Abstract
Objectives
We explored if knee pain or a history of knee injury was associated with a knee injury in the following 12 months.
Methods
We conducted longitudinal knee-based analyses among knees in the Osteoarthritis Initiative. We included both knees of all participants who had at least one follow-up visit with complete data. Our first sets of exposures were knee pain (chronic knee symptoms and severity) at baseline, 12-month, 24-month, and 36-month visits. Another exposure was a history of injury, which we defined as a self-reported injury at any time prior to baseline, 12-month, 24-month, or 36-month visits. The outcome was self-reported knee injury during the past year at 12-month, 24-month, 36-month, and 48-month visits. We evaluated the association between ipsilateral and contralateral knee pain or history of injury and a new knee injury within 12 months of the exposure using generalized linear mixed model for repeated binary outcomes.
Results
A knee with reported chronic knee symptoms or ipsilateral or contralateral history of an injury was more likely to experience a new knee injury in the following 12 months than a knee without chronic knee symptoms (odds ratio [OR]=1.84, 95% confidence interval [CI]=1.57, 2.16) or prior injury (prior ipsilateral knee injury OR=1.81, 95% CI=1.56, 2.09; prior contralateral knee injury OR=1.43, 95% CI=1.23, 1.66).
Conclusion
Knee pain and a history of injury are associated with new knee injuries. It may be beneficial for individuals with knee pain or a history of injury to participate in injury prevention programs.
Key Indexing Terms: knee injuries, osteoarthritis, musculoskeletal pain
INTRODUCTION
Individuals with a history of knee injury are 3 to 6 times more likely to develop knee osteoarthritis (KOA) (1, 2) and are on average diagnosed with osteoarthritis approximately 10 years younger than individuals without a history of knee injury (3). Knee injuries are also strongly associated with an accelerated form of knee osteoarthritis (4). Understanding risk factors for knee injury may provide important insight into osteoarthritis prevention. Despite extensive research assessing risk factors for knee injuries among young physically active individuals (under 35 years of age)(5–7) it remains unclear which factors may predispose older adults with, or at risk for, KOA to experience a knee injury.
Individuals with knee pain are at greater risk of falls (8–11) but it is unclear if they are also at risk of knee injuries. Knee pain is associated with altered proprioception (12), which may increase the risk of falls (13, 14). Hence, knee pain may be a risk factor for knee injuries among older adults.
A history of knee injury to the ipsilateral or contralateral knee may also be risk factors for new knee injuries (15–17). Specifically, young physically active individuals with an anterior cruciate ligament (ACL) tear are more than five times as likely to sustain another ACL tear in either knee (16). Despite a history of knee injury being one of the most important risk factors for knee injuries in young physically active individuals (18, 19) there is little evidence to determine if it is also an important risk factor among older and more sedentary adults (20, 21).
The aim of this study was to assess whether knee pain or a history of knee injury increases the risk for a knee injury in the subsequent 12 months among older adults with, or at risk for, KOA. We hypothesized that chronic knee symptoms and greater pain severity predict injuries among individuals with, or at risk for, KOA. Furthermore, we hypothesized that a history of ipsilateral or contralateral knee injury is associated with new injuries.
MATERIALS AND METHODS
To test for an association of knee pain and history of knee injury, with subsequent knee injuries, we conducted longitudinal knee-based analyses using data from the Osteoarthritis Initiative (OAI). We focused on knee-based analyses to test our hypotheses that knee pain or histories of knee injury in the ipsilateral or contralateral knee were important risk factors for new knee injuries. The OAI is a longitudinal observational study of KOA that occurred at four clinical sites in the United States: Memorial Hospital of Rhode Island, The Ohio State University, University of Maryland and John Hopkins University, and the University of Pittsburgh. The staff at the 4 clinical sites enrolled 4,796 men and women (45 to 79 years of age) between February 2004 and May 2006. The OAI cohort comprised three groups classified at baseline: 1) progression subcohort, including individuals with at least one knee with symptomatic radiographic KOA, 2) incidence subcohort, including individuals at risk for symptomatic radiographic KOA, and 3) non-exposed control subcohort, which included individuals with no KOA and no risk factors for KOA. Detailed descriptions of the eligibility criteria for each subcohort and the OAI protocol are publicly available at the OAI website (22). Institutional review boards at each OAI clinical site and the OAI coordinating center (University of California, San Francisco) approved the OAI study.
In this study, we included all knees among OAI participants who attended the baseline visit and at least one follow-up visit, irrespective of whether or not they had KOA. Our first sets of exposures were knee pain (chronic knee symptoms and severity) at baseline, 12-month, 24-month, and 36-month visits. Another exposure was a history of injury, which we defined as a self-reported injury at any time prior to baseline, 12-month, 24-month, or 36-month visits. The outcome was self-reported knee injuries that occurred during the subsequent year – assessed at 12-month, 24-month, 36-month, and 48-month OAI visits.
