Abstract
Means for high-density multiparametric physiological mapping and stimulation are critically important in both basic and clinical cardiology. Current conformal electronic systems are essentially 2D sheets, which cannot cover the full epicardial surface or maintain reliable contact for chronic use without sutures or adhesives. Here we create 3D elastic membranes shaped precisely to match the epicardium of the heart via the use of 3D printing, as a platform for deformable arrays of multifunctional sensors, electronic and optoelectronic components. Such integumentary devices completely envelop the heart, in a form-fitting manner, and possess inherent elasticity, providing a mechanically stable bioti-/abiotic interface during normal cardiac cycles. Component examples range from actuators for electrical, thermal and optical stimulation, to sensors for pH, temperature and mechanical strain. The semiconductor materials include silicon, gallium arsenide and gallium nitride, co-integrated with metals, metal oxides and polymers, to provide these and other operational capabilities. Ex vivo physiological experiments demonstrate various functions and methodological possibilities for cardiac research and therapy.
Introduction
Tools for cardiac physiological mapping are indispensable for the clinical identification and understanding of mechanisms of excitation-contraction coupling, metabolic dysfunction, arrhythmia and others. Devices developed in the 1980s attempted to address this need by using synthetic fabrics sewn to loosely resemble the shape of the ventricle, with bulk electrodes manually assembled and woven into this platform1–4. Although such schemes provide some utility, they do not enable uniform quality of contact across the heart, practical deployment in clinical settings, high-density mapping capabilities, provision for multifunctional, precision measurement/stimulation or deployment as chronic implants. As a result, alternative strategies based on serial mapping with point-contact catheters or on imaging techniques that use fluorescence, nuclear magnetic resonance or ultrasound have emerged, even though each has significant shortcomings5–8.
The ideal scenario remains one in which device functionality integrates directly and non-invasively with the heart, suitable for long-term use. The essential challenge is that the heart is a complex electromechanical syncytium with numerous elements working in synchrony to reliably pump blood and respond to changing metabolic demands. Although much has been gained from isolated cellular studies, the integral functional behavior on the organ level and the interaction between the electrical, metabolic and mechanical remodeling in disease states, especially in vivo, remain poorly explored due to paucity of adequate tools. Thus there is an unmet need for multiparametric mapping capabilities inclusive but far beyond electrical sensing in a conformal, high-resolution manner, which cannot be realized using conventional materials, device technologies or imaging modalities.
Recent developments in materials and mechanics concepts for stretchable electronics9–14 create an opportunity to meet this challenge of direct, full 3D integration of devices with the epicardial surface. Here we expand on previously reported small-scale electronic devices as 2D flexible sheets15, to build multifunctional semiconductor systems in lithographically defined configurations on 3D, thin elastic membranes, custom-formed to match the shape of the heart. The physical format resembles that of the naturally occurring membrane that surrounds the heart, i.e. the pericardium. These systems, which we refer to as 3D multifunctional integumentary membranes (3D-MIMs) provide conformal interfaces to all points on the heart, with robust but non-invasive contacts enabled by the soft elasticity of the membrane itself, throughout dynamic cardiac cycles, even when completely immersed in fluid media. Measurements on isolated perfused rabbit hearts demonstrate the utility of these ideas as a general platform for multifunctional, high-density epicardial mapping/stimulation. The results provide advanced methodological possibilities for basic and clinical cardiology.
Results
Design and fabrication
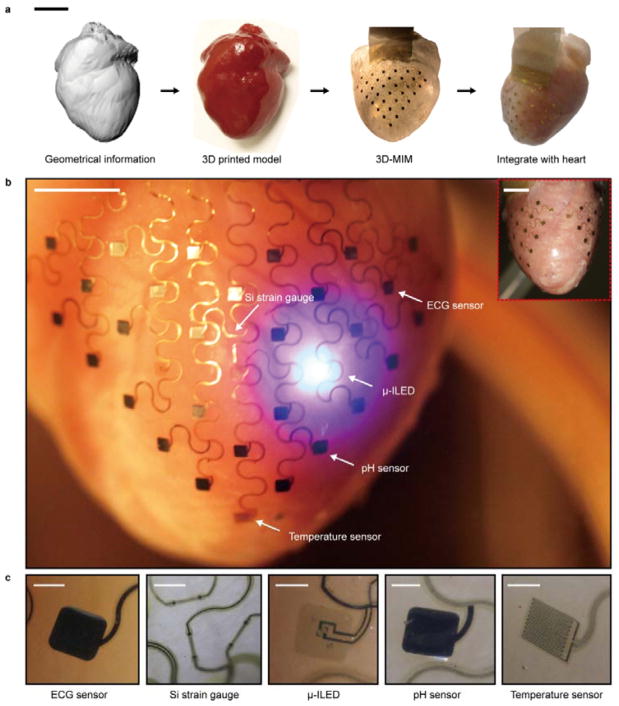
The fabrication begins with the creation of a thin, 3D elastic membrane shaped to the heart. As shown in Fig. 1a, optical segmentation techniques first capture the full 3D geometry of a heart of interest16. A commercial 3D printer (ZPrinter 450, Z-Corporation) then renders a solid model of the heart in a proportionally scaled form, as described later, to serve as a substrate for mounting ultrathin electronic/optoelectronic and sensor systems, separately prefabricated on planar substrates. Casting and curing a thin layer of silicone elastomer on top of the heart model with these multifunctional devices on its surface defines the overall format. The front faces of the device components contact the model while the back faces bond to the elastomer. Removing the system (i.e. 3D membrane with integrated device components) from the model prepares it for installation around a living heart, as a type of ‘instrumented’, artificial pericardium.
Figure 1. 3D-MIMs for spatiotemporal measurement and stimulation across the entire epicardial surface.
