Abstract
Purpose
The purpose of the present study was to investigate ethnic differences in trauma-related mental health symptoms among adolescents, and test the mediating and moderating effects of polyvictimization (i.e., number of types of traumas/victimizations experienced by an individual) and household income, respectively.
Methods
Data were drawn from the first wave of the National Survey of Adolescents replication study (NSA-R), which took place in the U.S. in 2005 and utilized random digit dialing to administer a telephone survey to adolescents ages 12-17. Participants included in the current analyses were the 3,312 adolescents (50.2% female; Mean age = 14.67 years) from the original sample of 3,614 who identified as non-Hispanic White (n = 2,346, 70.8%), non-Hispanic Black (n = 557, 16.8%), or Hispanic (n = 409, 12.3%). Structural equation modeling was utilized to test hypothesized models.
Results
Non-Hispanic Black and Hispanic participants reported higher levels of polyvictimization and trauma-related mental health symptoms (symptoms of posttraumatic stress and depression) compared to non-Hispanic Whites, though the effect sizes were small (γ ≤ .07). Polyvictimization fully accounted for the differences in mental health symptoms between non-Hispanic Blacks and non-Hispanic Whites, and partially accounted for the differences between Hispanics and non-Hispanic Whites. The relation between polyvictimization and trauma-related mental health symptoms was higher for low-income youth than for high-income youth.
Conclusions
Disparities in trauma exposure largely accounted for racial/ethnic disparities in trauma-related mental health. Children from low-income family environments appear to be at greater risk of negative mental health outcomes following trauma exposure compared to adolescents from high-income families.
Keywords: health disparities, ethnic minority issues, PTSD, depression, trauma
A burgeoning body of evidence suggests Hispanics and non-Hispanic Blacks living in the United States (U.S.) experience higher rates of traumatic events compared to non-Hispanic Whites1 [1, 2]. Given these disparities in trauma exposure, and the often deleterious mental health effects of traumatic events, ethnic and racial minority group members would appear to be at greater risk for developing disorders frequently associated with trauma exposure, such as posttraumatic stress and depression. Yet, studies evaluating ethnic differences in trauma-related mental health have produced mixed results, and studies investigating these differences in child and adolescent populations have evidenced complex patterns of findings [3]. The present study adds to this literature in two ways. First, the present study investigates ethnic disparities in the two most common mental health problems following trauma exposure in adolescence, PTSD and depression, in the updated National Survey of Adolescents replication study (NSA-R). Second, this investigation evaluates polyvictimization, or the exposure to different types of trauma/victimization, as a mediator of ethnic disparities in trauma-related mental health. Further understanding of the links between ethnic and racial disparities in trauma exposure and trauma-related mental health problems would likely improve public health initiatives aimed at alleviating mental health disparities.
Racial and Ethnic Differences in Lifetime Trauma Exposure and Related Psychopathology
Non-Hispanic Black Americans and Hispanic Americans report experiencing multiple types of potentially traumatic events more than Whites [4-11]. The definition of the Diagnostic and Statistical Manual, Fourth Edition of the American Psychiatric Association [12] outlines two criteria for traumatic events: (1) an event in which a “person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others” and (2) the person's response involved intense fear, helplessness, or horror.” Under this definition, the potentially traumatic events reported more frequently by African Americans than Hispanic Americans include experiencing violence, child maltreatment, and crime victimization in general [4-10]. Similarly, Hispanic Americans report more incidents of child maltreatment, witnessing violence, and violence victimization than non-Hispanic Whites [5, 6, 8, 9, 11]. Moreover, non-Hispanic Black and Hispanic Americans report disparities in the quantity and severity of violence exposure, which is often categorized as one type of traumatic event [8, 9]. In the original NSA study, a nationally-representative survey of traumatic events and mental health symptoms among youth, racial/ethnic2 differences in violence exposure persisted even after accounting for racial/ethnic differences in income [6].
Despite racial/ethnic differences in exposure to multiple types of violence, approximately equal percentages of non-Hispanic White, non-Hispanic Black, and Hispanic adults report having experienced at least one traumatic event [11, 13]. Thus, binary indicators of trauma exposure likely do not adequately reflect racial and ethnic differences in trauma exposure [8, 9]. Composites that attempt to define trauma exposure as a continuous variable have found (using different definitions and methods for counting traumatic events) that such measures are associated with more severe symptoms of posttraumatic stress disorder (PTSD), higher rates of functional impairment, and higher rates of physical health problems [14-16]. As an individual's exposure to a specific type of trauma—specifically, violence victimization—increases, PTSD and depression symptom and disorder co-occurrence also increase among adults [15] and children [17]. Previous findings with the original NSA sample have replicated these results with adolescents [14]. Others have found that the total number of different types of potentially traumatic events (e.g., parental physical abuse, physical assault, sexual assault) also significantly predict symptom severity and disorder co-occurrence of PTSD and depression [18-26]. Moreover, the sum of different types of trauma, also called polyvictimization [22], appears to account for much—in many cases all—of the relation between individual trauma types and mental health outcomes, such as PTSD and depression [22, 24]. Polyvictimization also appears to predict PTSD and depression symptoms better than sums of trauma exposures within a single type of trauma (e.g., multiple experiences of physical abuse) [22]. National samples of victimization among youth also suggest that youth in the U.S. have experienced an average of two different types of traumatic events and approximately 18% of youth have experienced four or more different types of traumatic events [22]. Additionally, non-Hispanic Black youth experience higher levels of polyvictimization compared with White youth [26]. It is unclear if Hispanic youth also experience greater degrees of polyvictimization, though some studies seem to suggest that Hispanic youth may be overrepresented among youth who experience the highest degrees of polyvictimization [22].
Despite potential racial/ethnic differences in polyvictimization, research examining racial/ethnic differences in PTSD has produced complex findings. Some studies have found small, but statistically significant differences in trauma-related mental health with non-Hispanic Blacks experiencing more symptoms than non-Hispanic Whites (e.g., OR = 1.21; 95% CI = 1.05, 1.40) [11], whereas others have found no difference [1]. Further complicating results, when racial/ethnic differences are found, some evidence supports trauma exposure as a mediator [27], whereas other evidence does not [11]. Results with Hispanics are similarly mixed. Compared to non-Hispanic Whites, Hispanic adults report higher rates of PTSD following trauma exposure in some studies [28], but report no differences in others [1]. Similar to non-Hispanic Blacks, other evidence suggests that trauma exposure may not account for disparate rates of PTSD among Hispanic adults [29, 30]. Little research, however, has focused on polyvictimization as a potential mediator of racial/ethnic differences in PTSD or depression among youth.