Knee Pain
To determine if knee pain was associated with subsequent knee injuries we defined pain based on the presence of chronic knee symptoms or pain severity. At each OAI visit participants answered “During the past 12 months, have you had any pain, aching, or stiffness in or around your right knee?” If the participant answered “yes” then they were asked “During the past 12 months, have you had pain, aching, or stiffness in or around your right knee on most days for at least one month? By most days, we mean more than half the days of a month.” The same questions were asked for the left knee. We defined chronic knee symptoms as pain on most days of a month in past 12 months (23, 24).
Knee pain severity was based on the WOMAC pain subscale, a validated outcome measure for KOA(25). The WOMAC pain subscale has five questions that inquire about pain in the last 7 days with walking, stairs, lying in bed, sitting or lying down, and standing. The WOMAC pain subscale was knee specific and we used data from both knees. Each item is scored 0 (none) to 4 (extreme pain) and the subscale ranges from 0 to 20. However, across the annual OAI visits, 95% of knees had WOMAC pain scores between 0 and 9 and > 50% had a WOMAC pain score=0 or 1. Furthermore, we detected a nonlinear association between WOMAC pain and injury. Because of the skewed pain scores and nonlinear association we dichotomized knee severity for our primary analyses as no-to-little pain (0 to 2) or knee pain (≥ 3). The knee pain data are publicly available (Files: allclinical00 (version 0.2.2), allclinical01 (version 1.2.1), allclinical03 (3.2.1), allclinical05 (5.2.1)) (22).
History of Knee Injuries
To determine if a history of joint-specific knee injury was associated with subsequent knee injuries we defined a history of knee injury based on self-reported data from the baseline, 12-, 24-, and 36-month OAI visits. At the OAI baseline visit participants answered “Have you ever injured your right knee badly enough to limit your ability to walk for at least two days?” At each follow-up visit, participants were asked “Since your last annual visit to the OAI clinic about 12 months ago, have you injured your right knee badly enough to limit your ability to walk for at least two days?” Similar questions were asked for the left knee. The injury data are publicly available (Files: allclinical00 (version 0.2.2) allclinical01 (version 1.2.1), allclinical03 (3.2.1), allclinical05 (5.2.1)) (22).
New Knee Injuries
Our main outcome was self-reported knee injury at an OAI follow-up visit. This was defined based on the follow-up visit self-reported questions listed in the previous section. These data are publicly available (Files: allclinical01 (version 1.2.1), allclinical03 (3.2.1), allclinical05 (5.2.1), allclinical06 (version 6.2.1))(22).
Radiographic Assessments
We conducted secondary analyses based on the absence or presence of radiographic KOA at the OAI baseline visit. Weight-bearing, bilateral, fixed-flexion, posterior-anterior knee radiographs were obtained at the OAI baseline. Central readers scored the images for Kellgren-Lawrence Grades (0 to 4). We defined the subset with radiographic KOA as individuals with both knees having Kellgren-Lawrence Grade ≥ 2. We defined the subset without radiographic KOA as individuals with both knees having Kellgren-Lawrence Grade=0 or 1 throughout the study period (baseline to 48 months). We also defined a subset with unilateral KOA as individuals with no osteoarthritis in the ipsilateral knee but with contralateral radiographic KOA. The agreement for these readings (read-reread) was good (weighted kappa (intra-rater reliability)=0.70 to 0.78). These Kellgren-Lawrence grades are publicly available (File: kXR_SQ_BU##_SAS (version 0.6, 1.6, 3.5, 5.5, 6.3))(22).
Clinical Data
Demographic, anthropometric, and other participant characteristics were acquired based on a standard protocol. We extracted age, body mass index (BMI), sex, self-reported strong prescription medication use, Physical Activity Scale for the Elderly scale, and responses regarding frequent knee bending activities. For post hoc analyses we adjusted for frequent knee bending, which we defined as a person who did any of the following tasks for ≥4 days per week in the 30 days prior to a study visit: 1) climbed up “10 or more flights of stairs during a single day”, 2) kneeled “30 minutes or more during a single day”, 3) squatted “30 minutes of more during a single day”, or 4) got “in and out of a squatting position 10 or more times during a single day”. The protocol and data are publicly available (Files: enrollees (version 20), allclinical## (version 0.2.2, 1.2.1, 3.2.1, 5.2.1, 6.2.1) (22).
