Abstract
The purpose of this study was to assess the outcome of humeral shaft fractures treated with Unreamed Humeral Nailing (UHN) system. Fixation of the humeral shaft fractures in this study was performed by minimal incision UHN system, without using its distal locking properties. Forty one patients were treated this way. Functional status of shoulder and elbow were evaluated using Society of the American Shoulder and Elbow Surgery (SASES) scoring system. During follow up period, no superficial or deep infections were observed. Mean union time was 13 weeks. Shoulder and elbow functions using SASES scale were excellent or good in 93 % of the patients. Complications included delayed union in 3(7.3 %), nonunion in 2(4.8 %) and radial nerve palsy in 1(2.4 %). Antegrade unreamed humeral Nailing is an acceptable, safe and reliable treatment for humeral shaft fractures.
Keywords: Humeral shaft, Fractures, Treatment, Antegrade, Humeral nailing, Unreamed
Introduction
Humeral shaft fractures are one of the most common orthopedic problems, accounting for approximately 3 % of all fractures [1]. Treatment approaches for this type of injuries continue to advance in both operative and non-operative methods. It is generally accepted that most of the humeral shaft fractures are managed best non-operatively, while some indications of primary or secondary operative approaches include polytrauma with substantial chest and/or head injury, an ipsilateral fracture of both bones of the forearm (floating elbow), extensive local associated injury involving the joint, brachial plexus, muscle, or tendon, inadequate reduction of the humeral shaft fracture by closed means, and pathological humeral shaft fracture [2, 3].
Despite the good results of union in non-operative management, there are still some issues such as long-term treatment and patient intolerance, particularly among the young and active patients who always make researchers and surgeons discuss operative management. The encouraging results that have been reported with recent advances in internal fixation techniques and instrumentations have led to an expansion of surgical indications for such fractures [4]. Fixation by means of plates has been considered as the standard method. Problems associated with this method include wound complications such as infection, high probability of delayed fusion (especially when the principles of plate fixation were not performed accurately), non-union, and fixation failure [5, 6]. Intra-medullary nailing is another appropriate surgical technique that could be performed through both antegrade and retrograde approaches. There are various results in the literature about unreamed humeral nailing (UHN) and some trials reported various rates of non-unions [7, 8]. We believe that because of the shoulder joint’s wide range of motion UHN with the antegrade approach without distal locking, except of little increasing the risk of non-union, will not cause any significant complication, but it may reduce the time of operation and lower the chance of radial nerve injury. The aim of this study is to evaluate the outcomes of UHN through antegrade approach in patients with humeral shaft fractures.
Materials and Methods
A prospective study of management of acute humeral shaft fractures by antegrade UHN was undertaken in our hospitals over a period of 2 years (January 2003 to January 2005). The average follow-up period was 1 year (range 10–24 months).
The protocol of the study was approved by the institutional committee of Shahid Beheshti Medical University (SBMU) and each patient before participating in the study provided the informed consent. Forty-one patients with closed acute humeral shaft fractures requiring operative management were treated with UHN. The inclusion criteria were: (1) humeral shaft fractures which indicated operative treatment and were managed through interlocking and (2) patients with age of over 18 years. The exclusion criteria were: (1) patients of age less than 18 years, (2) segmental fractures, (3) fractures were within 4 cm of proximal or distal end of humerus, (4) pathological fractures. All patients had suitable clinical and radiological evaluation before making a decision about surgical intervention. All fractures were classified according to the Muller AO classification. After using the inclusion and exclusion criteria, we included 41 patients for UHN. For proximal entrance, a 1–2 cm incision was carefully made on the anterolateral portion of the shoulder in order to minimize the injury to deltoid muscle, and the rotator cuff antegrade interlocking method was applied with an intra-medullary nail (Russell-Taylor type) (Fig. 1).
Fig. 1.
