Abstract
Background
Patients hospitalized with heart failure are often readmitted. Health literacy may play a substantial role in the high rate of readmissions. The purpose of this study was to examine the association of health literacy with the composite end point of heart failure readmission rates and all-cause mortality in patients with heart failure living in rural areas.
Methods and Results
Rural adults (n = 575), hospitalized for heart failure within the last 6 months completed the Short Test of Functional Health Literacy in Adults (STOFHLA) to measure health literacy and were followed for at least two years. The percent of patients with the end point of heart failure readmission or all-cause death was different (p=0.001) among the three STOFHLA score levels. Unadjusted analysis revealed that patients with inadequate or marginal health literacy were 1.94 (95% confidence intervals [CI] 1.43, 2.63; p < 0.001) times, and 1.91 (95% CI 1.36, 2.67; p < 0.001) times, respectively, more likely to experience the outcome. After adjustment for covariates, health literacy remained a predictor of outcomes. Of the other covariates, worse functional class, higher comorbidity burden and higher depression score predicted worse outcomes.
Conclusion
Inadequate or marginal health literacy is a risk factor for heart failure rehospitalization or all-cause mortality among rural heart failure patients.
Clinical Trials Registration: ClinicalTrials.gov; NCT00415545; http://clinicaltrials.gov/ct2/show/NCT00415545?term=dracup&rank=3
Keywords: Health literacy, heart failure, rural
Heart failure patients have 30-day hospital readmission rates of about 25%, which are higher than those seen in other chronic conditions in Medicare-aged individuals, [1-3] and account for the majority of the cost associated with heart failure care. Risk models or scores to predict risk of readmission among heart failure patients usually are limited to factors predominantly linked to patient demographics and clinical characteristics.[4] For example, demographic characteristics such as age, gender, and race are associated with heart failure readmission.[1, 5-10] Clinical factors associated with heart failure readmission include comorbidity burden.[5, 10-12] There are, however, potentially other important, modifiable predictors of rehospitalization.
Because heart failure management is complex it requires a high level of patient participation.[13, 14] Having adequate heart failure knowledge and the requisite skills to engage in appropriate self-care are fundamental to avoiding preventable hospitalizations. Although few investigators have evaluated the impact of health literacy on heart failure readmission and mortality rates, general medical patients with poor health literacy were more likely to be hospitalized in one study of the Medicare population.[15] Specifically among heart failure patients, poor health literacy is associated with higher all-cause mortality in an integrated managed care organization.[16]
Health literacy is "the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions."[17] As such, although it is related to literacy, it is a construct distinct from literacy. Many literate people have low levels of health literacy, thus it is not sufficient to assume that if one is literate, one will have adequate health literacy.
In the rural setting where patients typically have lower socioeconomic resources, the impact of health literacy on heart failure admission is unknown. Moreover, previous investigators have not controlled for variables in analyses, such as depression, [15, 16, 18] which is known to be common among patients with heart failure and is associated with outcomes in such patients, and that therefore could affect the association of health literacy with outcomes. Some analyses were limited to Medicare populations [15] or managed care organizations.[16] We therefore performed an analysis in a multicenter, rural sample enrolled in a randomized clinical trial of an education intervention designed to reduce heart failure related hospitalization.[19] We specifically examined the association of health literacy measured using the Short Test of Functional Health Literacy in Adults (STOFHLA) with heart failure readmission rates and all-cause mortality, while controlling for demographic, clinical and psychological covariates potentially related to the outcome or to health literacy.
Study Design and Sample
The study was conducted within the context of the randomized controlled trial, Rural Education to Improve Outcomes in Heart Failure (REMOTE-HF).[19] In brief, we tested an education and counseling intervention among rural heart failure patients with limited access to treatment in order to improve self-care abilities and decrease preventable readmissions. Patients were randomly assigned to one of the following three groups: 1) usual care; 2) Fluid Watchers LITE, which included the education program with minimal follow-up; and 3) Fluid Watchers PLUS, which included the education program with attention to individualization and biweekly follow-up.
