Abstract
Patients with knee osteoarthritis often present with signs of mixed tibiofemoral and patellofemoral joint disease. It has been suggested that altered frontal and transverse plane knee joint mechanics play a key role in compartment-specific patterns of knee osteoarthritis, but invivo evidence in support of this premise remains limited. Using Dynamic Stereo X-ray techniques, the aim of this study was to compare the frontal and transverse plane tibiofemoral kinematics and patellofemoral malalignments during the loading response phase of downhill gait in three groups of older adults: patients with medial tibiofemoral compartment and coexisting patellofemoral osteoarthritis (n=11); patients with lateral tibiofemoral compartment and coexisting patellofemoral osteoarthritis (n=10); and an osteoarthritis-free control group (n=22). Patients with lateral compartment osteoarthritis walked with greater and increasing degrees of tibiofemoral abduction compared to the medial compartment osteoarthritis and the control groups who walked with increasing degrees of tibiofemoral adduction. Additionally, the medial and lateral compartment osteoarthritis groups demonstrated reduced degrees of tibiofemoral internal rotation compared to the control group. Both medial and lateral compartment osteoarthritis groups also walked with increasing degrees of lateral patella tilt and medial patella translation during the loading response phase of downhill gait. Our findings suggest that despite the differences in frontal and transverse plane tibiofemoral kinematics between patients with medial and lateral compartment osteoarthritis, the malalignments of their arthritic patellofemoral joint appears to be similar. Further research is needed to determine if these kinematic variations are relevant targets for interventions to reduce pain and disease progression in patients with mixed disease.
Keywords: Patellofemoral Joint, Tibiofemoral Joint, Knee Osteoarthritis, Biomechanics, Kinematics
INTRODUCTION
Osteoarthritis (OA) is one of the leading causes of mobility limitation and chronic disability in the elderly (Ma et al., 2014). With nearly a 50% lifetime risk of developing symptomatic disease, the knee is one of the joints most commonly affected by OA (Murphy et al., 2008), with up to 13.3 million cases of knee OA in the US alone (Dillon et al., 2006). Although knee OA can develop in either the medial or the lateral tibiofemoral (TF) joint, medial compartment OA appears to be more common than lateral compartment disease (Dillon et al., 2006; Felson et al., 2002). To this end, frontal-plane mechanics of the TF joint have been deemed as a key determinant of compartment-specific patterns of TF OA. Whereas the more commonly observed genu varum malalignment of the TF joint leads to higher mechanical loading and increased risk of medial compartment OA development, genu valgum increases the risk of lateral TF compartments involvement (Sharma et al., 2010; Tanamas et al., 2009; Yang et al., 2010).
Different and diverging patterns of frontal and transverse plane TF joint motion and loading patterns have also been previously reported during gait for patients with medial and lateral compartment knee OA (Butler et al., 2011; Weidow et al., 2006). More specifically, patients with medial compartment OA generally walk with greater frontal plane knee adduction angles and moments that are believed to lead to increased loading of the medial TF compartment (Zhao et al., 2007). Conversely, patients with lateral TF OA commonly walk with increasing knee abduction angles but lower peak knee adduction moments that are thought to shift a greater portion of the compressive knee joint loads to the lateral TF compartment (Agneskirchner et al., 2007). Reduced transverse plane TF joint internal rotation has also been reported for patients with medial compartment OA compared to those with lateral compartment disease (Weidow et al., 2006). It has been suggested that the reduction in TF internal rotation may be a compensatory mechanism to decrease anterior translation of the medial TF condyle over the central and anterior regions of the medial TF compartment, where cartilage damage is commonly observed (Saari et al., 2005; Weidow et al., 2002).
Although, knee OA is predominantly viewed as a disease that affects the TF joint; the involvement of the patellofemoral (PF) joint has gained more attention as of late. In a recent magnetic resonance imaging assessment of 970 knees, PF joint structural damage was deemed to be at least as common as, if not more common than, TF Joint damage (Stefanik et al., 2013). Evidence further suggests that the prevalence of mixed TF and PF OA in older adults with painful knees is much higher (40%) compared to either TF OA (4%) or PF OA (24%) in isolation (Duncan et al., 2006). Given the inherent anatomical relationship between the TF and PF joints, it has been suggested that the abnormal frontal and transverse plane motions of the TF joint can influence the congruency of the patella within the trochlear groove, leading to altered stress distributions that can contribute to the pathomechanics of the PF joint (Powers, 2003). For instance, excessive TF abduction is thought to increase the lower extremity Q-angle (the angle between the quadriceps load vector and the patellar tendon load vector), leading to increased lateral patella tilt, lateral patella translation, and greater lateral patella facet compressive forces (Huberti and Hayes, 1984; Mizuno et al., 2001). Conversely, excessive TF adduction is thought to decrease the Q-angle, increasing the medial patella tilt and translation, thus leading to increased compressive loading of the medial patella facet (Huberti and Hayes, 1984; Mizuno et al., 2001). Similarly, while excessive TF external rotation in the transverse plane increases the contact stresses on the lateral PF joint facet, excessive internal rotation of the TF joint places greater loads on the medial side of the PF joint (Lee et al., 1994).
