Abstract
Background
This case study examines the influence of an Ankle Foot Orthosis Footwear Combination (AFO-FC) on musculotendon lengths and gait kinematics and kinetics after right thrombotic stroke resulting in left hemiplegia.
Case Description and Methods
Gait analysis was performed over three visits where the subject walked with an AFO-FC with two shank-to-vertical alignments, a posterior leaf spring AFO (PLS AFO), and shoes alone. Musculotendon lengths, kinematics, and kinetics were evaluated for each condition.
Finding and Outcomes
The AFO-FC improved walking speed and non-paretic kinematics compared to the PLS AFO and shoes alone. The operating length of the paretic gastrocnemius decreased with the AFO-FC improving knee kinematics in swing, but not stance.
Conclusion
Musculoskeletal modeling demonstrated that AFO-FCs altered gastrocnemius operating length during post-stroke hemiplegic gait. Using these tools to evaluate muscle operating lengths can provide insight into underlying mechanisms that may improve gait and guide future AFO-FC design.
Clinical Relevance
Modeling musculotendon operating length during movement has the potential to provide additional information about how AFO-FCs effect stiff muscles and improve mobility after stroke.
Keywords: ankle foot orthoses, musculoskeletal modeling, muscle length, gait, tuning
Background
Stroke negatively affects mobility with 50% of stroke survivors achieving only a limited level of functional ambulation.1 To achieve better outcomes we need an improved understanding of the mechanisms that hinder mobility and better methods for prescribing and optimizing function of assistive devices. Ankle Foot Orthoses (AFOs) are an assistive device commonly used to improve gait after stroke, with many designs available to provide support and alignment, compensate for muscle weakness, and help prevent secondary musculoskeletal deformities. Recently, Ankle Foot Orthosis Footwear Combinations (AFO-FCs) have been suggested to improve gait for individuals with neuromuscular problems.2,3,4,5 AFO-FCs comprise a rigid, non-articulated AFO set at an ankle angle (AA) predicated on muscle length6, a shank-to-vertical angle (SVA) modified by intrinsic or extrinsic heel wedges to center the knee over the middle of the foot during midstance7, and footwear modified to allow stance phase rollover given restriction of ankle and possibly metatarsophalangeal joint motion.8 By dynamically adjusting the SVA and rocker profile of the footwear, orthotists can “tune” the sagittal plane orientation of the vertical ground reaction force vector with respect to the knee and hip during terminal stance and pre-swing.2,9 Tuning an AFO-FC was shown to improve walking speed, knee kinematics, and knee pain in an individual after stroke.10
The efficacy of AFO-FCs is thought to be related to musculotendon dynamics during gait.9 Contracture, spasticity, and increased tone are common after stroke and can contribute to pathologic gait patterns.11 For example, contracture or spasticity of the gastrocnemius, which crosses both the knee and ankle, may contribute to reduced push-off in terminal stance, increased knee hyperextension, and inadequate knee flexion in swing.12,13 Tuning an AFO-FC to reduce the operating length of the gastrocnemius during gait may reduce the effect of contracture and spasticity, improving knee kinematics. Operating length is defined as the length of the muscle-tendon unit from origin to insertion during movement. Orthotists can adjust the ankle angle of the AFO to alter the operating length of the gastrocnemius or other muscles during activities of daily living such as gait.9 However, changes in muscle operating lengths with AFO-FCs are unknown. Understanding the effect of AFO-FCs on muscle operating lengths may inform orthotic prescription, design, and tuning.
This case study evaluated whether tuning an AFO-FC altered muscle operating length, contributing to improved kinematics during gait. We evaluated a single subject with left hemiplegia post-stroke who presented with gastrocnemius contracture and a stiff-knee gait. Evaluations were conducted over three visits while walking with shoes alone, a posterior leaf spring AFO (PLS AFO), and an AFO-FC with two shank-to-vertical alignments. We hypothesized that the AFO-FC would decrease gastrocnemius operating length and improve knee kinematics during gait.
