Abstract
IMPORTANCE
Trabeculectomy is the surgical standard of care for patients with medically refractory glaucoma. The use of antimetabolite agents, such as mitomycin, has increased the rate of complications after trabeculectomy.
OBJECTIVE
To determine the rate of trabeculectomy-related complications during a 25-year study.
DESIGN, SETTING, AND PARTICIPANTS
For this retrospective, population-based study, we enrolled the residents of Olmsted County, Minnesota, who underwent a trabeculectomy from January 1, 1985, through December 31, 2010, at the Mayo Clinic and Olmsted Community Hospital. Data were collected from August 2012 to September 2013 followed by data analysis through January 2014.
EXPOSURES
After reviewing the patient records, we determined the occurrence of complications, including bleb leak, hypotony, hyphema, choroidal effusion, choroidal hemorrhage, blebitis, and endophthalmitis, as they relate to the mitomycin concentration administered during the operation. We reviewed relevant publications in Ovid, MEDLINE, and PubMed to identify studies representative of the reported trabeculectomy complication rate.
MAIN OUTCOMES AND MEASURES
Cumulative probabilities of short- and long-term complications, determined using the Kaplan-Meier method, and the relation to mitomycin concentration applied during trabeculectomy.
RESULTS
In 334 patients, 460 eyes underwent trabeculectomy (mean [SD; range] follow-up, 7.7 [5.7; 0–27.7] years). Among them, 159 eyes had complications, with early complications (<3 months) in 100 eyes and late complications (≥3 months) in 59 eyes during the follow-up. Ten eyes had an early and a late complication. The 20-year cumulative chances of early, late, or any complication were 19.7% (95% CI, 16.2%–23.6%), 26.0% (95% CI, 15.0%–36.0%), and 45.0% (95% CI, 38.0%–52.0%), respectively. The cumulative probabilities of vision-threatening complications during 20 years were 2.0% (95% CI, 0%–4.0%) for blebitis and 5.0% (95% CI, 1.0%–9.0%) for endophthalmitis. Association between the rate of trabeculectomy complications and mitomycin dose used was P = .77. In total, 98 cases (21.3%) underwent further surgical procedures related directly to the complication.
CONCLUSIONS AND RELEVANCE
The rate of trabeculectomy-related complications does not appear to be associated with mitomycin use during a mean follow-up of 7.7 years. The rate of vision-threatening complications appears to be comparable to those of previous studies of shorter duration.
Trabeculectomy has historically been the surgical standard of care for patients with medically refractory glaucoma. The introduction of adjunctive antimetabolite agents, such as fluorouracil and mitomycin, has increased the success rate of trabeculectomy by reducing scarring at the filtration site, although these agents have also been reported to increase the rate of posttrabeculectomy complications.1–5
The number of trabeculectomies performed during the past 15 years has declined. The explanation for this decline is likely multifactorial, including an increase in medical management with additional topical agents, concern about trabeculectomy-related complications, and an increase in the use of minimally invasive glaucoma procedures and glaucoma drainage devices. The Medicare claims from 1995 through 2004 indicated a 53% decrease in the number of trabeculectomies and a concomitant 184% increase in tube-shunt procedures.6 The Medicare data likely included a glaucoma filtration device (ExPress; Alcon) as a tube shunt because of initial coding errors when the device was introduced. The downward trend of trabeculectomy was also supported by a survey of members of the American Glaucoma Society,7,8 which showed an increasing preference toward tube shunts and a decline in trabeculectomy combined with mitomycin treatment because of trabeculectomy-associated complications, including blebitis and endophthalmitis.
At the Mayo Clinic, Rochester, Minnesota, the initial surgical intervention for uncontrolled open-angle glaucoma is trabeculectomy. In 2007, the concentration of mitomycin used at the Mayo Clinic with trabeculectomy was decreased from 0.4 to 0.2 mg/mL in an attempt to decrease the number of complications. Unless contraindicated by other risk factors, the use of mitomycin was standardized at 0.2 mg/mL. In this study, we determined the rate of trabeculectomy-related complications in Olmsted County, Minnesota, and the cumulative probabilities of complications over a longer follow-up. We also evaluated the relationship between the concentration of intraoperative mitomycin and postoperative complications for potential changes in the complication rate. Prior studies report the incidence of endophthalmitis as 1.3% during mean follow-ups of 16 months9 and 2.7 years.10 This study constitutes, to our knowledge, the longest population-based study to examine patients for an extensive period and to more accurately assess the long-term risk of complications, such as endophthalmitis, over the lifetime of the trabeculectomy, which may not be reflected in studies of shorter duration.