Currently, direct in-vivo quantification of the joint contact loads in patients with mixed knee OA is not feasible. However, considerations for knee joint kinematics can describe the relative positioning of the articular surfaces with respect to the line of action of the ground reaction and muscle forces to provide a surrogate indicator of how contact loads are distributed within the TF and PF joints. Therefore, the aim of the current study was to compare the frontal and transverse plane kinematics of the TF joint along with measures of PF joint malalignment during the loading response phase of downhill gait in three groups of older adults: patients with medial TF compartment and coexisting PF OA (medial OA); patients with lateral TF compartment and coexisting PF OA (lateral OA); and an OA-free control group (control). It was hypothesized that patients with medial compartment OA would walk with greater degrees of TF joint adduction/external rotation and greater medial patella tilt/translation compared to the control group. It was also hypothesized that patients with lateral compartment OA would walk with greater TF joint abduction/internal rotation and greater lateral patella tilt/translation compared to their control counterparts.
MATERIALS AND METHODS
Participants
Forty-three participants were recruited for this study (Table 1). All participants with knee OA met the American College of Rheumatology clinical classification criteria for knee OA (Altman et al., 1986) and had evidence of radiographic TF and PF OA of grade II or greater according to the Kellgren and Lawrence (KL) scale (Kellgren and Lawrence, 1957). Participants with primary medial compartment TF OA and coexisting PF OA comprised the medial OA group, whereas those with primary lateral compartment TF OA and coexisting PF OA made up the lateral OA group. In addition, 22 subjects without evidence of radiographic TF or PF OA who reported no history of knee pain served as the control group. Subjects were excluded if they required an assistive device or a rest break to ambulate a distance of 30.5m (100 feet) or reported two or more falls within the past year. All participants signed a consent form approved by the Institutional Review Board of the University of Pittsburgh prior to participation in the study.
Table 1.
Mean subject demographics.
| Demographics | OA-free Control (N = 22) | Medial Knee OA (N = 11) | Lateral Knee OA (N = 10) | P-value |
|---|---|---|---|---|
| Age (years) | 68.1 (7.0) | 70.3 (10.0) | 73.1 (9.5) | 0.31 |
| Female (%) | 11 (50.0) | 7 (63.6) | 3 (30.0) | 0.30 |
| Height (cm) | 174.8 (13.0) | 171.4 (11.9) | 172.7 (6.7) | 0.72 |
| Weight (kg) | 77.1 (16.6) | 86.8 (17.9) | 77.5 (7.5) | 0.22 |
| BMI (kg/m2) | 25.1 (3.7) | 29.6 (5.7)* | 26.0 (1.6) | 0.01 |
OA = Osteoarthritis; BMI = body mass index; Values are mean (SD) or N (%).
Significantly different than the control group
Dynamic Stereo X-ray Testing
Dynamic Stereo X-ray (DSX) methods were used to quantify 3-dimensional (3D) TF and PF joint kinematics from biplane radiographic images. The biplane X-ray system contained two X-ray gantries that were configured with their beam paths intersecting at 60° in a plane parallel to the floor. Each gantry contained a 100 kW pulsed X-ray generator (CPX 3100CV; EMD Technologies, Quebec, Canada), a 40 cm image intensifier (Thales, Neuilly-sur-Seine, France), and a high-speed 4 megapixel digital video camera (Phantom v10, Vision Research, Wayne, New Jersey, USA). The X-ray generators were customized to provide short-duration pulses at very high repetition rates. For the current study, radiographs were generated with a 1 ms pulse width at 100 Hz, with a maximum radiographic protocol of 90 kVp/200 mA and a 1 second collection time (100 ms total x-ray exposure) per trial.
Participants’ knees were imaged during a downhill gait condition (7% grade, 0.75 m/s) on an instrumented treadmill (Bertec Corp., Columbus, OH, USA). The decision to use a downhill gait condition was made based on our previous clinical experience with patients with knee OA and PF dysfunction who reported frequent difficulty and pain while walking downhill, most likely due to increased knee flexion angles, vertical ground reaction forces and knee joint moments as compared to level gait (Kuster et al., 1995; Lay et al., 2006; McIntosh et al., 2006; Redfern, 1997). Additionally, a relatively slow gait velocity of 0.75 m/s was chosen for our experimental set up based on the result of our pilot testing demonstrating that most patients with knee OA had difficulty walking downhill at higher gait speeds. Our pilot testing also revealed that the magnitude of the ground reaction forces and the external moments placed on the knee joint were comparable (within 4%) between downhill walking on a 7% grade at 0.75 m/s compared to walking on level ground at the normal average speed of 1.3 m/s.