Proximal entrance incision site
The important hypothesis in this study is that according to the shoulder’s wide range of motion even if not locking the distal portion causes some extent of non-union, it would not cause any rotation limit. Not locking the distal portion would significantly reduce the duration of the operation and lower the risk of radial nerve injury. Active and passive motions of the elbow and pendulum exercises of the shoulder were started immediately after operation. And after 2 weeks, active and passive flexion and abduction of the shoulder were started. Rotational movements of the shoulder especially against resistance for at least 3 weeks were prohibited. Patients were visited within 1–2 month interval for at least 6 months. Union status was investigated using control radiographies. Side effects were recorded for each patient. The functional status of the shoulder and elbow was evaluated using the Society of the American Shoulder and Elbow Surgery (SASES) scoring system (see Appendix 1). Scores (98 to 100) were considered excellent, (95 to 98) good and under 95 were unacceptable. As defined by the standard, duration for normal union is 8 to12 weeks, delayed union is 3 to 6 months and for non-union it is more than 6 months. The exact time that takes for each patient to return to daily activities was recorded. Statistical analysis was carried out by means of SPSS 18.0 software for Windows. The results are expressed as means±SD and student t test analysis were performed for their comparison. Probability values of less than .05 were considered significant.
Results
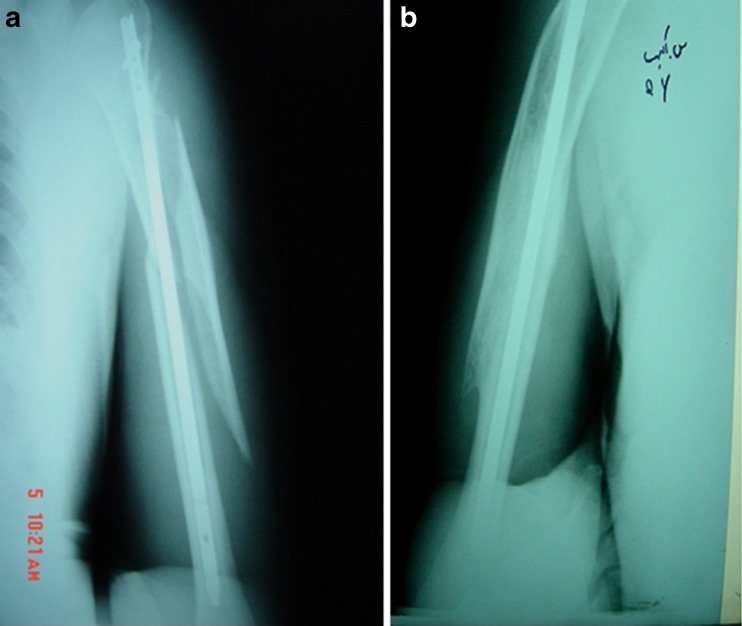
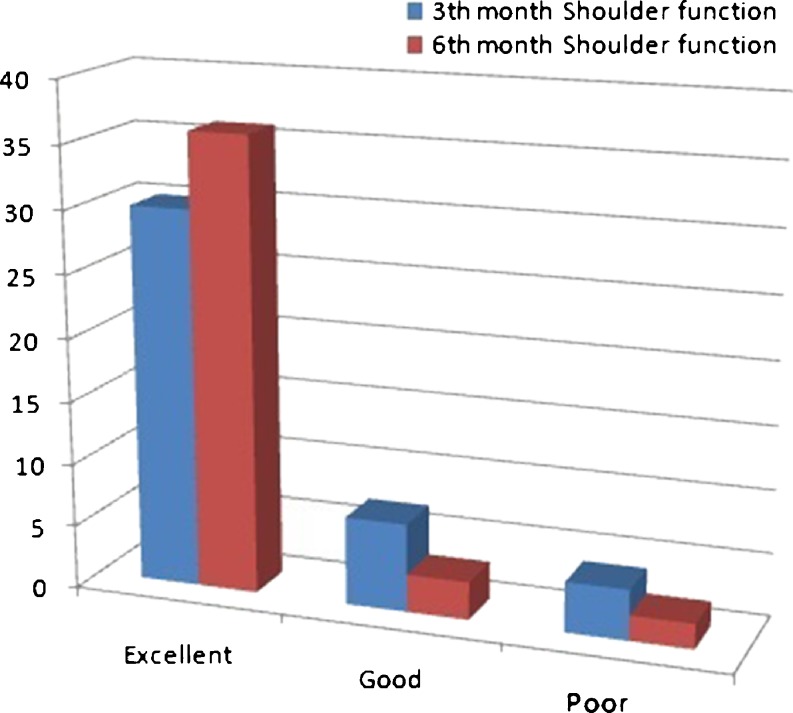
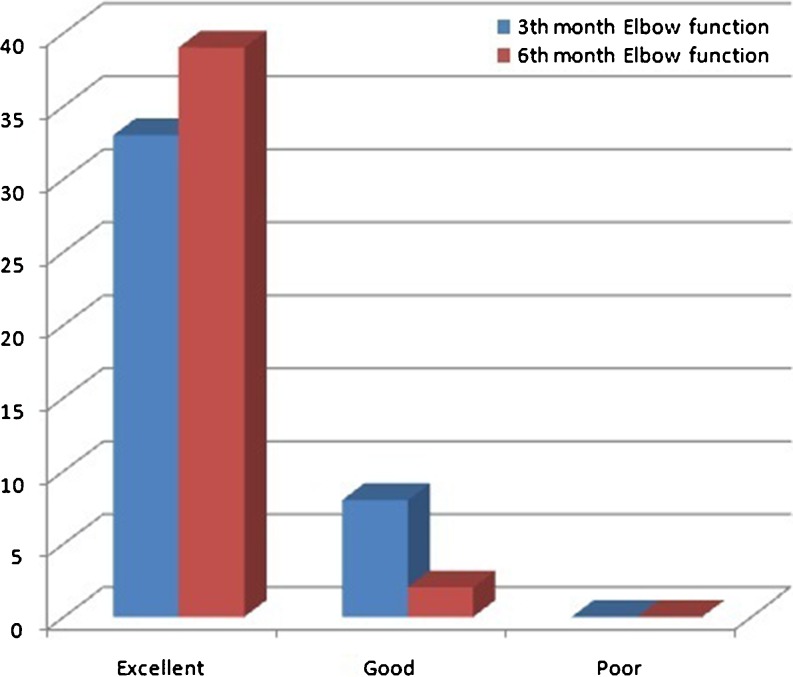
