Abstract
Purpose:
The aim of this study was to compare the efficacy and safety between standard trabeculectomy and the Ex-PRESS shunt implantation.
Methods:
A retrospective review of the records of 100 eyes of 100 patients who underwent trabeculectomy or Ex-PRESS shunt implantation between July 2010 and June 2012 was conducted. Of these, 61 (61%) eyes underwent trabeculectomy and 39 (39%) eyes underwent Ex-PRESS shunt implantation. Demographic information, glaucoma type, surgical details, preoperative, and postoperative data including intraocular pressure (IOP), number of medications, reoperation, and occurrence of any complications were recorded.
Results:
No differences in IOP reduction or number of postoperative IOP-lowering medications were demonstrated between the 2 procedures. Success rates were 86.9% for trabeculectomy and 84.6% for Ex-PRESS shunt. Rates of failure and hypotony were not significantly different between the groups. No parameter was correlated with success or failure of any procedure.
Conclusions:
Standard trabeculectomy and Ex-PRESS shunt have similar efficacy and safety profiles. As the Ex-PRESS shunt is considerably more expensive, its use may be unjustified, especially as a primary procedure.
Key Words: trabeculectomy, Ex-PRESS, glaucoma, intraocular pressure
Trabeculectomy is the most commonly performed surgery for intraocular pressure (IOP) reduction in patients with glaucoma.1 This procedure has been in clinical use for over 40 years,2 and its success and complication rates are well established.3,4
The Ex-PRESS miniature glaucoma implant (Alcon Laboratories Inc., Fort Worth, TX) is a biocompatible, nonvalved stainless steel tube. Originally, it was intended to be used for subconjunctival implantation near the limbus and drain aqueous fluid into the subconjunctival space.5 This would have resulted in a simpler and faster surgical procedure for the reduction of IOP than standard trabeculectomy. However, subconjunctival Ex-PRESS implantation was associated with an unacceptably high rate of complications, including persistent hypotony, flat anterior chamber, choroidal detachment, suprachoroidal hemorrhage, conjunctival scarring, and implant extrusion.6–10 Therefore, the Ex-PRESS is currently implanted under a partial-thickness sclera flap, as first suggested by Dahan and Carmichael.11 The procedure is similar to standard trabeculectomy, and includes creation of a sclera flap and a conjunctival filtration bleb, but no peripheral iridectomy is required when implanting the Ex-PRESS.12
Although the Ex-PRESS shunt is gaining popularity, there are currently no clearly established indications for the use of the Ex-PRESS implant, and reports concerning the relative safety and efficacy of standard trabeculectomy and Ex-PRESS are controversial and at times contradictory. The purpose of this study is to compare the results of the 2 surgical procedures, and to identify any patient characteristics that are associated with increased efficacy or safety with any of the procedures. This study was designed to include a large patient cohort for these analyses, and also focus on the P-200 Ex-PRESS shunt model, which has been less studied than the P-50 model. A comprehensive review of the literature was also conducted.
METHODS
Patient Selection
After approval by the Institutional Review Board of The Tel Aviv Medical Center, the records of all consecutive patients who underwent trabeculectomy or Ex-PRESS miniature glaucoma shunt implantation in our institution between July 1, 2009 and June 30, 2012 were retrospectively reviewed.
All included patients were 18 years of age or older at the time of surgery. Patients who had undergone previous ocular trauma or any surgical procedure other than cataract extraction or previous trabeculectomy were excluded. Only phakic or pseudophakic patients with intraocular lens (IOL) within the capsular bag throughout the follow-up period were included in this study, and aphakic and pseudophakic patients with the anterior chamber, iris fixated, or sulcus IOLs were excluded. Patients whose surgery was combined with any other procedure other than cataract extraction and IOL implantation within the capsular bag were excluded. Exclusion criteria also included any history of retinal detachment, retinal vascular occlusion, optic neuropathy, or trauma. A minimum of 3 months of follow-up after the surgery was required for inclusion in this study. In addition, patients whose records were incomplete were excluded from this study.
Data Collection
Data were retrieved from the medical notes before the surgery, the surgical reports, the in-patient department charts, and the outpatient clinic charts. The parameters recorded included demographic information, history of diabetes mellitus or hypertension, previous ocular history, type of glaucoma, previous glaucoma treatment by laser or trabeculectomy, preoperative IOP and number of antiglaucoma medications, lens status, the occurrence of any postoperative complications, and the need for any additional surgical interventions throughout the follow-up period.