Given many of the mixed results regarding racial and ethnic differences in trauma and mental health, additional factors beyond trauma exposure may require further exploration. As one example, traumatic events experienced during childhood and adolescence appear to predict negative mental health outcomes in adulthood more than trauma experienced later in life, and these effects are larger when multiple traumatic events are experienced during childhood [31, 32]. Relatedly, trauma-related mental health symptoms during adolescence may serve as an independent risk factor for future trauma exposure [33, 34]. As a result, understanding racial/ethnic disparities in trauma exposure and related mental health difficulties among adolescents may aid in understanding complex disparities in adulthood.
In addition to experiencing more traumatic events, compared to non-Hispanic Whites, racial and ethnic minority members face more resource-related difficulties that appear to worsen posttraumatic responding, such as: greater post-disaster loss [35], less access to trauma-related mental health services [36], and longer durations of symptoms if untreated [37]. As such, low-resource environments may impede recovery from traumatic experiences and as a result increase the likelihood of developing subsequent mental health difficulties. Thus, accounting for income-related differences in the relation between trauma exposure and mental health outcomes appears crucial to better understanding racial/ethnic disparities in trauma-related mental health.
Purpose and Hypotheses
The current study sought to extend previous results on racial/ethnic disparities with the NSA and NSA-R in two major ways. First, we examined polyvictimization as a potential mediator of racial/ethnic disparities. Some portions of the mediational role of trauma exposure had been examined previously in the original NSA, but have not been replicated within the NSA-R, nor did these analyses consider polyvictimization specifically. Studies with the original NSA data suggested Hispanic and non-Hispanic Black youth met criteria for PTSD [3] and a larger proportion reported exposure to potentially traumatic events compared with non-Hispanic White youth [6]. Additionally, greater exposure to violence positively predicted comorbid PTSD and major depression [14]. Yet, these studies investigated frequencies of trauma exposure within a specific type of trauma/victimization (e.g., violence victimization) and did not investigate polyvictimization. Additionally, these studies examined the relation between trauma exposure and diagnoses of PTSD and major depression. Thus, whether findings hold across the full continuum of trauma-related mental health symptoms (e.g., subsyndromal concerns) has not been explored. Further, studies with NSA and NSA-R data have yet to directly examine the mediational role of polyvictimization. Lastly, income had previously been examined as a control covariate with the original NSA data [6], but the moderating role of income has yet to be examined in either the original or replication samples. Given previous results, including results with the original NSA, two primary hypotheses were examined:
- H1: It was expected that polyvictimization would mediate racial/ethnic disparities in trauma related mental health, such that:
- non-Hispanic Black and Hispanic youth would report greater depression and PTSD symptoms than non-Hispanic White youth in the NSA-R sample,
- non-Hispanic Black and Hispanic youth would report greater polyvictimization than non-Hispanic White youth,
- polyvictimization would positively predict PTSD and depression symptoms, and
- polyvictimization would account for a significant portion of racial/ethnic differences in PTSD and depression symptoms as measured by the indirect relation between race/ethnicity and mental health symptoms.
H2: It was predicted that income would moderate the relationship between polyvictimization, and PTSD and depression symptoms, such that those with lower income would evidence a greater relation between polyvictimization and symptomology.
Method
Procedures
Data were drawn from the National Survey of Adolescents-Replication (NSA-R). The NSA-R was initiated in 2005 as an epidemiological study of youth ages 12 to 17 years using computer-assisted telephone interviewing technology. Data for the present study were taken from the first wave of the study, which was completed in 2005. A survey research firm, Shulman, Ronca, and Bucuvalas, Inc., conducted the procedures, which were approved by an institutional review board and consisted of household probability sample selection and computer-assisted phone interviews. Participants were sampled using random-digit-dialing. Sampling procedures were identical to those used in the original National Survey of Adolescents. Interviews were conducted in English using computer-assisted telephone interviewing technology. In total, 6,694 adolescents were contacted for the study. Of these, 3,080 were not included in the first wave for various reasons: 1,268 (18.9%) parents refused participation; 188 (2.8%) parents were consented, but the adolescent refused participation; 199 (1.8%) adolescents agreed to participate and initiated participation, but were unable to complete the interview; finally, 1,505 (22.5%) caregivers consented to the study, but the adolescent was unavailable. The remaining 3,614 adolescents and their parents agreed to participate and were included in the study (52.2% participation). After informed consent was obtained, a brief parent interview was first conducted. Then, adolescent assent to participate was obtained before the interview began. Interviews assessed household characteristics (e.g., family income, number of individuals in the home), traumatic event exposure, mental health symptoms, and demographics. Adolescent participants were compensated with $10 for their participation in the interview.
Participants
Analyses of the present study were conducted with the 3,312 adolescents who self-identified as of Hispanic (n = 409, 12.3%), non-Hispanic Black (n = 557, 16.8%), or non-Hispanic White (n = 2,346, 70.8%) during the NSA-R. Mean age was 14.67 (SD = 1.66) and approximately equal percentages of participants were female (n = 1,664, 50.2%) and male (n = 1,648, 49.8%). Additional demographic information can be found in Table 1.
Table 1. Participant Descriptive Information.
