TMD Consortium website: http://www.rdc-twdinternational.org/OtherResources/ResearchProtocols.Aspx.
*Note: The time frames of one year noted for question #1, and 30 days for question #2 were specific to the data set available as presented in this manuscript. Other contexts in the assessment of headaches might dictate different time frames for these questions, but these have been employed in past investigations.
Footnotes
Conflict of interest statement The authors declare that there is no conflict of interest.
References
- 1.Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders. Cephalalgia. (2nd edn) 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.Olesen J, Steiner T, Bousser MG, et al. Proposals for new standardized general diagnostic criteria for the secondary headaches. Cephalalgia. 2009;29:1331–1336. doi: 10.1111/j.1468-2982.2009.01965.x. [DOI] [PubMed] [Google Scholar]
- 3.Nilsson IM. Reliability, validity, incidence and impact of temporormandibular pain disorders in adolescents. Swed Dent J Suppl. 2007:7–86. [PubMed] [Google Scholar]
- 4.Franco AL, Goncalves DA, Castanharo SM, et al. Migraine is the most prevalent primary headache in individuals with temporomandibular disorders. J Orofac Pain. 2010;24:287–292. [PubMed] [Google Scholar]
- 5.Anderson GC, John MT, Ohrbach R, et al. Influence of headache frequency on clinical signs and symptoms of TMD in subjects with temple headache and TMD pain. Pain. 2011;152:765–771. doi: 10.1016/j.pain.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haley D, Schiffman E, Baker C, et al. The comparison of patients suffering from temporomandibular disorders and a general headache population. Headache. 1993;33:210–213. doi: 10.1111/j.1526-4610.1993.hed33040210.x. [DOI] [PubMed] [Google Scholar]
- 7.Schokker RP, Hansson TL, Ansink BJ. Craniomandibular disorders in patients with different types of headache. J Craniomandib Disord. 1990;4:47–51. [PubMed] [Google Scholar]
- 8.Glaros AG, Urban D, Locke J. Headache and temporomandibular disorders: evidence for diagnostic and behavioural overlap. Cephalalgia. 2007;27:542–549. doi: 10.1111/j.1468-2982.2007.01325.x. [DOI] [PubMed] [Google Scholar]
- 9.Ballegaard V, Thede-Schmidt-Hansen P, Svensson P, et al. Are headache and temporomandibular disorders related? A blinded study. Cephalalgia. 2008;28:832–841. doi: 10.1111/j.1468-2982.2008.01597.x. [DOI] [PubMed] [Google Scholar]
- 10.Ciancaglini R, Radaelli G. The relationship between headache and symptoms of temporomandibular disorder in the general population. J Dent. 2001;29:93–98. doi: 10.1016/s0300-5712(00)00042-7. [DOI] [PubMed] [Google Scholar]
- 11.Lim PF, Smith S, Bhalang K, et al. Development of temporomandibular disorders is associated with greater bodily pain experience. Clin J Pain. 2010;26:116–120. doi: 10.1097/AJP.0b013e3181c507ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marklund S, Wiesinger B, Wanman A. Reciprocal influence on the incidence of symptoms in trigeminally and spinally innervated areas. Eur J Pain. 2010;14:366–371. doi: 10.1016/j.ejpain.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Schokker RP, Hansson TL, Ansink BJ. The result of treatment of the masticatory system of chronic headache patients. J Craniomandib Disord. 1990;4:126–130. [PubMed] [Google Scholar]
- 14.Bergstrom I, List T, Magnusson T. A follow-up study of subjective symptoms of temporomandibular disorders in patients who received acupuncture and/or interocclusal appliance therapy 18–20 years earlier. Acta Odontol Scand. 2008;66:88–92. doi: 10.1080/00016350801978660. [DOI] [PubMed] [Google Scholar]
- 15.Ekberg E, Vallon D, Nilner M. Treatment outcome of headache after occlusal appliance therapy in a randomised controlled trial among patients with temporomandibular disorders of mainly arthrogenous origin. Swed Dent J. 2002;26:115–124. [PubMed] [Google Scholar]
- 16.Schiffman EL, Truelove EL, Ohrbach R, et al. The Research Diagnostic Criteria for Temporomandibular Disorders. I: Overview and methodology for assessment of validity. J Orofac Pain. 2010;24:7–24. [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson GC, Gonzalez YM, Ohrbach R, et al. The Research Diagnostic Criteria for Temporomandibular Disorders. VI: Future directions. J Orofac Pain. 2010;24:79–88. [PMC free article] [PubMed] [Google Scholar]
- 18.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 19.Schiffman EL, Ohrbach R, Truelove EL, et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: Methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain. 2010;24:63–78. [PMC free article] [PubMed] [Google Scholar]
- 20.Dworkin SF, LeResche L. Research Diagnostic Criteria for Temporomandibular Disorders: Review criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 21.Therneau TM, Atkinson B. [accessed June 2011];The RPART Package. 2005 http://roadrunner.cancer.med.umich.edu/comp/docs/R/rpart.pdf.