IOP measurements were recorded preoperatively and postoperatively at discharge, 1 week, 1 month, 3 months, 6 months, and every 6 months thereafter. IOP measurements included in this study were all obtained by Goldmann applanation tonometry. Along with the IOP measurements, the number of pressure-lowering medications in use at all timepoints was also recorded. Combination preparations (such as Cosopt and Combigan) were counted as 2 separate medications.
Success was defined as a 20% reduction in IOP from the preoperative value or IOP under 20 mm Hg. Success was complete if it was achieved without any postoperative use of antiglaucoma medication and qualified if additional treatment was needed. Failure was defined as either need for repeated surgery for glaucoma, persistent elevated IOP over 20 mm Hg despite medical therapy, or persistent hypotony (IOP<5 mm Hg). Patients who underwent additional trabeculectomy or glaucoma drainage device implantation for control of their glaucoma were considered as failures, and IOP values were censored after these procedures. Patients who required pars plana vitrectomy or keratoplasty were also considered as failures. Laser suture lysis was considered as a part of the normal management of the patients in this study and was therefore not analyzed. Needling procedures were also not considered as failures.
Surgical parameters included the review of surgical techniques as documented to ensure uniformity, and the presence or absence of a combined cataract extraction procedure.
The choice of surgical procedure depended on the availability of the Ex-PRESS shunt at the time of surgery. The Ex-PRESS shunt was sporadically available throughout the study period, and its use was not guided by any preoperative parameter. There was no bias in the selection of the surgical procedure.
Surgical Techniques
Surgical technique for trabeculectomy included creating a fornix-based peritomy, dissection of a scleral flap, followed by subconjunctival application of mitomycin C (MMC) (0.4 mg/mL) for 1 to 2 minutes, and thorough irrigation. The anterior chamber was then entered using a 1 mm stylet, and a peripheral punch was performed, followed by peripheral iridectomy. The scleral flap was sutured by 2 to 3 10-0 nylon sutures, and a bleb was formed by suturing the conjunctiva to the limbus using 2 10-0 mersilene sutures.
Surgical technique for Ex-PRESS miniature glaucoma shunt implantation included creating a fornix-based peritomy, dissection of a scleral flap, followed by subconjunctival application of MMC (0.4 mg/mL) for 1 to 2 minutes, and thorough irrigation. The anterior chamber was then entered using a 25 G needle, and the P-200 Ex-PRESS shunt was inserted and placed using its designed applicator, with no iridectomy. The scleral flap was sutured by 2 to 3 10-0 nylon sutures, and a bleb was formed by suturing the conjunctiva to the limbus using 2 10-0 mersilene sutures.
In all cases that were combined with cataract extraction, phacoemulsification and IOL implantation in the capsular bag were performed. The procedure was performed by a separate corneal incision, created after the irrigation of the MMC, to prevent its entry into the anterior chamber. Trabeculectomy or Ex-PRESS shunt implantation were then performed after phacoemulsification and IOL implantation.
All surgeries were performed by 1 of the 2 glaucoma surgeons, who contributed equally (S.K. performed 33 trabeculectomies and 21 Ex-PRESS shunt implantations, and G.S. performed 28 trabeculectomies and 18 Ex-PRESS shunt implantations).
After both types of surgery, all patients were treated with topical ofloxacin 0.3% and dexamethasone sulfate 0.1% 4 times a day, with cessation of all previous topical antiglaucoma therapy. Dexamethasone dosage was tapered 6 to 12 weeks after surgery.
Statistical Analysis
The t test was used to compare continuous variables between groups. The Fisher exact test was used to analyze associations between categorical parameters. Analysis of covariance (ANCOVA) with repeated measures over time was used to analyze the difference in IOP between the 2 surgical techniques. A P-value of 0.05 was used to declare statistically significant difference between the groups for all analyses. Data were analyzed using SPSS for windows version 17.
