Abstract
Objective
To assess the prevalence, symptom severity, functional impairment, and treatment of major depressive episode (MDE) in the Iraqi general population.
Methods
The Iraq Mental Health Survey is a nationally representative face-to-face survey of 4,332 non-institutionalized adults aged 18+ interviewed in 2006–2007 as part of the WHO World Mental Health Surveys. Prevalence and correlates of DSM-IV MDE were determined with the WHO Composite International Diagnostic Interview (CIDI).
Findings
Lifetime and 12-month prevalence of MDE were 7.4% and 4.0%, respectively. Close to half (46%) of the 12-month MDE cases were severe/very severe. MDE was more common among women and those previously married. Median age of onset was 25.2. Only one-seventh of 12-month MDE cases received treatment despite being associated with very substantial role impairment (on average 70 days out of role in the past year).
Conclusions
MDE is a commonly occurring disorder in the Iraqi general population and is associated with considerable disability and low treatment. Efforts are needed to decrease the barriers to treatment and to educate general medical providers in Iraq about the recognition and treatment of depression.
Introduction
In the past decades, there has been a rapid demographic and epidemiological transition in the Arab world that encompasses a significant increase of non-communicable diseases, with mental disorders–and especially depressive disorders–as conditions that merit attention from both policy planners and clinicians [1,2]. Globally, depression is ranked the 11th leading cause of Disability Adjusted Life Years worldwide, but, interestingly, the 3th in the Middle East region [3]. Despite the fact that depression is less extensively studied in the Arab and the Middle Eastern countries, there are indications that the disorder is quite common in the region. General population studies have been carried out in quite a number of Arab and Middle Eastern countries [4–14]. Based on these studies, median 12-month and lifetime estimates of depression (both Major Depressive Disorder [MDD] and Major Depression Episode [MDE]) are 4.7 and 8.9%, respectively. Depressive disorders were more prevalent among females (with a ratio of 4:1), those with lower education, or those never married. Especially persons with war experiences were at higher risks [9,14].
Virtually no data exist on the prevalence of depression in Iraq, except one lifetime estimate of MDD, i.e. [15]. Rudimental knowledge on comorbidity, burden, treatment, or associated suicidal behaviors of depression is non-existing. Nonetheless, such data are useful to study the impact of war on the general population. Since the early nineties of the previous century, and especially between 2003 and 2010, the war in Iraq has had a dramatic impact on the country resulting in decreased health status of the Iraqi people but also in the destruction of many of the country’s (mental) healthcare system [2]. In line with this, basic but essential vital health data can guide governments to proactive healthcare planning in further elaboration the strategic plan by the Iraqi Ministry of Health.
In the light of these limitations, the current study examines the epidemiology of MDE in the general population of Iraq. We use data from the Iraq Mental Health Survey (IMSH) that was conducted in 2006–2007 as part of the World Health Organization (WHO) World Mental Health (WMH) Survey Initiative (www.hcp.med.harvard.edu/WMH). The WMH comprises a series of psychiatric epidemiologic studies conducted in countries throughout the world. This study builds on an earlier study on mental disorders in Iraq [15] in which basic descriptive data on prevalence and correlates of mental disorders were investigated. The present study examines: (a) the 12-month and lifetime prevalence of MDE in the Iraqi general population; (b) socio-demographic risk factors; (c) comorbid mental disorders and suicidal behaviors, (c) associated impairments in role functioning, and (d) patterns of treatment.
Materials and Methods
Sampling and procedures
The Iraqi Mental Health Survey (IMHS; 18+ years, n = 4,332) was carried out in 2006–2007 by the Iraq Ministry of Health, the Iraq Central Organization for Statistics and Information Technology (COSIT), the Ministry of Health of the Kurdistan region (MoHK), the Kurdistan Regional Statistics Office (KRSO), and the College of Medicine at Al-Qadisiya University in conjunction with the WHO World Mental Health Surveys. Procedures for obtaining oral informed consent and protecting individuals were approved and monitored for compliance by the Institutional Review Boards of the organizations coordinating the survey. Permission for the study was granted by the Institutional Review Boards (IRB) of the Iraq Ministry of Health, the Iraq Central Organization for Statistics and Information Technology (COSIT), the Ministry of Health of the Kurdistan region (MoHK), the Kurdistan Regional Statistics Office (KRSO), and the College of Medicine at Al-Qadisiya University. Standardized descriptions of the goals and procedures of the study, data uses and protection, and the rights of respondents were provided in both written and verbal form to all predesignated respondents before obtaining verbal informed consent for participation in the survey. Oral consent was documented by the trained lay-interviewer. The survey was administered to a stratified multistage clustered area probability sample of household residents in the central and southern governorates in August-September 2006, in Anbar in October-November 2006, and in the Kurdistan region during February-March 2007. The response rate was 95.2%. More details about sampling are provided elsewhere [16].
All interviews were administered face-to-face by trained lay interviewers using training and field quality control procedures described in previous reports [17–19]. Training of local trainers and supervisors took place at the WMH Data Coordination Center at the University of Michigan (USA).
Measurements
Mental disorders
The WHO Composite International Diagnostic Interview Version 3.0 (CIDI) was the instrument administered in the survey [17]. The CIDI is a fully structured diagnostic interview that assesses mental disorders, their treatment, and a wide range of possible risk factors. The WHO translation, back-translation, and harmonization protocol was used to translate instruments and training materials. One of the implications of this approach procedure is that those characteristics that described the core symptoms of MDE were customized when the original wording did not match local language use. However, we did not alter any of the DSM-IV MDE criteria [20].
The disorders analyzed in this study are DSM-IV mood disorders (MDE and dysthymia), anxiety disorders (generalized anxiety disorder [GAD], panic disorder and/or agoraphobia, posttraumatic stress disorder [PTSD], and social phobia), alcohol abuse and/or dependence, and externalizing disorders (attention deficit disorder and intermittent explosive disorder) [21]. Clinical reappraisal studies carried out in four WMH countries provided evidence showing good concordance between CIDI-3.0 diagnoses and diagnoses based on blinded re-interviews, with area under the receiver operator characteristics curve ranging between 0.73–0.93 for lifetime mood/anxiety disorders, and 0.83–0.88 for 12-month mood/anxiety disorders [22].
