Abstract
Purpose:
To prospectively investigate the incidence of postoperative ptosis following trabeculectomy by comparing preoperative and postoperative margin reflex distance (MRD), and to analyze the clinical factors associated with ptosis.
Patients and Methods:
Patients who underwent trabeculectomy with mitomycin C in unilateral eye between 2010 and 2012 were enrolled. MRD was measured before and 3 and 6 months after trabeculectomy. The MRD is the distance between the light reflex at central cornea and the upper eyelid margin when the patient gazed at a pen light placed 50 cm away straightly. Postoperative ptosis was defined as a decrease in MRD≥2 mm from preoperative level. The correlation among ΔMRD (difference between preoperative and 6 mo postoperative MRD) and clinical factors comprising age, spherical equivalent, preoperative MRD, 6-month postoperative intraocular pressure (IOP), and IOP reduction (difference between preoperative and 6 mo postoperative IOP) was analyzed.
Results:
Thirty-six patients (36 eyes) were analyzed. Preoperative median MRD was not different between the operated eye and nonoperated fellow eye (both 4.0 mm, P=0.65). The 3- and 6-month postoperative MRD in the operated eye were significantly reduced compared with preoperative MRD (3.0 mm, P=0.04 and 2.5 mm, P=0.01, respectively). The 3- and 6-month postoperative MRD in the nonoperated eye were not different from preoperative MRD (4.0 mm, P=0.81 and 4.0 mm, P=0.85, respectively). The incidence of ptosis at 6 months after operation was 19% (7 of 36 eyes). The IOP was significantly decreased at 3 and 6 months after operation (both P<0.01). No correlation was observed between ΔMRD and all the factors analyzed.
Conclusions:
Ptosis is a major complication following trabeculectomy with mitomycin C, with an incidence of 19% at 6 months after operation.
Key Words: glaucoma, surgery, trabeculectomy, complication, ptosis, margin reflex distance
Trabeculectomy has become the most common procedure for surgical management of glaucoma that cannot be controlled with medical or laser treatment. Although trabeculectomy with mitomycin C has been reported to achieve control of intraocular pressure (IOP) in 60% to 71% of the patients at 3 to 8 years after operation,1–4 various postoperative complications including corneal astigmatism, dellen, cataract, and bleb-related infection may occur despite good control of IOP.5,6
Ptosis is also a postoperative complication following trabeculectomy. The incidence has been reported to range from 8% to 12% at 1 month to several years after operation.7–9 Among these previous reports, the only prospective study did not specify the definition of ptosis,7 and the 2 studies that reported the incidence of ptosis as defined by a change in margin reflex distance (MRD) before and after trabeculectomy were retrospective in design.8,9 Moreover, the clinical factors associated with the development of ptosis have not been investigated in detail.
The purpose of the present study was to prospectively investigate the incidence of postoperative ptosis following trabeculectomy by measuring the MRD before and after surgery, and to analyze the clinical factors associated with the development of ptosis.
MATERIALS AND METHODS
Subjects
Patients who underwent trabeculectomy in unilateral eye performed by the same surgeon (K.M.) between 2010 and 2012 at Tokyo Medical University Hospital were enrolled. Patients with a history of intraocular surgery including laser treatment, a history of extraocular surgery involving the orbit or eyelid, or endocrinological or neurological diseases that affect the eyelid morphology were excluded. Patients who underwent other procedures simultaneously, or required additional intraocular surgery in bilateral eyes within 6 months after the primary trabeculectomy were also excluded. The present study was approved by the ethical committee of Tokyo Medical University (Application No. 1986). The study was conducted in compliance with the Helsinki of Declaration. All patients gave informed consent before participation in the study.
In all patients, MRD in both eyes were measured by the same and unblinded examiner (A.N.-T.) before trabeculectomy, and 3 and 6 months after trabeculectomy. The MRD is the distance between the light reflex at central cornea and the upper eyelid margin when the patient gazed at a pen light placed 50 cm away straightly. Postoperative ptosis was defined as a decrease in MRD of ≥2 mm from the preoperative level.