RESULTS
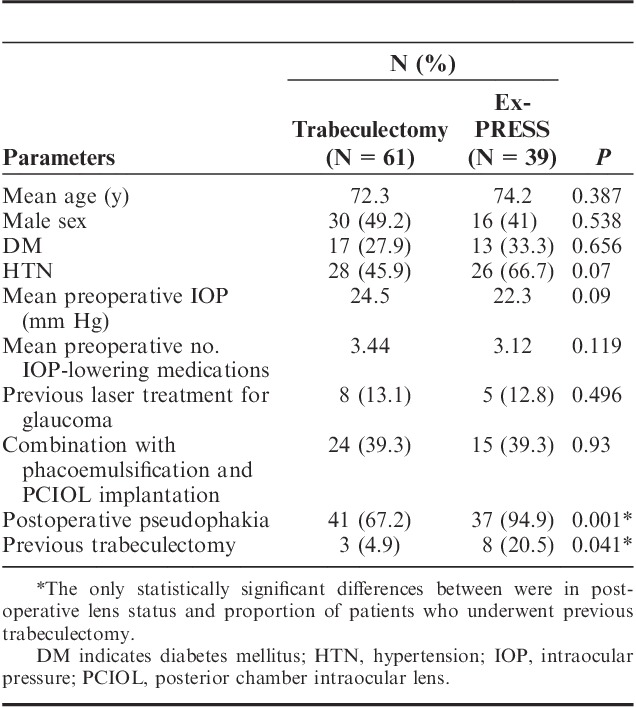
One hundred eyes of 100 patients fulfilled the inclusion criteria and were included in the study. These patients included 46 (46%) men and 54 (54%) women, with a mean age of 73.1±10.3 years (range, 41 to 94 y). Mean follow-up was 11.3±6.7 months (range, 3 to 31 mo). The surgical procedures consisted of 61 (61%) trabeculectomies and 39 (39%) Ex-PRESS miniature glaucoma shunt implantations. Surgery was combined with phacoemulsification in 39 (39%) eyes. It was combined in 24 (39.3%) of the eyes that underwent trabeculectomy and 15 (39.3%) of those that underwent Ex-PRESS shunt implantation, with no significant difference between the 2 groups (P=0.93). After surgery, 78 (78%) eyes were pseudophakic and 22 (22%) were phakic. However, during follow-up, a significantly greater proportion of eyes that underwent Ex-PRESS shunt implantation were pseudophakic (94.9% vs. 67.2% of the eyes that underwent trabeculectomy, P=0.001) (Table 1).
TABLE 1.
Baseline Information of Patients Who Underwent Trabeculectomy and Ex-PRESS Miniature Glaucoma Shunt Implantation
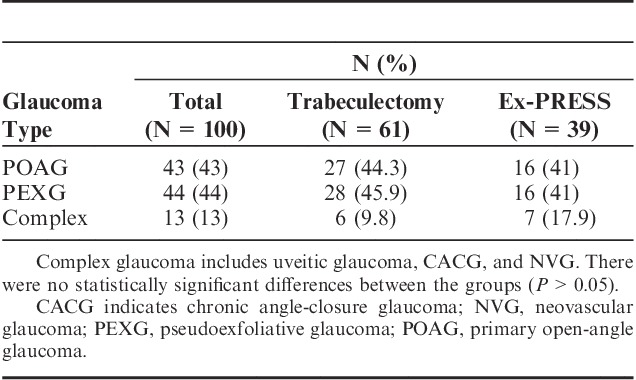
The type of glaucoma varied between patients in this study, and included primary open-angle glaucoma (POAG) (43%), pseudoexfoliative glaucoma (PEXG) (44%), uveitic glaucoma (6%), chronic angle-closure glaucoma (CACG) (5%), and neovascular glaucoma (NVG) (2%). Because of the relatively low proportion of uveitic glaucoma, CACG, and NVG, these eyes were analyzed collectively as a “complex glaucoma” group. The distribution of glaucoma types between the 2 groups is provided in Table 2. Eleven (11%) of the patients had previously undergone trabeculectomy, and the surgery analyzed in this study was a repeated procedure. Three of these patients underwent repeated trabeculectomy, whereas the other 8 underwent Ex-PRESS shunt implantation, resulting in a significantly higher proportion of previously operated patients in the Ex-PRESS group (P=0.041). A subanalysis excluding these cases was also performed to eliminate this potential source of bias between the groups. Of the remaining 89 patients who were operated for the first time, 13 (14.6%) had previously undergone argon laser trabeculoplasty and 1 (1.1%) had undergone selective laser trabeculoplasty, with no significant difference between the groups.
TABLE 2.