Suicidality
Suicidality was assessed using the CIDI 3.0 suicidality module [17]. This module includes an assessment of the 12-month occurrence of serious suicide ideation, plans, and attempts. Respondents who endorsed a 12-month history of suicidal ideation were classified as suicidal.
Role impairment
Role impairment was assessed by two measures. First, the WHO disability assessment schedule (WHO-DAS-2) to assess functional impairments in 5 domains during the past 30 days [23]. The first domain includes the number of days in the past 30 days when the respondent was partially or completely unable to work or carry out their normal activities because of physical or mental health problems. The remainder includes severity-persistence estimates of impairments in self-care (e.g. bathing, dressing), mobility (e.g. standing, walking), cognition (e.g. concentrating, remembering), and social functioning (e.g. conversing, maintaining emotional control while around others). The 5 WHO-DAS-2 scales were transformed to a theoretical range of 0 (no impairment at any time in the past 30 days) to 1.0 (complete inability to perform the functions throughout the full 30 days). Second, Respondents with MDE in the past 12 months were also administered the Sheehan Disability Scale (SDS) [24] to evaluate the degree of impairment in functioning due to depression in four domains during the worst month of the past year: work, household, close relationships, and social roles. Responses were scored as mild (1−3), moderate (4−6), severe (7−9) and very severe (10).
Symptom severity
Respondents with 12-month MDE were administered a modified version of the Quick Inventory of Depressive Symptomatology Self-Report (QIDS-SR) to assess symptom severity in the worst month of the past year [25]. The QIDS-SR is a fully-structured measure that is strongly related both to the clinician-administered Inventory of Depressive Symptomology (IDS-C) [26] and to the Hamilton Rating Scale of Depression (HRSD) [27]. Transformation rules developed for the QIDS-SR [28] were used to convert scores into clinical severity categories mapped to conventional HRSD ranges (i.e. mild, moderate, severe/very severe).
12-month treatment
Respondents were asked about 12-month treatment for emotional problems. The number and duration of 12-month visits were also assessed. Responses were used to classify 12-month treatment in the specialty mental health sector (inpatient treatment or outpatient treatment with a psychiatrist, psychologist, any other mental health professional, or a social worker or counselor in a mental health specialty setting, or use of a hotline), the general medical sector (outpatient treatment with a primary care physician, other medical specialist, nurse, or any other health professional not previously mentioned), human services sector (outpatient treatment with a religious or spiritual advisor or with a social worker or counselor in any setting other than a specialty mental health setting), and the complementary-alternative medical (CAM) sector (outpatient treatment with any other type of healer, participation in an internet support group, or participation in a self-help group).
Statistical methods
Cross-tabulations were used to calculate prevalence, comorbidity, symptom severity, impairment, and treatment. The Kaplan-Meier method was used to generate age-at-onset curves. We used logistic regression analysis to study socio-demographic correlates of prevalence and treatment. The regression coefficients were transformed to odds ratios (ORs) for ease of interpretation. Confidence intervals (Cis) were estimated using the Taylor series linearization method implemented in the SUDAAN software package [29]. Multivariate significance tests were calculated using Wald chi2 tests based on coefficient variance-covariance matrices that were adjusted for design effects using the Taylor series method. Since the IMHS was carried out using a multi-stage cluster design, and every individual was assigned a known non-zero probability of selection, all data were analyzed using the design weights for the survey. Standard errors were estimated using the Taylor series linearization method to adjust for design effects [30]. All statistical analyses were carried out in STATA version 9.2. Statistical significance was based on 2-sided design-based tests evaluated at the .05 level of significance.
Results
Description of the sample
The sample consisted of 4,332 respondents with an average age of 36.9 (range of 18–96), with equal numbers of men and women and 65.6% married. About eight in ten (i.e. 78.2%) had at least 12 years of education. Whereas 68.2% of men were employed, most women were not (86.9%). The survey did not assess religion given the sensitive nature of the topic at the time of data collection. More details on sample characteristics can be found elsewhere [15,31].
Prevalence of MDE and sociodemographic risk factors
Prevalence estimates were 7.4% for lifetime and 4.0% for 12-month MDE (Table 1). Almost 6 in 10 lifetime cases (or 57.4%) experienced an episode of MDE in the prior 12-month period. We found a linear increase of lifetime prevalence with age. Prevalence was higher in women than in men (OR = 1.7 [1.0–2.8]). Respondents who were previously married (i.e. separated, widowed, or divorced) were three times as likely to have 12-month MDE (OR = 3.0 [1.6–5.6]) as compared to married respondents. We did not find other sociodemographic correlates.
Table 1. 12-month and lifetime prevalence of DSM-IV major depressive episode (MDE) in the Iraqi general population, by cohort.