(a) Graphical depiction of the key steps in device design and fabrication. Scale bar: 2 cm. (b) Images of a representative 3D multifunctional integumentary membrane (3D-MIM) integrated on a Langendorff-perfused rabbit heart. The white arrows highlight various function elements in this system. The electronics can cover both anterior and posterior surfaces of the heart (inset). Scale bars: 6 mm. (c) Magnified views of the functional elements in conformal contact with the epicardium. The images are recorded from the back side of the devices. Scale bars: 500 μm.
Figure 1b shows a representative 3D-MIM that includes microscale, inorganic light emitting diodes (μ-ILEDs) based on indium gallium nitride (InGaN) for optical mapping, silicon (Si) nanomembranes for strain gauges, gold (Au) electrodes for electrical sensing/stimulation, iridium oxide (IrOx) pads for pH sensors and Au serpentine resistors for temperature sensors/heaters. The methods for creating these components exploit modern integrated circuit technologies and achieve spatial resolution far beyond that possible with manually assembled arrays. A thin, flexible heat-seal conductive cable (Elform, HST-9805-210) provides connection to external hardware for data acquisition, power supply and control. The 3D-MIM is engineered with overall dimensions slightly smaller than those of the real heart, to provide adequate elasticity and mechanical support for robust contact with the epicardium during diastole and systole, but with sufficiently small pressures to avoid disruption of natural behaviors of the cardiac tissue. The serpentine mesh that interconnects the device components covers the ventricle and conforms to the contours of the epicardium. Although this example is designed for research applications on rabbit hearts, the same strategies are applicable to human hearts, or even other organ systems. Here, the 3D geometries can be obtained using similar 3D printed substrates with patient specific MRI or CT organ segmentation.
Mechanical analysis
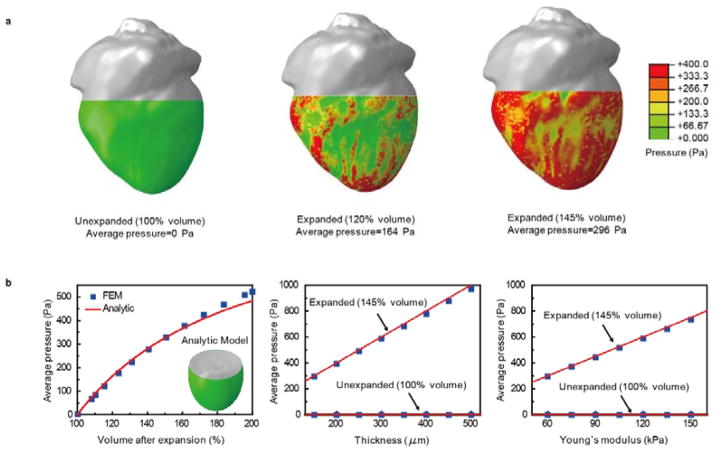
A critical feature of this type of device is that it can be designed to maintain a stable mechanical interface to the tissue while exerting minimal force on the contracting and relaxing heart muscle. In the cardiac anatomy of humans and other vertebrates, the myocardium is enclosed in a space sealed by the pericardium, which allows reversible volume change within a certain range. When a pathophysiological condition leads to inflammation, the pericardium exerts pressure to constrain the motions of the heart chambers. Quantitative analysis allows a comparative assessment of the pressure associated with our 3D device membrane on the epicardium, as well as the dependence of this pressure on materials properties and design parameters. Figure 2a shows results for a 3D-MIM with a membrane thickness of 150 μm and effective Young’s modulus of ~60 kPa (Ecoflex, Smooth-on) at various states of volume expansion (1+ε)3 of a heart geometry, calculated using 3D finite element methods (FEM), where ε is the linear expansion factor. The thickness of the membrane is uniform in the analysis; the nonuniformity due to the electronic devices results in local increase of the effective Young’s modulus to ~80 kPa and adds <50% of the approximate pressure, as discussed in details in Methods section and Supplementary Fig. 1. The form of the undeformed membrane follows that of a 3D model, proportionally size-reduced (~30% volume reduction comparing to the diastolic state of the real heart) to ensure a baseline level of pressure upon application on the real heart. Computations correspond to the heart at its contracted volume (3D model), and at systolic (120% of the contracted volume) and diastolic (145% of the contracted volume) conditions. The calculated average pressures are similar to those of pericardium under normal physiological conditions, and only ~20% of these pressures under conditions of pericardial constraint17–22. The results suggest that the device is unlikely to cause restrictive impact, as confirmed by ex vivo studies described subsequently. FEM and analytic modeling also establish general relationships between the pressure and the design parameters. Figure 2b shows the average pressure as a function of the volume expansion, the thickness of the membrane and its Young’s modulus. The analytic model uses a partial ellipsoid to approximate the geometry of the heart. Details appear in Methods section and Supplementary Fig. 1. The following expression connects the average pressure, the membrane geometry, mechanical properties and expansion factor:
| (1) |
where t is the thickness of the membrane, E and ν are the effective Young’s modulus and the Poisson’s ratio, respectively. The constant C decreases as the heart size increases, and C also depends on the shape of the heart (~0.2 mm−1 for a rabbit heart). Decreases in membrane thicknesses and Young’s moduli both linearly reduce the pressure. This scaling allows designs that provide pressures sufficiently large to maintain good contact between the sensor/actuator network and the epicardial surface, but sufficiently small to avoid impact on the intrinsic physiology. Monitoring the time course of several electrophysiological parameters that indicate ischemia in an isolated pressure loaded, working rabbit heart model23 with and without a 3D-MIM reveals the effects. The results, based on control (N=3) and experimental (N=3) hearts (Supplementary Fig. 2), suggest that there is no additional ischemia caused by the devices, as measured by ST elevation and the amplitude of the LV pressure waveform.
Figure 2. Analysis of pressures on the epicardium associated with integration of a 3D-MIM.
(a) Calculated pressure distribution induced by a device with total thickness of 150 μm and effective Young’s modulus of 60 kPa under various conditions of volume expansion of a heart geometry. (b) FEM and analytical results of average pressure as functions of volume expansion (left), thickness (middle) and Young’s modulus (right) of the membrane.