Methods
The Rochester Epidemiology Project is a database established to facilitate the study of the frequency and the natural history of disease in the residents of Rochester and Olmsted County in Minnesota and is described in detail elsewhere.11,12
Patients 18 years or older at the time of analysis who underwent trabeculectomy at the Mayo Clinic and Olmsted Community Hospital from January 1, 1985, through December 31, 2010, were identified in the Rochester Epidemiology Project with a computerized database search. Follow-up visits were included through 2013. This 25-year interval was chosen to provide adequate postsurgical follow-up and follow-up of a previous study by Parc et al,4 who used the same database to evaluate long-term outcomes of glaucoma filtration surgery from 1965 through 1980. The present study was approved by the institutional review board of the Mayo Clinic. The study complied with the Health Insurance Portability and Accessibility Act and adhered to the tenets of the Declaration of Helsinki. Informed consent was waived, and the data were deidentified.
The study primarily included Olmsted County residents with glaucoma who sought medical care. From these records, we recorded the concentration of mitomycin applied during surgery, intraoperative complications, and all postoperative complications. The postoperative complications were characterized as early onset (<3 months after surgery) and late onset (≥3 months after surgery). The complications included endophthalmitis, defined as the presence of hypopyon and vitreous inflammation; blebitis, defined as localized mucopurulent material in or around the bleb without evidence of hypopyon; and bleb leak, defined as a positive result of Seidel testing.10 Hypotony was defined as an intraocular pressure of no greater than 5 mm Hg. The remaining list of complications included choroidal effusion, choroidal hemorrhage, hyphema, microhyphema, and aqueous misdirection. All available follow-up information for each patient was recorded; all subsequent procedures to address complications were noted.
During the 25 years, all trabeculectomies were performed and managed by glaucoma specialists (including C.L.K.), with some assistance from ophthalmology residents. The primary treatment of the patients was provided by 8 surgeons. All surgeons used a limbal-based approach, with the exception of 1 surgeon, who preferred a fornix-based incision and closure technique. When used, mitomycin was applied by saturating cellulose sponges placed on the episcleral tissue at a concentration of 0.2 or 0.4 mg/mL for 10 seconds to 5 minutes. Mitomycin was adequately irrigated out of the subconjunctival space with balanced salt solution. From 1985 to 2007, mitomycin at a concentration of 0.4 mg/mL was applied for some patients on the basis of risk factors for failure. From 2008 to the present, the mitomycin concentration was standardized to 0.2 mg/mL with the surgeon’s discretion to increase this concentration in patients with other risk factors for failure.
Demographic information was obtained for risk assessment for complications. Ethnicity/race was recorded on the basis of how the patient self-identified on the clinical reports. The associations between complications and patient age, sex, ethnicity/ race, family history, prior cataract extraction, and prior laser trabeculoplasty were explored through Cox proportional hazards regression analysis. The 20-year cumulative percentage of each complication was determined with Kaplan-Meier analysis. The 95% CI was calculated for survival curves determined at various concentrations of mitomycin. Comparisons among various concentrations of mitomycin were completed through the Cox proportional hazards regression model that used robust sandwich estimates13 to account for the potential correlations among the eyes for patients with both eyes in the study. We reviewed Ovid, MEDLINE, and PubMed to identify studies representative of the trabeculectomy complication rates reported.
One of the glaucoma specialists(C.L.K.) trained 2 medical students (J.A.O. and M.B.H.) before the initial data collection, for quality assurance purposes, in ophthalmic terminology and definitions, visual acuity and visual field measurements, and interpretation of eye examination records. Meetings were conducted periodically to ensure appropriate and accurate data collection.
Results
We identified 348 patients in the Rochester Epidemiology Project who underwent trabeculectomy during the study period; 334 of these patients were included in the study (eFigure 1 in the Supplement shows the study flowchart with inclusion and exclusion criteria). The predominant type of glaucoma was open-angle, followed by pseudoexfoliation and narrow-angle glaucoma. Three patients with pediatric glaucoma were included in whom the initial trabeculectomy occurred in the pediatric years and subsequent trabeculectomy occurred at 18 years or older. All cases of neovascular glaucoma were excluded because our institution uses a primary glaucoma drainage device for these high-risk patients.