Statistical Analyses
We evaluated the association between knee pain (chronic symptoms and severity) and a history of knee injury prior to the baseline, 12-month, 24-month, 36-month OAI visits and a knee injury within 12 months by performing knee-based longitudinal analyses using a logistic regression with repeated measures (generalized linear mixed model) to adjust for correlations within person observations over time and between knees. We performed two primary analyses with new knee injuries being the outcome in each. The predictors in each analysis were from the annual visit prior to the outcome of self-reported knee injury status. For example, the analyses assessed whether knee pain at baseline would be associated with a self-reported injury between baseline and the 12-month OAI visit, when a participant reported an injury. The first primary analysis included the presence of chronic knee symptoms in the ipsilateral knee, the presence of chronic knee symptoms in the contralateral knee, the history of knee injury in the ipsilateral knee, and the history of knee injury in the contralateral knee. The second primary analysis was the same except we replaced chronic knee symptoms with knee pain severity in the ipsilateral and contralateral knee. Analyses were adjusted for sex, age, and BMI at each visit because they may be associated with knee pain (26–29) and knee injury (6, 30–34). We did not censor knees since a knee could suffer multiple injuries during the observation period. Each knee could contribute up to 4 observation periods.
As secondary analyses, we replicated our primary analyses in two subsets: 1) individuals with bilateral radiographic KOA and 2) individuals without radiographic KOA. We also conducted secondary analyses by replicating our primary analyses stratified by sex since rates and types of knee injuries vary by sex (6, 33). Finally, we performed a series of post hoc analyses to validate the findings: 1) analyses among individuals with unilateral KOA in the contralateral knee; 2) replication of our analyses after adjusting for a history of knee pain (chronic knee symptoms or severe knee pain), self-reported strong prescription pain medication (e.g., narcotics) use on more than half the days in the month prior to a study visit, physical activity (Physical Activity Scale for the Elderly), or frequent knee bending; 3) person-based analyses in which the outcome was a new knee injury in either knee and the predictors were knee pain in either knee and a history of knee injury in either knee; and 4) analyses of knee pain severity with WOMAC knee pain entered as a continuous variable. We performed all analyses with SAS version 9.3. We considered 95% confidence intervals of odds ratios that excluded 1 to be statistically significant.
RESULTS
For our primary analyses, we identified 8,870 knees (4,435 individuals) in the OAI that had data available at baseline and at one or more follow-up visits. This sample was primarily female and on average 61 (SD=9) years of age and overweight (BMI=28.6 (4.8) kg/m2) at baseline: bilateral radiographic osteoarthritis (age=63 (9) years, BMI=30.4 (5.0) kg/m2), no radiographic osteoarthritis (age=59 (9) years, BMI=27.0 (4.4) kg/m2), unilateral radiographic osteoarthritis (age=62 (9) years, BMI=28.3 (4.2) kg/m2). Approximately, one-third of knees had reported chronic knee symptoms or had a WOMAC pain score ≥3 at baseline. For our secondary and post hoc analyses, we identified 2,694 knees among 1,443 eligible individuals with bilateral radiographic KOA at baseline, 2,408 knees among 1,347 individuals without radiographic KOA throughout the study period, and 653 knees with unilateral KOA in the contralateral knee. The baseline characteristics of these secondary samples are presented in Table 1. Within the full cohort, 875 new knee injuries occurred between OAI baseline and the 48-month follow-up visit among 772 (8.7%) knees. Overall, 683 (7.7%) knees had one reported knee injury, 77 (0.9%) knees had two reported injuries, and 12 (0.1%) knees had three or four reported injuries during the observation period. Of the 875 new knee injuries, 335 new injuries occurred among those with radiographic KOA at baseline, 153 new injuries occurred among those without radiographic KOA, and 46 new injuries occurred among those with unilateral KOA.
Table 1.
Descriptive Baseline Characteristics of the Study Knees in Primary and Secondary Analyses
| Full OAI Cohort (n = 8,870 knees) | Bilateral ROA (n = 2,694 knees) | No ROA (n = 2,408 knees) | Unilateral ROA (n = 653 knees) | |
|---|---|---|---|---|
| Females (n (%)) | 5182 (58.4%) | 1676 (62.2%) | 1346 (55.9%) | 320 (49.0%) |
| Chronic knee symptoms (n (%))1 | 3221 (36.3%) | 1264 (46.9%) | 639 (26.6%) | 146 (22.4%) |
| WOMAC knee pain score ≥ 3 (n (%))1 | 2916 (32.9%) | 1221 (45.3%) | 512 (21.3%) | 120 (18.4%) |
Note. ROA = radiographic osteoarthritis (Kellgren-Lawrence Grade ≥ 2).
Frequent and WOMAC knee pain are reported for both knees within a participant for the Full OAI cohort and among those with bilateral ROA or No ROA because both knees could contribute an outcome. Frequent and WOMAC knee pain are reported for the knee without ROA.