Spatiotemporal cardiac measurements and stimulation
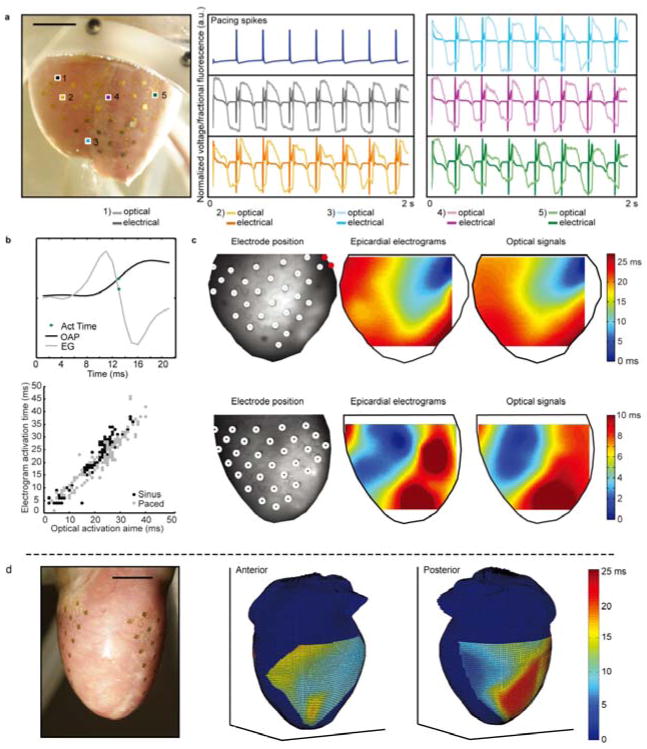
To demonstrate the various functional modes of operation we begin with high precision mapping of epicardial electrical activity. These experiments, and all of those that follow, used explanted Langendorff-perfused rabbit hearts. The 3D geometrical information was obtained from a representative rabbit heart. A single 3D-MIM can accommodate some range in specific sizes and shapes associated with a single type of animal model, due to its soft, elastic construction. The device here incorporates 68 Au electrodes (1 mm2 surface area and spacing of 3.5 mm), distributed across both the anterior and posterior surfaces of the epicardium (Fig. 3a, d, and Supplementary Fig. 3). The electrochemical impedances of individual electrodes are ~2 kΩ at frequency of 1 kHz, measured in phosphate buffered saline (Supplementary Fig. 4). The transparency of the membrane allows simultaneous optical mapping through voltage dependent fluorescence, as a means for validating the electrical measurements5. Experiments involved signals acquired from 4 hearts for a variety of conditions: normal sinus rhythms, and paced at a range of frequencies and from a range of electrode pairs to increase the variability of the propagation patterns in the spatial activation maps. The surface electrograms captured various key morphologies associated with the QRS and T waves (Fig. 3a). Representative maps and correlations between electrical and optical activation times appear in Fig. 3c and 3b, respectively. The overall linear correlations between optical and electrical activation times were 0.957 for sinus data and 0.943 for paced data. These studies indicate that this configuration of measurement electrodes can replicate patterns of activation to a resolution that captures the spatial variations observed optically. Analyses for additional electrophysiological parameters are summarized in Supplementary Fig. 6. Figure 3d presents a 3D map derived from signals recorded from both anterior and posterior surface of the heart. Unlike optical mapping where motion artifacts dramatically impact the measurement quality and static heart geometries are required, electrophysiological mapping with 3D-MIMs can be applied under normal beating condition. As shown in Supplementary Video, the integrated sensors move synchronously with the underlying cardiac tissue. Although it is practically difficult to avoid relative lateral motion between the sensors and the epicardium during beating cycles, due to the engineered geometries of 3D-MIMs, the displacement can be minimized to be less than the characteristic sizes of the sensors and to have negligible impact to the signal quality (Supplementary Fig. 5). This feature is necessary for extending the mapping capabilities beyond laboratory studies and implementing in clinical electrophysiology.
Figure 3. High-density electrical mapping.
(a) Representative optical and electrical signals acquired simultaneously from the corresponding numbered electrode locations on a Langendorff-perfused rabbit heart. Scale bar: 7 mm. (b) Top: schematic illustration of a representative optical action potential (OAP), unipolar electrogram (EG) and position of the activation time, defined as for the OAP and for the EG. Bottom: correlation of electrical and optical activation times for hearts tested in a variety of states. (c) Interpolated spatial activation maps determined from the electrical and optical measurements. Top: heart paced by the red pair of electrodes on the membrane. Bottom: sinus rhythm. (d) 3D mapping of electrical signaling from both the anterior and posterior surfaces of the heart. Interpolated spatial maps of electrical activation time are projected on a representative rabbit heart geometry, for purposes of visualization. Scale bar: 7 mm.