We obtained appropriate Institutional Review Board approval from all sites. Informed signed consent to participate was received from each patient. Patients living in rural California, Nevada, and Kentucky were recruited. Patients were recruited from outpatient clinics and hospitals after referral to the study by healthcare providers working at these sites. Inclusion criteria included the following: 1) age 18 years and older with stable heart failure at the time of enrollment; 2) heart failure hospitalization in the past 12 months; 3) ability to read and write English; 4) living independently (i.e., not institutionalized). Exclusion criteria included the following: 1) serious life-limiting comorbidity (i.e., disease or illness predicted to cause death within the next 12 months); 2) diagnosed major psychiatric illness such as schizophrenia; 3) impaired cognition; or 4) concurrent participation in a heart failure disease management program. Cognitive screening using the Mini-Cog, which is a global measure of cognitive status,[20] was performed on patients who met other inclusion criteria to identify cognitive dysfunction that would preclude participation. Patients with a word recall score of < 3 or an abnormal clock drawing score were excluded.
After obtaining consent and before randomization, patients completed questionnaires and trained research associates reviewed their medical records. Data on sociodemographic (i.e., age, gender, race, marital status, employment status, education level), clinical (i.e., comorbidity burden, b-type natriuretic peptide, New York Heart Association [NYHA] functional class, and left ventricular ejection fraction [LVEF], and psychological variables (i.e., depression), as well as health literacy were collected at this time. All patients were followed for the composite end-point of heart failure rehospitalization or all-cause death for at least 2 years.
Measures
Outcome
The combined end-point was heart failure rehospitalization or all-cause death. Patients were followed for at least 2 years to collect these data, which were determined using patient and family interview, medical record and hospital administrative database review, healthcare provider contact, and review of death records. Patients were phoned monthly in order to decrease the likelihood that we would miss an event and to increase retention.
Covariates
Health literacy was measured at baseline and before randomization using the S-TOFHLA, which has 36-items. Patients are scored on the number of items they get correct in seven minutes. The S-TOFHLA measures the patient’s ability to read and understand health-related passages using a section on preparation for an x-ray procedure and a Medicaid application. The S-TOFHLA uses the Cloze procedure, in which an omitted word in a sentence must be chosen by the patient from a multiple choice list. Results are categorized into the following three levels: 1) inadequate (0-16 correct answers); 2) marginal (17-22 correct answers); and 3) adequate health literacy (23-36 correct answers). Adequate reliability and validity have been demonstrated for the S-TOFHLA, and it has been widely used in research in a variety of patient populations.[21] The Cronbach’s alpha in our study was 0.762.
Comorbidity burden was assessed using the Charlson Comorbidity Index (CCI)[22] The CCI has well-established reliability and validity for the prediction of cumulative mortality attributable to comorbid disease.[22] The CCI is weighted for severity of comorbidity and is computed as a total score. A higher CCI score implies higher comorbidity burden.
Depression was measured using the Patient Health Questionnaire-9.[23, 24] This instrument is composed of nine items that are reflective of each of the nine symptoms for diagnosing major depressive disorder based on DSM-IV criteria. Responding by using a 4-point Likert scale, patients consider how commonly they have experienced the symptoms referred to in the items in the past two weeks. Score are totaled and can range from 0 to 27 with higher scores reflecting more severe depressive symptoms. This instrument is brief, reliable, valid and sensitive.[23-25] Cronbach’s alpha assessing the reliability of the instrument in this study was 0.873.
New York Heart Association functional classification was assigned by trained cardiovascular research nurses based on careful interview done at the time of enrollment. B-type natriuretic peptide was measured at the time of enrollment using point of care testing equipment that was calibrated before each use. Left ventricular ejection fraction was retrieved from the medical record and the measure made closest to the enrollment date was used. A standardized form was used to collect demographic information. These data were age, gender, marital status, education, and employment.