Trabeculectomy Procedure
A sliding type lid speculum was used to open the eyelids. After instilling 4% lidocaine eye drops (Xylocaine Ophthalmic Solution 4%; AstraZeneca K.K., Osaka), a fornix-based conjunctival flap was constructed at the superior temporal quadrant. Conjunctiva and Tenon capsule were dissected together from the sclera, and 1.5 mL of 2% lidocaine (Lidocaine for Intravenous Injection 2% Syringe; Terumo Co. Ltd., Tokyo) was injected into sub-Tenon capsule with a blunt injection needle. After cauterizing the blood vessel on the surface of the sclera, a scleral flap one half the thickness of the sclera was made. The shape of the scleral flap was square, and its size was approximately 3×3 mm. Small pieces of surgical sponge soaked in mitomycin C (Mitomycin Injection 2 mg; Kyowa Hakko Kirin Co. Ltd., Tokyo) dissolved in saline to a concentration of 0.4 mg/mL (0.04%) were placed under the conjunctival flap for 3 minutes. After the sponge pieces were removed, the area was irrigated with a balanced salt solution. At the edge of the corneoscleral bed, a block of clear corneal and trabecular meshwork tissue was removed and peripheral iridectomy was performed. The scleral flap was sutured using 10-0 nylon with spatula needle (10-0 Nylon Black Mono, with needle, code 1404; Mani Co. Ltd., Tochigi), adjusted so that no shallowing of the anterior chamber was observed. The conjunctival flap was closed using 10-0 nylon suture. All these procedures were performed without a bridle suture through the superior rectus muscle or holding the muscle by forceps. When necessary, the eyeball was stabilized by a 7-0 silk (Alcon Suture Silk; Alcon Japan Co. Ltd., Tokyo) suture placed at the peripheral cornea.
Postoperative IOP increase was controlled by eye globe massage, laser suture lysis, and/or needling. Postoperative hypotony was managed by transconjunctival resuturing of the scleral flap10 or compression suture11 when necessary. Levofloxacin (Cravit ophthalmic solution; Santen Pharmaceutical, Osaka, Japan) and 0.1% betamethasone (Rinderon ophthalmic solution; Shionogi, Osaka, Japan) were prescribed as postoperative medications to be taken 4 times daily for 3 months.
Outcome Measures and Statistical Analyses
Mann-Whitney U tests were used to compare preoperative MRD versus 3- and 6-month postoperative MRD in both eyes, and paired t tests were used to compare preoperative IOP versus 3- and 6-month postoperative IOP in the operated eye. Postoperative ptosis in the operated eye was defined as a decrease in MRD of ≥2 mm compared with preoperative level, and the incidence of 6-month postoperative ptosis was calculated. Wilcoxon signed-rank tests were used to compare the preoperative and 3- and 6-month postoperative MRD of the operated eye with those of the nonoperated eye. Spearman correlation was used to investigate correlation among ΔMRD (difference between preoperative MRD and 6 mo postoperative MRD) and clinical factors comprising age, spherical equivalent, preoperative MRD, 6-month postoperative IOP, and IOP reduction (difference between preoperative IOP and 6 mo postoperative IOP). Statistical analyses of all data were performed using MedCalc version 12.1.4.0 (MedCalc Software bvba, Mariakerke, Belgium). A P-value <0.05 was considered significant.