Case Description and Methods
Subject
A 56 year old male (height = 190cm, weight = 88.5kg) who sustained a right middle cerebral artery injury with subsequent left hemiplegia was first evaluated using instrumented gait analysis eleven months post-stroke. Clinical exam indicated that the subject had restricted passive ankle range of motion on the left: 10° dorsiflexion (knee at 90° flexion) and 5° plantar flexion (knee at 0°). The left knee had 5° hyperextension. The university's Institutional Review Board approved this study and informed consent was obtained from the subject prior to participation.
Orthotic conditions
The subject visited the motion analysis laboratory on three occasions. As part of his preceding clinical care the subject had been provided an off-the-shelf polypropylene PLS AFO. At the first visit (11 months post-stroke), his gait was assessed with the PLS AFO. The subject was also fitted with a custom polypropylene AFO-FC with an ankle angle of 8° plantar flexion (based on passive ankle range of motion with the knee extended) and an SVA of 15° (Figure 1). The AFO-FC was tuned by a certified orthotist with over 20 years of experience in the orthotic management of individuals post-stroke. The subject wore this AFO-FC full-time for 5 months between the first and second visit. At the second visit (16 months post-stroke), the subject's gait was evaluated with the AFO-FC with SVA of 15°.
Figure 1.
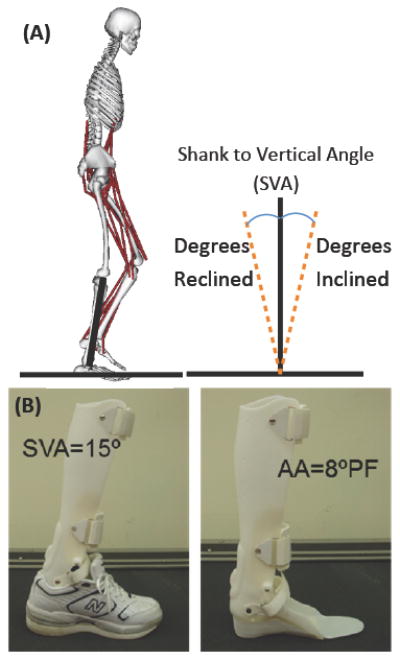
(A) Shank-to-vertical angle (SVA) is defined as being either reclined or inclined. During normal walking, the SVA at midstance is 10° inclined. (B) Alignment of the AFO-FC showing Ankle Angle set at 8° plantar flexion and SVA of 15° inclination when the orthosis is placed inside a modified shoe.
Based upon this analysis, the AFO-FC was adjusted (i.e., re-tuned) by the orthotist, reducing the SVA from 15° to 12° by removing material from beneath the heel of the shoe. This was done to improve the sagittal plane orientation of the vertical ground reaction force vector with respect to the knee joint such that greater knee extension might be achieved in terminal stance. The subject returned 1 month later (17 months post-stroke) to evaluate the re-tuned AFO-FC with SVA of 12°, which was worn full-time during the intervening month. During this final visit, the subject's gait was also evaluated with shoes alone for comparison.
It should be noted that the subject walked with a quad cane when using the PLS AFO and shoes alone but ambulated without an assistive device when the AFO-FC was worn. At the first visit, the subject refused to walk with shoes alone, which is why the PLS AFO was used as the comparison condition. At the final visit, the subject agreed to walk with shoes alone.
Gait analysis
An eight-camera real-time motion capture system (Motion Analysis Corporation, Santa Rosa, CA) was used to acquire three-dimensional marker data at 120 Hz. Markers were placed on the subject by the same investigator for all analyses based on a modified Helen-Hayes marker set.14 Ground reaction forces were acquired at 960 Hz using six force plates (Advanced Mechanical Technology Inc., Watertown, MA).