Of our 41 patients, 7 (17 %)] were women and 34 (83 %) were men. The youngest patient in our trial was 21 years while the oldest was 59 years, and the mean age was 39. The maximum incidence was seen in age groups 21–30 and 31–40 years. Motor vehicle accidents accounted for about 78 % of the fractures followed by other causes. All of the fractures could be classified as A3 and B2 of the AO classification, and 68 % happened in the middle third of the humerus shaft. Associated medical problems included diabetes mellitus in three patients, hypertension in four patients and ischemic heart disease in two patients. All of our patients were nailed in a close manner and the operation time averaged 34 min (34 ± 10.1). Pre-operative radial nerve palsy was seen in three cases (7.3 %) in our cases. All patients with pre-operative radial nerve palsy after stabilization recovered completely, representing a neuropraxia kind of injury. The average union time was 13 weeks (13 ± 7.3) (Fig. 2). Operation associated complications have been summarized in Table 1. One patient developed post-operative radial nerve palsy, but after about 6 weeks this patient stated no problem in association with radial nerve territory. The average union time in four patients with radial nerve palsy (before and after surgery) was 20 weeks, which is statistically significant from the group without radial nerve palsy (P < 0.05). Shoulder and elbow functions are shown in Table 1 and Figs. 3 and 4. The average time of returning to daily activities was 4 weeks and turning back to their jobs was about 10 weeks. In an incidental finding after 1 year in six patients who underwent UHN extraction, bone growing in the distal portion of the nail’s canal was found, which we think that it may facilitate rotational stability of the fracture site in spite of nailing without distal locking (Fig. 5).