In our primary analyses, we found that knees with reported chronic knee symptoms were 1.84 times as likely to experience an ipsilateral knee injury in the following 12 months (Table 2) compared with knees without chronic knee symptoms. Similarly, knees with greater knee pain severity (WOMAC pain score ≥3) were almost twice as likely to have an ipsilateral knee injury in the following 12 months (Table 3). Contralateral knee pain (chronic knee symptoms or pain severity) was not associated with a knee injury in the following 12 months. Knees with a history of knee injury in the ipsilateral or contralateral knee were more likely to have a new knee injury (history of ipsilateral knee injury OR=1.81; history of contralateral knee injury OR=1.43, Table 2). Similar findings were observed when adjusting for knee pain severity instead of chronic knee symptoms (Table 3).
Table 2.
Chronic knee symptoms and history of injury predict a new knee injury within 12 months
| Frequency of Injuries/Total Observations | Unadjusted Odds Ratio for Injury | Adjusted* Odds Ratio for Injury | |
|---|---|---|---|
| Full Osteoarthritis Initiative (4,435 participants, 875 injuries) | |||
| No Chronic Ipsilateral Knee Symptoms | 422/21312 (2.0%) | Reference | Reference |
| Chronic Ipsilateral Knee Symptoms | 453/10118 (4.5%) | 2.09 (1.82, 2.40) | 1.84 (1.57, 2.16) |
| No Chronic Contralateral Knee Symptoms | 502/21311 (2.4%) | Reference | Reference |
| Chronic Contralateral Knee Symptoms | 373/10119 (3.7%) | 1.52 (1.32, 1.75) | 1.02 (0.87, 1.20) |
| No History of Ipsilateral Knee Injury | 443/22275 (2.0%) | Reference | Reference |
| History of Ipsilateral Knee Injury | 432/9155 (4.7%) | 2.09 (1.81, 2.41) | 1.80 (1.56, 2.09) |
| No History of Contralateral Knee Injury | 518/22275 (2.3%) | Reference | Reference |
| History of Contralateral Knee Injury | 357/9155 (3.9%) | 1.63 (1.41, 1.89) | 1.43 (1.23, 1.66) |
| Bilateral ROA (1,347 participants, 335 injuries) | |||
| No Chronic Ipsilateral Knee Symptoms | 123/5324 (2.3%) | Reference | Reference |
| Chronic Ipsilateral Knee Symptoms | 212/4177 (5.1%) | 2.00 (1.59, 2.52) | 1.78 (1.37, 2.30) |
| No Chronic Contralateral Knee Symptoms | 147/5323 (2.8%) | Reference | Reference |
| Chronic Contralateral Knee Symptoms | 188/4178 (4.5%) | 1.56 (1.24, 1.96) | 1.09 (0.85, 1.41) |
| No History of Ipsilateral Knee Injury | 153/6198 (2.5%) | Reference | Reference |
| History of Ipsilateral Knee Injury | 182/3303 (5.5%) | 1.89 (1.49, 2.39) | 1.65 (1.29, 2.10) |
| No History of Contralateral Knee Injury | 168/6198 (2.7%) | Reference | Reference |
| History of Contralateral Knee Injury | 167/3303 (5.1%) | 1.82 (1.44, 2.32) | 1.63 (1.28, 2.09) |
| No ROA at All Visits (1,204 participants, 153 injuries) | |||
| No Chronic Ipsilateral Knee Symptoms | 100/7460 (1.3%) | Reference | Reference |
| Chronic Ipsilateral Knee Symptoms | 53/2091 (2.5%) | 1.77 (1.25, 2.50) | 1.62 (1.07, 2.45) |
| No Chronic Contralateral Knee Symptoms | 110/7461 (1.5%) | Reference | Reference |
| Chronic Contralateral Knee Symptoms | 43/2090 (2.1%) | 1.37 (0.95, 1.97) | 1.01 (0.66, 1.56) |
| No History of Ipsilateral Knee Injury | 90/7333 (1.2%) | Reference | Reference |
| History of Ipsilateral Knee Injury | 63/2218 (2.8%) | 2.11 (1.50, 2.97) | 2.00 (1.39, 2.86) |
| No History of Contralateral Knee Injury | 107/7333 (1.5%) | Reference | Reference |
| History of Contralateral Knee Injury | 46/2218 (2.1%) | 1.39 (0.95, 2.02) | 1.19 (0.81, 1.75) |
In addition to the variables indicated above each model was adjusted for sex, age, and body mass index at each visit. Bold = significant odds ratios.
Table 3.