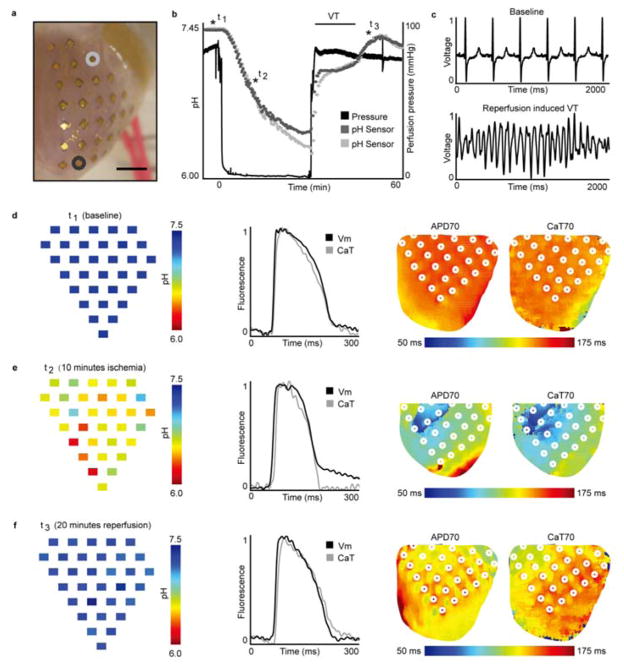
Mapping of changes in pH provides useful information on the metabolic state of the heart. Here, iridium oxide (IrOx), a well-established material for pH sensing, enables the measurement24. Electrodeposited IrOx on Au electrodes provides pH sensors with average open circuit potential (OCP) responses of 68.9 mV/pH with standard deviation of 8.6 mV/pH for 32 sensors over the array at 37 °C in Tyrode’s solution (Supplementary Fig. 7). The temperature dependence of the pH sensors is ~−1.6 ± 0.02 mV/° C (μ±σ), which corresponds to ~0.02 pH for a 1 ° C change in temperature. Temperature variations over a physiologically relevant range will, therefore, have a small effect on the pH measurement. For cases where large changes in temperature are externally introduced, the temperature dependence of the pH sensor must be accounted for explicitly. Such pH sensors, along with optical mapping techniques, enable acquisition of maps of pH, transmembrane potential (Vm), and calcium transient (CaT) signals during global no-flow ischemia-reperfusion. The pH sensors cover the left anterior and posterior surface of the rabbit heart (Fig. 4a). At baseline, all pH sensors record values between 7.34 and 7.40. The responses of two pH sensors (highlighted by grey and charcoal colors) are plotted (Fig. 4b.) throughout the protocol. Complete spatial pH maps at time points t1 (baseline), t2 (10 minutes into ischemia), and t3 (20 minutes into reperfusion) appear in Fig. 4d–e (left). Turning off the perfusion pump immediately reduced coronary pressure to 0 mmHg and led to an approximately linear decrease in pH to minimum values of 6.40 (grey) and 6.22 (charcoal). Upon reperfusion, the pH rapidly increased until initiation of ventricular tachycardia (VT) where the pH stabilized at levels somewhat below baseline values. A sample far-field ECG of reperfusion-induced VT appears in Fig. 4c. After spontaneous conversion back to sinus rhythm, the pH values increased again to pre-ischemic values. Figure 4d–f shows pH maps (left), representative optical signals (Vm—black and CaT—grey; middle) and side-by-side action potential duration at 70% repolarization (APD70) and calcium transient duration at 70% return to baseline (CaT70) maps. At the baseline, pH, APD70, and CaT70 maps highlight that the pH and electrophysiological parameters were initially uniform over the surface of the heart. After 10 minutes of ischemia, pH, APD70, CaT70 changed, though not in a spatially uniform manner. CaT alternans (short and long duration) were observed during ischemia and here we show a short CaT70 in Figure 4e. After 20 minutes of reperfusion, parameters returned to values close to the baseline levels. This experiment demonstrates possibilities in multiparametric mapping during ischemia/reperfusion. The information establishes anatomical relationships between metabolism and excitation-contraction coupling.
Figure 4. High-density pH and optical mapping of transmembrane potential and calcium transients.
(a) 3D-MIM with pH sensors array integrated on a Langendorff-perfused rabbit heart with 2 pH sensors highlighted and values displayed in (b). Scale bar: 7 mm. (b) Temporal change in pH during 30 minutes of no-flow ischemia followed by 30 minutes of reperfusion. Three times starred as t1, t2, and t3 correspond to spatial pH maps in (d–f). (c) Representative far-field ECG during baseline and reperfusion induced VT. (d–f) pH map of 32 sensors (left), representative transmembrane potential and calcium transient signals (middle), and APD70—CaT70 maps (right) at baseline (d), 10 minutes of no-flow ischemia (e), and 20 minutes of reperfusion (f). The results provide maps of the anterior-posterior LV. The Vm and CaT are taken from the same pixel, but the location may vary slightly due to shrinkage of the heart during no-flow ischemia. White circles denote pH sensors positions. VT, ventricular tachycardia; Vm, transmembrane potential; CaT, calcium transient; APD70, action potential duration at 70% repolarization; CaT70, calcium transient duration at 70% relaxation.
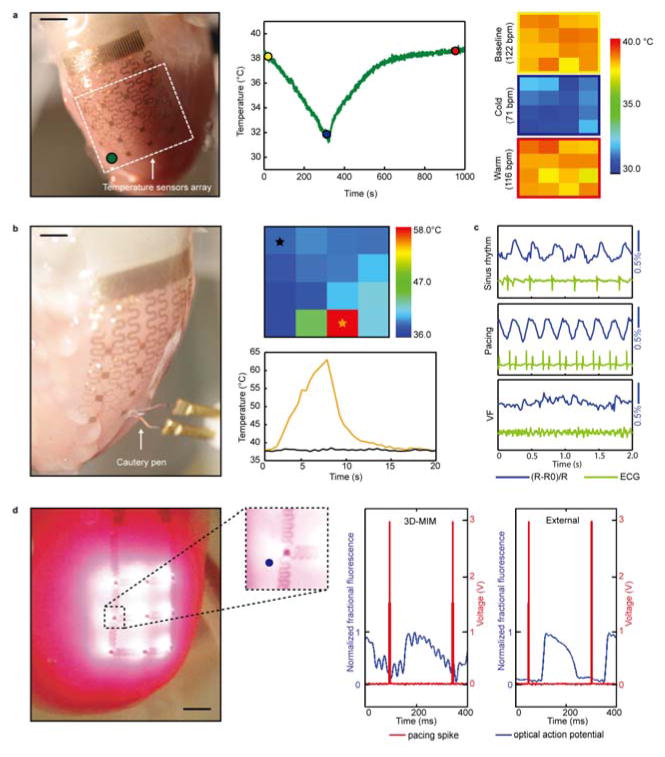
A 3D-MIM with arrays of temperature sensors illustrates capabilities in monitoring spatial distributions of cardiac temperature. The temperature sensor elements use designs established previously, consisting of serpentine traces of gold (20 μm wide, 50 nm thick) (Supplementary Fig. 8) in which changes in resistance correlate to changes in temperature25. The temperature sensors exhibit linear responses over physiological range, with a measurement precision of ~23 mK when sampled at 2 Hz in typical hospital settings. Figure 5a shows a 3D-MIM with 16 integrated temperature sensors during use on a beating heart. The sensors are calibrated in temperature controlled water bath before the animal experiments, exhibiting average responses of 1.23Ω/° C with standard deviation of 0.05 Ω/° C over 16 sensors across the array (Supplementary Fig. 9). In one experiment, the temperature of the heart was changed by altering the temperature of the perfusion. As shown in Fig. 5a, the measured epicardial temperature gradually decreased by ~7 ° C during cooling of the perfusate, with a uniform distribution of temperature across the heart. The heart rate, determined from the far-field electrogram, decreased with decreasing temperature and recovered to the original value as the temperature returned to physiological levels, indicating temperature controlled rate of myocardial metabolism. In a second experiment, a cautery pen was used to acutely burn a small region of the epicardium, simulating clinical ablation. The associated temperature map (Fig. 5b) shows localized elevation of temperature near the point of ablation. Such information can be used as feedback for clinical control of ablation time and size of affected area. In combination with electrical sensors, such device could provide real-time relation between temperature and excitation.