| 12-month MDE (1) | Lifetime MDE (1) | 12-month MDE among lifetime MDE | |||||
|---|---|---|---|---|---|---|---|
| Cohort | Denominator (1) | n | %(SE) | n | %(SE) | n | %(SE) |
| 18–34 | 2148 | 70 | 2.8 (0.5) | 126 | 4.9 (0.6) | 70 | 57.6 (7.5) |
| 35–49 | 1332 | 69 | 5.3 (0.9) | 115 | 8.4 (1.0) | 69 | 63.6 (6.9) |
| 50–64 | 589 | 27 | 5.3 (1.3) | 66 | 12.0 (2.1) | 27 | 43.9 (6.8) |
| 65+ | 263 | 21 | 6.5 (1.5) | 34 | 13.0 (2.1) | 21 | 49.8 (8.8) |
| All ages | 4332 | 187 | 4.0 (0.4) | 341 | 7.4 (0.6) | 187 | 54.8 (4.2) |
| significance | Chi2 = 2.6, p = .064 | Chi2 = 9.7, p < .001 | Chi2 = 2.3, p = .088 |
(1) MDE refers to Major Depressive Episode
Age-of-onset of MDE and cohort effects
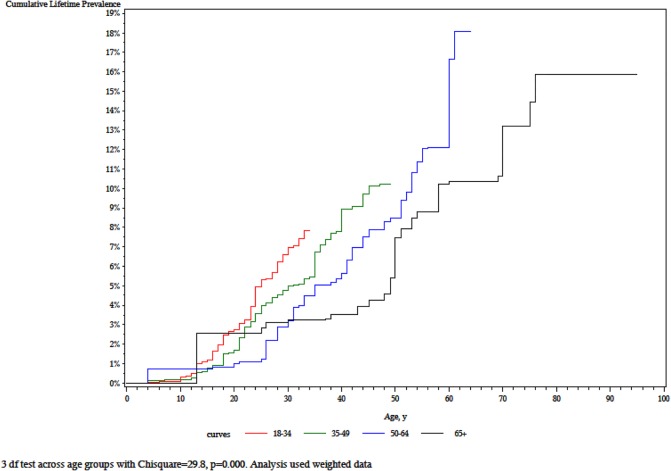
Mean age of onset was 29.8 years (SE = 1.1) and the mean duration of an episode was 22 weeks (SE = 2.4). The cumulative lifetime prevalence curves are significantly different from each other (χ2 = 29.8, p < .001), with in general low risks before the teen years, and then increasing steep slopes in the younger cohorts (Fig 1). We also found a monotonic increase in lifetime prevalence with cohort (i.e. 18–29, 30–44, 45–59, and 50+), from 4.9% in the youngest up to 13.0% in the oldest group (Table 1).
Fig 1. Cumulative lifetime prevalence of DSM-IV major depressive by birth cohort in Iraq.
Psychiatric comorbidity and suicidality
Approximately 6 in 10 respondents with 12-month MDE also met criteria for another 12-month mental disorder, with anxiety disorders, and especially GAD, as the most common comorbid disorder (i.e. 31.1% of those with MDE also meet criteria for GAD, OR = 24.8 [14.2–43.5]) (Table 2). Significant comorbidity associations were also found between MDE and substance abuse and impulse control disorders but we should be careful in interpreting these because of the very low numbers in each cell. Only 23 respondents (or 7.3% among those with MDE; OR = 8.3[4.4–15.8]) also met criteria for PTSD. Further, among those with past year MDE, 7.6% reported suicidal ideation in the same timespan (OR = 11.9 [4.9–29.0]), 2.2% reported suicide plan, (OR = 14.5 [5.4–39.1]), and 2.6% suicide attempt (OR = 16.7 [4.8–58.1]).
Table 2. Comorbidity patterns of DSM-IV major depressive episode with other DSM-IV mental disorders and suicidal behaviors in the Iraqi general population.
| 12-month disorders | 12-month MDE (1) | # with comorbid disorder | % (SE) | OR (95%CI) | significance |
|---|---|---|---|---|---|
| Dysthymia | 187 | 16 | 7.5 (3.4) | 0.0 (0.0–0.0) | Chi2 = 84.2, p < .001 |
| Any mood disorder | 187 | 20 | 11.2 (2.5) | 0.0 (0.0–0.0) | Chi2 = 88.1, p < .001 |
| Generalized anxiety disorder | 187 | 58 | 31.1 (5.1) | 24.8 (14.2–43.5) | Chi2 = 131.7, p < .001 |
| Specific phobia | 187 | 30 | 17.4 (5.0) | 6.7 (3.2–14.0) | Chi2 = 26.7, p < .001 |
| Social phobia | 187 | 6 | 5.1 (2.5) | 12.7 (3.9–41.7) | Chi2 = 18.4, p < .001 |
| Post-traumatic stress disorder | 187 | 23 | 7.3 (1.8) | 8.3 (4.4–15.8) | Chi2 = 44.1, p < .001 |
| Panic disorder | 187 | 14 | 11.0 (4.1) | 20.5 (8.8–48.0) | Chi2 = 50.7, p < .001 |
| Any anxiety disorder | 187 | 99 | 50.7 (6.1) | 16.1 (9.4–27.5) | Chi2 = 107.0, p < .001 |
| Any substance disorder | 187 | 2 | 2.5 (2.4) | 15.3 (1.8–128.3) | Chi2 = 6.6, p = .010 |
| Intermittent explosive disorder | 187 | 9 | 4.7 (2.4) | 3.4 (1.0–11.1) | Chi2 = 4.1, p = .043 |
| Any impulse disorder | 187 | 10 | 5.1 (2.4) | 3.6 (1.2–11.3) | Chi2 = 5.2, p = .022 |
| Any disorder | 187 | 111 | 58.5 (5.8) | 18.4 (11.1–30.5) | Chi2 = 134.5, p < .001 |
| Exactly 1 disorder | 187 | 68 | 34.9 (6.8) | 12.9 (6.8–24.7) | Chi2 = 62.8, p < .001 |
| Exactly 2 disorders | 187 | 32 | 14.6 (3.9) | 14.5 (5.4–39.1) | Chi2 = 102.9, p < .001 |
| 3+ disorders | 187 | 11 | 9.0 (3.9) | 16.7 (4.8–58.1) | Chi2 = 48.0, p < .001 |
| 12-month suicidal behaviors | |||||
| Suicidal ideation | 187 | 24 | 7.6 (2.8) | 11.9 (4.9–29.0) | Chi2 = 31.0, p < .001 |
| Suicidal plans | 187 | 10 | 2.2 (0.9) | 14.5 (5.4–39.1) | Chi2 = 29.2, p < .001 |
| Suicidal attempt | 187 | 8 | 2.6 (1.2) | 16.7 (4.8–58.1) | Chi2 = 20.4, p < .001 |
(1) Specific disorders with n<5 are omitted in Table 2. Any mood disorder also includes bipolar disorder (n = 5), any anxiety disorder also includes agoraphobia without panic (n = 4), any substance disorder also includes alcohol abuse disorder (n = 1) and drug abuse disorder (n = 1), any impulse disorder also includes attention deficit disorder (n = 2).