Knee pain severity and history of injury predict a new knee injury within 12 months
| Frequency of Injuries/Total Observations | Unadjusted Odds Ratio for Injury | Adjusted* Odds Ratio for Injury | |
|---|---|---|---|
| Full Osteoarthritis Initiative (4,435 participants, 877 injuries) | |||
| No Ipsilateral Knee Pain (WOMAC ≤ 2) | 441/22188 (2.0%) | Reference | Reference |
| Ipsilateral Knee Pain (WOMAC ≥ 3) | 436/9292 (4.7%) | 2.25 (1.96, 2.59) | 1.94 (1.66, 2.26) |
| No Contralateral Knee Pain (WOMAC ≤ 2) | 536/22187 (2.4%) | Reference | Reference |
| Contralateral Knee Pain (WOMAC ≥ 3) | 341/9293 (3.7%) | 1.47 (1.27, 1.70) | 0.98 (0.84, 1.15) |
| No History of Ipsilateral Knee Injury | 444/22321 (2.0%) | Reference | Reference |
| History of Ipsilateral Knee Injury | 433/9159 (4.7%) | 2.09 (1.81, 2.41) | 1.76 (1.52, 2.05) |
| No History of Contralateral Knee Injury | 518/22321 (2.3%) | Reference | Reference |
| History of Contralateral Knee Injury | 359/9159 (3.9%) | 1.64 (1.42, 1.91) | 1.44 (1.23, 1.67) |
| Bilateral ROA (1,347 participants, 335 injuries) | |||
| No Ipsilateral Knee Pain (WOMAC ≤ 2) | 124/5533 (2.3%) | Reference | Reference |
| Ipsilateral Knee Pain (WOMAC ≥ 3) | 211/4072 (5.2%) | 2.15 (1.70, 2.71) | 1.90 (1.47, 2.45) |
| No Contralateral Knee Pain (WOMAC ≤ 2) | 156/5433 (2.9%) | Reference | Reference |
| Contralateral Knee Pain (WOMAC ≥ 3) | 179/4072 (4.4%) | 1.46 (1.16, 1.83) | 1.01 (0.78, 1.30) |
| No History of Ipsilateral Knee Injury | 153/6201 (2.5%) | Reference | Reference |
| History of Ipsilateral Knee Injury | 182/3304 (5.5%) | 1.89 (1.49, 2.39) | 1.64 (1.28, 2.09) |
| No History of Contralateral Knee Injury | 168/6201 (2.7%) | Reference | Reference |
| History of Contralateral Knee Injury | 167/3304 (5.1%) | 1.83 (1.44, 2.32) | 1.66 (1.29, 2.12) |
| No ROA at All Visits (1,204 participants, 154 injuries) | |||
| No Ipsilateral Knee Pain (WOMAC ≤ 2) | 111/7866 (1.4%) | Reference | Reference |
| Ipsilateral Knee Pain (WOMAC ≥ 3) | 43/1723 (2.5%) | 1.69 (1.16, 2.45) | 1.40 (0.93, 2.10) |
| No Contralateral Knee Pain (WOMAC ≤ 2) | 116/7866 (1.5%) | Reference | |
| Contralateral Knee Pain (WOMAC ≥ 3) | 38/1723 (2.2%) | 1.47 (1.00, 2.15) | 1.19 (0.78, 1.82) |
| No History of Ipsilateral Knee Injury | 90/7366 (1.2%) | Reference | |
| History of Ipsilateral Knee Injury | 64/2223 (2.9%) | 2.13 (1.51, 3.00) | 2.00 (1.39, 2.87) |
| No History of Contralateral Knee Injury | 107/7366 (1.5%) | Reference | |
| History of Contralateral Knee Injury | 47/2223 (2.1%) | 1.41 (0.97, 2.05) | 1.18 (0.81, 1.74) |
In addition to the variables indicated above each model was adjusted for sex, age, and body mass index at each visit. Bold = significant odds ratios.
These findings were supported in our secondary and post hoc analyses. One exception was that a history of a contralateral knee injury was not related with a new knee injury among those without radiographic osteoarthritis at baseline. Analyses among 653 participants with unilateral KOA were limited because only 46 injuries occurred. In unadjusted analyses, we found that knees without radiographic osteoarthritis – but with contralateral radiographic osteoarthritis – were more likely to have a new knee injury if they had chronic knee symptoms in either knee, severe knee pain in the ipsilateral knee, and a history of knee injury in either knee (see Supplemental File, Tables 1 and 2).
We conducted several post hoc analyses by adjusting for potential confounders among the full cohort and they supported the primary results (see Supplemental File, Tables 3 and 4). The person-based analyses supported the primary results that an individual with knee pain (frequent [OR=1.69] or severe [OR=1.62]) or a history of injury (OR=1.88) was more likely to have a new knee injury in either knee (see Supplemental File, Tables 5 and 6). Finally, WOMAC knee pain as a continuous predictor (scale 0 to 20) was associated with a new knee injury (OR=1.11, per one point increase in WOMAC pain score; see Supplemental File, Table 7).