Data Analysis
Data were analyzed using SPSS for Windows version 20.0. Patient characteristics were compared among the three health literacy groups using chi-square or ANOVA as appropriate. Rates of occurrence of the end-point were compared among the three health literacy groups using chi-square. Unadjusted Cox proportional hazards regression was used to determine the predictive ability of health literacy for time to the composite end-point without covariates. We then used Cox proportional hazards regression modeling to determine predictive ability for time to the first occurrence of the composite end-point of all-cause death or heart failure hospitalization from the covariates of age, gender, education, marital status, employment status, study, group, LVEF, b-type natriuretic peptide level, comorbidity burden, NYHA class, depression and health literacy. The covariates were included in the model using forced entry of all variables simultaneously. Proportional hazards assumptions were tested by examination of the deviations between the observed cumulative martingale residuals and the values of the explanatory variables from random simulations, and by evaluation of the Kolmogorov-type supremum tests from multiple simulated patterns. There were no violations of the assumptions.
Results
Of the 614 rural heart failure patients enrolled and followed for at least 2 years, 575 patients (93.6%) had baseline STOFHLA data and complete follow-up. There were no differences in characteristics between the 575 patients who had complete data and the 39 who did not have complete data.
Patients scored a mean of 25.6 ± 8.8 items (71.1 ± 24.3%) correct on the STOHFLA. A total of 110 (19.1%) patients received scores placing them in the inadequate health literacy category, 96 (16.7%) in the marginal category and 369 (64.2%) in the adequate category. Comparison of baseline characteristics among the three categories of health literacy revealed that patients differed in age, gender, education, employment, and depression score among the three groups (Table 1). Patients who were older, male, less educated, and unemployed, were more likely to be in a lower health literacy group. Patients with higher depression scores were more likely to be in the marginal health literacy group.
Table 1.
Baseline Characteristics Compared by Health Literacy Groups
| Health Literacy Groups (N=575) | ||||
|---|---|---|---|---|
|
Inadequate
Score=0-16 n = 110 |
Marginal
Score = 17-22 n = 96 |
Adequate
Score= 23-36 n = 369 |
p-value | |
| Characteristics | ||||
| Age, mean ± SD | 73.9 ± 10.7 | 68.0 ± 11.9 | 63.0 ± 12.6 | <0.001 |
| Charlson Comorbidity Index, mean ± SD |
3.4 ± 1.73 | 3.4 ± 1.8 | 3.3 ± 1.8 | 0.791 |
| Left ventricular ejection fraction, % |
40.1 ± 15.8 | 41.0 ± 15.9 | 39.1 ± 15.7 | 0.518 |
| B-type natriuretic peptide, pcg/ml |
524 ± 1474 | 444 ± 555 | 376 ± 904 | 0.396 |
| Depression score | 6.5 ± 5.5 | 8.8 ± 7.2 | 7.2 ± 6.4 | 0.026 |
| N (%) | N (%) | N (%) | ||
| Caucasian | 99 (90.9) | 84 (87.5) | 328 (88.9) | 0.850 |
| Female | 35 (31.8) | 35 (36.5) | 164 (44.4) | 0.040 |
| Currently married or cohabitating |
63 (57.3) | 61 (63.5) | 205 (55.6) | 0.371 |
| Education | <0.001 | |||
| less than high school | 31 (28.2) | 20 (20.8) | 43 (11.7) | |
| high school graduate | 53 (48.2) | 47 (49.0) | 185 (50.1) | |
| beyond high school | 26 (23.6) | 29 (30.2) | 141 (38.2) | |
| Employed | 5 (4.5) | 8 (8.3) | 72 (19.5) | <0.001 |
| NYHA functional class I-II III-IV |
61 (55.5) 49 (44.5) |
55 (57.3) 41 (42.7) |
260 (70.7) 108 (29.3) |
0.002 |
| Study group Usual care LITE PLUS |
45 (40.9) 33 (30.0) 32 (29.1) |
35 (36.5) 34 (35.4) 27 (28.1) |
120 (32.5) 125 (33.9) 124 (33.6) |
0.498 |
NYHA = New York Heart Association; STOFHLA = Short Test of Functional Health Literacy in Adults
A total of 63 deaths from all causes occurred during the study period. There were almost twice as many deaths in the inadequate and marginal health literacy groups as in the adequate group (Table 2). There were 249 heart failure admissions and there were significantly more in the inadequate and marginal health literacy groups than in the adequate health literacy group (Table 2).