- 22.Fletcher RH, Wagner EH, Fletcher SW. Clinical Epidemiology: The Essentials. 3rd edn Williams & Wilkins; Baltimore: 1996. p. 276. [Google Scholar]
- 23.Laslett M, Aprill CN, McDonald B, et al. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10:207–218. doi: 10.1016/j.math.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Schwarzer AC, Derby R, Aprill CN, et al. The value of the provocation response in lumbar zygapophyseal joint injections. Clin J Pain. 1994;10:309–313. doi: 10.1097/00002508-199412000-00011. [DOI] [PubMed] [Google Scholar]
- 25.McFadden JW. The stress lumbar discogram. Spine (Phila Pa 1976) 1988;13:931–933. doi: 10.1097/00007632-198808000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Thevenet P, Gosselin A, Bourdonnec C, et al. pHmetry and manometry of the esophagus in patients with pain of the angina type and a normal angiography. Gastroenterol Clin Biol. 1988;12:111–117. [PubMed] [Google Scholar]
- 27.Janssens J, Vantrappen G, Ghillebert G. 24-hour recording of esophageal pressure and pH in patients with non-cardiac chest pain. Gastroenterology. 1986;90:1978–1984. doi: 10.1016/0016-5085(86)90270-2. [DOI] [PubMed] [Google Scholar]
- 28.Vaksmann G, Ducloux G, Caron C, et al. The ergometrine test: effects on esophageal motility in patients with chest pain and normal coronary arteries. Can J Cardiol. 1987;3:168–172. [PubMed] [Google Scholar]
- 29.Couppe C, Torelli P, Fuglsang-Frederiksen A, et al. Myofascial trigger points are very prevalent in patients with chronic tension-type headache: a double-blinded controlled study. Clin J Pain. 2007;23:23–27. doi: 10.1097/01.ajp.0000210946.34676.7d. [DOI] [PubMed] [Google Scholar]
- 30.Wise CM, Semble EL, Dalton CB. Musculoskeletal chest wall syndromes in patients with noncardiac chest pain: a study of 100 patients. Arch Phys Med Rehabil. 1992;73:147–149. [PubMed] [Google Scholar]
- 31.Kokkonen SM, Kurunlahti M, Tervonen O, et al. Endplate degeneration observed on magnetic resonance imaging of the lumbar spine: correlation with pain provocation and disc changes observed on computed tomography diskography. Spine. 2002;27:2274–2278. doi: 10.1097/00007632-200210150-00017. [DOI] [PubMed] [Google Scholar]
- 32.Kircos LT, Ortendahl DA, Mark AS, et al. Magnetic resonance imaging of the TMJ disc in asymptomatic volunteers. J Oral Maxillofac Surg. 1987;45:852–854. doi: 10.1016/0278-2391(87)90235-7. [DOI] [PubMed] [Google Scholar]
- 33.Katzberg RW, Westesson PL, Tallents RH, et al. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. 1996;54:147–153. doi: 10.1016/s0278-2391(96)90435-8. discussion 153–155. [DOI] [PubMed] [Google Scholar]
- 34.Tasaki MM, Westesson PL, Isberg AM, et al. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop. 1996;109:249–262. doi: 10.1016/s0889-5406(96)70148-8. [DOI] [PubMed] [Google Scholar]
- 35.Larheim TA, Westesson P, Sano T. Temporomandibular joint disk displacement: comparison in asymptomatic volunteers and patients. Radiology. 2001;218:428–432. doi: 10.1148/radiology.218.2.r01fe11428. [DOI] [PubMed] [Google Scholar]
- 36.Arima T, Svensson P, Arendt-Nielsen L. Experimental grinding in healthy subjects: a model for postexercise jaw muscle soreness? J Orofac Pain. 1999;13:104–114. [PubMed] [Google Scholar]
- 37.Jensen R. Pathophysiological mechanisms of tension-type headache: a review of epidemiological and experimental studies. Cephalalgia. 1999;19:602–621. doi: 10.1046/j.1468-2982.1999.019006602.x. [DOI] [PubMed] [Google Scholar]
- 38.Loder E, Rizzoli P. Tension-type headache. BMJ. 2008;336:88–92. doi: 10.1136/bmj.39412.705868.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The President's Conference on the Examination, Diagnosis and Management of Temporomandibular Disorders; Chicago: American Dental Association; 1983. [DOI] [PubMed] [Google Scholar]
- 40.Ohrbach R, List T, Goulet JP, et al. Recommendations from the International Consensus Workshop: convergence on an orofacial pain taxonomy. J Oral Rehabil. 2010;37:807–812. doi: 10.1111/j.1365-2842.2010.02088.x. [DOI] [PubMed] [Google Scholar]
- 41. [accessed June 2011];2004 http://www.rdc-twdinternational.org/OtherResources/ResearchProtocols.Aspx.
- 42.Stuginski-Barbosa J, Macedo HR, Bigal ME, et al. Signs of temporomandibular disorders in migraine patients: a prospective, controlled study. Clin J Pain. 2010;26:418–421. doi: 10.1097/AJP.0b013e3181d10691. [DOI] [PubMed] [Google Scholar]