Role impairment and severity
Analyses on the WHO-DAS-2 components (Table 3) showed that recent MDE (i.e. meeting MDE criteria in the 30 days before the interview) is associated with statistically significant impairments in all 5 WHO-DAS-2 domains (compared with respondents who never met criteria for MDE). Respondents with recent MDE had scores that were on average 4 times higher than the WHO-DAS-2 scores of those who never met MDE criteria. Additional analyses revealed that the average number full out of role days in respondents with MDE in the year before the interview was 70.0, with severe or very severe cases being associated with most days out of role (83.2 days per year) compared to mild (20.5 days per year), and moderate cases (79.0 days per year). In addition, the proportion of respondents with severe or very severe impairment in at least one of the role domains on the SDS was one in four (i.e. 25.9%) among those with mild QIDS-SR scores, about one in two (i.e. 53.3%) among those with moderate QIDS-SR scores, and the vast majority (i.e. 85.8%) among those with severe or very severe QIDS-SR scores.
Table 3. Thirty-day standardized comparisons of functional impairment by the WHO-DAS-2 among respondents with vs. without DSM-IV major depressive episode in the Iraqi general population.
| Past 30 days | Past 12 months | >12 months ago | No lifetime MDE | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WHO-DAS-2 domains | n | Mean(SE) and 95% CI | n | Mean(SE) and 95% CI | n | Mean(SE) and 95% CI | n | Mean(SE) and 95% CI | F3,55 across 4 recency categories | Significance |
| Out of role | 83 | 44.2 (SE = 7.7) (1) | 104 | 42.2 (SE = 8.0) (1) | 154 | 23.4 (SE = 3.4) (1) | 3991 | 12.3 (SE = 0.6) | 25.6 | p < .001 |
| Self-care | 83 | 8.5 (SE = 3.0) (1) | 104 | 16.7 (SE = 5.8) (1) | 154 | 4.1 (SE = 2.2) | 3991 | 1.0 (SE = 0.1) | 3.9 | p = .013 |
| Mobility | 83 | 18.8 (SE = 4.3) (1) | 104 | 16.7 (SE = 5.1) (1) | 154 | 10.8 (SE = 1.6) (1) | 3991 | 3.0 (SE = 0.2) | 12.4 | p < .001 |
| Cognition | 83 | 9.7 (SE = 2.2) (1) | 104 | 7.5 (SE = 2.7) (1) | 154 | 4.2 (SE = 1.1) (1) | 3991 | 1.0 (SE = 0.1) | 16.5 | p < .001 |
| Social functioning | 83 | 8.6 (SE = 2.5) (1) | 104 | 10.1 (SE = 2.9) (1) | 154 | 3.9 (SE = 1.7) (1) | 3991 | 0.6 (SE = 0.1) | 6.7 | p < .001 |
| Total WHO-DAS-2 score | 83 | 18.0 (SE = 2.8) (1) | 104 | 18.6 (SE = 4.0) (1) | 154 | 9.3 (SE = 1.1) (1) | 3991 | 3.6 (SE = 0.2) | 26 | p < .001 |
Abbreviations: DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth edition; MDE = Major Depressive Episode; WHO-DAS-2, World Health Organization-Disability Assessment Schedule-2
(1) Significantly different from respondents with no lifetime MDE at the .05 level, 2-sided test
As summarized in Table 4, about 86% of the respondents with 12-month MDE were independently classified by the QIDS-SR as clinically depressed during the worst month of the year, with 16.1% mild, 23.7% moderate, and 45.9% severe or very severe. Compared to the mild and moderate cases, severe or very severe MDE was associated with more days out of role (up to 83.2 days per year), a higher role impairment (up to 85.8% with severe or very severe impairment on at least one SDS role domain), and more comorbidity, but did not last longer than average (i.e. 22 weeks).
Table 4. Distributions and correlates of symptom severity of 12-month DSM-IV major depressive episode in the Iraqi general population.
| Mild MDE | Moderate MDE | Severe or very severe MDE | Total | ||
|---|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Significance across severity | |
| QIDS distribution of severity (1) | 16.1 (4.4) | 23.7 (6.2) | 45.9 (5.4) | 100.0(0.0) | —- |
| Duration (weeks) (2) | 20.6 (6.4) | 17.4 (4.9) | 24.4 (2.6) | 22.0 (2.4) | F = 2.3, p = .113 |
| WHO-DAS-2 Days full out of role (3) | 20.5 (10.2) | 79.0 (43.1) | 83.2 (25.5) | 70.0 (17.6) | F = 4.9, p = .011 |
| SDS percentage of role impairment (4) | 25.9 (9.4) | 53.3 (11.0) | 85.8 (5.7) | 67.8 (5.6) | chi2 = 25.2, p < .001 |
(1) Percent of people with the Quick Inventory of Depressive Symptomatology- Self Report (QIDS-SR) symptom severity domain.
(2)Number of weeks depressed in the 365 days before the interview.
(3)Number of WHO-DAS-2 days fully out of role (i.e. unable to work or carry on usual activities because of MDE) in the 365 days prior to the interview
(4)Percent who reported severe or very severe impairment in at least one Sheehan Disability Scales (SDS) role domains.
12-month treatment
Only 25 out of the 187 MDE cases reported to have received services in the past year. Given this limitation in statistical power, close to one in seven (or 14.5%) of the MDE cases received treatment in the past year (Table 5), with more severe cases receiving treatment than non-severe cases (19.4 versus 7.7%, respectively). MDE cases were mostly treated in specialized mental health settings (8.6%) and human services settings (4.7%). General medical and CAM settings were less frequently used providers.
Table 5. 12-month treatment patterns for DSM-IV major depressive episode in the Iraqi general population.
| Treatment sectors | # respondents with MDE | # respondents with MDE in treatment | % (SE) | OR (CI) (1) | Significance |
|---|---|---|---|---|---|
| Specialty sector | 187 | 8 | 8.6 (4.1) | 27.3 (7.4–101.1) | Chi2 = 25.6, p < .001 |
| General medical sector | 187 | 7 | 3.7 (2.4) | 6.0 (1.3–27.2) | Chi2 = 5.6, p = .018 |
| Human services sector | 187 | 12 | 4.7 (2.3) | 5.9 (1.7–20.4) | Chi2 = 8.2, p = .004 |
| CAM sector | 187 | 1 | 0.1 (0.1) | 1.9 (0.2–24.1) | Chi2 = 0.3, p = .600 |
| Any treatment in any sector | 187 | 25 | 14.5 (4.7) | 9.2 (3.9–21.8) | Chi2 = 26.5, p < .001 |
(1) The OR refers to the odds of being treated in one of the indicated sectors for respondents with 12-month Major Depressive Episode compared to those without the disorder.