Participants were positioned on a treadmill within the biplane X-ray system so that the knee of interest would remain in the system's 3D imaging volume throughout the loading response phase of gait. Loading response was selected as a critical time period associated with high demands on the knee joint and reports of dynamic alignment change in patients with knee OA (Astephen and Deluzio, 2005; Schipplein and Andriacchi, 1991). For participants with knee OA, the knee in which they reported symptoms or the most painful knee in bilateral cases was designated as the test knee. For control participants, the knee from the dominant lower limb was designated as the test knee. For each subject, data were collected for 3 individual gait trials and the loading response phase was defined for each trial as the first 20% of the stance phase (Perry and Burnfield, 2010).
Quantification of Knee Joint Kinematics
All participants underwent computed tomography (CT) imaging of their knee. The CT field of view was approximately 28 × 28 cm, slice thickness ranged from 0.6 to 1.25 mm, and in-plane resolution was approximately 0.55 mm per pixel. The CT images of the tibia, femur, and patella were manually segmented and custom software was used to perform feature-based interpolation to create 3D bone models. A model-based tracking algorithm was then employed to determine 3D joint angles and translations by matching the radiographic images with projections through the 3D volumetric bone models as previously described (Anderst et al., 2009; Bey et al., 2008). Joint rotation and translation excursions were then determined by subtracting the minimum from the maximum joint angles or positions. This experimental approach has previously been shown to have excellent accuracy for quantifying TF and PF joint motion with measurement bias of better than 0.5-1.0° for rotations and 0.3-0.7mm for translations and measurement precision of better than 0.4-0.9° for rotations and 0.1-0.7mm for translations (Anderst et al., 2009; Bey et al., 2008).
Statistical Analysis
Analysis of variance (ANOVA) and chi-square tests were used to determine group differences in subject characteristics and joint motion excursions. Post-hoc tests consisting of paired t-tests with Tukey corrections were performed when a significant ANOVA test was identified. Group differences in TF and PF joint kinematics were also compared at 0%, 25%, 50%, 75%, and 100% of the loading response phase of downhill gait using a 3 × 5 (group by percentage of loading response) factorial ANOVA, with percentage of loading response as a repeated measure. The ANOVAs were performed with and without body mass index (BMI) as a covariate. Because BMI was not a significant covariate, only the results of the ANOVA without BMI as a covariate are presented to improve clarity. For all factorial ANOVA tests, significant main effects were reported only if there were no significant interactions. A p<0.05 was considered statistically significant.
RESULTS
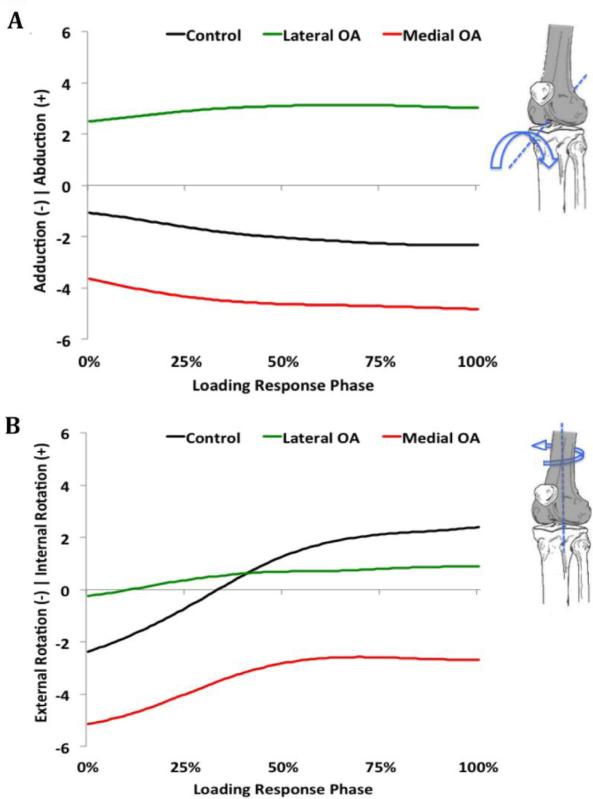
The ANOVA results for the frontal plane TF joint motion revealed a significant group by percentage of loading response interaction (F8,160=7.3; P<0.001), with the lateral OA group demonstrating greater and increasing degrees of knee abduction motion throughout the loading response phase of downhill gait compared to the control and the medial OA groups who walked with greater and increasing degrees of knee adduction motion (Figure 1A). A significant group by percentage of loading response interaction was also observed for the transverse plane TF joint motion (F8,160=4.2; P<0.01). Although all 3 groups moved towards TF internal rotation during the loading response phase of downhill gait, the medial OA group remained externally rotated throughout the loading response phase of downhill gait compared to the control and the lateral OA groups who moved from an externally rotated position into an internally rotated position (Figure 1B). Additionally, the medial OA (p=0.02) and the lateral OA (p=0.01) groups had significantly less internal rotation motion excursions compared to the control group (Table 2).