Distribution of Glaucoma Types Between Patients Who Underwent Trabeculectomy and Ex-PRESS Miniature Glaucoma Shunt Implantation
Preoperative IOP was a little higher among patients who underwent trabeculectomy (24.5 vs. 22.3 mm Hg), but this difference was not statistically significant (P=0.09). There was no significant difference in the preoperative number of antiglaucoma medications in use (P=0.119), nor in any of the other recorded demographic or baseline parameters between both the patient groups (Table 1).
IOP Analysis
Preoperative IOP was 24.5±9.2 mm Hg in patients who underwent trabeculectomy and 22.3±9.3 mm Hg in patients who underwent Ex-PRESS shunt implantation. There was no significant difference in preoperative IOP values or the number of IOP-lowering medications used by patients who underwent trabeculectomy or Ex-PRESS shunt implantation. IOP and the number of IOP-lowering medications in use were not significantly different between the 2 groups at any timepoint. Analysis of covariance with repeated measures over time was used to compare the IOP during the first 6 months after surgery between the 2 surgical techniques, and demonstrated no significant difference between the groups (Fig. 1A). A corresponding analysis of the number of IOP-lowering medications also demonstrated no difference between the 2 groups (Fig. 1B).
FIGURE 1.
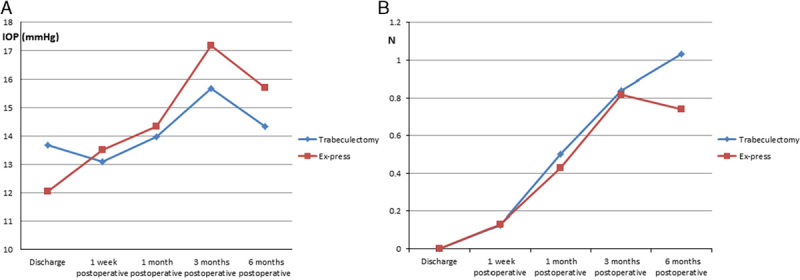
A comparison of the postoperative IOP (A) and number of IOP-lowering medications in use (B) over 6 months between patients who underwent trabeculectomy and Ex-PRESS miniature glaucoma shunt implantation. No significant difference was demonstrated. IOP indicates intraocular pressure.
Among patients who underwent trabeculectomy, success was achieved in 53 (86.9%) eyes. Complete success was achieved in 38 (62.3%) eyes and qualified success was achieved in 15 (24.6%) eyes. Among patients who underwent Ex-PRESS shunt implantation, success was achieved in 33 (84.6%) eyes. Complete success was achieved in 26 (66.6%) eyes and qualified success was achieved in 7 (17.9%) eyes. No significant differences were found between the groups in the rates of overall, complete, or qualified success. Success rates were not affected by the inclusion of patients with “complex glaucoma.” When these 13 patients were excluded, success rates were 87.2% for trabeculectomy and 84.4% for the Ex-PRESS shunt.
As 2 of the patients’ baseline characteristics were significantly different, separate analyses controlling for these factors were performed. First, a subanalysis was performed excluding the 11 patients who previously underwent trabeculectomy. Comparing postoperative IOP and the number of IOP-lowering medications demonstrated no significant differences between patients who underwent trabeculectomy and Ex-PRESS shunt implantation (Figs. 2A, B). Second, postoperative IOP was compared between phakic and pseudophakic eyes, and no significant difference was demonstrated. In addition, an intragroup comparison between phakic and pseudophakic eyes that underwent trabeculectomy did not reveal any significant difference in IOP. Combination of any of the surgical procedures with phacoemulsification was also not associated with any significant difference in postoperative IOP. A separate analysis was performed including only the 78 postoperatively operated eyes, and again no significant differences in IOP or use of IOP-lowering medications were found between patients who underwent trabeculectomy and Ex-PRESS shunt implantation.
FIGURE 2.
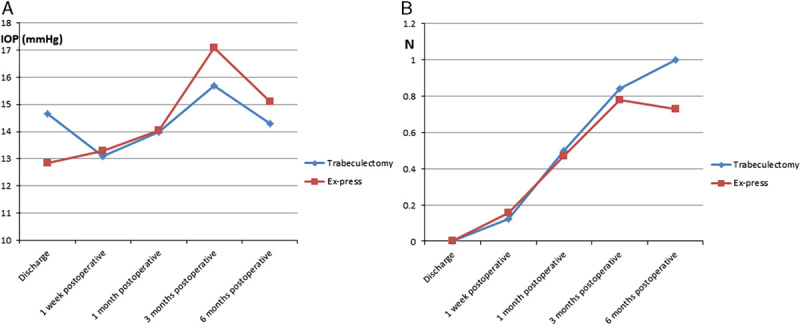
A comparison of the postoperative IOP (A) and number of IOP-lowering medications in use (B) over 6 months between patients who underwent trabeculectomy and Ex-PRESS miniature glaucoma shunt implantation, excluding those who had undergone previous trabeculectomy before inclusion in this study. No significant difference was demonstrated. IOP indicates intraocular pressure.