Discussion
This is the first study providing information about the epidemiology of MDE in Iraq based on a nationally representative sample using a standardized methodology. We found that MDE is a common mental disorder in Iraq, annually affecting around 475,000 Iraqi adults, of which 46% are severe or very severe cases. The disorder generally starts around the age of 25 (with remarkably higher risks for those born in more recent cohorts) with higher risks for those previously married and female persons.
In general, our data on prevalence of MDE are consistent with the earlier studies in Arab and Middle East countries [4–14]. We also found consistency with previous literature that women and those previously married were at higher risk for MDE. The OR between MDE and being previously married is somewhat higher in our study than the one commonly reported; this may be related to the societal position and associated social difficulties of divorced people, especially in women in a patriarchal society [32,33]. Our data are also in line with studies performed globally, with MDE emerging as a highly impairing disorder with a considerable comorbidity [21,34–37]. In terms of the proportion of 12-month cases among lifetime cases, the IMHS data provide roughly comparable estimates than those commonly found (i.e. 57% in the IMHS and 40–55% in previous studies [36,38,39], suggesting that MDE is a episodically chronic recurrent disorder for the majority of persons. We also confirm the relatively young age at which MDE generally starts, although MDE in Iraq seems to start 5 years earlier than in Lebanon [12]. Comparable data of other countries are not available. Data on the impairments associated with MDE are in line with other evidence that this disorder is burdensome. We did find however that Iraqi respondents with MDE reported more than twofold days out of role per year compared to what is generally reported [35–37].
There are some results that are not consistent with earlier reported data. First, available research shows that being exposed to war is associated with up to fourfold higher rates of MDE [9,10,40–42]. Against estimations that armed violence in Iraq resulted in nearly 350,000 deaths, disabled persons, and injuries between 2003 and 2010 [2,43], we would have expected a higher rate of MDE cases in our survey than we actually did. We do not know why exactly this is the case but one explanation could be that we underestimated the prevalence of MDE because of the bereavement criterion stipulated in DSM-IV [44]. Given that bereavement is an exclusion criterion of MDE, it may be that a number of respondents may have been excluded from MDE because their episode lasted under 2 months and was classified as bereavement instead of MDE [45]. Another possibility is that stigma-related concerns, i.e. not disclosing emotional problems to others, may lead to a significant underreporting of MDE [46]. To the extent that this is the case, the prevalence of MDE might be higher than the one we actually estimated. As this is the first study that aims to estimate the prevalence of MDE in the general population of Iraq, further studies should confirm or refute our findings. Second, we found a rather atypical comorbidity pattern of MDE as only a few respondents met criteria for both MDE and substance abuse disorder. This could either be a real difference or it might be an artifact because of a possible systematic under-reporting related to the non-acceptability of use of alcohol and substances [47]. The other factor for the low prevalence could be the protective role of cultural and religious practices that preclude use of these substances. In any case, this finding remains for further research to clarify. In addition, only 7% of the MDE cases also met criteria for PTSD. The scarce data available from other studies using general populations with [15] but also without war experiences [48] suggest stronger associations between MDE and PTSD than those we found. A third discrepancy with literature is that the associations between MDE and suicidal behaviors appeared to be stronger in this study (i.e. in the 11.9–16.9 range) than in other general population studies in developing countries (i.e. in the 1.5–3.2 range) [49]. Although we should be careful in interpreting this because of the low numbers, this finding confirms the idea that suicidal behaviors and MDE are strongly associated in (post)war times [50]. Taken together, although prevalence estimates are comparable to earlier reports, our findings suggest that MDE in Iraq is characterized by a few specific features, i.e. starting at earlier age age than commonly reported, stronger associated with days out of role than average, and stronger associated with suicidal behaviors than commonly found. To what extent these features are war-related is unknown and speculative, but they support the hypothesis that impairments of MDE may be exacerbated in people with war experiences. This should be investigated in future studies.
One of the most important findings from this study is the dramatically low treatment rate for MDE. Only 1 in 7 MDE cases received any form of mental health care, even if we include treatment received by CAM providers. Comparable figures have been reported from other countries in the region (e.g. Lebanon [51]) but, nonetheless, this low treatment rate is a matter of great concern. The low level of receipt of care may be due to several factors, including lack of awareness about the medical nature of depression [52], stigma associated with the receipt of care [53], or the lack of acknowledging any need for treatment [54]. Still, a prominent reason for the unmet need for care is likely to be the difficulty in accessing relevant services. Moreover, the limited availability of general health services and in particular mental health services, especially in small cities and towns where there are no psychiatrists and psychiatric facilities, is likely to limit the use of the services [55]. Remarkably, male and female respondents had similar probabilities of receiving treatment, a finding that contradicts the common relationship between female gender and the use of services [56]. Cultural issues factors may explain why women may be more reluctant to seek professional help, especially for mental health reasons. Women were found to be more likely to seek help from traditional healers than men [33] but it may also be that disclosing negative emotions is more likely to be accepted within the family than with third parties. Although we have not yet investigated specific reasons for not seeking help, our findings so far strongly suggest that the unmet need for MDE may be considerable, and that there might be significant inequalities to detect in further study. In a hospitalized-based healthcare system, health reforms in Iraq face a call for realignment of the entire health system [2], with a great emphasis on access to care. Acknowledging that it may not be easy to increase the proportion of depressive people seeking professional help in a country that has suffered from wars and economic sanctions, different strategies–maybe implemented in tandem with increased treatment resources and the national health plan–will need to be implemented to target barriers that prevent people from receiving available care [57].