Figure 5. Temperature and strain sensing combined with imaging using integrated μ-ILEDs.
(a) Application of a 3D-MIM for temperature monitoring during cold perfusion. Left: image of a 3D-MIM with 4 x 4 temperature sensors array integrated on a Langendorff-perfused rabbit heart. Middle: temperature recordings from a representative sensor illustrated in the left inset. Right: temperature maps at representative time points in the middle inset with corresponding heart rate calculated from ECG. Each pixel in the color map corresponds to recording from one temperature sensor. Scale bar: 1 cm. (b) Temperature measurements during an ablation experiment. Positions of the sensors array and cautery pen are shown in the left inset. Temperature map during ablation (upper right) and recordings from representative sensors (bottom right) are shown respectively. Scale bar: 7 mm. (c) Responses of a Si strain sensor under representative physiological conditions, compared with simultaneous ECG recordings. (d) Left: image of a 3D-MIM with μ-ILEDs array in optical mapping experiments. Inset shows a magnified view of area around a representative μ-ILED. Right: comparison of optical signals from a representative pixel (blue dot on the left inset) recorded during excitation using μ-ILEDs on 3D-MIM and external optical excitation, respectively. Scale bar: 3 mm.
In addition to electrical and chemical evaluation, mechanical characteristics can be determined. Here, strain sensors based on piezoresistive effects in nanomembranes of Si allow monitoring of the mechanics of contractions of the heart during a variety of propagation states. Careful mechanical design of the serpentine interconnect structures allow accurate measurement in spite of the fact that typical epicardial strains26 greatly exceed the fracture threshold of Si, as described in previously reported small-scale 2D devices15. In the present design, the 3D-MIM strain sensors include three p-doped Si piezoresistors in a rosette configuration (Supplementary Fig. 10). Two of the piezoresistors, with longitudinal axes perpendicular to each other, are aligned to the <110> crystalline directions of the Si, offering effective longitudinal gauge factor of ~0.33 and effective transverse gauge factor of ~−0.06 for each piezoresistor (Supplementary Fig. 11). The other piezoresistor is aligned to the <100> crystalline direction and exhibit relatively small changes in resistance under strain, due to the intrinsic sensitivity associated with the crystalline direction as well as the overall device geometry. The piezoresistors aligned to the <110> directions provide maximum sensitivity for characterization of mechanical rhythms of the heart while the piezoresistor aligned to the <100> direction can be used to calibrate for effects of temperature. Experiments revealed the mechanical behaviors during sinus rhythm, ventricular pacing, and pharmacologically induced ventricular fibrillation (VF) with Pinacidil (30μM bulk dose). The use of Pinacidil significantly reduces the action potential duration and subsequently increases the vulnerability to reentrant arrhythmias when stimulated with 50Hz A/C burst pacing. Bath electrodes simultaneously recorded a far-field ECG to establish the temporal correlation between the electrical and mechanical behavior. Figure 5c shows the response of a representative piezoresistor aligned to the <110> direction. The measurements reveal mechanical rhythms of the cardiac cycles, with consistent cycling with ECG recordings. During VF condition, both the strain gauges and ECG show that the waveform lost normal rhythm and displayed a random pattern typical for VF.
A final demonstration exploits arrays of μ-ILEDs27, 28 to illustrate the capacity for advanced semiconductor integration and optical mapping/stimulation. Here, nine ultrathin (3 μm), microscale (300×300 μm2) light emitting diodes (LEDs) based on aluminum indium gallium phosphide (AlInGaP) with peak emission wavelengths of 670 nm (Supplementary Fig. 12 and S13) served as local light sources for excitation of voltage sensitive dyes. Changes in fluorescence associated with these dyes allowed measurement of the cardiac action potential. Figure 5d compares signals obtained with an external light source (Prizmatix, 630nm) and with the integrated μ-ILEDs. In spite of their small sizes, the LEDs enable recording of clear action potentials, with waveform shapes consistent with external light. The signal to noise ratio of the μ-ILED excited action potentials is lower than the externally excited action potentials due to a necessary decrease in light intensity to minimize the power delivered to the device. The results demonstrate the future possibility of an in vivo optical mapping using either externally applied dyes or internal fluorescent indicators and/or stimulation system in a 3D integration format.