Complications, Reoperations, and Failure Analysis
Complications encountered in this study (Table 3) included 1 case (1%) of blebitis, 7 (7%) early postoperative bleb leaks, 4 (4%) overfiltrating blebs, and 9 (9%) eyes with hypotony, of which 4 were complicated by choroidal detachment. One (1%) patient with NVG who underwent Ex-PRESS shunt implantation was complicated by choroidal and vitreous hemorrhage with extremely elevated IOP 5 months postoperatively, and required pars plana vitrectomy. No corneal decompensation or endophthalmitis were encountered. Because of the small number of complications, only hypotony was compared between the groups. In the trabeculectomy group, hypotony was documented in 6 (9.8%) eyes, and in the Ex-PRESS group it was documented in 3 (7.7%) eyes, with no significant difference between the groups (P=0.215). Of these 9 eyes, hypotony was temporary in 6 and remained persistent in 3 by the end of follow-up.
TABLE 3.
Distribution of Complications Encountered Included in This Study

Reoperation for uncontrolled glaucoma was required in 4 (4%) patients, 2 from each group. Two of them underwent trabeculectomy and 2 were referred for Ahmed valve implantation. One of the latter was 1 of the 11 patients who had undergone previous trabeculectomy before inclusion in the study. None of the 4 patients who required reoperation belonged to the complex glaucoma group.
According to the study definitions, 14 (14%) eyes were considered as failures. The distribution of causes for failure in these eyes is provided in Table 4. There were 8 (13.1%) failures in the trabeculectomy group and 6 (15.4%) in the Ex-PRESS implantation group, with no significant difference between the 2 surgical procedures (P=0.774). Kaplan-Meier product-limit estimate of the survival curve revealed no significant difference between standard trabeculectomy and Ex-PRESS shunt implantation (P=0.855) (Fig. 3).
TABLE 4.
Causes for Failure Among the Eyes Included in This Study

FIGURE 3.
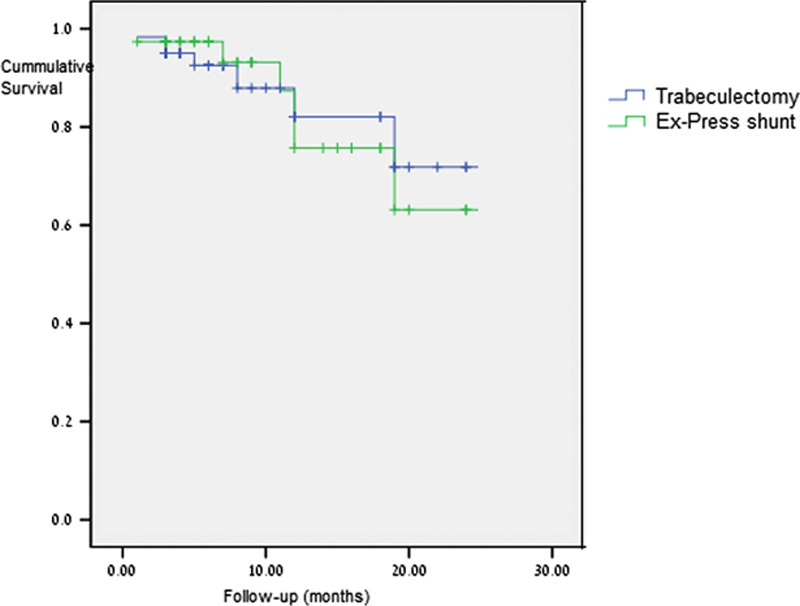
Kaplan-Meier product-limit estimate of the survival of trabeculectomy and Ex-PRESS shunt. No significant difference was demonstrated between the 2 procedures.
Failure was not correlated with any of the patients’ characteristics or surgical details. A slight trend was noted toward an increased risk for failure with advanced age, but it did not reach statistical significance (P=0.063).