Table 2.
Occurrence of Heart Failure Admission or All-Cause Death by Health Literacy
| Health Literacy Groups, N = 575 | ||||
|---|---|---|---|---|
|
Inadequate
Score = 0-16 n = 110 |
Marginal
Score = 17-22 n = 96 |
Adequate
Score= 23-36 n = 369 |
p-value | |
| N (%) | N (%) | N (%) | ||
| All-cause deaths | 17 (15.5) | 14 (14.6) | 32 (8.7) | 0.001 |
| Heart failure rehospitalizations |
44 (40.0) | 33 (34.4) | 172 (29.9) | |
| Did not experience the end- point |
49 (44.5) | 49 (51.0) | 242 (65.6) | |
Group (N=575)
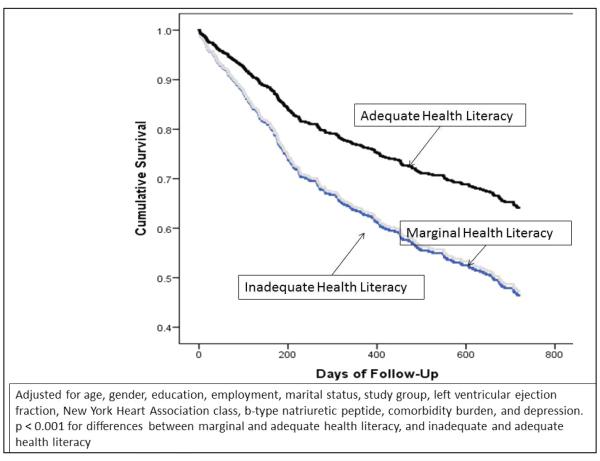
Unadjusted Cox regression revealed that patients with inadequate or marginal health literacy were 1.94 (95% confidence intervals [CI] 1.43, 2.63; p < 0.001) times, and 1.91 (95% CI 1.36, 2.67; p < 0.001) times, respectively, more likely to experience the outcome (Figure 1). After adjustment for all covariates, health literacy remained a strong predictor of outcomes (Figure 2). Patients with inadequate or marginal health literacy were 1.71 (95% confidence intervals [CI] 1.20, 2.44; p = 0.003) times, and 1.66 (95% CI 1.16, 2.39; p = 0.006) times, respectively, more likely to experience the outcome (Table 3). Of the other covariates, only NYHA class, comorbidity burden and depression score predicted outcomes. Patients with worse NYHA class, greater comorbidity burden, and higher depression scores have worse outcomes.
Figure 1.
Unadjusted Cox Proportional Hazards Regression Model Survival Curve For Prediction of Composite End-point of Heart Failure Hospitalization or All-Cause Death from Health Literacy
Figure 2.
Cox Proportional Hazards Regression Model Survival Curve for Prediction of Composite End-point of Heart Failure Hospitalization or All-Cause Death from Health Literacy, Adjusted for Covariates
Table 3.