We evaluated the records from 460 eyes of these 334 patients. The mean age at first trabeculectomy was 71 (median, 74) years; mean (SD;range) follow-up was7.7(5.7;0–27.7) years. Demographic information about patients with complications is listed in Table 1. Baseline clinical characteristics among patients with and without complications were similar. Age, sex, ethnicity/race, family history, prior cataract extraction, and prior laser trabeculoplasty were not predictors of late trabeculectomy complications (P > .10, Cox proportional hazards regression analysis). As depicted in Table 1, men had a higher rate of severe complications than did women (39 of 133 [29.3%] vs 27 of 201 [13.4%]). The risk for blebitis or endophthalmitis was 5.3% (7 of 133) in men and 2.0% (4 of 201) in women. During the follow-up period, complications developed in 159 eyes, with early complications in 100 eyes and late complications in 59 eyes. Ten eyes had an early and a late complication. The cumulative risk for any trabeculectomy-related complication during the 20 years was 45.0% (95% CI, 38.0%–52.0%) (eFigure 2 in the Supplement). The overall, early, and late complication rates are summarized in Table 2.
Table 1.
Demographic Characteristics of the Study Population Experiencing Severe Complications
| Characteristic | Complicationa | All Patients (N = 334)b | |||
|---|---|---|---|---|---|
| Bleb Leak (n = 31) | Choroidal Effusion/ Hemorrhage (n = 24) | Blebitis (n = 3) | Endophthalmitis (n = 8) | ||
| Patient age at initial surgery, mean (SD; range), y | 63 (21; 6–88) | 74 (17; 0–86) | 57 (15; 40–68) | 65 (24; 6–80) | 71 (15; 0–103) |
| Sex | |||||
| Male | 18 | 14 | 3 | 4 | 133 |
| Female | 13 | 10 | 0 | 4 | 201 |
| Ethnicity/race | |||||
| White | 28 | 22 | 3 | 7 | 312 |
| Black | 3 | 0 | 0 | 1 | 8 |
| Asian | 0 | 2 | 0 | 0 | 5 |
| Hispanic | 0 | 0 | 0 | 0 | 1 |
| Other/unknown | 0 | 0 | 0 | 0 | 8 |
| Family history of glaucoma | |||||
| Yes | 17 | 8 | 2 | 3 | 162 |
| No | 14 | 16 | 1 | 5 | 172 |
| Laterality, No. of eyes | |||||
| Right | 13 | 8 | 1 | 3 | 225 |
| Left | 18 | 16 | 2 | 5 | 235 |
| Previous cataract, No. of eyes | |||||
| Yes | 1 | 1 | 0 | 2 | 30 |
| No | 30 | 23 | 3 | 6 | 430 |
| Previous laser trabeculoplasty, No. of eyes | |||||
| Yes | 11 | 17 | 2 | 4 | 188 |
| No | 20 | 7 | 1 | 4 | 272 |
Values are expressed as number of patients unless specified otherwise.
Includes 460 eyes.
Table 2.
Postoperative Complication Rates
| Complication | No. (%) of Eyes | ||
|---|---|---|---|
| Early (n = 100)a | Late (n = 59)b | All (N = 159) | |
| Hyphema | 38 (38.0) | 5 (8.5) | 43 (27.0) |
| Bleb leak | 13 (13.0) | 18 (30.5) | 31 (19.5) |
| Hypotony | 17 (17.0) | 13 (22.0) | 30 (18.9) |
| Microhyphema | 17 (17.0) | 1 (1.7) | 18 (11.3) |
| Choroidal effusion | 7 (7.0) | 10 (16.9) | 17 (10.7) |
| Endophthalmitis | 0 | 8 (13.6) | 8 (5.0) |
| Choroidal hemorrhage | 7 (7.0) | 0 | 7 (4.4) |
| Blebitis | 1 (1.0) | 2 (3.4) | 3 (1.9) |
| Aqueous misdirection | 0 | 2 (3.4) | 2 (1.3) |
Indicates less than 3 months after trabeculectomy.
Indicates 3 months or longer after trabeculectomy.
Early and Late Complications
Hyphema and microhyphema were the most frequent early-onset complications, followed by hypotony, bleb leak, and choroidal effusion or hemorrhage, respectively. Most hyphema and microhyphema resolved without intervention within a few weeks of surgery. No cases of aqueous misdirection or endophthalmitis were noted within the first 3 months after surgery.
The most frequent complication at 3 months and later was late bleb leak, which persisted and often led to a surgical intervention. The second most frequent late-onset complication was hypotony followed by late choroidal effusion. Severe complications, such as blebitis (2 eyes) and endophthalmitis (8 eyes), developed as time after surgery increased. Three of the 8 patients with endophthalmitis had concurrent bleb leaks, and 1 patient had undergone previous treatment with a scleral buckle procedure for retinal detachment in the affected eye. One of the 3 patients with pediatric glaucoma developed bleb leak and endophthalmitis.