DISCUSSION
Despite knee injuries being associated with a greater risk for early-onset osteoarthritis (3) and accelerated KOA (4) very little is known about possible risk factors for injuries among adults over 45 years of age. We found that among knees with or without KOA that a history of knee injury and ipsilateral knee pain are associated with new knee injuries. These findings were consistent when we defined pain based on severity or the presence of chronic knee symptoms.
Since knee pain, irrespective of the presence of radiographic osteoarthritis, is associated with a greater risk of injuries it may be beneficial to determine if aggressive treatment of knee pain is an important intervention to prevent future knee injuries. If so, then it may be advisable for clinicians to manage knee pain, even in the absence of radiographic osteoarthritis, based on KOA treatment guidelines. Most osteoarthritis treatment guidelines (35) advocate managing knee symptoms with a pharmacological intervention as well as exercise programs, which could include goals for pain modification and injury/fall prevention.
These exercise programs could also be beneficial if applied to individuals with a history of knee injury. We found that a history of knee injury, in either knee, was associated with a new knee injury. This was consistent among knees with and without KOA; however, a history of contralateral knee injury was not associated with new injuries among knees without radiographic KOA. A history of knee injury could be related to bilaterally altered biomechanics (36–39) or neuromuscular control (40–42), that predisposes the ipsilateral or contralateral knee to a new injury. For example, individuals with a history of an ACL injury have altered biomechanics and neuromuscular control in the injured and uninjured knees, both of which could predispose the knees to a future ACL injury (38, 40). This may explain why an injury in either knee could increase the risk of a new injury. Furthermore, knee pain in either knee was associated with a new injury in the unadjusted analyses. However, when we combine all the variables into the model contralateral knee pain is no longer associated with new knee injuries. This could be because ipsilateral knee pain or a history of injury in either knee is more relevant when assessing risk of a new knee injury. Hence, knees with a history of knee injury, with or without osteoarthritis, may benefit from exercise programs that incorporate neuromuscular training with a goal of preventing injuries or falls.
Injury prevention programs are commonly advocated for young physically active individuals because these programs improve performance, reduce the risk of injuries, and may subsequently reduce the risk of osteoarthritis. This last point is based on consistent evidence that knee injuries increase the risk of KOA (1–3). We previously demonstrated that among adults over 45 years of age that knee injuries are associated with incident KOA, particularly accelerated KOA (4). Based on the current analyses, we found that knee pain and a history of knee injury increases the risk of a knee injury among adults with and without radiographic osteoarthritis. This supports a hypothesis that some knees may experience a dangerous cycle of injuries, pain, and structural progression (see Figure 1). Prior to the onset of KOA (accelerated or common osteoarthritis) ipsilateral knee pain and a history of injury may be risk factors for a new injury that could trigger the onset of accelerated or common KOA, which are associated with knee symptoms. Once a patient has osteoarthritis we found that a history of knee injury or ipsilateral knee pain, which could be attributable to osteoarthritis, are still risk factors for a new knee injury. This new injury could exacerbate osteoarthritis progression and increase knee symptoms. We should strive to avoid this vicious cycle. Therefore, among older adults who report knee pain or a history of knee injury we should explore injury/fall prevention strategies.
Figure 1.
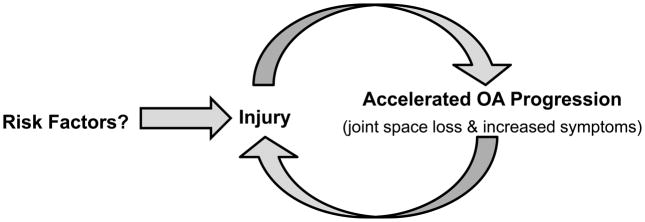
A Vicious Cycle of Injury and Accelerated Knee Osteoarthritis
Despite evidence that knee pain and a history of knee injury are associated with a greater risk for knee injuries there are a few key limitations. Firstly, the current study could not identify the underlying cause of knee pain (e.g., referred hip pain, patellofemoral lesions, tendinopathy, pre-radiographic degenerative changes). Furthermore, it is unclear if the knee had pain immediately prior to the new injury. Despite these limitations, we observed an association between knee pain and knee injuries. Interestingly, we found similar associations between pain and injuries among those with and without radiographic osteoarthritis. Prior research has indicated that knee pain was associated with falls (8–10, 13), even when most (>80%) of the individuals with knee pain had no clinician-diagnosed KOA (14). This highlights the importance of knee pain as a risk factor for knee injuries irrespective of whether or not KOA was present. Some sources of knee pain (e.g., patellofemoral pathology, ligamentous instability, effusion) may be more likely alter proprioception (12) or increase the risk of subsequent injuries than other sources of pain. Future research that clarifies the source of the knee pain may help us understand the possible link between knee pain and subsequent injuries and ultimately lead to better injury prevention strategies.