Discussion
The results presented here suggest routes for integrating active electronic materials and sensors in 3D, organ—specific designs, with potential utility in both biomedical research and clinical applications. With attention to materials, engineering mechanics and functional devices, these systems can establish conformal interfaces with the epicardium, and perform a variety of high density physiological multiparametric mapping and stimulation. The use of transfer printing and the reported scheme for integration onto the printed 3D heart structure allows diverse sensor/actuator devices on a single platform. Separate electrical connection, with a single trigger channel to synchronize the timing, eliminates effects of crosstalk. The devices can provide local information on the metabolic, excitable, ionic, contractile, and thermal state for investigations of both the spatial and temporal responses to a variety of insults, diseases, and therapies. The devices could be used to identify critical regions that indicate the origin of pathophysiological conditions such as arrhythmias, ischemia, or heart failure. These regions could then be used to guide therapeutic interventions. The techniques in microfabrication, transfer printing and 3D shape definition are scalable to larger sizes and smaller, denser arrays of sensors. To increase the resolution and numbers of sensors, it may be necessary to incorporate transistors into the device to allow multiplexed addressing. Remaining challenges for use as a chronic implant include means for power supply, control/communication, and encapsulation. However, these approaches present a promising opportunity to design and implement high definition implantable devices for diagnostics and therapy of lethal heart diseases.
Methods
Fabrication of 3D-MIMs
The process, detailed in Supplementary Methods, starts with standard planar processing of inorganic semiconductor materials (Si, InGaN or AlInGaP) followed by transfer printing onto substrates coated either with a bilayer of polyimide (PI) on poly(methyl methacrylate) (PMMA) or poly(ethylene terephthalate) (PET) on poly(dimethylsiloxane) (PDMS)15, 27–30. Dissolution of the PMMA or delamination from the PDMS allows release of the devices. Metal layers (Cr/Au) are vacuum deposited and patterned to form interconnects, resistors and electrodes. Application and patterning of a polymer encapsulation layer (PI or a photosensitive epoxy, SU8) on top of the devices completes their fabrication. Transfer printing delivers the resulting structures to a thin film of a low modulus silicone elastomer (Ecoflex, Smooth-on). A flexible conductive cable (Elform) bonded to contact pads at the periphery provides an interface to external hardware. A lamination process attaches the devices to a desired 3D printed model of the heart, with the sensors in direct contact with the surface. Casting and curing another layer of the same type of elastomer defines the overall 3D geometry of the system. In some cases, elastomer straps molded enhanced the maneuverability for use in Langendorff-perfused heart experiments (Supplementary Fig. 14). Additional openings in the membrane can be included to prevent fluid build-up associated with flow in the supporting bath. Removal from the model allows electrodeposition of IrOx on to yield pristine surfaces for precision pH sensing.
Mechanical analysis
Numerical analysis by 3D FEM
The 3D FEM is used to study the pressure between the 3D-MIM and the heart for a wide range of device parameters and the expansion of the heart. The 3D geometric model of the heart is reconstructed from the data obtained with optical segmentation. The geometric model is imported into the pre-processor in the ABAQUS finite element program32. The heart and the 3D-MIM are modeled by the 4-node, linear tetrahedron solid element C3D4 and the 4-node quadrilateral membrane element M3D4 in ABAQUS, respectively. The total number of elements exceeds 60,000, and mesh refinement ensures the accuracy of the numerical results. For the prescribed expansion of the heart, FEM gives the pressure distribution at the interface between the 3D-MIM and the heart. The average pressure is then obtained over the contact area between the 3D-MIM and the heart, i.e. the ventricles of the heart as in the experiment, as shown in Fig. 2a.
The pressure
The part of the heart that is covered by the 3D-MIM (Fig. 2a) is approximately a partial axisymmetric ellipsoid with the lengths a and b of semi-principal axes, as shown in Supplementary Fig. 1. The 3D-MIM on the heart surface is modeled as a membrane, which deforms from Z2/a2 +R2/b2= 1 when being fabricated on the model to z2/[(1+ε)2 a2] + r2/[(1+ε)2 b2] = 1 due to the linear expansion ε of the heart, where (Z, R) and (z,r)=[(1+ε)Z, (1+ε)R] are axial and radial coordinates of the 3D-MIM without and with expansion in the axisymmatric coordinates, respectively. The plane stress state of the 3D-MIM with biaxial linear strain ε gives the biaxial stress as Eε/(1−ν), where E and ν are the Young’s modulus and the Poisson’s ratio of the 3D-MIM, respectively. The membrane force, accounting for the change of length due to linear expansion, is
| (2) |
where t is the thickness of the 3D-MIM. For a planar curve r=r(z), the principal curvature along the meridional direction is −(dr2/dz2)/[1+(dr/dz)2]3/2 at any point (z, r) on the surface. The other principal curvature along the circumferential direction is given by . For z = (1+ε)Z and r = (1+ε)R, the two principal curvatures are given by
| (3) |
The pressure on the heart is obtained in terms of the membrane tension and curvatures as in Ref. 33.
| (4) |
Its average over the part of (Z0 ≤ Z ≤ a, Supplementary Fig. 1a) of the ellipsoid surface that is in contact with the heart is by
| (5) |
This gives Eq. (1) in the main text, and
| (6) |
For a = 15 mm, b = 0 mm and X0 = −5.5 mm, which best fit the geometric model of the heart, the average pressure in Eq. (1) agrees well with the 3D FEM results, as shown in Fig. 2b.
The analysis above does not account for the effect of electronic devices on the pressure between the 3D-MIM and heart. Such an effect can be estimated from Eq. (1) by replacing the tensile stiffness Et of the 3D-MIM with the effective tensile stiffness of the 3D-MIM with the electronic devices. The inset in Supplementary Fig. 1b shows an electronic device on a sheet of the membrane material (62.8×24.3×0.15 mm3), consisting of the interconnects and electrodes. All of the interconnects consist of the Au: 120nm/Cr: 2nm composite layer sandwiched by 1.2 μm-thick polyimide (PI) layers on each side. The cross section of the electrodes is similar to that of interconnects but without the top 1.2μm-thick PI layer to expose Au. The sheet is modeled by the 8-node solid element C3D8R, and interconnects and electrodes are modeled by the 4-node shell element S4R in ABAQUS, respectively. FEM gives its tensile stiffness to be approximately 1.5 times that without the electronic devices, as shown in Supplementary Fig. 1b.