DISCUSSION
There are relatively few studies comparing the Ex-PRESS miniature glaucoma shunt with standard trabeculectomy. The majority of these studies have reported no significant difference in IOP reduction between the 2 procedures.13–17 One study demonstrated a significantly higher success rate with the Ex-PRESS shunt.18 However, it should be noted that its success rate was similar to that reported in the other studies, and the statistically significant difference found probably resulted from the low rate of success for standard trabeculectomy. In a long-term extension of that study, no difference in IOP was demonstrated 3 years postoperatively.19
The Ex-PRESS shunt is associated with a reduced rate of early postoperative hypotony.13,14,16,17,20 None of the studies reported any difference in the occurrence of other complications or long-term safety with the Ex-PRESS shunt. An assessment of bleb morphology also demonstrated no differences between the 2 procedures.17
A recent Ophthalmic Technology Report by the American Academy of Ophthalmology focused on novel glaucoma procedures including a review of previously reported information on the Ex-PRESS shunt. All studies were categorized as level III incidence, except for 1 nonrandomized retrospective study13 that was categorized as level II evidence. The conclusion was that available data are insufficient to demonstrate any superiority or inferiority between the Ex-PRESS shunt and standard trabeculectomy. The only advantage noted with the Ex-PRESS shunt is the reduced rate of early postoperative hypotony, and it was suggested to reflect the more uniform filtration through the standard-sized internal lumen of the device.12 Another theoretical advantage of the Ex-PRESS shunt is a reduced rate of early postoperative intraocular inflammation, as iridotomy is not performed.
Our study revealed no significant differences in IOP reduction, the need for additional IOP-lowering medications postoperatively, rates of complete and qualified success, or in the occurrence of any complications between the Ex-PRESS shunt and standard trabeculectomy. These results echo those that have been reported by most previous comparative studies,13–17 and we believe that they are further proof of the equal efficacy and safety of these 2 procedures. As noted earlier, the Ex-PRESS shunt was originally designed as a simpler surgical procedure to achieve aqueous filtration to a subconjunctival bleb with similar results to trabeculectomy.5 However, when implanted under a sclera flap, the procedure is almost the same as standard trabeculectomy. Therefore, it is not surprising that results of both the procedures are very similar.
In our subanalysis, similar efficacy and safety were demonstrated between the Ex-PRESS shunt and trabeculectomy when performed as the first procedure for lowering IOP (Fig. 2). One study reported the Ex-PRESS shunt as an alternative procedure after failed previous trabeculectomy.20 Excluded from the subanalysis were 11 patients who underwent repeated surgery, 3 who underwent re-trabeculectomy and 8 who underwent Ex-PRESS shunt implantation. The number of these cases was too small to perform valid statistical comparisons between them, but similar results were recorded in both subgroups.
Our second subanalysis demonstrated no significant differences in the results between phakic and pseudophakic eyes. This finding is consistent with previous reports on the efficacy of the Ex-PRESS shunt in combination with cataract extraction.6,21 It has also been demonstrated that the Ex-PRESS is equally effective both alone and when performed with cataract extraction.22
No patient characteristic or surgical detail was correlated with the success or failure of the performed procedure. The Ex-PRESS shunt was not superior to standard trabeculectomy in patients with “complex glaucomas” or who had undergone previous surgery. This is of clinical importance, as these findings imply that there is no basis for preoperative evaluation that could guide the surgeon in the selection of procedure to perform. It should be noted that our complication and failure rates were comparable to those reported in the TVT study at the same postoperative time.23
In light of the seemingly equal efficacy and safety of the Ex-PRESS shunt and standard trabeculectomy, one should take into consideration the economic difference between them. A recent US study reported the disposable item cost for Ex-PRESS shunt to be 3.5 times higher than for trabeculectomy ($1203 vs. $339, respectively). From the economic perspective, it was concluded that standard trabeculectomy was “the ‘best buy’ for a glaucoma patient’s health care dollar when the necessary indications are met.”24 As there are no proven indications for favoring the Ex-PRESS shunt, this means that trabeculectomy is a significantly more cost-effective procedure for IOP reduction in glaucoma patients. In our institution, the Ex-PRESS shunt implantation also costs about $800 more than trabeculectomy. A Canadian comparative study of the economic differences between the Ex-PRESS shunt and trabeculectomy calculated an incremental cost-effectiveness ratio of $9913 for 1 year success gain favoring standard trabeculectomy.25 Another recent review has reported that the Ex-PRESS shunt was not associated with significantly different rates of success or complications, and predicted that its markedly higher cost will be a major limitation in its adoption into clinical practice.26
Limitations of this study include its retrospective nature and sample size. However, it should be noted that most previous studies included fewer patients, and ours is among the largest series directly comparing the Ex-PRESS shunt and trabeculectomy. Whereas previous studies included mostly POAG patients,14,16,18,19 our study included a variety of glaucoma types. We note that no difference was found between the 2 procedures in any of the glaucoma types—POAG, PXF, and the “complex glaucomas.” Another potential limitation is the fact that lens status and number of previously operated eyes were different at baseline between the 2 groups. However, subanalyses controlling for these parameters were performed, and have shown that the results were not affected by these differences. Finally, it should be noted that in our series the P-200 Ex-PRESS shunt was used, whereas most previous studies included the R-50 shunt.