It would also be beneficial to understand which injuries increase the risk of subsequent injuries and which new injuries are occurring. We could not address these important questions with existing data within the OAI. Despite not knowing the source of the knee pain or the type of injury this study represents an important first step in understanding the association between knee pain, history of knee injury, and new knee injuries. Future studies could also pursue this research in population-based cohorts but these findings will likely be confirmed since they complement the existing literature about the association between knee pain and falls (8–10, 13) and findings among younger physically active individuals (15–17).
In conclusion, we found that self-reported knee pain and a history of knee injury are associated with a greater risk for a new knee injury among knees with or without KOA. Hence, some knees may experience a dangerous cycle of injuries, pain, and structural progression. Since knee injuries are a key risk factor for KOA it may be ideal to test the benefit of implementing injury prevention strategies among adults with knee pain or a history of knee injuries. This may entail treatment strategies to reduce knee pain as well as exercise programs that aim to promote neuromuscular control and reduce the risk of injury/falls (8–10).
Supplementary Material
Acknowledgments
Sources of Support: These analyses were supported by grants from the National Institute of Health (Eaton: 268201000020C-1-0-1 and Driban: 1R01AR065977-01A1). The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. Dr. Lo is supported by K23 AR062127, an NIH/NIAMS funded mentored award. This work is also supported in part with resources at the VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (#CIN 13-413), at the Michael E. DeBakey VA Medical Center, Houston, TX. This manuscript does not reflect the views of the US government or the Veterans Administration.
References
- 1.Muthuri SG, McWilliams DF, Doherty M, Zhang W. History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthritis Cartilage. 2011;19:1286–93. doi: 10.1016/j.joca.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41(8):1343–55. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 3.Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20:739–44. doi: 10.1097/01.bot.0000246468.80635.ef. [DOI] [PubMed] [Google Scholar]
- 4.Driban JB, Eaton CB, Lo GH, Ward RJ, Lu B, McAlindon TE. Association of knee injuries with accelerated knee osteoarthritis progression: data from the Osteoarthritis Initiative. Arthritis Care Res. 2014;66:1673–9. doi: 10.1002/acr.22359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeng C, Gao SG, Wei J, Yang TB, Cheng L, Luo W, et al. The influence of the intercondylar notch dimensions on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:804–15. doi: 10.1007/s00167-012-2166-4. [DOI] [PubMed] [Google Scholar]
- 6.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–5. doi: 10.1016/j.arthro.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Alentorn-Geli E, Mendiguchia J, Samuelsson K, Musahl V, Karlsson J, Cugat R, et al. Prevention of anterior cruciate ligament injuries in sports. Part I: systematic review of risk factors in male athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22:3–15. doi: 10.1007/s00167-013-2725-3. [DOI] [PubMed] [Google Scholar]
- 8.Muraki S, Akune T, Ishimoto Y, Nagata K, Yoshida M, Tanaka S, et al. Risk factors for falls in a longitudinal population-based cohort study of Japanese men and women: The ROAD Study. Bone. 2013;52:516–23. doi: 10.1016/j.bone.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Arden NK, Crozier S, Smith H, Anderson F, Edwards C, Raphael H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Care & Research. 2006;55:610–5. doi: 10.1002/art.22088. [DOI] [PubMed] [Google Scholar]
- 10.Foley SJ, Lord SR, Srikanth V, Cooley H, Jones G. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthritis Cartilage. 2006;14:533–9. doi: 10.1016/j.joca.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Dore AL, Golightly YM, Mercer VS, Shi XA, Renner JB, Jordan JM, et al. Lower limb osteoarthritis and the risk of falls in a community-based longitudinal study of adults with and without osteoarthritis. Arthritis Care Res. 2014 doi: 10.1002/acr.22499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Felson DT, Gross KD, Nevitt MC, Yang M, Lane NE, Torner JC, et al. The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum. 2009;61:1070–6. doi: 10.1002/art.24606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Nakamura K, et al. Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis Care Res. 2011;63:1425–31. doi: 10.1002/acr.20562. [DOI] [PubMed] [Google Scholar]
- 14.Arden NK, Crozier S, Smith H, Anderson F, Edwards C, Raphael H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Rheum. 2006;55:610–5. doi: 10.1002/art.22088. [DOI] [PubMed] [Google Scholar]
- 15.Oates KM, Van Eenenaam DP, Briggs K, Homa K, Sterett WI. Comparative injury rates of uninjured, anterior cruciate ligament-deficient, and reconstructed knees in a skiing population. Am J Sports Med. 1999;27:606–10. doi: 10.1177/03635465990270051001. [DOI] [PubMed] [Google Scholar]
- 16.Faude O, Junge A, Kindermann W, Dvorak J. Risk factors for injuries in elite female soccer players. Br J Sports Med. 2006;40:785–90. doi: 10.1136/bjsm.2006.027540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rugg CM, Wang D, Sulzicki P, Hame SL. Effects of prior knee surgery on subsequent injury, imaging, and surgery in NCAA collegiate athletes. Am J Sports Med. 2014;42:959–64. doi: 10.1177/0363546513519951. [DOI] [PubMed] [Google Scholar]
- 18.Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196–200. doi: 10.1177/03635465010290021301. [DOI] [PubMed] [Google Scholar]
- 19.Hägglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40:767–72. doi: 10.1136/bjsm.2006.026609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun K, Song J, Lee J, Chang RW, Eaton CB, Ehrlich-Jones L, et al. Relationship of Meeting Physical Activity Guidelines With Health-Related Utility. Arthritis Care Res. 2014;66:1041–7. doi: 10.1002/acr.22262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis Rheum. 2011;63:3372–82. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. [Accessed April 1, 2015];Osteoarthritis Iniatiive [Internet] Available from: http://oai.epi-ucsf.org.