Our study should be interpreted within the context of the following three main limitations. First, mental disorders were assessed using structured interviews by trained lay interviewers. Although previous CIDI validation studies have shown acceptable validity and reliability [23,58], there may be an underestimation of lifetime prevalence because of the effect that self-reported data on mental health or quality of life data may be flawed [59]. Second, our results may be biased because the survey was administered in the two official languages of Iraq (Arabic and Kurdish) whereas Assyrian Neo-Aramaic and South Azeri are recognized regional languages, aside from different other regional languages spoken by Iraqi citizens. Furthermore, individuals with mental disorders could have more frequently rejected to participate in the survey. Although weighting strategies were used to optimize the representativity of the general population, it is plausible that our results were biased because persons with a history of mental disorders might have been less likely to participate [60,61]. A third limitation pertains to the assessment of MDE. It might have been that the use of stem questions in the screening section of the CIDI-3.0 have led to underestimates of MDE [21]. The interview translation, back-translation, and harmonization process in the WMH surveys included customization of the wording used to describe the core MD symptoms based on clinical experiences of local collaborators and the results of pilot studies [19]. However, we made no attempts to develop cut-off points in the CIDI diagnostic algorithms for different countries or to go beyond the DSM-IV criteria to develop distinct criteria for different countries that might have increased our ability to detect depression or depression-equivalents. Last, since people with depression may experience cognitive impairment and somatic symptoms as core symptoms, we might have excluded sub-threshold or atypical cases of depression that would otherwise have qualified for being a case and treatment in a clinical setting. Although clinical reappraisal studies were carried out, no such study was performed in the Iraqi survey.
Conclusions
MDE is a common disorder in the Iraqi general population, associated with significant impairments in daily life. We found an especially strong association between MDE and suicidal behaviors but this finding needs to be studied in more detail further on. Despite this major burden of MDE, still a very low proportion actually receive treatment. There are good reasons to believe that access to care may be amongst the most important barriers that prevent people from effectively seeking help. One major implication then may be the emphasis on the need for sustainable and structural efforts aimed at increasing access to care, not just for people with MDE, but probably also for other (severe) mental disorders and suicidal behaviors.
Acknowledgments
This report is carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the Mental Health Burden Study: Contract number HHSN271200700030C, the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, the Eli Lilly & Company Foundation, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, Bristol-Myers Squibb, and Shire. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/. Implementation of the Iraq Mental Health Survey (IMHS) and data entry were carried out by the staff of the Iraqi MOH and MOP with direct support from the Iraqi IMHS team with funding from both the Japanese and European Funds through United Nations Development Group Iraq Trust Fund (UNDG ITF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
Data underlying the supplemental tables are from the WHO World Mental Health Survey, whose authors may be contacted via http://www.hcp.med.harvard.edu/wmh. All other relevant data are within the paper. The authors welcome and support PLOS commitment to transparency and information sharing with the research community. The authors allow public access to the instrument, sample description and all methods used. The authors are also able to reanalyze data to evaluate any reasonable suggestions made by reviewers or readers and to share printouts of results of reanalysis based on these suggestions. However, the authors are not able to share raw data due to prohibitions on doing so in their respondent consent documents and in their agreements with the WMH consortium to limit comparative analyses to those carried out within the consortium. The authors are also constrained in their ability to allow outside investigators to work remotely on their dataset due to the complexity of the data, the fact that the data are not documented in such a way that external users could make sense of the data without substantial help from the authors’ internal analysts, and funding constraints on the amount of time the authors’ analysts have available for such consultation with external users.
Funding Statement
This report is carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. The authors thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the Mental Health Burden Study: Contract number HHSN271200700030C, the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, the Eli Lilly & Company Foundation, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, Bristol-Myers Squibb, and Shire. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/. Implementation of the Iraq Mental Health Survey (IMHS) and data entry were carried out by the staff of the Iraqi MOH and MOP with direct support from the Iraqi IMHS team with funding from both the Japanese and European Funds through United Nations Development Group Iraq Trust Fund (UNDG ITF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Mokdad AH, Jaber S, Aziz MI, AlBuhairan F, AlGhaithi A, AlHamad NM et al. (2014) The state of health in the Arab world, 1990–2010: an analysis of the burden of diseases, injuries, and risk factors. Lancet 25: 309–320. [DOI] [PubMed] [Google Scholar]
- 2. Al Hilfi TK, Lafta R, Burnham G (2013) Health services in Iraq. Lancet 381: 939–948. 10.1016/S0140-6736(13)60320-7 [DOI] [PubMed] [Google Scholar]
- 3. Ferrari AJ, Charslon FJ, Norman RE, Patten SB, Freedman G, Murray CJL et al. (2013) Burden of depressive disorders by country, sex, age, and year: Findings from the Global Burden of Disease Study 2010. Plos medicine 10: e1001547 10.1371/journal.pmed.1001547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kilzieh N, Rastam S, Maziak W, Ward KD (2008) Comorbidity of depression with chronic diseases: a population-based study in Aleppo, Syria. International journal of psychiatry in medicine 38: 169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Noorbala AA, Bagheri Yazdi SA, Yasamy MT, Mohammad K (2004) Mental health survey of the adult population in Iran. Nordic journal of psychiatry 184: 70–73. [DOI] [PubMed] [Google Scholar]