In conclusion, we have found no significant differences in the efficacy or safety between the Ex-PRESS shunt and standard trabeculectomy in IOP reduction in glaucoma patients. None of the preoperative patient characteristics or surgical details has proven to be associated with the success or failure of any procedure. We believe our series represents the clinical reality in Ex-PRESS use—it is used in all types of glaucoma, with no clear indications guiding its selection. On the basis of our results and literature review, it seems that using the Ex-PRESS is not associated with any improvement in efficacy or safety. The only advantage it offers is a reduced rate of early hypotony, but this short-term difference was never shown to translate into a clinically significant better outcome. The only clear difference between the procedures is in cost, with the Ex-PRESS shunt being much more expensive than trabeculectomy. We believe that in current practice, in the majority of cases the investment in the Ex-PRESS shunt does not produce any added value to glaucoma patient care and is therefore unjustified. In our opinion, the Ex-PRESS shunt should not be used as a primarily surgical procedure for IOP reduction. It may serve as a secondary procedure after failed trabeculectomy,20 but comparative studies in such cases have not been conducted, and it is likely that glaucoma drainage devices are preferable for this purpose.27,28 Further prospective randomized clinical studies comparing the 2 techniques are required to formulate indications for Ex-PRESS use that would guide its selection in a cost-effective manner.
Footnotes
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.Coleman AL. Advances in glaucoma treatment and management: surgery. Invest Ophthalmol Vis Sci. 2012;53:2491–2494. [DOI] [PubMed] [Google Scholar]
- 2.Cairns D. Trabeculectomy: a preliminary report of a new method. Am J Ophthalmol. 1968;66:673–679. [PubMed] [Google Scholar]
- 3.Borisuth NS, Phillips B, Krupin T. The risk profile of glaucoma filtration surgery. Curr Opin Ophthalmol. 1999;10:112–116. [DOI] [PubMed] [Google Scholar]
- 4.Gedde SJ, Herndon LW, Brandt JD, et al. Surgical complications in the Tube Versus Trabeculectomy Study during the first year of follow-up. Am J Ophthalmol. 2007;143:23–31. [DOI] [PubMed] [Google Scholar]
- 5.Mermoud A. Ex-PRESS implant. Br J Ophthalmol. 2005;89:396–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Traverso CE, De Feo F, Messas-Kaplan A, et al. Long term effect on IOP of a stainless steel glaucoma drainage implant (Ex-PRESS) in combined surgery with phacoemulsification. Br J Ophthalmol. 2005;89:425–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart RM, Diamond JG, Ashmore ED, et al. Complications following Ex-PRESS glaucoma shunt implantation. Am J Ophthalmol. 2005;140:340–341. [DOI] [PubMed] [Google Scholar]
- 8.Tavolato M, Babighian S, Galan A. Spontaneous extrusion of a stainless steel glaucoma drainage implant (Ex-PRESS). Eur J Ophthalmol. 2006;16:753–755. [PubMed] [Google Scholar]
- 9.Dahan E. Subconjunctival insertion of Ex-PRESS R-50 miniature glaucoma implant. J Cataract Refract Surg. 2008;34:716. [DOI] [PubMed] [Google Scholar]
- 10.Wamsley S, Moster MR, Rai S, et al. Results of the use of the Ex-PRESS miniature glaucoma implant in technically challenging advanced glaucoma cases: a clinical pilot study. Am J Ophthalmol. 2004;138:1049–1051. [DOI] [PubMed] [Google Scholar]
- 11.Dahan E, Carmichael TR. Implantation of a miniature glaucoma device under a sclera flap. J Glaucoma. 2005;14:98–102. [DOI] [PubMed] [Google Scholar]