RESULTS
Clinical Findings of Subjects
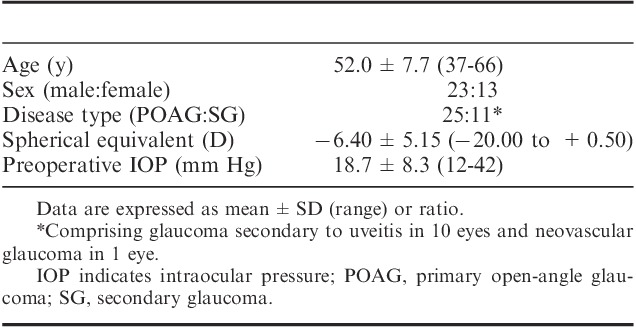
Initially 37 patients (37 eyes) were enrolled. Among them, 1 patient was transferred to another hospital 4 months after trabeculectomy. Eventually, 36 patients (36 eyes) were analyzed. All patients were Japanese. The patient background is shown in Table 1. None of the patients had intraoperative complications. During operation, suturing at the peripheral cornea to stabilize the eyeball was done in 5 patients. During 6 months after operation, laser suture lysis was conducted in 26 eyes and needling in 4 eyes for control of IOP increase. For management of hypotony, transconjunctival scleral flap resuturing was performed in 6 eyes, and compression suture in 1 eye.
TABLE 1.
Patient Background
Comparisons of MRD and IOP
The MRD and IOP measured before and after operation are shown in Table 2, and the box-and-whisker plots for MRD measured before and after operation are presented in Figure 1. Preoperative MRD did not differ between the operated and nonoperated eyes. In the operated eye, the 3- and 6-month postoperative MRD were significantly reduced compared with preoperative MRD. The 3- and 6-month postoperative MRD of the operated eye were significantly lower than those of the nonoperated eye. The IOP of the operated eye was reduced significantly after operation.
TABLE 2.
MRD and IOP Measured Before and After Trabeculectomy
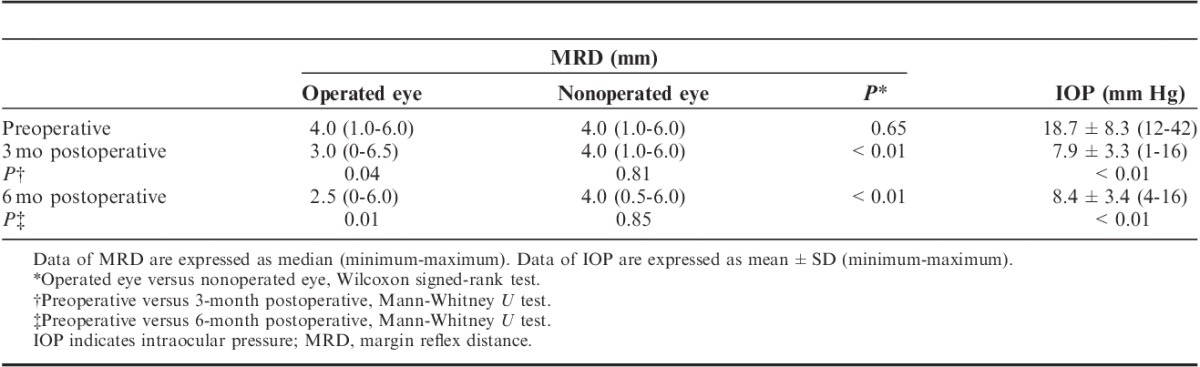
FIGURE 1.
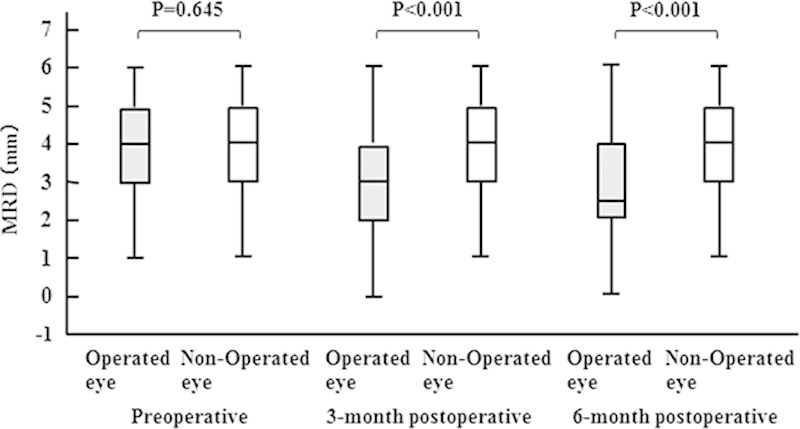
Box-and-whisker plots showing the distribution profiles of MRD measured before and after operation. The box encloses the 25th to 75th percentile of the data; whiskers define lowest and highest observation. The line through the box is the median. Outlier points are not shown. MRD indicates margin reflex distance.