Musculoskeletal modeling
OpenSim, an open-source musculoskeletal modeling and simulation software platform15, was used to calculate gait kinematics and estimate musculotendon lengths. A generic musculoskeletal model with 19 degrees of freedom and 92 muscles16 was scaled to the subject based upon anatomical landmarks. For each trial, inverse kinematics was used to calculate joint angles, minimizing the distance between the three-dimensional marker trajectories from gait analysis and the virtual markers placed on the model.
Musculotendon operating lengths of major lower-limb muscles were calculated from the distance of each muscle's path from origin to insertion during the gait cycle. Muscle paths are based upon cadaveric and imaging data and have previously been used to evaluate muscle lengths and velocities in unimpaired individuals and individuals with neurological disorders.17 To facilitate comparison with unimpaired individuals, musculotendon lengths were normalized by the length of each muscle with the hip, knee, and ankle joints in the anatomic position. Joint moments were calculated using inverse dynamics. Joint kinematics, kinetics, and musculotendon operating lengths were normalized to 101 points for each gait cycle and averaged over a minimum of 9 gait cycles for each condition.
Musculotendon operating lengths have previously been shown to be dependent on walking speed.18 Hence, results were compared to previously collected kinematics and musculotendon lengths of a group of unimpaired subjects walking at very slow speeds (N=8, data available at: https://simtk.org/home/mspeedwalksims).19
Findings and Outcomes
Compared to unimpaired individuals, the subject walked with inadequate hip extension, excessive stance phase knee flexion, reduced stance phase ankle dorsiflexion, and reduced swing phase knee flexion on the paretic side when wearing shoes alone or the PLS AFO (Figures 2 A, B, C). On the non-paretic side, hip, knee, and ankle kinematics were also abnormal with shoes alone and PLS AFO, with a prolonged support time (Figures 2 D, E, F). For the same conditions (shoes alone and PLS-AFO), the paretic side hamstrings operated at near normal maximum length at initial contact (Figure 3A, solid and dotted gray lines) while paretic side gastrocnemius length (Figure 3B, solid and dotted gray lines) was reduced during stance phase compared to unimpaired gait. Maximum paretic side gastrocnemius length in terminal stance was similar to the maximum length measured during passive ankle dorsiflexion in the clinical exam (Figure 3B, red horizontal line).
Figure 2.

Average sagittal plane kinematics at the hip, knee, and ankle of the non-paretic and paretic sides with shoes alone (solid gray lines), PLS AFO (dotted gray lines), AFO-FC with 15° SVA (dotted black line) and AFO-FC with 12° SVA (solid black lines) normalized to one gait cycle. The gray shaded band depicts the average ± one standard deviation of unimpaired gait at very slow speeds. Circles and vertical lines indicate toe-off for each condition for the subject with stroke and unimpaired individuals, respectively. Positive values of hip and knee angles are flexion and positive values of ankle angle are dorsiflexion.
Figure 3.