Figure 1.
Average frontal (A) and transverse (B) plane tibiofemoral joint rotations during the loading response phase of downhill gait in participants with medial or lateral tibiofemoral compartment osteoarthritis (OA) along with coexisting patellofemoral joint OA and participants in an OA-free control group. All rotations are reported in degrees.
Table 2.
Mean tibiofemoral and patellofemoral joint excursions during the loading response phase of downhill gait.
| OA-free Control (N = 22) | Medial Knee OA (N = 11) | Lateral Knee OA (N = 10) | P-value | |
|---|---|---|---|---|
| Tibiofemoral Joint Adduction/Abduction (°) | 1.6 (1.2) | 1.3 (0.6) | 1.5 (1.0) | 0.83 |
| Tibiofemoral Joint Internal Rotation (°) | 6.5 (3.5) | 3.6 (1.4)* | 3.4 (1.3)* | <0.01 |
| Patellofemoral Joint Lateral Tilt (°) | 6.8 (4.3) | 4.7 (1.9) | 3.5 (2.0)* | 0.04 |
| Patellofemoral Joint Medial-Lateral Translation (mm) | 3.4 (2.5) | 3.3 (1.5) | 2.7 (0.5) | 0.65 |
Significantly different than the control group
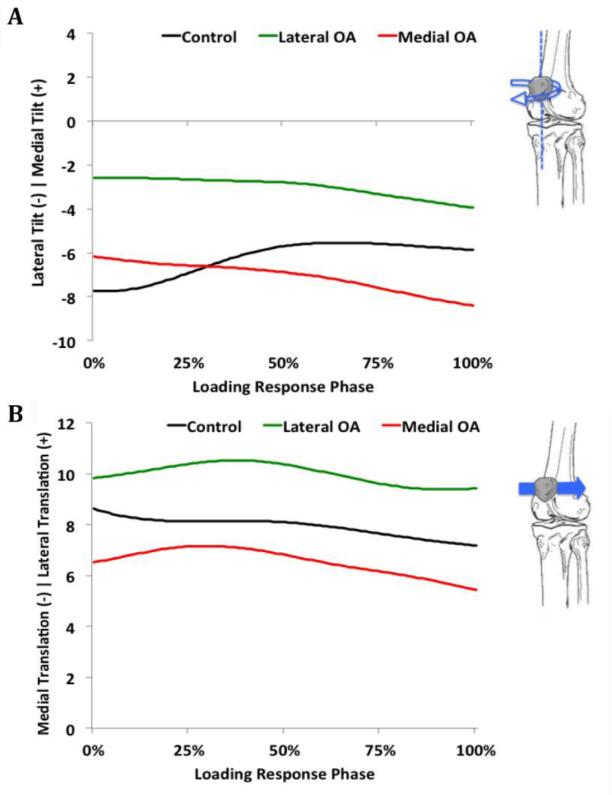
The ANOVA results for the transverse plane PF joint tilt revealed a significant group by percentage of loading response interaction (F8,160=2.8; P=0.006). Whereas the control group demonstrated a pattern of decreasing lateral patella tilt during the loading response phase of downhill gait, both knee OA groups moved into increasing degrees of lateral patella tilt (Figure 2A). The lateral OA group also had significantly less patella tilt excursion motion compared to the control group (p=0.04; Table 2). Additionally, although a significant interaction was not observed for the medial-lateral translation of the patella (F8,160=0.9; P=0.54), there was a significant main effect for the pattern of decreasing lateral patella translation during the loading response phase of downhill gait for all 3 groups (F4,160=7.4; P<0.001; Figure 2B).
Figure 2.
Average patella tilt (A) and translation (B) during the loading response phase of downhill gait in participants with medial or lateral tibiofemoral compartment osteoarthritis (OA) along with coexisting patellofemoral joint OA and participants in an OA-free control group. All rotations are reported in degrees, while translations are reported in millimeters.