| Total Sample | Non-Hispanic Black | Hispanic | Non-Hispanic White | |
|---|---|---|---|---|
|
| ||||
| N or Mean (SD or %) | N or Mean (SD or %) | N or Mean (SD or %) | N or Mean (SD or %) | |
| Gender | ||||
|
| ||||
| Male | 1,648 (49.8%) | 268 (48.1%) | 200 (48.9%) | 1,180 (50.3%) |
| Female | 1,664 (50.2%) | 289 (51.9%) | 209 (51.1%) | 1,166 (49.7%) |
|
| ||||
| Income Category | ||||
| Poverty | 418 (12.6%) | 168 (30.2%) | 73 (17.8%) | 177 (7.5%) |
| Non-poverty | 2,894 (87.4%) | 345 (61.9%) | 308 (75.3%) | 2,008 (85.6%) |
|
| ||||
| Age | 14.67 (1.66) | 14.60 (1.65) | 14.62 (1.63) | 14.70 (1.67) |
|
| ||||
| Total of trauma types | 1.80 (1.76) | 2.07 (1.80) | 1.98 (1.82) | 1.71 (1.74) |
| At least one trauma type | 2,196 (66.3%) | 319 (75.2%) | 188 (70.4%) | 1,489 (63.5%) |
| Four or more trauma types | 565 (17.1%) | 118 (21.2%) | 85 (20.8%) | 364 (15.5%) |
|
| ||||
| Mental health symptom totals | ||||
| Depression total | 3.43 (5.82) | 4.30 (6.40) | 3.66 (6.00) | 3.22 (5.69) |
| Avoidance total | 0.60 (1.22) | 0.70 (1.30) | 0.70 (1.32) | 0.57 (1.17) |
| Reexperiencing total | 0.30 (0.72) | 0.32 (0.68) | 0.36 (0.80) | 0.28 (0.71) |
| Hyperarousal total | 0.59 (1.05) | 0.73 (1.09) | 0.60 (1.05) | 0.56 (1.03) |
| Combined symptoms | 4.92 (7.96) | 6.05 (8.64) | 5.32 (8.27) | 4.63 (7.74) |
| At least one symptom | ||||
| Depression | 1,376 (41.5%) | 248 (44.5%) | 196 (47.9%) | 932 (39.7%) |
| Avoidance | 949 (71.3%) | 180 (32.3%) | 129 (31.5%) | 640 (27.3%) |
| Reexperiencing | 634 (19.1%) | 122 (21.9%) | 95 (23.2%) | 417 (17.8) |
| Hyperarousal | 1,068 (32.2%) | 187 (33.6%) | 164 (40.1%) | 717 (30.6%) |
| Any symptom | 1,675 (53.6%) | 1,211 (51.6%) | 245 (59.9%) | 319 (57.3%) |
Measures
Polyvictimization
Traumatic events were assessed in the categories of physical assault, sexual assault, physical abuse, sexual abuse, non-assaultive events, and witnessed violence in the home, school, or community. Similar to prior research with poyvictimization, categories of traumatic events were further broken down [22], resulting in 13 distinct trauma types. To increase accuracy of responses, the interview included behaviorally specific terminology and introductory statements to orient adolescents to questions for each trauma type [3]. Exposure to each type of traumatic event was assessed using a number of yes/no items. Participants were coded as having experienced each category of traumatic events if they endorsed any item within that category during their lifetime. Then, similar to methodology in other studies examining polyvictimization [18-26], polyvictimization was calculated by summing the total number of traumatic experiences participants endorsed. The number of trauma types endorsed ranged from zero to nine. Most participants (66.3%) reported experiencing at least one type of traumatic event. Table 1 includes additional description information regarding polyvictimization. For additional detailed description of individual traumatic events within each category, see Cisler and colleagues [38].
PTSD and depression symptoms
PTSD and depression symptoms were assessed utilizing a structured interview of DSM-IV-TR disorder criteria. The interview has demonstrated substantial diagnostic and concurrent validity [39]. To further extend previous NSA findings and in order to capture wider variability in PTSD and depression outcomes compared to discrete (present/absent) diagnostic categories, continuous symptom counts were used in the present study. For the symptom counts used in the present study, participants indicated if they had experienced each symptom during the previous six months. Present symptoms were then totaled within each diagnostic category. PTSD symptoms were summed across three domains: (1) hyperarousal, (2) avoidance, and (3) re-experiencing symptoms. A single depression symptom sum was also calculated. Most participants (53.6%) reported at least one symptom. Additional descriptive information for PTSD and depression symptoms is available in Table 1.
Demographics
During the interview, multiple demographic variables were assessed. Adolescents reported their gender, age, and race/ethnicity. Income was assessed during the parent portion of the survey, with parents self-identifying in one of three household income categories: (1) Below $20,000, (2) between $20,000 and $50,000, (3) above $50,000. The first category approximately corresponds with the 2005 U.S. federal poverty level for a four-person household ($19,350) and 200% of the U.S. federal poverty level for a two-person household ($19,140) [40], which, respectively, represent the average (Mean = 4.17, Median = 4.00) and smallest household sizes of the adolescents included in the current study. During initial analyses, no differences were found between the second and third income groups across trauma exposure, mental health symptoms, age or gender (p-values > .05). Additionally, no significant differences were found between these two groups in the primary hypothesized relations (p-values < .05). As a result, these groups were combined and two dichotomous groups were utilized to conduct analyses. The first contained participants who reported less than $20,000, herein referred to as the poverty group. The second group contained participants who reported earnings greater than $20,000, herein referred to as the non-poverty group.
Analytic Approach and Data Preparation
Prior to data analyses, data were examined to ensure analytic assumptions were met. Data were significantly multivariate kurtotic (Mardia's coefficient = 145.47). Polyvictimization, and PTSD and depression symptom sums were individually kurtotic. These variables were logarithmically transformed to resolve violations of normality. Following transformations, data were no longer significantly multivariate or univariate kurtotic (Mardia's coefficient = 2.23). The transformed variables were used in all data analyses of research hypotheses. Untransformed values are presented in descriptive analyses. All other analytic assumptions were met. Data were estimated with expectation maximization, as Little's MCAR test suggested they were not systematically missing (p > .05).
All hypotheses were examined utilizing structural equation modeling, a covariance modeling technique that is often used to account for the error in measuring latent constructs (e.g., trauma-related mental health) and provides an assessment of overall fit of a specified model to given data (e.g., assessing the fit of a mediational model). In accordance with recommendations by Byrne [41, p. 164], prior to examining models testing hypotheses, measurement models of latent constructs were first constructed and hypothesized models were subsequently examined. In the best fitting measurement model, PTSD and depression symptoms loaded onto a single factor, herein referred to as trauma-related mental health. Descriptive information on combined symptom totals can be found in Table 1.
In order to test hypothesis 1a—that Hispanic and non-Hispanic Black youth would endorse greater trauma-related mental health symptoms than non-Hispanic White youth—Model 1 was constructed to examine the relation between race/ethnicity and trauma-related mental health symptoms. Two race/ethnicity variables were “dummy-coded” to represent non-Hispanic Black and Hispanic identification, and non-Hispanic White identification was used as the referent category. Given prior results suggesting significant age and gender differences in depression and PTSD symptoms [26, 42, 43], age and gender were used as control covariates.
Model 2 was created to test parts b, c, and d of hypothesis 1 by adding polyvictimization as a mediator to Model 1 (see Figure 2). Additionally, maximum likelihood bootstrapping was used to test the significance of indirect paths with 2,000 bootstrapped samples.
Figure 2.
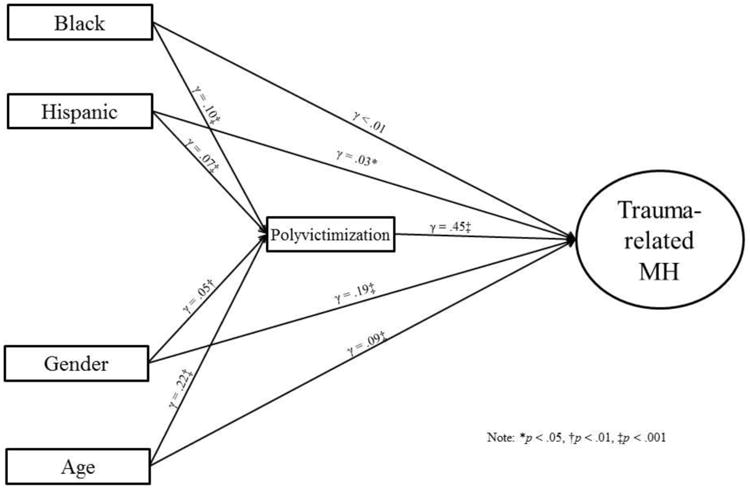
Structural Model of Polyvictimization Mediating Ethnic Differences in Mental Health Outcomes. Gamma weights, which in structural equation modeling are similar to regression coefficients, are presented.