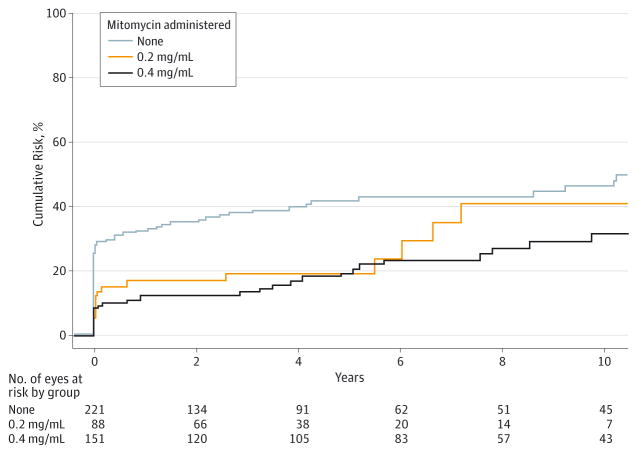
The 20-year cumulative risk for each complication is shown in Figure 1. The chances of having vision-threatening complications, such as blebitis and endophthalmitis, during the 20 postoperative years were 2.0% (95% CI, 0%–4.0%) and 5.0% (95% CI, 1.0%–9.0%), respectively (Kaplan-Meier). The probability of any late-onset complications during the 20 years was 26.0% (95% CI, 15.0%–36.0%). No difference in the trabeculectomy-related complication rate was seen when we compared complications before and after 2007 (P = .61).
Figure 1. Cumulative Risk for Trabeculectomy-Related Complications.
The 20-year cumulative percentage of trabeculectomy-related complications were calculated by Kaplan-Meier analysis. Error bars indicate 95% CI.
Complications and Mitomycin Administration
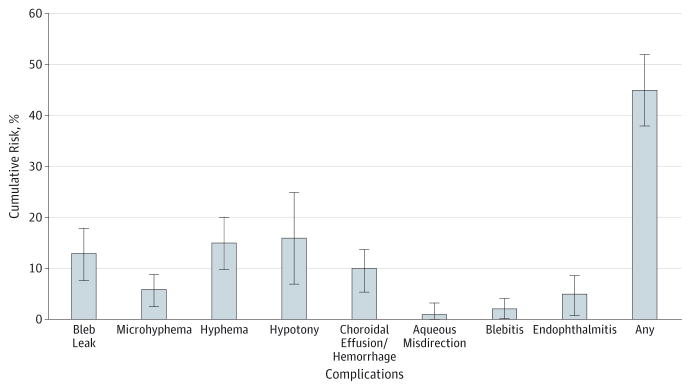
Table 3 shows the distribution of mitomycin doses at none, 0.2, and 0.4 mg/mL in the 460 eyes. Among the 239 eyes receiving mitomycin with trabeculectomy, the duration of mitomycin administration ranged from 10 seconds to 5 minutes in 223 (93.0%). Mean exposure to mitomycin (calculated as time in seconds per concentration in milligrams per milliliter) was 36.8 and the median (SD; range), 24 (32.8; 0–120). We found no increased risk for complications with increased mitomycin concentration. Trabeculectomy-related complications were not significantly different between those receiving mitomycin concentrations of 0.2 and 0.4 mg/mL (P = .88). We found no difference in the rate of endophthalmitis (P = .44) or in the rate of late complications (P = .77) among the 3 mitomycin treatment groups, as depicted in Figure 2. This study had an 80% chance of finding a difference as small as 16% when such a difference existed between the mitomycin and no-mitomycin groups (α = .05 and β = 0.20, with the number based on each group).
Table 3.
Relation Between Mitomycin Concentration and Complications
| Mitomycin Dose, mg/mL | No. of Eyes | Cases, No. (%) of Eyes | |
|---|---|---|---|
| Endophthalmitis | Any Complication | ||
| None | 221 | 4 (1.8) | 74 (33.5) |
| 0.2 | 88 | 2 (2.3) | 22 (25.0) |
| 0.4 | 151 | 2 (1.3) | 35 (23.2) |
| All | 460 | 8 (1.7) | 131 (28.5) |
Figure 2. Kaplan-Meier Curve of Trabeculectomy-Related Complications With Various Mitomycin Concentrations.