Results of Multivariable Cox Regression Analysis
| Variables | Hazard Ratio | P Value | 95% Confidence Intervals |
|---|---|---|---|
| Male gender | 1.229 | .191 | .902-1.675 |
| Age | 1.010 | .254 | .993-1.026 |
| Not married, divorced or widowed (vs married or cohabitate) |
.995 | .971 | .747-1.324 |
| Education level | 1.187 | .443 | .766-1.841 |
| Employed for pay (vs all else) | 1.031 | .754 | .605-1.757 |
| Intervention group Control vs LITE Control vs PLUS |
1.325 1.013 |
.167 .096 .941 |
.952-1.846 .724-1.417 |
| Left ventricular ejection fraction | .996 | .397 | .986-1.006 |
| NYHA class III/IV (vs I/II) | 1.850 | <.001 | 1.389-2.465 |
| B-type natriuretic peptide | 1.00 | .180 | 1.000-1.000 |
| Comorbidity burden | 1.101 | .012 | 1.022-1.186 |
| Depression score | 1.036 | .002 | 1.013-1.058 |
| Health literacy Marginal vs adequate Inadequate vs adequate |
1.714 1.662 |
.002 .003 .006 |
1.202-2.443 1.156-2.391 |
Discussion
Since the publication of studies demonstrating the low level of health literacy among adults in the United States,[17, 26] researchers and clinicians began expressing concern about the impact of poor health literacy on health in people with chronic conditions like heart failure.[27-29] Poor health literacy among patients with heart failure has been found to be associated with low levels of knowledge about the condition,[18, 30-32] poor adherence to medication regimens,[33] poor self-care,[18, 34] less self-efficacy,[18] and more frequent use of the emergency department for heart failure exacerbations.[35] These associations suggest that health literacy is also likely to be associated with rehospitalization rates and mortality. Indeed these outcomes are worse among those with poor health literacy in a general Medicare population,[15] and all-cause mortality, but not rehospitalization rate, was higher among low literacy heart failure patients in a managed care system.[16] Recently, investigators have demonstrated, in ambulatory heart failure patients, that low health literacy was associated with both heart failure readmissions and all-cause mortality.[18]
In our large sample of rural patients from geographically different areas of the United States, we noted that slightly more than one-third of the sample had marginal or inadequate health literacy. These rates compare similarly to comparable samples of heart failure patients in which the same instrument was used to measure health literacy,[18, 32, 34] and are lower than the 61% reported in an urban, largely male and minority population.[36] In our study, patients in either the marginal or inadequate health literacy categories had substantially greater risk for heart failure rehospitalization or all-cause mortality than those patients with adequate health literacy, even in the context of other strong risk factors like depression, comorbidity burden and functional status. These data highlight the unique importance of health literacy to clinical outcomes in heart failure, and provide direction for future education efforts, and changes to policy and healthcare systems.[36]
Special approaches are needed in caring for patients with poor health literacy to ensure optimal outcomes. Such approaches may include improved provider-patient communication, development of appropriate patient education materials, and self-care promotion interventions. Use of more direct, collaborative communication practices by clinicians when interacting with patients, which involve conversation, not just delivery of instructions may improve health literacy or outcomes in low literacy patients.[37] With this communication approach, both the patient and health care provider are better able to understand how well the intended message was communicated. Prevailing evidence indicates that most heart failure patient education materials in hospitals and clinics do not meet criteria that make their content appropriate for most patients because of lack of understandability.[38] This finding suggests that all heart failure patient education materials need to be assessed for relevancy to those with low health literacy and revised, if needed, to make them useful. There are however, no studies in which revision of commonly used materials has been tested directly.
Very few investigators have tested disease management interventions designed to improve outcomes of self-care among low literacy heart failure patients. In one effort, a multilevel pharmacist-led disease management intervention that included patient-centered written material with visual aids for low literacy was successful in improving patient satisfaction and medication adherence, and reducing emergency department visits and hospital readmissions, but only while the intervention was active.[39] In another test of a single-session versus a multisession self-care intervention that was designed to be literacy-sensitive, there were no differences in outcomes (i.e., quality of life, hospitalization or death) between the groups.[40] Trends in the data from this study suggest that among low literacy patients, the multisession intervention may have reduced hospitalization and mortality.[40] Taken together, the data on success of interventions to improve health literacy in patients with heart failure is quite modest, and much more work in this area is needed to clearly delineate the components of interventions necessary to enhance health literacy.
Some have suggested that the importance of the finding of a link between health literacy and outcomes lies in identification of a strong predictor of outcomes that could be measured easily by clinicians.[16] More importantly, however, these data demonstrate the importance of patient-centered variables, like health literacy, that are commonly overlooked by clinicians who are trained to concentrate on patients’ clinical characteristics. The emphasis on medications and devices to manage heart failure without attention to the impact of health literacy on uptake of these therapies by patients and on the uptake of related self-care behaviors reduces their effectiveness in many cases.