In model 3, income was evaluated as a moderator by conducting chi-square difference tests of constrained and unconstrained multigroup structural model comparisons, in accordance with recommendations by Byrne [44]. Participants were assigned to one of two groups based on reported income (“poverty” or “non-poverty”). In the unconstrained model, all estimates were allowed to vary between the poverty and non-poverty groups. In the constrained model, the path between polyvictimization and trauma-related mental health symptoms was constrained to be equal across the poverty and non-poverty groups.
Results
Model 1: Examining Ethnic Differences in Trauma-Related Mental Health Symptoms
For the first model, most indicators suggested good model fit (χ2 = 186.35, df = 20, p < .001, CFI = .97, RMSEA = .05, SRMR = .03), and both race/ethnicity variables significantly predicted trauma-related mental health symptoms such that youth who identified as non-Hispanic Black (γ = .04, p = .018) and Hispanic (γ = .07, p < .001) reported greater trauma-related mental health symptoms compared to non-Hispanic White participants, but the effect size for both groups was small (i.e., γ < .10). The initial model is depicted in Figure 1.
Figure 1.
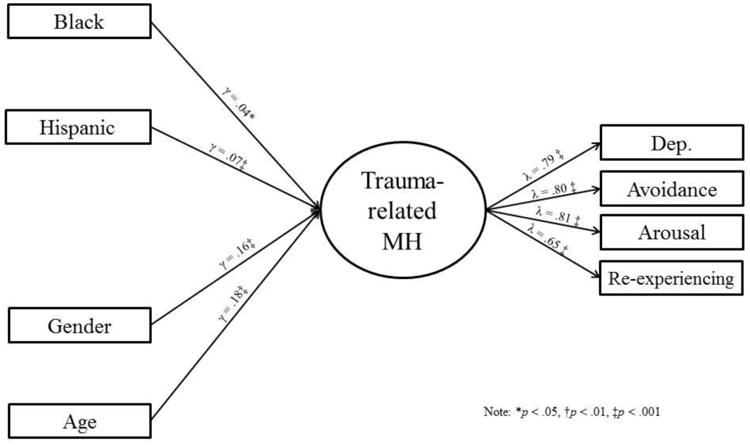
Initial Model Depicting Ethnic Differences in Trauma-related Mental Health. Gamma weights, which in structural equation modeling are similar to regression coefficients, are presented. Lambda weights, which estimate how much a manifest item (e.g., symptom counts) loads onto a latent factor (e.g., trauma-related mental health), are also presented.
Model 2: Examining Polyvictimization as a Mediator
In the second model, most indicators suggested good model fit (χ2 = 211.2365, df = 23, p < .001, CFI = .97, RMSEA = .05, SRMR = .03). Individuals who identified as non-Hispanic Black or Hispanic reported experiencing more traumatic events than non-Hispanic White participants (p-values < .05). Additionally, polyvictimization positively predicted trauma-related mental health symptoms (γ = .45, p = < .001). After controlling for polyvictimization, Hispanic youth continued to report significantly more trauma-related mental health symptoms compared to non-Hispanic White youth (γ = .03, p = .039); however, non-Hispanic Black youth did not (γ =< .01, p = .91). Lastly, bootstrapped standard errors were used in order to test the indirect relation between ethnicity and trauma-related mental health symptoms with polyvictimization as a mediator. The indirect relations of ethnicity and trauma-related mental health symptoms were positive and significant (p-values < .05). Significance tests of indirect effects are contained in Table 2.
Table 2. Polyvictimization Mediation Path Coefficients Predicting Trauma-Related Mental Health.
| Predictor variable | Standardized coefficient | Bootstrapped 95% CI | Bootstrapped p-value |
|---|---|---|---|
| Hispanic | |||
| Direct Effect | .05 | .02, .08 | .012 |
| Indirect Effect | .02 | .01, .03 | .003 |
| Total Effect | .07 | .03, .09 | .001 |
| Non-Hispanic Black | |||
| Direct Effect | < .01 | -.02, .04 | .631 |
| Indirect Effect | .04 | .02, .05 | < .001 |
| Total Effect | .04 | .01, .08 | < .001 |
| Age | |||
| Direct Effect | .11 | .08, .15 | .001 |
| Indirect Effect | .07 | .06, .09 | .001 |
| Total Effect | .18 | .15, .22 | .001 |
| Gender | |||
| Direct Effect | .19 | .15, .22 | < .001 |
| Indirect Effect | -.02 | -.04, -.01 | .002 |
| Total Effect | .16 | .13, .20 | < .001 |
Note: Effects were evaluated with bootstrapping in structural equation modeling. This technique allows for testing of the portion of an effect that is accounted for by a third (e.g., mediator) variable. This effect is called the indirect effect and is evaluated based on whether it is significantly different from zero according to p-values and 95% confidence intervals.
Model 3: Examining Income as Moderator and Polyvictimization as a Mediator
In the unconstrained model, polyvictimization significantly and positively predicted trauma-related mental health symptoms in both the poverty (γ = .47, p < .001) on non-poverty groups (γ = 38, p < .001). According to most indicators of model fit, the unconstrained model fit the data well (Model fit: χ2 = 252.16, df = 46, p < .001, CFI = .97, RMSEA = .04, SRMR = .06) and the chi-square difference test was significant (χ2 = 6.98, df = 1, p = .008), such that the unconstrained model fit significantly better than the constrained model. For further description of differences between the poverty and non-poverty groups, see Figure 3.
Figure 3.