Kaplan-Meier curve shows the cumulative risk of all complications with no administration of mitomycin or mitomycin concentrations of 0.2 and 0.4 mg/mL during a 10-year follow-up.
Management and Outcome
The median duration of the 159 complications recorded was 13 days; the 25th percentile was 6 days and the 75th percentile was 37 days. In 98 eyes (21.3%), additional surgical procedures were needed to resolve the complication (eFigure 3 in the Supplement). Many of the early complications were self-limiting; in contrast, 34 eyes with late-onset complications (58%) required surgical intervention. Of the complications, hypotony and bleb leaks were the main indications for bleb revisions. The most common interventions were bleb revision in 41 eyes (42%), drainage of choroidal effusion or hemorrhage in 18 eyes (18%), and intraocular injections in 14 eyes (14%). Although cataract progression was not documented, 106 eyes (23.0%) had cataract extraction at some time after trabeculectomy.
Blebitis and endophthalmitis did not progress after treatment with topical or intravitreal antibiotics, respectively. Bleb revisions or subsequent trabeculectomies after bleb failure, intraocular pressure spikes, and decreased vision were not considered a complication but rather failure of the trabeculectomy. These variables are not discussed in this report.
Discussion
Overall Complications
This study shows an overall lower rate of trabeculectomy-related complications than previous reports with shorter follow-ups. The 20-year cumulative probability of early complications (<3 months after trabeculectomy) at 19.7% (95% CI, 16.2%–23.6%) is lower than the probability in other published reports,14,15 in which it ranged from 37% to 47% in the short term. Our late complication cumulative probability of 26.0% (95% CI, 15.0%–36.0%) is comparable to that of other reports,10,14,15 which ranged from 14% to 42% for long-term complications (mean follow-up, about 5 years). The variability in complication rates in previous studies may be from the arbitrary cutoff of early vs late complications, which fluctuated from 2 weeks to 3 months postoperatively. Another source of variability in reported complication rates is related to the varying definitions of trabeculectomy complications. In our study, complications included hyphema, hypotony, aqueous misdirection, choroidal effusion or hemorrhage, bleb leaks, blebitis, and endophthalmitis. Cataract formation or progression, a well-known trabeculectomy-related complication,16 was not documented formally. Of the listed complications, our study identified hyphema and microhyphema as the most common early complications, similar to other reports, followed by hypotony and bleb leak. Although most of these early complications were transient and self-remitting, any remnant or persistent complication after 3 months postoperatively should be monitored and treated accordingly to prevent further complications.
Bleb-Related Infections
During the study interval, the rate of endophthalmitis was 1.7%, with a mean follow-up of 7.7 years. This rate is comparable to the endophthalmitis rates of 0.3% to 4.9% found in other retrospective studies1,5,9,10,15,17–28 and is lower than that of prospective studies (eTable in the Supplement). In the previous Mayo Clinic study of long-term filtration surgery outcomes from 1965 to 1980, Parc et al4 reported an endophthalmitis rate of 4% (2 of 49 patients). Despite our endophthalmitis rate that was significantly lower than that of the previous Mayo Clinic study,4 our results were comparable to other similar studies9 that reported the cumulative incidence of bleb-associated endophthalmitis from 0.2% to 9.6% after various filtration procedures with or without antimetabolite use.
The similarity in surgical history and demographic characteristics between the study by Parc et al4 and our study indicated that surgical technique might be a major contributing factor for a low rate of complications, especially endophthalmitis. In addition, the rate of endophthalmitis (8 cases in 460 eyes) was higher than that of blebitis (3 cases in 460 eyes) and had a risk of 2% during 20 years, illustrated through Kaplan-Meier analysis. The increased rate of endophthalmitis in comparison with blebitis was attributed to the patients’ delay in returning to the clinic during early onset of infection or individual risk factors for disease severity. Men also had a higher rate of severe complications than women in this study. The factors contributing to this result are unclear. The incidence of severe complications in each subset was too small to draw accurate conclusions about sex predilections for complications. One could theorize that hormonal factors in women contributed to a lower rate of complications; however, the association or the mechanism has not been proved.
Recent studies reported bleb leaks as the most common complication of trabeculectomy with mitomycin19,20,22,25,27 and as a predisposing factor for blebitis and endophthalmitis.17,20,21,29,30 Soltau et al31 reported a likelihood of late-onset bleb leakage in bleb-related infection 25.8 times that of a noninfected eye for having a late-onset bleb leak in the postoperative period. Our study confirms the association between bleb leaks and endophthalmitis; 3 of our patients with endophthalmitis had late-onset bleb leaks before the infection. Although routine postoperative examination includes Seidel testing at each visit, Seidel testing might not have been performed at each visit during the entirety of the 7-year mean follow-up and thus was underreported.