Fig. 2.
a-Post-operation radiograph of UHN. b-Radiograph of good results with interlocking nailing
Table 1.
Outcomes and operation associated complications in our patients
| N (41) | % | |
|---|---|---|
| Shoulder function at 3th month | ||
| Excellent | 30 | 73.2 |
| Good | 7 | 17 |
| Poor | 4 | 9.8 |
| Elbow function at 3th month | ||
| Excellent | 33 | 80.5 |
| Good | 8 | 19.5 |
| Poor | 0 | 0 |
| Shoulder function at 6th month | ||
| Excellent | 36 | 87.8 |
| Good | 3 | 7.3 |
| Poor | 2 | 4.9 |
| Elbow function at 6th month | ||
| Excellent | 39 | 95.1 |
| Good | 2 | 4.9 |
| Poor | 0 | 0 |
| Delayed union | 3 | 7.3 |
| Non union | 2 | 4.9 |
| Infection | 0 | 0 |
| Nerve palsy | 1 | 2.5 |
Fig. 3.
Comparison of shoulder function
Fig. 4.
Comparison of elbow function
Fig. 5.
Bone growing in distal portion of the nail’s canal may lead to rotational stability of the fracture site
Discussion
Most of the fractures of the humerus shaft could be treated with non-operative techniques [9]. But there are always some problems such as long duration of the treatment and low compliance of patients, which have led researchers to operative techniques. The standard technique for the operative approach is plate fixation. Nevertheless one of the common complications in this method is radial nerve injury, which has been reported in about 3–20 % of patients [5, 6, 8]; non-union has also been reported in about 2–6 % of patients [5, 8, 10, 11]. In the UHN technique, radial nerve injury in 2–4 % of patients has been reported [7–9], and non-union has been seen in 5–10 % of patients [9, 12–14]. In all these articles, proximal and distal locking has been performed simultaneously. Malfunction of the shoulder has been reported in the antegrade technique due to rotator cuff injury [7, 8]. This study has been performed with two main hypotheses:
Not locking the distal portion will not cause an important problem for patients due to the shoulder’s wide range of motion, and it may help union process by putting stress on the site.
Rotator cuff injury would be least if the minimally invasive method in proximal entrance with 1–2 cm approach in anterolateral portion of the shoulder is used.
Pretell et al. [15] operated the humeral pathologic shaft fractures by means of intra-medullary nailing and the mean operating time was 48 minutes (range 35–160 min). Koike et al. [16] evaluated the clinical and radiographic results of the intra-medullary nailing retrospectively and the mean operation time was 84 min (range 54–114 min). In comparison with mentioned studies, our technique can significantly reduce the operating time of nail insertion in patients with humeral shaft fractures (P < 0.05). McCormack et al. [17] compares the outcomes of humeral shaft fractures via intra-medullary nailing and dynamic compression plate, and the rate of non-union in the nailing group was 9.5 %. Also, Singisetti and Ambedkar [4] in a prospective study compared the clinical results of nailing and plating, and the non-union rate of the nailing group was 5 %. With regard to the above studies, our technique leads to slightly increased non-union rate. McCormack et al. [17] reported three cases of post-operative radial nerve palsy among 21 patients who underwent intra-medullary nailing (14.2 %). In our patients, only one case of post-operative radial nerve palsy was detected, and the patient recovered after about 6 weeks of operation.
In our study, the rate of union was perfectly acceptable, and the functions of the shoulder and elbow were in excellent or at least good range in most of the patients; two hypotheses concluded to be correct. The important point is that all the patients who had radial nerve palsy had delayed union. And the only case of non-union was in a patient with radial nerve palsy.
Conclusion
Overall it seems that the use of minimally invasive antegrade UHN without distal locking method is safe, easy and acceptable for humerus shaft fractures, and reduces the risk of radial nerve injury and union period.