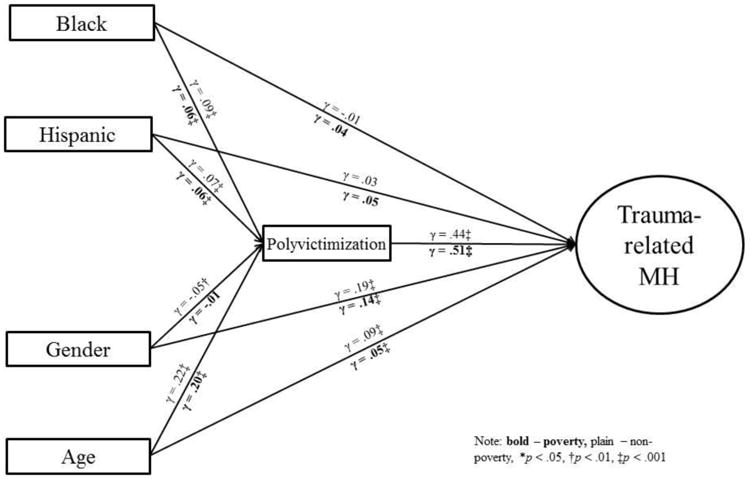
Multigroup model showing differences between poverty and non-poverty groups. Gamma weights, which in structural equation modeling are similar to regression coefficients, that are located above paths pertain to the non-poverty group and gamma weights below the path pertain to the poverty group.
Discussion
The current study sought to advance current knowledge of ethnic differences in depression and PTSD symptoms in multiple ways: by evaluating polyvictimization as a potential mediator of ethnic differences in depression and PTSD symptoms; evaluating the moderating role of income in trauma-related symptoms; and evaluating these relations in a nationally representative sample of non-Hispanic White, non-Hispanic Black, and Hispanic youth. First, similar to findings with adults [11] and similar to previous findings with the original NSA [3], non-Hispanic Black and Hispanic adolescents reported greater depression and PTSD symptoms than non-Hispanic White youth; however, even prior to controlling for trauma exposure and examining the moderating role of income, these differences were small. In the current study, less than a quarter of a standard deviation separated all three racial and ethnic groups across all mental health symptoms. The regression coefficients were similarly small (γ-values ≤ .07). Despite findings of statistical significance in the current study, with such small effect sizes, a large sample (i.e., more than 2,000 participants) would be necessary to detect differences among the three racial and ethnic groups examined. Small effect sizes may explain why previous studies found no differences between these three racial and ethnic groups [1] and largely fits with other studies reporting small, but statistically significant differences [11] similar to the current results.
Similar to previous studies suggesting that PTSD and depression often co-occur among adolescents [17, 45], depression and PTSD symptoms overlapped heavily in the current sample and as a result were examined together as a single latent factor. The large overlap found here coalesces with prior work suggesting that the majority of youth who have met criteria for PTSD in their lifetime have also met criteria for depression, and that lifetime co-morbidity may be as high as 75% when using the DSM-IV three factor model [45]. As such, PTSD and depression symptoms among youth may represent a broader construct of trauma-related mental health difficulties or at least trauma-related internalizing disorders—disorders with primary symptoms related to mood and emotion [46] Given that PTSD and depression are both internalizing disorders, the grouping of trauma-related mental health may not apply to other diagnostic categories. For example, externalizing symptoms may develop from different mechanisms than internalizing symptoms (e.g., different family environments may differentially predict internalizing and externalizing symptoms [47]). Future research would do well to examine internalizing and externalizing symptoms within the same model. Nevertheless, results of this study do seem to indicate that non-Hispanic Black and Hispanic youth experience slightly, but detectably higher rates of trauma-related internalizing symptoms when compared to non-Hispanic White youth.
Polyvictimization and Racial/Ethnic Differences in PTSD and Depression
Of the small differences found, polyvictimization appeared to significantly account for much of the racial and ethnic differences in mental health symptoms. Similar to previous findings examining individual types of traumatic events within the original NSA sample [6] and similar to previous findings from other studies examining polyvictimization [22, 26], Hispanic and non-Hispanic Black youth endorsed exposure to more traumatic events than non-Hispanic White youth. For non-Hispanic Black youth, differences in polyvictimization appeared to fully account for differences in mental health symptoms compared to non-Hispanic White youth (γ < .01 after controlling for polyvictimization). The indirect effect—the portion of the difference between African and non-Hispanic Whites that polyvictimization accounted for—was also significant and comprised nearly all of the total effect. For Hispanic youth, polyvictimization did appear to account for some of the difference in depression and PTSD symptoms when compared to non-Hispanic White youth, but not all of the difference. The indirect effect was significant, and the difference between Hispanic and non-Hispanic White youth was smaller after controlling for polyvictimization. Trauma-related mental health symptoms, however, remained slightly higher among Hispanic youth than among non-Hispanic White youth. Polyvictimization may not sufficiently explain the higher rate of depression and PTSD symptoms among Hispanic youth compared to non-Hispanic White youth. Given that more than a third (35.5%) of Hispanics in the U.S. are also immigrants [48] and immigration to the U.S. for many Hispanics is often accompanied by multiple stressful or traumatic events [49], immigration-related factors may have contributed to the differences found. Despite the extensive and behaviorally-specific nature of the trauma assessment conducted, the current study may not have assessed traumatic events more likely to occur during immigration. Although not assessed in the current study, future research should examine potential immigration-related differences in trauma exposure and related mental health.
While polyvictimization appeared to account for a significant portion of ethnic and racial differences in mental health, racial and ethnic differences in polyvictimization were small. Similar to differences in symptomology, less than a quarter of a standard deviation separated all three racial and ethnic groups. Using raw differences, non-Hispanic Black and Hispanic youth reported approximately half a traumatic event more per person than non-Hispanic White youth. The relation between polyvictimization and mental health symptoms, however, was large; polyvictimization accounted for more than 20% of the variance in depression and PTSD. The current results, combined with similar previous findings [18-26], suggest that the relation between polyvictimization and mental health may be strong enough that even small differences in trauma exposure result in detectably higher risk of depression and PTSD.
Although polyvictimization overlaps significantly with PTSD and depression symptoms, it may not fully assess trauma exposure. Nevertheless, polyvictimization appears to account for a significant portion of trauma-related mental health outcomes. In previous literature, experiencing multiple different traumatic events (e.g., sexual and physical assault) conferred significantly greater risk of mental health difficulties than experiencing a single traumatic event (e.g., sexual assault only) [22]. When measured along a continuum, as in the current study and others [18-26], cumulative may provide even greater predictive ability for risk of PTSD and depression.
The Moderating Role of Income
Since poverty increases adolescents' risk of mental health difficulties, decreases the likelihood of seeking mental health services, and disparately impacts Hispanic and non-Hispanic Black youth [50-52], income was examined as a moderator for the relation between polyvictimization and trauma-related mental health symptoms. Among those with low household incomes, polyvictimization predicted mental health symptoms even more strongly. The relation among youth with medium-to-high household income remained large and roughly equivalent to the effect size seen with the overall sample. Said differently, polyvictimization strongly predicts negative mental health outcomes regardless of available resources; in low-resource environments, however, polyvictimization predicts depression and PTSD even more strongly. Bornstein & Bradley [53] review the relationship between social support and stress and suggest low-resource environments place additional strain on caregivers and other sources of social support. As a result, when traumatic events do happen, youth in these environments may receive less or less quality social support, a known protective factor following traumatic events [54-59]. Families with lower resources also have less access to mental health services, receive lower quality mental health services, and on average perceive mental health services as less helpful compared to those with higher income—see, for example, the review by Santiago, Kaltman, & Miranda on the relationship between poverty and service utilization [52].