Complications and Mitomycin Administration
Our study suggests that the rate of trabeculectomy-related complications does not appear to be associated with mitomycin use as it has been in other studies. An increase in mitomycin concentration applied in patients with stable complication risk, the surgical technique used, a limited duration of mitomycin administration, or accurate assessment of risk factors may contribute to the lack of association. Given that only higher-risk patients undergo mitomycin administration with trabeculectomy, the difference in complications based on mitomycin dose might not have been significant. These patients may be at a higher risk for trabeculectomy failure and therefore have a decreased risk for choroidal effusion or hemorrhage, bleb leaks, and endophthalmitis based on this pattern of care at our institution. The 8 glaucoma specialists involved in the trabeculectomies were experienced in assessing appropriate mitomycin applications, which might account for the similar complication rate with or without mitomycin administration. The sample size in each group receiving mitomycin at doses of none, 0.2, and 0.4 mg/mL was sufficient to provide an 80% chance of finding a minimum difference of 16% between groups if a difference this large existed (α = .05 and β = 0.20). However, the inconsistency of mitomycin application time, ranging from 10 seconds to 5 minutes, showed a wide distribution too complex for computing complication risk assessment.
In this study, the complication rate was unchanged during the 25-year study period regardless of changes in mitomycin administration before and after 2007. This unchanged rate could be attributed to consistency in surgical technique during the study years among the 8 glaucoma specialists in Olmsted County. Soltau et al31 reported young age, black race, primary open-angle glaucoma, and an inferior location of filtering bleb as risk factors for trabeculectomy complications. Although some of these risk factors were assessed in this study, black individuals constituted 2.4% of the study population, and inferior trabeculectomy was not used by the 8 surgeons. The white homogeneity of our study population requiring less mitomycin exposure could be another possible confounding variable for the lack of increased risk for complications with mitomycin administration.
Complication-Related Interventions
Most of the trabeculectomy complications (ie, hyphema, hypotony, and bleb leaks) were self-limited; however, the more persistent complications required surgical intervention. Our rates of bleb revision (8.9%) and overall complication-related surgical intervention (21.3%) were similar to rates of 2% to 17% for bleb revisions in other reports10,14,15,17,26 and 7% to 85% for all procedures.5,14,15,21,28 The large discrepancy in the intervention rate reported in the literature resulted in part from differences in the inclusion or exclusion of specific procedures, such as laser suture lysis and cataract extraction.
Study Advantages and Limitations
Our study has the advantages of being a large patient series, including short- and long-term complications, having a mean follow-up of more than 7 years, and using analysis of surgical outcome with Kaplan-Meier statistics. The use of surgical judgment to adjust mitomycin concentrations may be considered a strength in realistic settings for favorable outcomes. The overall complication rate may reflect the performance of the trabeculectomy by glaucoma specialists, a surgical group experienced in adjusting mitomycin exposure. The limitations of the study include its retrospective design, multiple surgeons, and a homogeneous population of white patients that is unrepresentative of the general population of patients with glaucoma. Therefore, the study results may not be applicable for a more heterogeneous population. The mixture of pediatric and adult glaucoma, although small, is a confounding factor given that pediatric glaucoma presents with a varying assemblage of complications compared with adult glaucoma and has an elevated risk for vision-threatening complications.
Conclusions
We report a 25-year review of the trabeculectomy complication rate in a well-defined population. This study indicates that our complication rates are favorable compared with many published studies that reported a higher complication risk during a shorter study period. Our study did not show a linear trend in complications with mitomycin, which may reflect surgical techniques and the surgical judgment of mitomycin application by the glaucoma specialists. Given the higher rate of endophthalmitis juxtaposed with blebitis, further care will be given for patient education regarding a timely return visit for postoperative complications to prevent late detection of vision-threatening outcomes.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported in part by research grant R01AG034676 from the National Institutes of Health (Rochester Epidemiology Project); by an unrestricted grant from Research to Prevent Blindness, Inc; and by the Mayo Foundation for Medical Education and Research.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Additional Contributions: Jay W. McLaren, PhD, Department of Ophthalmology at the Mayo Clinic, Rochester, Minnesota, provided critical review and comments on the manuscript. No compensation was received for this role.
Author Contributions: Dr Khanna had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Khanna.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Olayanju, Khanna.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Hodge, Khanna.