Details of the American Shoulder and Elbow Surgeons’ (ASES) score
(4 = normal; 3 = mild compromise, 2 = difficulty, 1 = with aid, 0 = unable, NA = not available)
Back pocket
Perineal care
Wash opposite axilla
Eat with utensil
Comb hair
Use arm at shoulder level
Carry 10 lb at side
Dress
Sleep on affected side
Pull
Use hand overhead
Throw
Lift
References
- 1.Tsai CH, Fong YC, Chen YH, Chang CH, Hsu HC. The epidemiology of traumatic humeral shaft fractures in Taiwan. Int Orthop. 2009;33(2):463–467. doi: 10.1007/s00264-008-0537-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foster RJ, Dixon GL, Jr, Bach AW, Appleyard RW, Green TM. Internal fixation of fractures and non-unions of the humeral shaft. Indications and results in a multi-center study. J Bone Joint Surg Am. 1985;67(6):857–864. [PubMed] [Google Scholar]
- 3.Sarmiento A, Waddell JP, Latta LL. Diaphyseal humeral fractures: treatment options. Instr Course Lect. 2002;51:257–269. [PubMed] [Google Scholar]
- 4.Singisetti K, Ambedkar M. Nailing versus plating in humerus shaft fractures: a prospective comparative study. Int Orthop. 2010;34(4):571–576. doi: 10.1007/s00264-009-0813-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bell MJ, Beauchamp CG, Kellam JK, McMurtry RY. The results of plating humeral shaft fractures in patients with multiple injuries. The Sunnybrook experience. J Bone Joint Surg Br. 1985;67(2):293–296. doi: 10.1302/0301-620X.67B2.3980544. [DOI] [PubMed] [Google Scholar]
- 6.Heim D, Herkert F, Hess P, Regazzoni P. Surgical treatment of humeral shaft fractures—the Basel experience. J Trauma. 1993;35(2):226–232. doi: 10.1097/00005373-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Ingman AM, Waters DA. Locked intramedullary nailing of humeral shaft fractures. Implant design, surgical technique, and clinical results. J Bone Joint Surg Br. 1994;76(1):23–29. [PubMed] [Google Scholar]
- 8.Rommens PM, Blum J, Runkel M. Retrograde nailing of humeral shaft fractures. Clin Orthop Relat Res. 1998;350:26–39. doi: 10.1097/00003086-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Blum J, Rommens PM, Janzing H. The unreamed humeral nail—a biological osteosynthesis of the upper arm. Acta Chir Belg. 1997;97(4):184–189. [PubMed] [Google Scholar]
- 10.Bandi W. Indication to and technique for osteosynthesis in the shoulder. Helv Chir Acta. 1964;31:89–100. [PubMed] [Google Scholar]
- 11.Bleeker WA, Nijsten MW, ten Duis HJ. Treatment of humeral shaft fractures related to associated injuries. A retrospective study of 237 patients. Acta Orthop Scand. 1991;62(2):148–153. doi: 10.3109/17453679108999244. [DOI] [PubMed] [Google Scholar]
- 12.Brug E, Westphal T, Schäfers G. Differential treatment of diaphyseal humerus fractures. Unfallchirurg. 1994;97(12):633–638. [PubMed] [Google Scholar]
- 13.Brumback RJ. The rationales of interlocking nailing of the femur, tibia, and humerus. Clin Orthop Relat Res. 1996;324:292–320. doi: 10.1097/00003086-199603000-00036. [DOI] [PubMed] [Google Scholar]
- 14.Derweduwen J. A new intramedullary compression device for fractures and pseudarthroses of the long bones. A preliminary report. Acta Orthop Belg. 1979;45(6):659–665. [PubMed] [Google Scholar]
- 15.Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop. 2010;34(4):559–563. doi: 10.1007/s00264-009-0833-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koike Y, Komatsuda T, Sato K. Internal fixation of proximal humeral fractures with a Polarus humeral nail. J Orthop Traumatol. 2008;9(3):135–139. doi: 10.1007/s10195-008-0019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82(3):336–339. doi: 10.1302/0301-620X.82B3.9675. [DOI] [PubMed] [Google Scholar]