The histograms of ΔMRD at 3 and 6 months after operation are shown in Figure 2. Five of 36 eyes (14%) at 3 months, and 7 of 36 eyes (19%) at 6 months after operation had MRD reduced by ≥2 mm compared with preoperative MRD, hence the incidence of ptosis was 19%.
FIGURE 2.
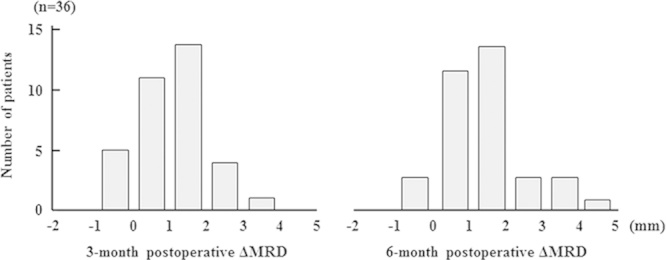
Histogram of ΔMRD at 3 and 6 months after operation. MRD indicates margin reflex distance; ΔMRD, difference between preoperative MRD and 6-month postoperative MRD.
Relationship Between Change in MRD and Clinical Factors
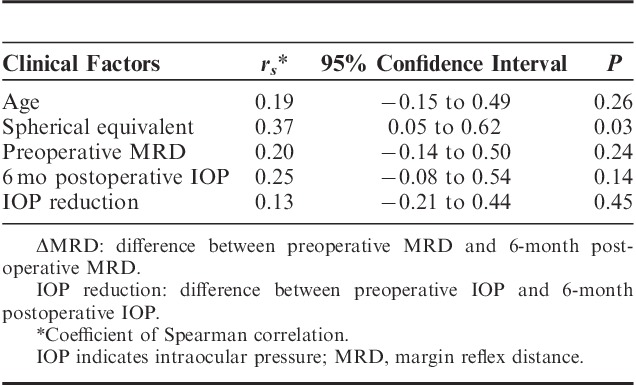
Table 3 shows the correlation between ΔMRD and clinical factors comprising age, spherical equivalent, preoperative MRD, 6-month postoperative IOP, and IOP reduction. The correlation observed between ΔMRD and all the factors was weak.
TABLE 3.
Correlation Between ΔMRD and Clinical Factors
DISCUSSION
We conducted a prospective study to examine the incidence of ptosis following trabeculectomy with mitomycin C. Our results showed significant decreases in MRD after trabeculectomy when compared with preoperative MRD and when compared with MRD of the nonoperated eyes. The incidence of ptosis at 6 months after operation was 19%, and no clinical factor associated with ptosis was identified.
The incidence of ptosis after trabeculectomy has been reported to range from 8% to 12% at 1 month to several years postoperatively.7–9 Among these previous reports, the only prospective study by Jampel et al7 examined the early complications of 465 eyes that underwent trabeculectomy among subjects entered in a multicenter randomized controlled trial comparing trabeculectomy versus topical medications as the initial treatment for open-angle glaucoma; the Collaborative Initial Glaucoma Treatment Study. Ptosis occurred at a frequency of 12% in the first month after operation, but this report did not specify the diagnostic criteria of ptosis, and ptosis was judged subjectively by the examiners. In contrast, 2 retrospective studies that examined the frequency of ptosis following trabeculectomy defined ptosis as a decrease in MRD of ≥2 mm from preoperative level. The incidence of ptosis at 6 months after trabeculectomy was 11% (n=105 eyes) in the study by Song et al8 and 8% (n=13 eyes) in the study by Altieri et al.9 Our prospective study demonstrated an incidence of ptosis of 19% at 6 months following trabeculectomy. We cannot explain the higher incidence of ptosis in our study than in previous reports.