Obtained funding: Khanna.
Administrative, technical, or material support: Olayanju, Hassan, Khanna.
Study supervision: Khanna.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Contributor Information
Jessica A. Olayanju, Currently a medical student at Mayo Clinic College of Medicine, Rochester, Minnesota.
Mohamed B. Hassan, Currently a medical student at Mayo Clinic College of Medicine, Rochester, Minnesota.
David O. Hodge, Department of Health Sciences Research, Mayo Clinic, Jacksonville, Florida.
Cheryl L. Khanna, Department of Ophthalmology, Mayo Clinic, Rochester, Minnesota.
References
- 1.Higginbotham EJ, Stevens RK, Musch DC, et al. Bleb-related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmology. 1996;103(4):650–656. doi: 10.1016/s0161-6420(96)30639-8. [DOI] [PubMed] [Google Scholar]
- 2.Lama PJ, Fechtner RD. Antifibrotics and wound healing in glaucoma surgery. Surv Ophthalmol. 2003;48(3):314–346. doi: 10.1016/s0039-6257(03)00038-9. [DOI] [PubMed] [Google Scholar]
- 3.Palmer SS. Mitomycin as adjunct chemotherapy with trabeculectomy. Ophthalmology. 1991;98(3):317–321. doi: 10.1016/s0161-6420(91)32293-0. [DOI] [PubMed] [Google Scholar]
- 4.Parc CE, Johnson DH, Oliver JE, Hattenhauer MG, Hodge DO. The long-term outcome of glaucoma filtration surgery. Am J Ophthalmol. 2001;132(1):27–35. doi: 10.1016/s0002-9394(01)00923-0. [DOI] [PubMed] [Google Scholar]
- 5.Reibaldi A, Uva MG, Longo A. Nine-year follow-up of trabeculectomy with or without low-dosage mitomycin-C in primary open-angle glaucoma. Br J Ophthalmol. 2008;92(12):1666–1670. doi: 10.1136/bjo.2008.140939. [DOI] [PubMed] [Google Scholar]
- 6.Ramulu PY, Corcoran KJ, Corcoran SL, Robin AL. Utilization of various glaucoma surgeries and procedures in Medicare beneficiaries from 1995 to 2004. Ophthalmology. 2007;114(12):2265–2270. doi: 10.1016/j.ophtha.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Desai MA, Gedde SJ, Feuer WJ, Shi W, Chen PP, Parrish RK., II Practice preferences for glaucoma surgery. Ophthalmic Surg Lasers Imaging. 2011;42 (3):202–208. doi: 10.3928/15428877-20110224-04. [DOI] [PubMed] [Google Scholar]
- 8.Joshi AB, Parrish RK, II, Feuer WF. 2002 Survey of the American Glaucoma Society: practice preferences for glaucoma surgery and antifibrotic use. J Glaucoma. 2005;14(2):172–174. doi: 10.1097/01.ijg.0000151684.12033.4d. [DOI] [PubMed] [Google Scholar]
- 9.Greenfield DS, Suñer IJ, Miller MP, Kangas TA, Palmberg PF, Flynn HW., Jr Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114(8):943–949. doi: 10.1001/archopht.1996.01100140151007. [DOI] [PubMed] [Google Scholar]
- 10.DeBry PW, Perkins TW, Heatley G, Kaufman P, Brumback LC. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol. 2002;120(3):297–300. doi: 10.1001/archopht.120.3.297. [DOI] [PubMed] [Google Scholar]
- 11.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, III, Rocca WA. Generalizability of epidemiological findings and public health decisions. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Stat Assoc. 1989;84:1074–1078. [Google Scholar]
- 14.Edmunds B, Thompson JR, Salmon JF, Wormald RP. The National Survey of Trabeculectomy, III: early and late complications. Eye (Lond) 2002;16(3):297–303. doi: 10.1038/sj.eye.6700148. [DOI] [PubMed] [Google Scholar]
- 15.Gedde SJ, Herndon LW, Brandt JD, et al. Tube vs Trabeculectomy Study Group. Postoperative complications in the Tube vs Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012;153(5):804–814. e1. doi: 10.1016/j.ajo.2011.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.AGIS (Advanced Glaucoma Intervention Study) Investigators. The Advanced Glaucoma Intervention Study, 8: risk of cataract formation after trabeculectomy. Arch Ophthalmol. 2001;119 (12):1771–1779. doi: 10.1001/archopht.119.12.1771. [DOI] [PubMed] [Google Scholar]