Limitations and Alternate Explanations
Findings of the current study must be weighed in the context of its limitations. First, the current study explored only cross-sectional data. Even though the sample is large and nationally representative of non-Hispanic White, non-Hispanic Black, and Hispanic youth, polyvictimization could not be fully evaluated as a mediator of ethnic differences in PTSD and depression symptoms through the use of cross-sectional data. As an alternative explanation, polyvictimization and mental health symptoms among youth may be common outcomes resulting from high stress environments in which racial and ethnic minority youth are more likely to reside. Additionally, non-Hispanic Black and Hispanic youth are more likely to experience discrimination [60] and their groups are more likely to have faced historical trauma than non-Hispanic White youth [61]. Both discrimination and historical trauma have previously been linked to PTSD and depression symptoms [61, 62], and may explain at least some of the results found in the current study as historical trauma, and parent and child discrimination may make youth more susceptible to additional exposure to traumatic events. Finally, those who experience PTSD symptoms may also be more likely to experience subsequent traumatic events [63]. In order to better evaluate these relations, future studies would benefit from examining longitudinal data and more accurately assessing the timing of traumatic events, the ecological context of the adolescent, and the development of mental health symptoms.
Results with the current sample enhance current knowledge of the relation between ethnic disparities, polyvictimization and mental health among youth in the U.S. Yet, results should be interpreted within this context and may not generalize to other developmental stages (e.g., adulthood). Additionally, the study examined only internalizing symptoms. As stated previously, these findings likely cannot be extended to other symptom types (e.g., externalizing). Although trauma exposure may greatly inform the risk of externalizing symptoms in youth, they likely develop differently and result from different factors [47, 59].
Assessment methods also temper findings from the current study. First, self-reported income may not fully capture a family's access to resources. Social capital and neighborhood poverty, which may influence various forms of social capital and moderate the relation between social capital and internalizing mental health symptoms [64], should be considered in future studies. Additionally, polyvictimization was assessed by summing each type of traumatic experience an adolescent reported. Although this is a common method for assessing polyvictimization [18-26] and provided a singular measure of trauma exposure that more readily allows for mediational analyses, additional measurement methods and more complex modeling procedures (e.g., including multiple measures of trauma exposure as mediators of racial/ethnic differences) may provide more nuance. Similarly, symptom count variables may limit the assessment of PTSD and depression. While symptom count variables account for the breadth of symptoms experienced, they do not assess the severity of each symptom. Finally, little work has examined the cross-cultural or intergroup validity and measurement equivalence of many of the instruments used. While the mental health assessment was based on DSM-IV criteria and trauma assessments included in the current study were extensive and behaviorally-specific, future studies may benefit from examining ethnic invariance across trauma and mental health assessment methods used in the present study.
Conclusion
Similar to previous studies with the NSA samples, the current study of the NSA-R sample provided evidence for slightly, but detectably higher levels of depression and PTSD symptoms among non-Hispanic Black and Hispanic youth compared to non-Hispanic White youth. Extending beyond previous studies with either NSA sample, trauma exposure largely accounted for the small differences that were found. For non-Hispanic Black youth, polyvictimization fully accounted for this difference. Among Hispanic youth, polyvictimization accounted for a significant portion of the elevated depression and PTSD symptoms, but not all. Although racial/ethnic differences in trauma exposure were also small, polyvictimization predicted depression and PTSD symptoms strongly enough that even small differences in trauma exposure appeared to account for differences in symptom outcomes. Further, results from the current study suggest polyvictimization may relate even more strongly to PTSD and depression symptoms among low-income families.
Acknowledgments
This manuscript was supported in part by grants R01DA025616-04S1 from the National Institute on Drug Abuse (NIDA), NIH, and T32MH18869 from the National Institute of Mental Health (NIMH), NIH. Views expressed in this article do not necessarily reflect those of the funding agencies acknowledged.
Footnotes
We use the terms non-Hispanic Black, non-Hispanic White, and Hispanic in order to be consistent with labelling used by the NSA, NSA-R and the U.S. Census Bureau. Although definitions of race and ethnicity vary, the U.S. Census refers to White and Black/African American as racial categories, and refers to Hispanic as an ethnicity. According to the U.S. Census Bureau, the term Hispanic refers to anyone “of Cuban, Mexican, Puerto Rican, South or Central American, or other Spanish cultural or origin regardless of race”, the term “White refers to a person having origins in any of the original peoples of Europe, the Middle East, or North Africa”, and the term Black “refers to a person having origins in any of the Black racial groups of Africa.” [65] As such, while we understand that various terms exist to describe different racial, ethnic, and cultural groups, in the current manuscript, non-Hispanic Black refers to someone who is Black and not of Hispanic origin, non-Hispanic White similarly refers to someone who is White and not of Hispanic origin, and Hispanic refers to someone of Hispanic origin and who may be of any race.
When discussing differences between non-Hispanic Black, non-Hispanic White, and Hispanic groups, we use the term racial/ethnic differences in order to reflect that the descriptors of each group refer to race and ethnicity per the U.S. Census Bureau [65].