Although there is no report that compares the incidence of postoperative ptosis for trabeculectomy with that for other intraocular surgeries, ptosis seems to occur at a higher frequency following trabeculectomy than after cataract surgery. Altieri et al9 found that ptosis occurred in 4 of 97 eyes (4%) that underwent phacoemulsification and intraocular lens implantation compared with 1 in 13 eyes (8%) that underwent trabeculectomy (no statistical comparison). Other studies also reported that postoperative ptosis occurred after cataract surgery at rates ranging from 5% to 14%,12–15 and the surgeries in these studies used larger incisions and regional anesthesia. The frequency of ptosis is expected to be even lower in recent cataract surgeries, which use small incisions under topical anesthesia. Hence the incidence of ptosis following trabeculectomy is speculated to be higher than after cataract surgery.
In general, ptosis that arises after ophthalmic surgeries are associated with myogenic or neurogenic factors due to anesthetic effects, mechanical factors due to edema or hematoma of the eyelid, or aponeurotic factors due to traction on the aponeurosis of the levator palpebrae muscle separating it from the tarsal plate.16,17 Whereas ptosis caused by myogenic, neurogenic, or mechanical factors would improve with time after operation, ptosis caused by aponeurotic factor likely persists. Traction on the levator aponeurosis has been reported to be caused by traction of the superior rectus muscle complex by bridle suture or forceps, traction due to the lid speculum, or excessive infraduction.13,15,18 In trabeculectomy, the above-mentioned manipulations are often necessary to obtain an adequate surgical field, which may partially account for the high incidence of ptosis. In addition, use of antimetabolites, postoperative globe massage or needling, chronic stimulation of the eyelid by the filtering bleb, and other factors may also contribute to the high incidence. Further analysis of the association of these factors with ptosis is necessary.
In the present study, no correlation was observed between ΔMRD and any of the clinical factors studied, comprising age, spherical equivalent, preoperative MRD, 6-month postoperative IOP, and IOP reduction. Moreover, the existence of intraoperative traction suture at the peripheral cornea or postoperative intervention (laser suture lysis, needling, transconjunctival scleral flap resuturing, or compression suture) did not affect the incidence of ptosis (the data are not shown). This may be due to several factors such as the small number of cases in this series, subjects limited to younger patients who underwent trabeculectomy only, and short follow-up period. Further study is required.
This study has several limitations. First, postoperative observation was conducted for a short period of 6 months, and MRD was measured by unblinded examiner. Second, to exclude the effect of other surgical modalities, patients undergoing simultaneous trabeculectomy and cataract surgery as well as those with a history of ocular surgery were excluded, which prevented entry of elderly patients. As older persons tend to have weakened elevator aponeurosis, there is a possibility that the incidence of postoperative ptosis increases with age, but this possibility could not be examined in the present study. Third, the morphology and property of the filtering bleb may also affect the incidence of ptosis. However, the morphology of the filtering bleb varied diversely among patients, and could not be grouped easily for analysis. Further observer-masked study should include elderly patients, observation for a prolonged period, and analysis of the relationship between bleb findings and ptosis.
In the present prospective study that examined the incidence of ptosis following trabeculectomy by measuring preoperative and postoperative MRD, ptosis was observed in 19% of the patients at 6 months after trabeculectomy. For glaucoma patients with visual field defect, the additional visual field impairment due to ptosis will further decrease the quality of vision. Attention has to be given to ptosis as a major complication following trabeculectomy with mitomycin C.