In our study, we also identified three other independent predictors of poor outcomes along with inadequate or marginal health literacy. These predictors were higher depression scores, worse NYHA functional class, and greater comorbidity burden. These findings are not new, but serve to confirm previous findings of the importance of these factors for defining risk for poor outcomes. Both clinically diagnosed depression and depressive symptoms are linked, independently, to morbidity and mortality. [41-44] We have previously demonstrated that depressive symptoms are an even stronger predictor for poor outcomes among patients with heart failure than b-type natriuretic peptide levels.[45] The independent association of both health literacy and depression with poor outcomes highlights the importance of cognitive and psychological variables in the clinical management of heart failure.
Greater comorbidity burden and worse NYHA functional class, common in patients with heart failure, both independently (and jointly) portend worse rehospitalizations and mortality outcomes.[46, 47] We have demonstrated previously that functional status mediates the relationship between poor quality of life and cardiac event-free survival in heart failure.[46] These two prognostic indicators of poor outcomes are easily assessed in the clinical setting and provide important targets for intervention.
Limitations
Although a strength of this study is the enrollment of a large sample of patients with heart failure living in rural areas, this also serves as a limitation in that we are not able to generalize to non-rural populations.
Conclusion
Marginal or inadequate health literacy measured using a brief standardized reliable and valid instrument to assess health literacy is associated with higher risk of earlier heart failure hospitalization or all-cause death among rural patients with heart failure. Research is needed to define effective interventions to provide heart failure patients with limited health literacy the knowledge and skills they need to manage heart failure, and determine if such interventions also improves rehospitalization and mortality outcomes.
Highlights.
We studied health literacy in the context of demographic, clinical and psychological covariates.
This was a multicenter study of rural patients.
Inadequate or marginal health literacy, as assessed by the Short Test of Functional Health Literacy in Adults (STOFHLA), is a significant independent risk factor for heart failure rehospitalization or all-cause mortality among rural heart failure patients
Acknowledgment
Funding Sources: This study was funded by the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute of Nursing Research (NINR): 5R01HL83176-5
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None
Contributor Information
Debra K. Moser, University of Kentucky, College of Nursing.
Susan Robinson, University of California, San Francisco.
Martha J. Biddle, University of Kentucky.
Michele M. Pelter, University of Reno, Nevada.
Tom Nesbitt, University of California Davis.
Jeffery Southard, University of California, Davis.
Lawton Cooper, National Institutes of Health, National Heart Lung and Blood Institute.
Kathleen Dracup, University of California, San Francisco.
References
- [1].Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. The New England journal of medicine. 2011;365:2287–95. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- [2].Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- [3].Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circulation Cardiovascular quality and outcomes. 2011;4:53–9. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Betihavas V, Davidson PM, Newton PJ, Frost SA, Macdonald PS, Stewart S. What are the factors in risk prediction models for rehospitalisation for adults with chronic heart failure? Australian critical care : official journal of the Confederation of Australian Critical Care Nurses. 2011 doi: 10.1016/j.aucc.2011.07.004. [DOI] [PubMed] [Google Scholar]
- [5].Aranda JM, Jr., Johnson JW, Conti JB. Current trends in heart failure readmission rates: analysis of Medicare data. Clinical cardiology. 2009;32:47–52. doi: 10.1002/clc.20453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kossovsky MP, Sarasin FP, Perneger TV, Chopard P, Sigaud P, Gaspoz J. Unplanned readmissions of patients with congestive heart failure: do they reflect in-hospital quality of care or patient characteristics? Am J Med. 2000;109:386–90. doi: 10.1016/s0002-9343(00)00489-7. [DOI] [PubMed] [Google Scholar]