Animal Experiments
Experiments were conducted in accordance with the ethical guidelines of the National Institutes of Health and with the approval of the Institutional Animal Care and Use Committee of Washington University in St Louis. Briefly the heart is removed via a thoracotomy and a cannula is placed in the aorta to allow retrograde perfusion of oxygenated Tyrode’s solution. The perfusion mimics the electrolyte balance within the animal and provides an energy substrate for the heart to continue to function normally from an electrical perspective. The heart is submerged in a perfusion chamber maintained at 37°C with a pH in the range of 7.35–7.45, controlled by oxygen flow. The optical signals of transmembrane potential (Vm) and calcium transients (CaT) rely on the collection of fluorescent signals from a potentiometric dye (di-4 ANEPPS or RH-237) or calcium indicator (Rhod-2a) added to the perfusate with a CMOS camera; when needed to avoid motion artifacts an excitation-contraction uncoupler (Blebbistatin) is also added to the perfusate. Supplementary Fig. 15 illustrates representative experimental settings.
Data acquisition and processing
Electrophysiology
The electrical signals are recorded from the Au electrodes on the 3D-MIMs with a 240-channel unipolar electrogram acquisition system (Astrocard, Boston) and a custom-built interface. Both the optical and electrical signals are collected at a sampling frequency of 1 kHz, aligned with a trigger TTL pulse and post-processed separately in custom MATLAB software. Post-processing: The electrical signals acquired from the 3D-MIMs are first filtered with a 60 Hz notch filter internal to the acquisition software, then the electrophysiological parameter of interest activation time is calculated (Fig. 3c) and aligned to the spatial coordinates of the electrodes based on the optical background file. The optical signals are binned, filtered and normalized as previously described31. A spatial 3x3 binning filter is applied, as well as a 100 Hz low pass digital filter, and the amplitude of the fractional fluorescence is normalized to between 0 and 1 for each pixel’s temporal sequence. The electrophysiological parameters are calculated for the complete field of view. To create the spatial maps, the activation times are interpolated using MATLAB’s internal function for cubic interpolation of scattered data. The optical map is also sampled at the coordinates of the electrodes and the same interpolation method is applied to compare the full resolution optical pattern with the sampled optical map and the electrical map. pH data: pH data were acquired using measurement of open circuit potential of each sensor reference to an Ag/AgCl electrode, using Gamry Reference 600 potentiostat. A custom made relay system was used for multiplexing.
Temperature and strain
Data for temperature and strain sensors is acquired with measurements of resistance of each sensor using a custom built system based on National Instruments PXI-6289 board. The resistance of each of the 16 sensors is recorded simultaneously with a 160 μA probe current, a 16-bit A/D converter and a 15 ms sampling period at each sensor.
Supplementary Material
Acknowledgments
This material is based upon work supported by the NIH grants R01 HL115415, R01 HL114395, and R21 HL112278, and through the Frederick Seitz Materials Research Laboratory and Center for Microanalysis of Materials at the University of Illinois at Urbana-Champaign. L. X. acknowledges support from China Scholarship Council. R. C. W. acknowledges support from the National Science Foundation under Grant No. DGE-1144245. H. C. is a Howard Hughes Medical Institute International Student Research fellow. The authors would like to thank Byung-Gik Kim and Hsin-Yun Chao for the help on device fabrication and data processing.
Footnotes
Author contributions
L.X., S.R.G., A.P.B., M.S.S., N.L., H-J.C., I.R.E. and J.A.R. designed the experiments. L.X., A.P.B., N.L., H-J.C., K-I.J., M.Y., C.L., R.C.W., J-S.K., A.A., J-W.J., G.-T.K. and J.A.R. carried out the devices fabrication and characterization. L.X., S.R.G., A.P.B., M.S.S., N.L., H-J.C, K-I.J., M.Y., C.L., R.C.W., J-S.K., J.I.L., Y.L., J-W.J. and I.R.E carried out the animal experiments and data analysis. L.X., Y.S., Z.L., H.C., Y.H. and J.A.R. contributed to the mechanical modeling of the system. L.X., S.R.G., Y.S., M.S.S., H-J.C., Y.H., I.R.E. and J.A.R. co-wrote the paper.
Competing financial interests
The authors declare no competing financial interests.