- 6. Noorbala AA, Bagheri Yazdi SA, Hafezi M (2013) Trends in change of mental health status in the population of Tehran between 1998 and 2007. Archives of Iranian medicine 15: 201–204. [PubMed] [Google Scholar]
- 7. Modabernia MJ, Shodjai Tehrani H, Fallahi M, Shirazi M, Modabernia AH (2008) Prevalence of depressive disorders in Rasht, Iran: A community based study. Clinical practice and epidemiology in mental health 4: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Narimani M, Sadeghilh Ahari S, Abdi R (2011) Epidemiological survey of mental disorders in urban regions of Ardabil province (Iran). Journal of psychiatric mental health nursing 18: 368–373. 10.1111/j.1365-2850.2011.01700.x [DOI] [PubMed] [Google Scholar]
- 9. Cardozo BL, Bilukha OO, Crawford CA, Shaikh I, Wolfe MI, Gerber ML et al. (2004) Mental health, social functioning, and disability in postwar Afghanistan. Journal of the American medical association 292: 575–584. [DOI] [PubMed] [Google Scholar]
- 10. Karam EG, Howard DB, Karam AN, Ashkar A, Shaaya M, Melhem N et al. (1998) Major depression and external stressors: the Lebanon Wars. European archives of psychiatry and clinical neurosciences 248: 225–230. [DOI] [PubMed] [Google Scholar]
- 11. Jaalouk D, Okasha A, Salamoun MM, Karam EG (2012) Mental health research in the Arab world. Social psychiatry and psychiatric epidemiology 47: 1727–1731. 10.1007/s00127-012-0487-8 [DOI] [PubMed] [Google Scholar]
- 12. Karam EG, Mneimneh ZN, Dimassi H, Fayyad JA, Karam AN, Nasser SC et al. (2008) Lifetime prevalence of mental disorders in Lebanon: First.onset, treatment, and exposure to war. Plos medicine 5: 579–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Khatwa SA, Abdou MH (1999) Adult depression in Alexandria, Egypt, 1998. Journal of Egypt public health association 74:333–352. [PubMed] [Google Scholar]
- 14. Daradkeh TK1, Ghubash R, Abou-Saleh MT (2002) Al Ain community survey of psychiatric morbidity II. Sex differences in the prevalence of depressive disorders. Journal of affective disorders 72: 167–176. [DOI] [PubMed] [Google Scholar]
- 15. Alhasnawi S, Sadik S, Rasheed M, Baban A, Al-Alak MM, Othman AY et al. (2009) The prevalence and correlates of DSM-IV disorders in the Iraq Mental Health Survey (IMHS). World psychiatry 8: 97–109. [PMC free article] [PubMed] [Google Scholar]
- 16. Heeringa SG, Wells JE, Frost H, Mneimneh ZN, Chiu GT, Sampson NA et al. (2008) Sample Designs and Sampling Procedures In Kessler RC & Üstün TB, editors. The WHO World Mental Health Surveys: global Perspectives on the Epidemiology of Mental Disorders. Cambridge University Press: New York: pp. 14–32. [Google Scholar]
- 17. Kessler RC, Ustun TB (2004) The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International journal of methods in psychiatric research 13: 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pennell BE, Mneimneh ZN, Bowers A, Chardoul S, Wells JE, Viana MC et al. (2008). Implementation of the World Mental Health Surveys. Methods In Kessler RC & Üstün TB, editors. The WHO World Mental Health Surveys: global Perspectives on the Epidemiology of Mental Disorders. Cambridge University Press: New York: pp. 33–57. [Google Scholar]
- 19. Harkness J, Pennell BE, Villar A, Gebler N, Aguilar-Gaxiola S, Bilgen I. (2008). Translation Procedures and Translation Assessment in the World Mental Health Survey Initiative In Kessler RC & Üstün TB, editors. The WHO World Mental Health Surveys: global Perspectives on the Epidemiology of Mental Disorders. Cambridge University Press: New York: pp. 91–113. [Google Scholar]
- 20. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G et al. (2011) Cross-national epidemiology of DSM-IV major depressive disorder. BMC medicine 9: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. American Psychiatric Association. Diagnostic and Statistical Manual, 4th Edition Washington DC, American Psychiatric Association, 1994. [Google Scholar]
- 22. Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R et al. (2006) Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. International journal of methods in psychiatric research 15: 167–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Von Korff M, Crane PK, Alonso J, Vilagut G, Angermeyer MC, Bruffaerts R et al. (2008) Modified WHODAS-II provides valid measure of global disability but filter items .increased skewness. Journal of clinical epidemiology 61: 1132–1143. 10.1016/j.jclinepi.2007.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leon AC, Olfson M, Portera L, Farber L, Sheehan DV (1997) Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International journal of psychiatry in medicine 27: 93–105. [DOI] [PubMed] [Google Scholar]
- 25. Rush AJ, Carmody T, Reimitz PE (2000) The inventory of depressive symptomatology (IDS). International journal of methods in psychiatric research 9: 45–59. [Google Scholar]
- 26. Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH (1996) The inventory of depressive symptomatology (IDS) Psychological medicine 26: 477–486. [DOI] [PubMed] [Google Scholar]
- 27. Hamilton M (1960) A rating scale for depression. Journal of neurology neurology and psychiatry 23: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN et al. (2003) The 16-item quick inventory of depressive symptomatology (QIDS) clinician rating (QIDS-C) and self-report (QIDS-SR). Biological psychiatry 54: 573–583. [DOI] [PubMed] [Google Scholar]
- 29. Research Triangle Institute (2005) SUDAAN, Version 9.0.1 [computer program] Research Triangle Park, NC: Research Triangle Institute. [Google Scholar]
- 30. Bunting MB, Zaslavsky AM (2004) Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. Journal of health economics; 23: 525–542. [DOI] [PubMed] [Google Scholar]
- 31. Al-Hamzawi AO, Rosellini AJ, Lindberg M, Petukhova M, Kessler RC, Bruffaerts R (2014) The role of common mental and physical disorders in days out of role in the Iraqi general population: results from the WHO World Mental Health Surveys. Journal of psychiatric research 53: 23–29. 10.1016/j.jpsychires.2014.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jones GW (1997) Modernization and Divorce: Contrasting Trends in Islamic Southwest Asia and The West. Population and Development Review 23: 95–114. [Google Scholar]
- 33. Al-Krenawi A, Graham JR, Kandah J (2000) Gendered utilization differences of mental health services in Jordan. Community Mental Health Journal 36: 501–511. [DOI] [PubMed] [Google Scholar]
- 34. Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP et al. (2004) Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Journal of the American medical association 291: 2581–2590. [DOI] [PubMed] [Google Scholar]
- 35. Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA et al. (2010) Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depression and anxiety 27: 351–364. 10.1002/da.20634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR et al. (2003) National Comorbidity Survey Replication The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). Journal of the American medical association 289: 3095–3105. [DOI] [PubMed] [Google Scholar]