DISCUSSION
Our initial hypothesis that patients with medial OA would exhibit greater TF adduction while patients with lateral OA would walk with greater TF abduction during the loading response phase of downhill gait compared to OA-free individuals was confirmed by the data. It has been previously reported that the peak knee adduction moment during gait on a level surface, which is a surrogate indicator of medial TF compartment loading, is 29-52% higher in patients with medial OA who exhibit greater knee adduction angles compared to OA-free individuals (Butler et al., 2011; Weidow et al., 2006). Conversely, patients with lateral compartment OA exhibit 41-63% lower knee adduction moments while walking with greater knee abduction angles compared to OA-free individuals, implying a shift in loadbearing from the medial to the lateral TF compartment (Agneskirchner et al., 2007; Butler et al., 2011; Weidow et al., 2006). The divergent increases in the patterns of frontal plane TF joint motion in our patients with medial and lateral knee OA could have important clinical significance as excessive static and/or dynamic changes in frontal plane TF alignment have been linked with increased risk of compartment-specific OA progression in the biomechanically stressed compartment (Chehab et al., 2014; Miyazaki et al., 2002; Sharma et al., 2010). Therefore, it stands to reason that effective offloading of the medial versus laterally stressed TF compartments will likely require different intervention strategies (e.g. lateral versus medially wedged shoe insoles or valgus versus varus bracing).
Both knee OA groups in our study also demonstrated reduced TF internal rotation motion excursions during the loading response phase of downhill gait compared to the control group. This finding is suggestive of alterations in the normal reverse screw-home mechanism of the knee joint that allows the knee to unlock and flex to provide shock absorption through eccentric activity of the quadriceps muscles during the loading response phase of gait. Reduced TF internal rotation excurson could also facilitate progression of knee OA due to repetitive loading of the same areas of joint contact, which can cause microtrauma to finite regions of the articular cartilage. Our finding of an externally rotated TF joint in the medial OA group compared to the lateral OA and the control groups is also consistent with previous reports (Weidow et al., 2006). The externally rotated position of the TF joint in patients with medial OA has been previously proposed as a compensatory strategy to decrease TF joint loading over the commonly damaged central and anterior regions of the medial TF compartment (Saari et al., 2005; Weidow et al., 2002). Interestingly, reduced TF internal rotation during gait has also been observed in patients after total knee arthroplasty, suggesting that the abnormal kinematics observed after surgery might arise from changes which occurred preoperatively (Saari et al., 2005; Uvehammer et al., 2000; Yue et al., 2011).
The finding of increased lateral patella tilt in our lateral OA group was consistent with our initial hypothesis which was based on the premise that increasing frontal plane TF abduction would lead to an increased Q-angle and lateral tilt of the patella. Conversely, the finding of increasing lateral patella tilt in the medial OA group who moved into increasing degrees of TF adduction during the loading response phase of downhill gait was surprising and contrary to our proposed hypothesis. This unexpected finding could be the consequence of greater externally rotated TF joint in the medial OA group which can shift the tibial tubercle laterally to increase the Q-angle and therefore cause the patella to tilt laterally (Wittstein et al., 2006). Regardless of the underlying mechanism, the finding of increasing lateral patella tilt in our medial and lateral OA groups is suggestive of greater lateral PF compartment compressive loading and increased probability of lateral PF joint damage (Stephen et al., 2013). This premise is supported by previous reports of the association between increased lateral patella tilt and greater risk of lateral PF compartment bone marrow lesions, osteophytosis, cartilage loss and joint space narrowing (Kalichman et al., 2007a; Kalichman et al., 2007b).
Both knee OA groups in our study also exhibited increasing medial PF joint translation during the loading response phase of downhill gait that was similar to that of the control group. This finding is consistent with previous biomechanical and imaging studies suggesting that the lateral position of patella at full knee extension leads to medial translation of the patella as it descends into the more medially positioned trochlear groove with initiation of knee flexion (Hefzy and Yang, 1993; Nha et al., 2008). Although anatomically required, Gross and colleagues (Gross et al., 2012) suggested that the medial shift of the patella during the initiatory phase of knee flexion may increase the probability of excessive loading and damage of the medial PF joint based on their observation of high prevalence of medial PF cartilage damage in patients with knee OA. This suggestion is supported by the previously reported association between increased medial patella translation and greater progression of medial PF joint space narrowing over 36 months in older adults (Hunter et al., 2007).