References
- 1.Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. J Urban Health. 2004;81(4):530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am J Commun Psychol. 2007;40(3-4):313–332. doi: 10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- 3.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consul Clin Psych. 2003;71:692–700. doi: 10.1037/0022-006X.71.4.692. [DOI] [PubMed] [Google Scholar]
- 4.Acierno R, Resnick H, Kilpatrick DG, Saunders B, Best CL. Risk factors for rape, physical assault, and posttraumatic stress disorder in women: Examination of differential multivariate relationships. J Anxiety Disord. 1999;13:541–563. doi: 10.1016/S0887-6185(99)00030-4. [DOI] [PubMed] [Google Scholar]
- 5.Buka SL, Stichick TL, Birdthistle I, Earls FJ. Youth exposure to violence: prevalence, risks, and consequences. American Journal of Orthopsychiatry. 2001;71:298–310. doi: 10.1037/0002-9432.71.3.298. [DOI] [PubMed] [Google Scholar]
- 6.Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, Resnick HS. Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. J Community Psychol. 2000;28:625–641. doi: 10.1002/1520-6629(200011)28:6<625∷AID-JCOP6>3.0.CO;2-R. [DOI] [Google Scholar]
- 7.Frueh BC, Gold PB, de Arellano MA, Brady KL. A racial comparison of combat veterans evaluated for PTSD. J Pers Assess. 1997;68(3):692–702. doi: 10.1207/s15327752jpa6803_14. [DOI] [PubMed] [Google Scholar]
- 8.Schwab-Stone ME, Ayers TS, Kasprow W, Voyce C, Barone C, Shriver T, Weissberg RP. No safe haven: A study of violence exposure in an urban community. J Am Acad Child Psy. 1995;34(10):1343–1352. doi: 10.1097/00004583-199510000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Schwab-Stone M, Chen C, Greenberger E, Silver D, Lichtman J, Voyce C. No safe haven II: The effects of violence exposure on urban youth. J Am Acad Child Psy. 1999;38(4):359–367. doi: 10.1097/00004583-199510000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affair. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 11.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41(01):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, Text Revision (DSM-IV-TR) American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 13.Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM– IV–TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3:148–156. doi: 10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Macdonald A, Danielson CK, Resnick HS, Saunders BE, Kilpatrick DG. PTSD and comorbid disorders in a representative sample of adolescents: The risk associated with multiple exposures to potentially traumatic events. Child Abuse Neglect. 2010;34:773–783. doi: 10.1016/j.chiabu.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, et al. Koenen KC. Cumulative traumas and risk thresholds: 12-month PTSD in the world mental health (WMH) surveys. Depress Anxiety. 2014;31(2):130–142. doi: 10.1002/da.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hendrickson CM, Neylan TC, Na B, Regan M, Zhang Q, Cohen BE. Lifetime trauma exposure and prospective cardiovascular events and all-cause mortality: Findings from the Heart and Soul Study. Psychosom Med. 2013;75(9):849–855. doi: 10.1097/PSY.0b013e3182a88846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hodges M, Godbout N, Briere J, Lanktree C, Gilbert A, Kletzka NT. Cumulative trauma and symptom complexity in children: A path analysis. Child Abuse Neglect. 2013;37(11):891–898. doi: 10.1016/j.chiabu.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Finkelhor D, Hamby SL, Ormrod R, Turner H. The Juvenile Victimization Questionnaire: Reliability, validity, and national norms. Child Abuse Neglect. 2005;29:383–412. doi: 10.1016/j.chiabu.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. Am J Prev Med. 2010;38(3):323–330. doi: 10.1016/j.amepre.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Finkelhor D, Ormrod R, Turner H, Holt M. Pathways to poly-victimization. Child Maltreatment. 2009;14(4):316–29. doi: 10.1177/1077559509347012. [DOI] [PubMed] [Google Scholar]
- 21.Finkelhor D, Turner H, Hamby S, Ormrod R. Polyvictimization: Children's exposure to multiple types of violence, crime, and abuse. Juvenile Justice Bulletin – NCJ 235504 2011 [Google Scholar]
- 22.Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: A neglected component in child victimization. Child Abuse Neglect. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Finkelhor D, Ormrod RK, Turner HA. Lifetime assessment of poly-victimization in a national sample of children and youth. Child Abuse Neglect. 2009;33:403–11. doi: 10.1016/j.chiabu.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 24.Finkelhor D, Ormrod RK, Turner HA. Polyvictimization and trauma in a national longitudinal cohort. Dev Psychopathol. 2007;19(1):149–66. doi: 10.1017/S0954579407070083. [DOI] [PubMed] [Google Scholar]
- 25.Huang M, Schwandt ML, Ramchandani VA, George DT, Heilig M. Impact of multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic inpatients. Alcohol Clin Exp Res. 2012;36(6):1099–107. doi: 10.1111/j.1530-0277.2011.01695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finkelhor D, Shattuck A, Turner HA, Ormrod R, Hamby SL. Polyvictimization in developmental context. Journal of Child and Adolescent Trauma. 2011;4(4):291–300. doi: 10.1080/19361521.2011.610432. [DOI] [Google Scholar]
- 27.Green BL, Grace MC, Lindy JD, Leonard AC. Race differences in response to combat stress. J Trauma Stress. 1990;3:379–393. doi: 10.1002/jts.2490030307. [DOI] [Google Scholar]
- 28.Marshall GN, Schell TL, Miles JN. Ethnic differences in posttraumatic distress: Hispanics' symptoms differ in kind and degree. J Consult Clin Psych. 2009;77(6):1169–1178. doi: 10.1037/a0017721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galea S, Ahern J, Tracy M, Hubbard A, Cerda M, Goldmann E, Vlahov D. Longitudinal determinants of posttraumatic stress in a population-based cohort study. Epidemiology. 2008;19:47–54. doi: 10.1097/EDE.0b013e31815c1dbf. [DOI] [PubMed] [Google Scholar]
- 30.Pole N, Gone JP, Kulkarni M. Posttraumatic stress disorder among ethnoracial minorities in the United States. Clinical Psychology: Science and Practice. 2008;15(1):35–61. doi: 10.1111/j.1468-2850.2008.00109.x. [DOI] [Google Scholar]
- 31.Ogle CM, Rubin DC, Siegler IC. The impact of the developmental timing of trauma exposure on PTSD symptoms and psychosocial functioning among older adults. Dev Psychol. 2013;49(11):2191–2200. doi: 10.1037/a0031985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cloitre M, Stolbach BC, Herman JL, Kolk BVD, Pynoos R, Wang J, Petkova E. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. J Trauma Stress. 2009;22(5):399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- 33.Elwood LS, Smith DW, Resnick HS, Gudmundsdottir B, Amstadter AB, Hanson RF, et al. Kilpatrick DG. Predictors of rape: Findings from the National Survey of Adolescents. J Trauma Stress. 2011;24(2):166–173. doi: 10.1002/jts.20624. [DOI] [PubMed] [Google Scholar]