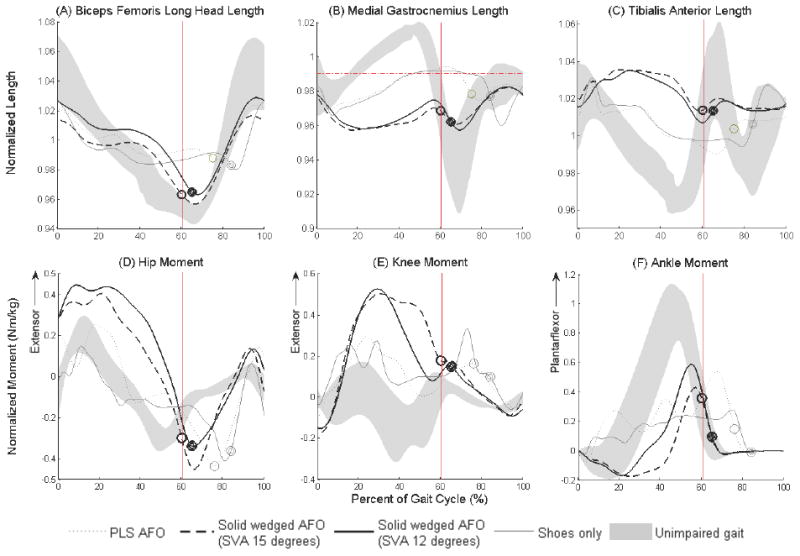
Average musculotendon operating length on the paretic side for the biceps femoris long head (A), medial gastrocnemius (B), and tibialis anterior (C) during trials with shoes alone (solid gray line), PLS AFO (dotted gray line), AFO-FC with SVA of 15° (dotted black line), and AFO-FC with SVA of 12° (solid black line) normalized to one gait cycle. The gray shaded band depicts the average ± one standard deviation of musculotendon operating lengths during very slow unimpaired gait. Circles and vertical lines indicate toe-off for each condition for the subject with stroke and unimpaired individuals, respectively. The horizontal red dotted line in (B) depicts gastrocnemius length at maximum ankle dorsiflexion with the knee extended. Musculotendon lengths were normalized by the length of each muscle in the anatomic position. Also shown are average sagittal plane internal joint moments at the hip (D), knee (E), and ankle (F) of the paretic side with shoes alone (solid gray lines), PLS AFO (dotted gray lines), AFO-FC with 15° SVA (dotted black line) and AFO-FC with 12° SVA (solid black lines) normalized to one gait cycle.
Paretic limb kinematics at the hip, knee and ankle improved with the AFO-FC at the second and third visits. The AFO-FC reduced support time and improved joint motion on the non-paretic side compared to gait with shoes alone and the PLS AFO. At the second visit, the AFO-FC with SVA of 15° reduced toe-off time from 88% to 76% of the gait cycle on the non-paretic side and 77% to 61% of the gait cycle on the paretic side. Knee range of motion remained less than unimpaired gait, but improved from 19.3° and 13.4° with shoes alone and the PLS AFO, respectively, to 26.1° in the AFO-FC with SVA of 12° at the final visit.
The AFO-FC altered musculotendon operating lengths and joint moments on the paretic side. In contrast to the shoes alone and PLS AFO conditions, the medial gastrocnemius did not exceed the maximum passive gastrocnemius length with the AFO-FCs because of the fixed plantar flexion angle. Although gastrocnemius operating length was reduced, paretic side knee extension during stance did not improve with the AFO-FCs (Figure 2B, solid and dotted black lines). However, changing the AFO-FCs SVA from 15° to 12° improved knee flexion during swing. Knee flexion during swing increased from 30.4° to 36.5° after retuning the AFO-FC. Hip flexion at heel contact improved from 14.1° to 18.8° with the retuned AFO-FC, but overall range of motion decreased. Reducing the AFO-FCs SVA from 15° to 12° also increased the internal ankle plantar flexor moment and decreased the internal knee extensor moment during terminal stance, helping to decrease the stiff-knee gait pattern.
Walking speed was also significantly improved with the AFO-FC. The subject's nondimensional velocity was 0.07 and 0.09 with the shoes alone and PLS AFO, respectively. With the initial AFO-FC, the nondimensional velocity was 0.21 and improved to 0.24 when the AFO-FC was retuned to an SVA of 12°. However, these velocities are still substantially less than the unimpaired subjects' very slow speed, which had an average nondimensionalized velocity of 0.54 ± 0.04 (Table 1).
Table 1.