- [7].Howie-Esquivel J, Dracup K. Effect of gender, ethnicity, pulmonary disease, and symptom stability on rehospitalization in patients with heart failure. The American journal of cardiology. 2007;100:1139–44. doi: 10.1016/j.amjcard.2007.04.061. [DOI] [PubMed] [Google Scholar]
- [8].Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hamner JB, Ellison KJ. Predictors of hospital readmission after discharge in patients with congestive heart failure. Heart & lung : the journal of critical care. 2005;34:231–9. doi: 10.1016/j.hrtlng.2005.01.001. [DOI] [PubMed] [Google Scholar]
- [10].Muzzarelli S, Leibundgut G, Maeder MT, Rickli H, Handschin R, Gutmann M, et al. Predictors of early readmission or death in elderly patients with heart failure. American heart journal. 2010;160:308–14. doi: 10.1016/j.ahj.2010.05.007. [DOI] [PubMed] [Google Scholar]
- [11].Hallerbach M, Francoeur A, Pomerantz SC, Oliner C, Morris DL, Eiger G, et al. Patterns and predictors of early hospital readmission in patients with congestive heart failure. American journal of medical quality : the official journal of the American College of Medical Quality. 2008;23:18–23. doi: 10.1177/1062860607310916. [DOI] [PubMed] [Google Scholar]
- [12].Greenberg BH, Abraham WT, Albert NM, Chiswell K, Clare R, Stough WG, et al. Influence of diabetes on characteristics and outcomes in patients hospitalized with heart failure: a report from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) American heart journal. 2007;154:277. doi: 10.1016/j.ahj.2007.05.001. e1-8. [DOI] [PubMed] [Google Scholar]
- [13].Moser DK, Dickson V, Jaarsma T, Lee C, Stromberg A, Riegel B. Role of self-care in the patient with heart failure. Current cardiology reports. 2012;14:265–75. doi: 10.1007/s11886-012-0267-9. [DOI] [PubMed] [Google Scholar]
- [14].Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141–63. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- [15].Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American journal of public health. 2002;92:1278–83. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Literacy CoH. Health Literacy: A Prescription to End Confusion. The National Academies Press; 2004. [PubMed] [Google Scholar]
- [18].Wu JR, Holmes GM, DeWalt DA, Macabasco-O'Connell A, Bibbins-Domingo K, Ruo B, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28:1174–80. doi: 10.1007/s11606-013-2394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Robinson S, Moser D, Pelter MM, Nesbitt T, Paul SM, Dracup K. Assessing health literacy in heart failure patients. J Card Fail. 2011;17:887–92. doi: 10.1016/j.cardfail.2011.06.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Steenland NK, Auman CM, Patel PM, Bartell SM, Goldstein FC, Levey AI, et al. Development of a rapid screening instrument for mild cognitive impairment and undiagnosed dementia. Journal of Alzheimer's disease : JAD. 2008;15:419–27. doi: 10.3233/jad-2008-15308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- [22].Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- [23].Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American journal of obstetrics and gynecology. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- [24].Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- [25].Kung S, Alarcon RD, Williams MD, Poppe KA, Jo Moore M, Frye MA. Comparing the Beck Depression Inventory-II (BDI-II) and Patient Health Questionnaire (PHQ-9) depression measures in an integrated mood disorders practice. Journal of affective disorders. 2013;145:341–3. doi: 10.1016/j.jad.2012.08.017. [DOI] [PubMed] [Google Scholar]
- [26].Kutner M, Greenberg E, Jin Y, Paulsen C. In: The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. Statistics USDoE, editor. National Center for Education; Washington, DC: 2006. [Google Scholar]
- [27].Evangelista LS, Rasmusson KD, Laramee AS, Barr J, Ammon SE, Dunbar S, et al. Health literacy and the patient with heart failure--implications for patient care and research: a consensus statement of the Heart Failure Society of America. J Card Fail. 2010;16:9–16. doi: 10.1016/j.cardfail.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Morrow D, Clark D, Tu W, Wu J, Weiner M, Steinley D, et al. Correlates of health literacy in patients with chronic heart failure. Gerontologist. 2006;46:669–76. doi: 10.1093/geront/46.5.669. [DOI] [PubMed] [Google Scholar]