Footnotes
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.Fontana H, Mahdavi KN, Lumba J, et al. Trabeculectomy with mitomycin C: outcome and risk factor for failure in phakic open-angle glaucoma. Ophthalmology. 2006;113:930–936. [DOI] [PubMed] [Google Scholar]
- 2.Law SK, Shih K, Tran DH, et al. Long-term outcome of repeat vs. initial trabeculectomy in open-angle glaucoma. Am J Ophthalmol. 2009;148:685–691. [DOI] [PubMed] [Google Scholar]
- 3.Shigeeda T, Tomidokoro A, Chen YN, et al. Long-term follow-up initial trabeculectomy with mitomycin C for primary open-angle glaucoma in Japanese patients. J Glaucoma. 2006;15:195–199. [DOI] [PubMed] [Google Scholar]
- 4.Beckers HJ, Kinders KC, Webers CA. Five-year results of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2003;241:106–110. [DOI] [PubMed] [Google Scholar]
- 5.Fellman R.Shaarawy TM. Trabeculectomy. Glaucoma Surgical Management. 2009Amsterdam: Elsevier;p111–p150. [Google Scholar]
- 6.Allingham RR, Damji KF, Freedman S, et al. Allingham RR. Filtering surgery. Shields Textbook of Glaucoma. 2011:6th edPhiladelphia: Lippincott Williams & Wilkins;487–523. [Google Scholar]
- 7.Jampel HD, Musch DC, Gillespie BW, et al. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol. 2005;140:16–22. [DOI] [PubMed] [Google Scholar]
- 8.Song MS, Shin DH, Spoor TC. Incidence of ptosis following trabeculectomy: a comparative study. Korean J Ophthalmol. 1996;10:97–103. [DOI] [PubMed] [Google Scholar]
- 9.Altieri M, Truscott E, Kingston AE. Ptosis secondary to anterior segment surgery and its repair in a two-year follow up study. Ophthalmologica. 2005;219:129–135. [DOI] [PubMed] [Google Scholar]
- 10.Shirato S, Maruyama K, Haneda M. Resuturing the scleral flap through conjunctiva for treatment of excess filtration. Am J Ophthalmol. 2004;137:173–174. [DOI] [PubMed] [Google Scholar]
- 11.Haynes WL, Alward WLM. Combination of autologous blood injection and bleb compression sutures to treat hypotony maculopathy. J Glaucoma. 1998;8:384–387. [PubMed] [Google Scholar]
- 12.Feibel RM, Custer PL, Gordon MO. Postcataract ptosis: a randomized, double-masked comparison of peribulbar and retrobulbar anesthesia. Ophthalmology. 1993;100:660–665. [DOI] [PubMed] [Google Scholar]
- 13.Loeffler M, Solomon LD, Renaud M. Postcataract extraction ptosis, effect of the bridle suture. J Cataract Refract Surg. 1989;16:501–504. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan LJ, Jaffe NS, Clayman HM. Ptosis and cataract surgery. A multivariant computer analysis of a prospective study. Ophthalmology. 1985;92:237–242. [DOI] [PubMed] [Google Scholar]
- 15.Paris GL, Quickert MH. Disinsertion of the aponeurosis of the levator palpebrae superioris muscle after cataract extraction. Am J Ophthalmol. 1976;81:337–340. [DOI] [PubMed] [Google Scholar]
- 16.Mehat MS, Sood V, Madge S. Blepharoptosis following anterior segment surgery: a new theory for an old problem. Orbit. 2012;31:274–278. [DOI] [PubMed] [Google Scholar]
- 17.Beard C.Beard C. Type of ptosis. Ptosis. 1981:3rd edSt Louis: CV Mosby;39–76. [Google Scholar]
- 18.Alpar JJ, Jaffe NS, Clayman HM. Ptosis following cataract and glaucoma surgery. Glaucoma. 1982;4:66–68. [Google Scholar]