- 23.Prevalence and impact of chronic joint symptoms--seven states, 1996. MMWR Morb Mortal Wkly Rep. 1998;(47):345–51. [PubMed] [Google Scholar]
- 24.Mili F, Helmick CG, Zack MM. Prevalence of arthritis: analysis of data from the US Behavioral Risk Factor Surveillance System, 1996–99. J Rheumatol. 2002;29:1981–8. [PubMed] [Google Scholar]
- 25.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 26.Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:507–15. doi: 10.1016/j.joca.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 27.Tanamas SK, Wluka AE, Davies-Tuck M, Wang Y, Strauss BJ, Proietto J, et al. Association of weight gain with incident knee pain, stiffness, and functional difficulties: a longitudinal study. Arthritis Care Res. 2013;65:34–43. doi: 10.1002/acr.21745. [DOI] [PubMed] [Google Scholar]
- 28.O’Reilly SC, Muir KR, Doherty M. Knee pain and disability in the Nottingham community: association with poor health status and psychological distress. Br J Rheumatol. 1998;37:870–3. doi: 10.1093/rheumatology/37.8.870. [DOI] [PubMed] [Google Scholar]
- 29.Andersen RE, Crespo CJ, Ling SM, Bathon JM, Bartlett SJ. Prevalence of significant knee pain among older Americans: results from the Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 1999;47:1435–8. doi: 10.1111/j.1532-5415.1999.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 30.Peat G, Bergknut C, Frobell R, Joud A, Englund M. Population-wide incidence estimates for soft tissue knee injuries presenting to healthcare in southern Sweden: data from the Skane Healthcare Register. Arthritis Res Ther. 2014;16:R162. doi: 10.1186/ar4678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nilstad A, Andersen TE, Bahr R, Holme I, Steffen K. Risk factors for lower extremity injuries in elite female soccer players. Am J Sports Med. 2014;42:940–8. doi: 10.1177/0363546513518741. [DOI] [PubMed] [Google Scholar]
- 32.Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Fellander-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40:1808–13. doi: 10.1177/0363546512449306. [DOI] [PubMed] [Google Scholar]
- 33.Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD. Epidemiology of 6. 6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med. 2012;19:378–85. doi: 10.1111/j.1553-2712.2012.01315.x. [DOI] [PubMed] [Google Scholar]
- 34.Jones JC, Burks R, Owens BD, Sturdivant RX, Svoboda SJ, Cameron KL. Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athl Train. 2012;47:67–73. doi: 10.4085/1062-6050-47.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43:701–12. doi: 10.1016/j.semarthrit.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 36.Scanlan SF, Chaudhari AM, Dyrby CO, Andriacchi TP. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech. 2010;43:1817–22. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wexler G, Hurwitz DE, Bush-Joseph CA, Andriacchi TP, Bach BR., Jr Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop Relat Res. 1998;348:166–75. [PubMed] [Google Scholar]
- 38.Goerger BM, Marshall SW, Beutler AI, Blackburn JT, Wilckens JH, Padua DA. Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP-ACL study. Br J Sports Med. 2015;49:188–95. doi: 10.1136/bjsports-2013-092982. [DOI] [PubMed] [Google Scholar]
- 39.Hart JM, Ko JW, Konold T, Pietrosimone B. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech (Bristol, Avon) 2010;25:277–83. doi: 10.1016/j.clinbiomech.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 40.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45:87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swanik CB, Lephart SM, Giraldo JL, Demont RG, Fu FH. Reactive muscle firing of anterior cruciate ligament-injured females during functional activities. J Athl Train. 1999;34:121–9. [PMC free article] [PubMed] [Google Scholar]
- 42.Goetschius J, Kuenze CM, Saliba S, Hart JM. Reposition acuity and postural control after exercise in anterior cruciate ligament reconstructed knees. Med Sci Sports Exerc. 2013;45:2314–21. doi: 10.1249/MSS.0b013e31829bc6ae. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