Involvement of the PF joint in patients with knee OA has been previously associated with increased symptoms and functional limitations (Englund and Lohmander, 2005; Farrokhi et al., 2013), altered gait biomechanics (Farrokhi et al., 2014) and decreased probability of clinical improvements after 12 weeks of supervised exercise therapy (Knoop et al., 2014). Therefore, finding effective treatment strategies to address PF joint dysfunction in patients with mixed knee OA has important clinical utility. Currently, most biomechanical treatments of PF OA, such as taping, bracing, or surgical realignment procedures, attempt to reduce malalignment by pulling the patella medially and away from the lateral trochlear facet (Feller et al., 2007; Mills and Hunter, 2014). The observation of combined lateral patella tilt and medial patella translation in our patients with PF OA suggests that although such strategies may be effective in mitigating the negative effects of increased lateral patella tilt by offloading the stressed lateral patella compartment, they will most likely also lead to an undesired increase in the medial patella translation and increased risk of medial PF joint damage (Hunter et al., 2007). Additionally intervention strategies aimed at improving PF joint malalignment through modification of frontal and transverse plane TF joint mechanics (e.g. gait retraining, wedged orthoses, etc.) should be used cautiously with their potential adverse influence on the coexisting arthritic TF joint in mind. Further research aimed at better understanding of TF and PF joint mechanics and their interactions in patients with mixed knee OA are needed before definitive clinical recommendations could be made.
The results of our study should be considered in light of a number of limitations. We acknowledge the potential limitations of the small sample size used in this investigation. The addition of more subjects would have improved the power of the study and may have identified additional differences between groups. Also, subjects in the medial OA group in our study had higher BMI than those in the Control group. Although significantly different, the mean BMI of our medial OA (29.6 kg/m2), lateral OA (26.0 kg/m2) and the control (25.1 kg/m2) groups fell within the same standard weight status category of overweight. Additionally, our statistical analysis revealed that BMI was not a significant covariate in the present study. Nevertheless, higher BMI has been previously shown to affect gait mechanics in obese older adults (Lai et al., 2008) and its effect on knee joint kinematics of patients with knee OA should be further evaluated in the future. Finally, given the cross-sectional nature of our study design, no causal relationships between altered TF or PF kinematics and disease status in either joint could be made. Future longitudinal, prospective studies are needed to investigate the relationship between altered joint kinematics and onset and progression of TF and/or PF OA.
Conclusions
Patients with medial or lateral TF compartment OA with coexisting PF OA have significantly different frontal and transverse plane TF joint kinematics during the loading response phase of downhill gait compared to an OA-free control group. However, the kinematics of the coexisting arthritic PF joint appears to be similar between patients with medial and lateral TF OA groups. The observed differences and similarities provide important insight regarding the function of the knee joint in patients with mixed TF and PF OA. Further research is needed to determine if these kinematic variations are relevant targets for interventions to reduce pain and disease progression in patients with mixed TF and PF joint disease.
ACKNOWLEDGMENTS
Funding for this study was provided by the Pittsburgh Claude D. Pepper Older Americans Independence Center (Grant P30 AG024827), the National Center for Research Resources, a component of the National Institutes of Health (NIH) and Roadmap for Medical Research (Grant 1 UL1 RR024153) and a National Center Medical Rehabilitation Research, National Institute of Child Health and Human Development / National Institute Neurological Disorders and Stroke, National Institutes of Health career development award (K12 HD055931).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT
No authors had any financial or personal relationships with other people or organizations that could have influenced this study.
References
- Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007;23:852–861. doi: 10.1016/j.arthro.2007.05.018. [DOI] [PubMed] [Google Scholar]
- Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis and Rheumatism. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- Anderst W, Zauel R, Bishop J, Demps E, Tashman S. Validation of three-dimensional model-based tibio-femoral tracking during running. Medical Engineering & Physics. 2009;31:10–16. doi: 10.1016/j.medengphy.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astephen JL, Deluzio KJ. Changes in frontal plane dynamics and the loading response phase of the gait cycle are characteristic of severe knee osteoarthritis application of a multidimensional analysis technique. Clinical Biomechanics (Bristol, Avon) 2005;20:209–217. doi: 10.1016/j.clinbiomech.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Bey MJ, Kline SK, Tashman S, Zauel R. Accuracy of biplane x-ray imaging combined with model-based tracking for measuring in-vivo patellofemoral joint motion. Journal of Orthopaedic Surgery and Research. 2008;3:38. doi: 10.1186/1749-799X-3-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler RJ, Barrios JA, Royer T, Davis IS. Frontal-plane gait mechanics in people with medial knee osteoarthritis are different from those in people with lateral knee osteoarthritis. Physical Therapy. 2011;91:1235–1243. doi: 10.2522/ptj.20100324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage. 2014 doi: 10.1016/j.joca.2014.08.009. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. The Journal of Rheumatology. 2006;33:2271–2279. [PubMed] [Google Scholar]
- Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis--it all depends on your point of view. Rheumatology. 2006;45:757–760. doi: 10.1093/rheumatology/kei270. [DOI] [PubMed] [Google Scholar]
- Englund M, Lohmander LS. Patellofemoral osteoarthritis coexistent with tibiofemoral osteoarthritis in a meniscectomy population. Annals of the Rheumatic Diseases. 2005;64:1721–1726. doi: 10.1136/ard.2005.035568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrokhi S, O'Connell M, Fitzgerald GK. Altered gait biomechanics and increased knee-specific impairments in patients with coexisting tibiofemoral and patellofemoral osteoarthritis. Gait and Posture. 2014 doi: 10.1016/j.gaitpost.2014.08.014. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrokhi S, Piva SR, Gil AB, Oddis CV, Brooks MM, Fitzgerald GK. Association of severity of coexisting patellofemoral disease with increased impairments and functional limitations in patients with knee osteoarthritis. Arthritis Care and Research. 2013;65:544–551. doi: 10.1002/acr.21866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM. Surgical biomechanics of the patellofemoral joint. Arthroscopy : the Journal of Arthroscopic and Related Surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007;23:542–553. doi: 10.1016/j.arthro.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Felson DT, Nevitt MC, Zhang Y, Aliabadi P, Baumer B, Gale D, Li W, Yu W, Xu L. High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheumatology. 2002;46:1217–1222. doi: 10.1002/art.10293. [DOI] [PubMed] [Google Scholar]
- Gross KD, Niu J, Stefanik JJ, Guermazi A, Roemer FW, Sharma L, Nevitt MC, Segal NA, Lewis CE, Felson DT. Breaking the Law of Valgus: the surprising and unexplained prevalence of medial patellofemoral cartilage damage. Annals of the Rheumatic Diseases. 2012;71:1827–1832. doi: 10.1136/annrheumdis-2011-200606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefzy MS, Yang H. A three-dimensional anatomical model of the human patellofemoral joint, for the determination of patello-femoral motions and contact characteristics. Journal of Biomedical Engineering. 1993;15:289–302. doi: 10.1016/0141-5425(93)90005-j. [DOI] [PubMed] [Google Scholar]
- Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. Journal of Bone and Joint Surgery-American volume. 1984;66:715–724. [PubMed] [Google Scholar]
- Hunter DJ, Zhang YQ, Niu JB, Felson DT, Kwoh K, Newman A, Kritchevsky S, Harris T, Carbone L, Nevitt M. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthritis Cartilage. 2007;15:1120–1127. doi: 10.1016/j.joca.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Felson DT, Hunter D. The association between patellar alignment and patellofemoral joint osteoarthritis features--an MRI study. Rheumatology. 2007a;46:1303–1308. doi: 10.1093/rheumatology/kem095. [DOI] [PubMed] [Google Scholar]
- Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Zhu Y, Felson DT, Hunter DJ. The association between patellar alignment on magnetic resonance imaging and radiographic manifestations of knee osteoarthritis. Arthritis Research and Therapy. 2007b;9:R26. doi: 10.1186/ar2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Annals of the Rheumatic Diseases. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoop J, Dekker J, van der Leeden M, van der Esch M, Klein JP, Hunter DJ, Roorda LD, Steultjens MP, Lems WF. Is the severity of knee osteoarthritis on magnetic resonance imaging associated with outcome of exercise therapy? Arthritis Care and Research. 2014;66:63–68. doi: 10.1002/acr.22128. [DOI] [PubMed] [Google Scholar]
- Kuster M, Sakurai S, Wood GA. Kinematic and kinetic comparison of downhill and level walking. Clinical Biomechanics (Bristol, Avon) 1995;10:79–84. doi: 10.1016/0268-0033(95)92043-l. [DOI] [PubMed] [Google Scholar]
- Lai PP, Leung AK, Li AN, Zhang M. Three-dimensional gait analysis of obese adults. Clinical Biomechanics. 2008;23(Suppl 1):S2–6. doi: 10.1016/j.clinbiomech.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Lay AN, Hass CJ, Gregor RJ. The effects of sloped surfaces on locomotion: a kinematic and kinetic analysis. Journal of Biomechanics. 2006;39:1621–1628. doi: 10.1016/j.jbiomech.2005.05.005. [DOI] [PubMed] [Google Scholar]
- Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clinical Orthopaedics and Related Research. 1994;302:69–74. [PubMed] [Google Scholar]
- Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Archives of Physical Medicine and Rehabilitation. 2014;95:986–995. e981. doi: 10.1016/j.apmr.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh AS, Beatty KT, Dwan LN, Vickers DR. Gait dynamics on an inclined walkway. Journal of Biomechanics. 2006;39:2491–2502. doi: 10.1016/j.jbiomech.2005.07.025. [DOI] [PubMed] [Google Scholar]
- Mills K, Hunter DJ. Patellofemoral joint osteoarthritis: an individualised pathomechanical approach to management. Best practice & research. Clinical Rheumatology. 2014;28:73–91. doi: 10.1016/j.berh.2014.01.006. [DOI] [PubMed] [Google Scholar]
- Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the Rheumatic Diseases. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y, Kumagai M, Mattessich SM, Elias JJ, Ramrattan N, Cosgarea AJ, Chao EY. Q-angle influences tibiofemoral and patellofemoral kinematics. Journal of Orthopaedic Research. 2001;19:834–840. doi: 10.1016/S0736-0266(01)00008-0. [DOI] [PubMed] [Google Scholar]
- Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, Dragomir A, Kalsbeek WD, Luta G, Jordan JM. Lifetime risk of symptomatic knee osteoarthritis. Arthritis and Rheumatism. 2008;59:1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nha KW, Papannagari R, Gill TJ, Van de Velde SK, Freiberg AA, Rubash HE, Li G. In vivo patellar tracking: clinical motions and patellofemoral indices. Journal of Orthopaedic Research. 2008;26:1067–1074. doi: 10.1002/jor.20554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry J, Burnfield JM. Gait analysis : normal and pathological function. 2nd ed. SLACK; Thorofare, NJ: 2010. [Google Scholar]
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. The Journal of Orthopaedic and Sports Physical Therapy. 2003;33:639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- Redfern MS. Biomechanics of descending ramps. Gait and Posture. 1997;6:119–125. [Google Scholar]
- Saari T, Carlsson L, Karlsson J, Karrholm J. Knee kinematics in medial arthrosis. Dynamic radiostereometry during active extension and weight-bearing. Journal of Biomechanics. 2005;38:285–292. doi: 10.1016/j.jbiomech.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. Journal of Orthopaedic Research. 1991;9:113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M. Varus and valgus alignment and incident and progressive knee osteoarthritis. Annals of the Rheumatic Diseases. 2010;69:1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanik JJ, Niu J, Gross KD, Roemer FW, Guermazi A, Felson DT. Using magnetic resonance imaging to determine the compartmental prevalence of knee joint structural damage. Osteoarthritis and Cartilage / OARS, Osteoarthritis Research Society. 2013;21:695–699. doi: 10.1016/j.joca.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephen JM, Kader D, Lumpaopong P, Deehan DJ, Amis AA. Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. Journal of Orthopaedic Research. 2013;31:1423–1429. doi: 10.1002/jor.22371. [DOI] [PubMed] [Google Scholar]
- Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis and Rheumatism. 2009;61:459–467. doi: 10.1002/art.24336. [DOI] [PubMed] [Google Scholar]
- Uvehammer J, Karrholm J, Brandsson S. In vivo kinematics of total knee arthroplasty. Concave versus posterior-stabilised tibial joint surface. The Journal of Bone and Joint Surgery. British volume. 2000;82:499–505. doi: 10.1302/0301-620x.82b4.10651. [DOI] [PubMed] [Google Scholar]
- Weidow J, Pak J, Karrholm J. Different patterns of cartilage wear in medial and lateral gonarthrosis. Acta Orthopaedica Scandinavica. 2002;73:326–329. doi: 10.1080/000164702320155347. [DOI] [PubMed] [Google Scholar]
- Weidow J, Tranberg R, Saari T, Karrholm J. Hip and knee joint rotations differ between patients with medial and lateral knee osteoarthritis: gait analysis of 30 patients and 15 controls. Journal of Orthopaedic Research. 2006;24:1890–1899. doi: 10.1002/jor.20194. [DOI] [PubMed] [Google Scholar]
- Wittstein JR, Bartlett EC, Easterbrook J, Byrd JC. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2006;22:643–649. doi: 10.1016/j.arthro.2006.03.005. [DOI] [PubMed] [Google Scholar]
- Yang NH, Canavan PK, Nayeb-Hashemi H. The effect of the frontal plane tibiofemoral angle and varus knee moment on the contact stress and strain at the knee cartilage. Journal of Applied Biomechanics. 2010;26:432–443. doi: 10.1123/jab.26.4.432. [DOI] [PubMed] [Google Scholar]
- Yue B, Varadarajan KM, Moynihan AL, Liu F, Rubash HE, Li G. Kinematics of medial osteoarthritic knees before and after posterior cruciate ligament retaining total knee arthroplasty. Journal of Orthopaedic Research. 2011;29:40–46. doi: 10.1002/jor.21203. [DOI] [PubMed] [Google Scholar]
- Zhao D, Banks SA, Mitchell KH, D'Lima DD, Colwell CW, Jr., Fregly BJ. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. Journal of Orthopaedic Research. 2007;25:789–797. doi: 10.1002/jor.20379. [DOI] [PubMed] [Google Scholar]