- 17.Palanca-Capistrano AM, Hall J, Cantor LB, Morgan L, Hoop J, WuDunn D. Long-term outcomes of intraoperative 5-fluorouracil versus intraoperative mitomycin C in primary trabeculectomy surgery. Ophthalmology. 2009;116 (2):185–190. doi: 10.1016/j.ophtha.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Mochizuki K, Jikihara S, Ando Y, Hori N, Yamamoto T, Kitazawa Y. Incidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5-fluorouracil treatment. Br J Ophthalmol. 1997;81(10):877–883. doi: 10.1136/bjo.81.10.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck AD, Wilson WR, Lynch MG, Lynn MJ, Noe R. Trabeculectomy with adjunctive mitomycin C in pediatric glaucoma. Am J Ophthalmol. 1998;126(5):648–657. doi: 10.1016/s0002-9394(98)00227-x. [DOI] [PubMed] [Google Scholar]
- 20.Solomon A, Ticho U, Frucht-Pery J. Late-onset, bleb-associated endophthalmitis following glaucoma filtering surgery with or without antifibrotic agents. J Ocul Pharmacol Ther. 1999;15 (4):283–293. doi: 10.1089/jop.1999.15.283. [DOI] [PubMed] [Google Scholar]
- 21.Bindlish R, Condon GP, Schlosser JD, D’Antonio J, Lauer KB, Lehrer R. Efficacy and safety of mitomycin-C in primary trabeculectomy: five-year follow-up. Ophthalmology. 2002;109(7):1336–1341. doi: 10.1016/s0161-6420(02)01069-2. [DOI] [PubMed] [Google Scholar]
- 22.Beckers HJ, Kinders KC, Webers CA. Five-year results of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2003;241(2):106–110. doi: 10.1007/s00417-002-0621-5. [DOI] [PubMed] [Google Scholar]
- 23.Muckley ED, Lehrer RA. Late-onset blebitis/endophthalmitis: incidence and outcomes with mitomycin C. Optom Vis Sci. 2004;81(7):499–504. doi: 10.1097/00006324-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Jongsareejit B, Tomidokoro A, Mimura T, Tomita G, Shirato S, Araie M. Efficacy and complications after trabeculectomy with mitomycin C in normal-tension glaucoma. Jpn J Ophthalmol. 2005;49(3):223–227. doi: 10.1007/s10384-004-0181-9. [DOI] [PubMed] [Google Scholar]
- 25.Shigeeda T, Tomidokoro A, Chen YN, Shirato S, Araie M. Long-term follow-up of initial trabeculectomy with mitomycin C for primary open-angle glaucoma in Japanese patients. J Glaucoma. 2006;15(3):195–199. doi: 10.1097/01.ijg.0000212202.57029.45. [DOI] [PubMed] [Google Scholar]
- 26.Fontana H, Nouri-Mahdavi K, Lumba J, Ralli M, Caprioli J. Trabeculectomy with mitomycin C: outcomes and risk factors for failure in phakic open-angle glaucoma. Ophthalmology. 2006;113 (6):930–936. doi: 10.1016/j.ophtha.2006.01.062. [DOI] [PubMed] [Google Scholar]
- 27.Giampani J, Jr, Borges-Giampani AS, Carani JC, Oltrogge EW, Susanna R., Jr Efficacy and safety of trabeculectomy with mitomycin C for childhood glaucoma. Clinics (Sao Paulo) 2008;63(4):421–426. doi: 10.1590/S1807-59322008000400002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jampel HD, Solus JF, Tracey PA, et al. Outcomes and bleb-related complications of trabeculectomy. Ophthalmology. 2012;119(4):712–722. doi: 10.1016/j.ophtha.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 29.Greenfield DS, Liebmann JM, Jee J, Ritch R. Late-onset bleb leaks after glaucoma filtering surgery. Arch Ophthalmol. 1998;116(4):443–447. doi: 10.1001/archopht.116.4.443. [DOI] [PubMed] [Google Scholar]
- 30.Scott IU, Greenfield DS, Schiffman J, et al. Outcomes of primary trabeculectomy with the use of adjunctive mitomycin. Arch Ophthalmol. 1998;116(3):286–291. doi: 10.1001/archopht.116.3.286. [DOI] [PubMed] [Google Scholar]
- 31.Soltau JB, Rothman RF, Budenz DL, et al. Risk factors for glaucoma filtering bleb infections. Arch Ophthalmol. 2000;118(3):338–342. doi: 10.1001/archopht.118.3.338. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.