- [29].Riegel B, Moser DK, Powell M, Rector TS, Havranek EP. Nonpharmacologic care by heart failure experts. J Card Fail. 2006;12:149–53. doi: 10.1016/j.cardfail.2005.10.004. [DOI] [PubMed] [Google Scholar]
- [30].Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- [31].Kollipara UK, Jaffer O, Amin A, Toto KH, Nelson LL, Schneider R, et al. Relation of lack of knowledge about dietary sodium to hospital readmission in patients with heart failure. Am J Cardiol. 2008;102:1212–5. doi: 10.1016/j.amjcard.2008.06.047. [DOI] [PubMed] [Google Scholar]
- [32].Chen AM, Yehle KS, Albert NM, Ferraro KF, Mason HL, Murawski MM, et al. Relationships between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Research in social & administrative pharmacy : RSAP. 2013 doi: 10.1016/j.sapharm.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Noureldin M, Plake KS, Morrow DG, Tu W, Wu J, Murray MD. Effect of health literacy on drug adherence in patients with heart failure. Pharmacotherapy. 2012;32:819–26. doi: 10.1002/j.1875-9114.2012.01109.x. [DOI] [PubMed] [Google Scholar]
- [34].Macabasco-O'Connell A, Dewalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26:979–86. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–8. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Dennison CR, McEntee ML, Samuel L, Johnson BJ, Rotman S, Kielty A, et al. Adequate health literacy is associated with higher heart failure knowledge and self-care confidence in hospitalized patients. J Cardiovasc Nurs. 2011;26:359–67. doi: 10.1097/JCN.0b013e3181f16f88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Seligman HK, Wang FF, Palacios JL, Wilson CC, Daher C, Piette JD, et al. Physician notification of their diabetes patients' limited health literacy. A randomized, controlled trial. J Gen Intern Med. 2005;20:1001–7. doi: 10.1111/j.1525-1497.2005.00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Taylor-Clarke K, Henry-Okafor Q, Murphy C, Keyes M, Rothman R, Churchwell A, et al. Assessment of commonly available education materials in heart failure clinics. J Cardiovasc Nurs. 2012;27:485–94. doi: 10.1097/JCN.0b013e318220720c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, et al. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med. 2007;146:714–25. doi: 10.7326/0003-4819-146-10-200705150-00005. [DOI] [PubMed] [Google Scholar]
- [40].DeWalt DA, Schillinger D, Ruo B, Bibbins-Domingo K, Baker DW, Holmes GM, et al. Multisite randomized trial of a single-session versus multisession literacy-sensitive self-care intervention for patients with heart failure. Circulation. 2012;125:2854–62. doi: 10.1161/CIRCULATIONAHA.111.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Johnson TJ, Basu S, Pisani BA, Avery EF, Mendez JC, Calvin JE, Jr., et al. Depression predicts repeated heart failure hospitalizations. J Card Fail. 2012;18:246–52. doi: 10.1016/j.cardfail.2011.12.005. [DOI] [PubMed] [Google Scholar]
- [42].Moraska AR, Chamberlain AM, Shah ND, Vickers KS, Rummans TA, Dunlay SM, et al. Depression, healthcare utilization, and death in heart failure: a community study. Circulation Heart failure. 2013;6:387–94. doi: 10.1161/CIRCHEARTFAILURE.112.000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Newhouse A, Jiang W. Heart failure and depression. Heart failure clinics. 2014;10:295–304. doi: 10.1016/j.hfc.2013.10.004. [DOI] [PubMed] [Google Scholar]
- [44].Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–37. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- [45].Song EK, Moser DK, Frazier SK, Heo S, Chung ML, Lennie TA. Depressive symptoms affect the relationship of N-terminal pro B-type natriuretic peptide to cardiac event-free survival in patients with heart failure. J Card Fail. 2010;16:572–8. doi: 10.1016/j.cardfail.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Le Corvoisier P, Bastuji-Garin S, Renaud B, Mahe I, Bergmann JF, Perchet H, et al. Functional status and co-morbidities are associated with in-hospital mortality among older patients with acute decompensated heart failure: a multicentre prospective cohort study. Age Ageing. 2015;44:225–31. doi: 10.1093/ageing/afu144. [DOI] [PubMed] [Google Scholar]
- [47].Grodin JL, Hammadah M, Fan Y, Hazen SL, Tang WH. Prognostic value of estimating functional capacity with the use of the duke activity status index in stable patients with chronic heart failure. J Card Fail. 2015;21:44–50. doi: 10.1016/j.cardfail.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]