- 34.Amstadter AB, Elwood LS, Begle AM, Gudmundsdottir B, Smith DW, Resnick HS, et al. Kilpatrick DG. Predictors of physical assault victimization: Findings from the National Survey of Adolescents. Addict Behav. 2011;36(8):814–820. doi: 10.1016/j.addbeh.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davidson TM, Price M, McCauley JL, Ruggiero KJ. Disaster impact across cultural groups: Comparison of Whites, African Americans, and Latinos. A J Commun Psychol. 2013;52:97–105. doi: 10.1007/s10464-013-9579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Swendsen J. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J Am Acad Child Psy. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown JS, Meadows SO, Elder GH., Jr Race-ethnic inequality and psychological distress: depressive symptoms from adolescence to young adulthood. Dev Psychol. 2007;43(6):1295–1311. doi: 10.1037/0012-1649.43.6.1295. [DOI] [PubMed] [Google Scholar]
- 38.Cisler JM, Begle AM, Amstadter AB, Resnick HS, Danielson CK, Saunders BE, Kilpatrick DG. Exposure to interpersonal violence and risk for PTSD, depression, delinquency, and binge drinking among adolescents: Data from the NSA-R. J Trauma Stress. 2012;25(1):33–40. doi: 10.1002/jts.21672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick PA, Roth S, van der Kolk B. The posttraumatic stress disorder field trial: Evaluation of the PTSD construct: Criteria A through E. In: Widiger T, Frances A, Pincus H, Ross R, First M, Davis W, Kline M, editors. DSM-IV sourcebook. American Psychiatric Press; 1998. pp. 803–844. [Google Scholar]
- 40.US Department of Health and Human Services. Annual update of the HHS poverty guidelines. Fed Regist. 2005;74:8373–5. [Google Scholar]
- 41.Byrne BM. Structural Equation Modeling Using AMOS. Basic concepts, applications, and programming 2010 [Google Scholar]
- 42.Poulin C, Hand D, Boudreau B, Santor D. Gender differences in the association between substance use and elevated depressive symptoms in a general adolescent population. Addiction. 2005;100(4):525–535. doi: 10.1111/j.1360-0443.2005.01033.x. [DOI] [PubMed] [Google Scholar]
- 43.Springer C, Padgett DK. Gender differences in young adolescents' exposure to violence and rates of PTSD symptomatology. American Journal of Orthopsychiatry. 2000;70(3):370. doi: 10.1037/h0087637. [DOI] [PubMed] [Google Scholar]
- 44.Byrne BM. Testing for multigroup equivalence of a measuring instrument: A walk through the process. Psicothema. 2008;20(4):872–882. [PubMed] [Google Scholar]
- 45.Ford JD, Elhai JD, Ruggiero KJ, Frueh C. Refining posttraumatic stress disorder diagnosis: Evaluation of symptom criteria with the national survey of adolescents. J Clin Psychiatry. 2009;70(5):748–55. doi: 10.4088/JCP.08m04692. [DOI] [PubMed] [Google Scholar]
- 46.Kovacs M, Devlin B. Internalizing disorders in childhood. J Child Psychol Psyc. 1998;39(1):47–63. [PubMed] [Google Scholar]
- 47.Leve LD, Kim HK, Pears KC. Childhood temperament and family environment as predictors of internalizing and externalizing trajectories from ages 5 to 17. J Abnorm Child Psych. 2005;33(5):505–20. doi: 10.1007/s10802-005-6734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Krogstad JM, Lopez MH. Hispanic nativity shift. Pew Research Center; 2014. http://www.pewhispanic.org/2014/04/29/hispanic-nativity-shift/#fn-20436-1. [Google Scholar]
- 49.Pumariega AJ, Rothe E, Pumariega JB. Mental health of immigrants and refugees. Community Ment Hlt J. 2005;41(5):581–97. doi: 10.1007/s10597-005-6363-1. [DOI] [PubMed] [Google Scholar]
- 50.Chow JCC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. 2003;93(5):792–797. doi: 10.2105/AJPH.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nikulina V, Widom CS, Czaja S. The role of childhood neglect and childhood poverty in predicting mental health, academic achievement and crime in adulthood. Am J Commun Psychol. 2011;48(3-4):309–321. doi: 10.1007/s10464-010-9385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Santiago CD, Kaltman S, Miranda J. Poverty and Mental Health: How Do Low-Income Adults and Children Fare in Psychotherapy? J Clin Psychol. 2013;69(2):115–126. doi: 10.1002/jclp.21951. [DOI] [PubMed] [Google Scholar]
- 53.Bornstein MH, Bradley RH, editors. Socioeconomic status, parenting, and child development. Routledge; 2014. [Google Scholar]
- 54.Bryant-Davis T, Ullman SE, Tsong Y, Gobin R. Surviving the Storm The Role of Social Support and Religious Coping in Sexual Assault Recovery of African American Women. Violence Against Wom. 2011;17(12):1601–1618. doi: 10.1177/1077801211436138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gabert-Quillen CA, Irish LA, Sledjeski E, Fallon W, Spoonster E, Delahanty DL. The impact of social support on the relationship between trauma history and posttraumatic stress disorder symptoms in motor vehicle accident victims. Int J Stress Manage. 2012;19(1):69–79. doi: 10.1037/a0026488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaniasty K. Predicting social psychological well-being following trauma: The role of postdisaster social support. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(1):22–33. doi: 10.1037/a0021412. [DOI] [Google Scholar]
- 57.Robinaugh DJ, Marques L, Traeger LN, Marks EH, Sung SC, Gayle Beck J, et al. Simon NM. Understanding the relationship of perceived social support to post-trauma cognitions and posttraumatic stress disorder. J Anxiety Disord. 2011;25(8):1072–1078. doi: 10.1016/j.janxdis.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tsai J, Harpaz-Rotem I, Pietrzak RH, Southwick SM. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry. 2012;75(2):135–149. doi: 10.1521/psyc.2012.75.2.135. [DOI] [PubMed] [Google Scholar]
- 59.Galambos NL, Barker ET, Almeida DM. Parents do matter: Trajectories of change in externalizing and internalizing problems in early adolescence. Child Dev. 2003;74(2):578–594. doi: 10.1111/1467-8624.7402017. [DOI] [PubMed] [Google Scholar]
- 60.Rosenbloom SR, Way N. Experiences of discrimination among African American, Asian American, and Latino adolescents in an urban high school. Youth Soc. 2004;35(4):420–51. [Google Scholar]
- 61.Williams DR, Neighbors HW, Jackson JS. Racial/Ethnic Discrimination and Health: Findings From Community Studies. Am J Public Health. 2003;93(2):200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Weems CF, Watts SE, Marsee MA, Taylor LK, Costa NM, Cannon MF, Carrion VG, Pina AA. The psychosocial impact of Hurricane Katrina: Contextual differences in psychological symptoms, social support, and discrimination. Behav Res Ther. 2007;45(10):2295–306. doi: 10.1016/j.brat.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 63.Orcutt HK, Erickson DJ, Wolfe J. A prospective analysis of trauma exposure: The mediating role of PTSD symptomatology. J Trauma Stress. 2002;15(3):259–66. doi: 10.1023/A:1015215630493. [DOI] [PubMed] [Google Scholar]
- 64.Caughy MO, O'Campo PJ, Muntaner C. When being alone might be better: neighborhood poverty, social capital, and child mental health. Soc Sci Med. 2003;57(2):227–37. doi: 10.1016/S0277-9536(02)00342-8. [DOI] [PubMed] [Google Scholar]
- 65.U.S. Census Bureau. Overview of race and Hispanic origin: 2010. 2010 Census Briefs. 2010 C2010BR-02. [Google Scholar]