- 12.Francis BA, Singh K, Lin SC, et al. Novel glaucoma procedures. A report by the American Academy of Ophthalmology. Ophthalmology. 2011;118:1466–1480. [DOI] [PubMed] [Google Scholar]
- 13.Maris PJG, Ishida K, Netland PA. Comparison of trabeculectomy with Ex-PRESS miniature glaucoma device implanted under sclera flap. J Glaucoma. 2007;16:14–19. [DOI] [PubMed] [Google Scholar]
- 14.Dahan E, Ben Simon GJ, Lafuma A. Comparison of trabeculectomy and Ex-PRESS implantation in fellow eyes of the same patient: a prospective, randomized study. Eye. 2012;26:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seider MI, Rofagha S, Lin SC, et al. Resident-performed Ex-PRESS shunt implantation versus trabeculectomy. J Glaucoma. 2012;21:469–474. [DOI] [PubMed] [Google Scholar]
- 16.Marzette L, Herndon LW. A comparison of the Ex-PRESS mini glaucoma shunt with standard trabeculectomy in the surgical treatment of glaucoma. Ophthalmic Surg Lasers Imaging. 2011;42:453–459. [DOI] [PubMed] [Google Scholar]
- 17.Good TJ, Kahook MY. Assessment of bleb morphologic features and postoperative outcomes after Ex-PRESS drainage device implantation versus trabeculectomy. Am J Ophthalmol. 2011;151:507–513. [DOI] [PubMed] [Google Scholar]
- 18.de Jong LAMS. The Ex-PRESS glaucoma shunt versus trabeculectomy in open-angle glaucoma: a prospective randomized study. Adv Ther. 2009;26:336–345. [DOI] [PubMed] [Google Scholar]
- 19.de Jong L, Lafuma A, Aguade AS, et al. Five-year extension of a clinical trial comparing the EX-PRESS glaucoma filtration device and trabeculectomy in primary open-angle glaucoma. Clin Ophthalmol. 2011;5:527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lankaranian D, Razeghinejad MR, Prasad A, et al. Intermediate-term results of the Ex-PRESS miniature glaucoma implant under a sclera flap in previously operated eyes. Clin Exp Ophthalmol. 2011;39:421–428. [DOI] [PubMed] [Google Scholar]
- 21.Rivier D, Roy S, Mermoud A. Ex-PRESS R-50 miniature glaucoma implant insertion under the conjunctiva combined with cataract extraction. J Cataract Refract Surg. 2007;33:1946–1952. [DOI] [PubMed] [Google Scholar]
- 22.Kanner EM, Netland PA, Sarkisian SR, Jr, et al. Ex-PRESS miniature glaucoma device implanted under a scleral flap alone or combined with phacoemulsification cataract surgery. J Glaucoma. 2009;18:488–491. [DOI] [PubMed] [Google Scholar]
- 23.Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the Tube Versus Trabeculectomy Study after one year of follow-up. Am J Ophthalmol. 2007;143:9–22. [DOI] [PubMed] [Google Scholar]
- 24.Valentine J, Zurakowski D, Ayyala RS. Comparison of acquisition costs of surgical supplies in different health care systems for cataract and glaucoma procedures. J Glaucoma. 2012Dec 13 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 25.Buys YM, Patel H, Drori Wagschal L, et al. Economic evaluation of ExPRESS versus trabeculectomy [abstract]. 2012 [Google Scholar]
- 26.Buys YM. Trabeculectomy with ExPRESS: weighing the benefits and cost. Curr Opin Ophthalmol. 2013;24:111–118. [DOI] [PubMed] [Google Scholar]
- 27.Gedde SJ, Schiffman JC, Feuer WJ, et al. Tube versus Trabeculectomy Study Group. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153:789–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gedde SJ, Singh K, Schiffman JC, et al. Tube Versus Trabeculectomy Study Group. The Tube Versus Trabeculectomy Study: interpretation of results and application to clinical practice. Curr Opin Ophthalmol. 2012;23:118–126. [DOI] [PubMed] [Google Scholar]