- 37. Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370: 851–858. [DOI] [PubMed] [Google Scholar]
- 38. WHO International Consortium in Psychiatric Epidemiology. Cross-national comparisons of the prevalences and correlates of mental disorders. Bulletin on the World Health Organization 78: 413–426. [PMC free article] [PubMed] [Google Scholar]
- 39. Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W et al. (2003). The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. International journal of methods in psychiatric research 12, 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Farhood LF, Dimassi H (2012) Prevalence and predictors for post-traumatic stress disorder, depression and general health in a population from six villages in South Lebanon. Social psychiatry and psychiatric epidemiology 47: 639–649. 10.1007/s00127-011-0368-6 [DOI] [PubMed] [Google Scholar]
- 41. Farhood L, Dimassi H, Lehtinen T (2006) Exposure to war-related traumatic events, prevalence of PTSD, and general psychiatric morbidity in a civilian population from southern Lebanon. Journal of transcultural nursing 17: 333–340. [DOI] [PubMed] [Google Scholar]
- 42. Priebe S, Bogic M, Ajdukovic D, Franciskovic T, Galeazzi GM, Kucukalic A et al. (2010) Mental disorders following war in the Balkans: a study in 5 countries. Archives of general psychiatry 67: 518–528. 10.1001/archgenpsychiatry.2010.37 [DOI] [PubMed] [Google Scholar]
- 43. Hicks MHR, Dardagan H, Bagnall PM, Spagat M, Sloboda JA (2011) Casualties in civilians and coalition soldiers from suicide bombings in Iraq: a descriptive study. Lancet 378: 906e14. [DOI] [PubMed] [Google Scholar]
- 44. Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA (2003) Life Event Dimensions of Loss, Humiliation, Entrapment, and Danger in the Prediction of Onsets of Major Depression and Generalized Anxiety. Archives of general psychiatry 60: 789–796. [DOI] [PubMed] [Google Scholar]
- 45. Morina N, von Lersner U, Prigerson HG (2011) War and bereavement: consequences for mental and physical distress. Plos one 6: 7: e22140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Eloul L, Ambusaidi A, Al-Adawi S (2009) Silent epidemic of depression in women in the Middle east and North Africa Region. Sultan Qaboos university medical journal 9: 5–15. [PMC free article] [PubMed] [Google Scholar]
- 47. Almarri TSK, Oei TPS (2008) Alcohol and substance use in the Arabian Gulf Region: a review. International journal of psychology 44: 222–233. [DOI] [PubMed] [Google Scholar]
- 48. Alonso J, Angermeyer M, Bernert S, Bruffaerts R, Brugha TS, Bryson H et al. (2004) Prevalence of mental disorders in Europe: Results from the European Study of Epidemiology of Mental Disorders (ESEMeD) Project. Acta psychiatrica scandinavica 109: 21–27. [DOI] [PubMed] [Google Scholar]
- 49. Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A et al. (2009) Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS med 6(8):e1000123 10.1371/journal.pmed.1000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Karam EG, Salamoun MM, Mneimeh ZN, Fayyad JA, Karam AN, Hajjar R et al. RC (2012) War and first onset of suicidality: the role of mental disorders. Psychological medicine 42: 2109–2118. 10.1017/S0033291712000268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Karam EG, Mneimneh ZN, Karam AN, Fayyad JA, Nasser SC, Chatterji S et al. (2006) Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. Lancet 367: 1000–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. El-Islam MR (1982). Arabic cultural psychiatry. Transcultural psychiatric research review 19: 5–24. [Google Scholar]
- 53. Dwairy M (2002) Foundations of psychosocial dynamic personality theory of collective people. Clinical Psychology Review 22: 343–360 [DOI] [PubMed] [Google Scholar]
- 54. Bener A, Ghuloum S (2010) Gender differences in the knowledge, attitude and practice towards mental health illness in a rapidly developing Arab society. International journal of social psychiatry 57: 480–486. 10.1177/0020764010374415 [DOI] [PubMed] [Google Scholar]
- 55. WHO. Country health information systems: a review of the current situation and trends Geneva: World health Organization, 2011. [Google Scholar]
- 56. Wang PS, Aguilar-Gaxiola E, Alonso J, Angermeyer MA, Borges G, Bromet EJ et al. (2007) Worldwide use of mental health services for anxiety, mood, and substance disorders: Results from 17 countries in the WHO World Mental Health (WMH) Surveys. Lancet 370: 841–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J et al. (2007) Barriers to improvement of mental health services in low-income and middle-income countries. Lancet 370: 1164–1174. [DOI] [PubMed] [Google Scholar]
- 58. Wittchen HU (1994) Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): a critical review. Journal of psychiatric research 28: 57–84. [DOI] [PubMed] [Google Scholar]
- 59. Atkinson M, Zibin S, Chuang H (1997) Characterizing quality of life among patients with chronic mental illness: a critical examination of the self-report methodology. American journal of psychiatry 154: 99–105. [DOI] [PubMed] [Google Scholar]
- 60. de Graaf R, Bijl RV, Smit F, Ravelli A, Vollebergh WA (2000) Psychiatric and sociodemographic predictors of attrition in a longitudinal study: The Netherlands Mental Health Survey and Incidence Study (NEMESIS). American journal of psychiatry 152: 1039–1047. [DOI] [PubMed] [Google Scholar]
- 61. Eaton WW, Anthony JC, Tepper S, Dryman A (1992) Psychopathology and attrition in the epidemiologic catchment area surveys. American journal of psychiatry 135:1051–1059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data underlying the supplemental tables are from the WHO World Mental Health Survey, whose authors may be contacted via http://www.hcp.med.harvard.edu/wmh. All other relevant data are within the paper. The authors welcome and support PLOS commitment to transparency and information sharing with the research community. The authors allow public access to the instrument, sample description and all methods used. The authors are also able to reanalyze data to evaluate any reasonable suggestions made by reviewers or readers and to share printouts of results of reanalysis based on these suggestions. However, the authors are not able to share raw data due to prohibitions on doing so in their respondent consent documents and in their agreements with the WMH consortium to limit comparative analyses to those carried out within the consortium. The authors are also constrained in their ability to allow outside investigators to work remotely on their dataset due to the complexity of the data, the fact that the data are not documented in such a way that external users could make sense of the data without substantial help from the authors’ internal analysts, and funding constraints on the amount of time the authors’ analysts have available for such consultation with external users.