References
- 1.Harrison L, et al. The sock electrode array - a tool for determining global epicardial activation during unstable arrhythmias. Pacing Clin Electrophysiol. 1980;3:531–540. doi: 10.1111/j.1540-8159.1980.tb05272.x. [DOI] [PubMed] [Google Scholar]
- 2.Worley SJ, et al. A new sock electrode for recording epicardial activation from the human heart - one size fits all. Pacing Clin Electrophysiol. 1987;10:21–31. doi: 10.1111/j.1540-8159.1987.tb05921.x. [DOI] [PubMed] [Google Scholar]
- 3.Farid TA, et al. Role of K-ATP channels in the maintenance of ventricular fibrillation in cardiomyopathic human hearts. Circ Res. 2011;109:1309–U1301. doi: 10.1161/CIRCRESAHA.110.232918. [DOI] [PubMed] [Google Scholar]
- 4.Faris OP, et al. Novel technique for cardiac electromechanical mapping with magnetic resonance imaging tagging and an epicardial electrode sock. Ann Biomed Eng. 2003;31:430–440. doi: 10.1114/1.1560618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Efimov IR, Nikolski VP, Salama G. Optical imaging of the heart. Circ Res. 2004;95:21–33. doi: 10.1161/01.RES.0000130529.18016.35. [DOI] [PubMed] [Google Scholar]
- 6.Rieke V, Pauly KB. MR thermometry. J Magn Reson Imaging. 2008;27:376–390. doi: 10.1002/jmri.21265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan KWY, et al. MRI-detectable pH nanosensors incorporated into hydrogels for in vivo sensing of transplanted-cell viability. Nat Mater. 2013;12:268–275. doi: 10.1038/nmat3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’hooge J, et al. Regional strain and strain rate measurements by cardiac ultrasound: Principles, implementation and limitations. Eur J Echocardiogr. 2000;1:154–170. doi: 10.1053/euje.2000.0031. [DOI] [PubMed] [Google Scholar]
- 9.Sekitani T, et al. A rubberlike stretchable active matrix using elastic conductors. Science. 2008;321:1468–1472. doi: 10.1126/science.1160309. [DOI] [PubMed] [Google Scholar]
- 10.Kaltenbrunner M, et al. An ultra-lightweight design for imperceptible plastic electronics. Nature. 2013;499:458–463. doi: 10.1038/nature12314. [DOI] [PubMed] [Google Scholar]
- 11.Lipomi DJ, et al. Skin-like pressure and strain sensors based on transparent elastic films of carbon nanotubes. Nature Nanotech. 2011;6:788–792. doi: 10.1038/nnano.2011.184. [DOI] [PubMed] [Google Scholar]
- 12.Yao HF, Shum AJ, Cowan M, Lahdesmaki I, Parviz BA. A contact lens with embedded sensor for monitoring tear glucose level. Biosens Bioelectron. 2011;26:3290–3296. doi: 10.1016/j.bios.2010.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim DH, et al. Epidermal electronics. Science. 2011;333:838–843. doi: 10.1126/science.1206157. [DOI] [PubMed] [Google Scholar]
- 14.Kim DH, et al. Materials for multifunctional balloon catheters with capabilities in cardiac electrophysiological mapping and ablation therapy. Nature Mater. 2011;10:316–323. doi: 10.1038/nmat2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim DH, et al. Electronic sensor and actuator webs for large-area complex geometry cardiac mapping and therapy. Proc Natl Acad Sci USA. 2012;109:19910–19915. doi: 10.1073/pnas.1205923109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lou Q, Li WW, Efimov IR. The role of dynamic instability and wavelength in arrhythmia maintenance as revealed by panoramic imaging with blebbistatin vs. 2,3-butanedione monoxime. Am J Physiol Heart Circ Physiol. 2012;302:H262–H269. doi: 10.1152/ajpheart.00711.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holt JP, Rhode EA, Kines H. Pericardial and ventricular pressure. Circ Res. 1960;8:1171–1181. doi: 10.1161/01.res.8.6.1171. [DOI] [PubMed] [Google Scholar]
- 18.Hancock EW. Subacute effusive-constrictive pericarditis. Circulation. 1971;43:183. doi: 10.1161/01.cir.43.2.183. [DOI] [PubMed] [Google Scholar]
- 19.Smiseth OA, Frais MA, Kingma I, Smith ER, Tyberg JV. Assessment of pericardial constraint in dogs. Circulation. 1985;71:158–164. doi: 10.1161/01.cir.71.1.158. [DOI] [PubMed] [Google Scholar]
- 20.Tyberg JV, et al. The relationship between pericardial pressure and right atrial pressure - an intraoperative study. Circulation. 1986;73:428–432. doi: 10.1161/01.cir.73.3.428. [DOI] [PubMed] [Google Scholar]
- 21.deVries G, Hamilton DR, Ter Keurs HEDJ, Beyar R, Tyberg JV. A novel technique for measurement of pericardial pressure. Am J Physiol Heart Circ Physiol. 2001;280:H2815–H2822. doi: 10.1152/ajpheart.2001.280.6.H2815. [DOI] [PubMed] [Google Scholar]
- 22.Shabetai R. Pericardial effusion: Haemodynamic spectrum. Heart. 2004;90:255–256. doi: 10.1136/hrt.2003.024810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neely JR, Lieberme H, Battersb Ej, Morgan HE. Effect of pressure development on oxygen consumption by isolated rat heart. Am J Physiol. 1967;212:804–814. doi: 10.1152/ajplegacy.1967.212.4.804. [DOI] [PubMed] [Google Scholar]
- 24.Chung H-J, et al. Stretchable, multiplexed pH sensors with demonstrations on rabbit and human hearts undergoing ischemia. Adv Healthc Mater. doi: 10.1002/adhm.201300124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Webb RC, et al. Ultrathin conformal devices for precise and continuous thermal characterization of human skin. Nature Mater. 2013;12:938–944. doi: 10.1038/nmat3755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moore CC, Lugo-Olivieri CH, McVeigh ER, Zerhouni EA. Three-dimensional systolic strain patterns in the normal human left ventricle: Characterization with tagged MR imaging. Radiology. 2000;214:453–466. doi: 10.1148/radiology.214.2.r00fe17453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim RH, et al. Waterproof AlGaInP optoelectronics on stretchable substrates with applications in biomedicine and robotics. Nature Mater. 2010;9:929–937. doi: 10.1038/nmat2879. [DOI] [PubMed] [Google Scholar]
- 28.Kim RH, et al. Flexible vertical light emitting diodes. Small. 2012;8:3123–3128. doi: 10.1002/smll.201201195. [DOI] [PubMed] [Google Scholar]
- 29.Ahn JH, et al. Heterogeneous three-dimensional electronics by use of printed semiconductor nanomaterials. Science. 2006;314:1754–1757. doi: 10.1126/science.1132394. [DOI] [PubMed] [Google Scholar]
- 30.Kim HS, et al. Unusual strategies for using indium gallium nitride grown on silicon (111) for solid-state lighting. Proc Natl Acad Sci USA. 2011;108:10072–10077. doi: 10.1073/pnas.1102650108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laughner JI, Ng FS, Sulkin MS, Arthur RM, Efimov IR. Processing and analysis of cardiac optical mapping data obtained with potentiometric dyes. Am J Physiol Heart Circ Physiol. 2012;303:H753–H765. doi: 10.1152/ajpheart.00404.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dassault Systèmes Abaqus analysis user’s manual v.6.10. Dassault Systèmes Simulia Corp; Rhode Island: 2010. [Google Scholar]
- 33.Timoshenko S, Woinowsky-Krieger S. Theory of Plates and Shells. McGraw-Hill; Kogakusha: 1959. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.