Temporal-spatial and kinematic changes in gait with each condition.
| First visit (11 months post-stroke) | Second visit (16 months post-stroke) | Third visit (17 months post-stroke) | ||
|---|---|---|---|---|
| PLS AFO | AFO-FC (SVA 15°) | AFO-FC (SVA 12°) | Shoe only | |
| Stride Length (cm) | 45.5 | 72.8 | 76.0 | 47.3 |
| Nondimensional Velocity* | 0.09 | 0.21 | 0.24 | 0.07 |
| Cadence (steps/min) | 68.8 | 98.0 | 104.2 | 50.1 |
| Step Width (cm) | 27.7 | 23.7 | 23.7 | 32.8 |
| Paretic Toe Off Time (%) | 77 | 61 | 66 | 85 |
| Paretic Hip Range of Motion (°) | 17 | 16.4 | 13.4 | 18.1 |
| Paretic Knee Range of Motion (°) | 13.4 | 19.7 | 26.1 | 19.3 |
| Paretic Ankle Range of Motion (°) | 15.7 | 9.2 | 11.4 | 16.4 |
The nondimensional velocity normalizes walking velocity by . Where g is gravity and Lleg is subject leg length. PLS AFO=posterior leaf spring ankle foot orthosis; AFO-FC= ankle foot orthosis-footwear combination; SVA=shank-to-vertical angle.
Discussion
In this case study, we used musculoskeletal modeling to evaluate the influence of AFO-FCs on musculotendon lengths and gait kinematics and kinetics. Our results indicate that the AFO-FC reduced gastrocnemius operating length during gait and improved walking speed, stiff-knee gait, and non-paretic limb kinematics compared to both shoes alone and a PLS AFO. Given that PLS AFOs are designed primarily to assist swing phase ankle alignment, it was not surprising that stance phase kinematics and kinetics were similar to walking with shoes alone. We had hypothesized that a shortened gastrocnemius was contributing to impaired knee motion and that reducing gastrocnemius operating length during gait with an AFO-FC would improve knee kinematics. Our hypothesis was partially supported by our results: we demonstrated that the gastrocnemius was operating at its maximum length during gait with the PLS AFO and shoes alone; while the AFO-FC reduced gastrocnemius operating length and knee kinematics improved in swing, but not stance.
Sagittal plane joint moments provide insight into the mechanisms underlying changes in knee kinematics. First, since gastrocnemius operating length was reduced throughout the gait cycle to below the subject's maximum length based on clinical exam, a shortened gastrocnemius no longer contributed to inadequate dorsiflexion or excessive knee flexion in stance. However, reducing the effect of a stiff gastrocnemius does not directly translate to improved knee kinematics. In swing, maximum knee flexion is largely dependent upon ankle and knee moments in terminal stance. With the AFO-FCs, the subject had greater internal ankle plantar flexor and knee extensor moments in terminal stance than shoes alone (Figure 3 E and F), which helped improve knee flexion in swing. With the initial AFO-FC (SVA of 15°), the internal ankle plantar flexor moment increased in terminal stance, but there was also an excessive internal knee extensor moment. Reducing the SVA from 15° to 12° shifted the orientation of the ground reaction force such that the internal ankle plantar flexor moment increased and the internal knee extensor moment decreased, improving knee flexion in swing.20 This demonstrates the importance of tuning the SVA of AFO-FCs and that even a small change in SVA can have a dramatic effect on knee kinetics.
In stance, knee extension did not improve with the AFO-FCs, even though the gastrocnemius operating length was reduced. With shoes and the PLS AFO, the gastrocnemius was operating at its maximum length and likely contributed to inadequate ankle dorsiflexion and knee extension. While, the AFO-FC dramatically changed the dynamics of the ankle joint, a reduced gastrocnemius operating length did not translate to improved ankle and knee kinematics in stance. In unimpaired gait, the ankle plantar flexors play an important role in helping to extend the knee through dynamic coupling: ankle plantar flexion-knee extension couple.21,22 In an AFO-FC the ankle is held rigid and the ankle plantar flexor muscles can no longer contribute to knee extension acceleration. Furthermore, as SVA increases, the forward tilt of the shank causes greater knee flexion and increases the internal knee extensor moment required to maintain a stable posture. Additionally, increasing SVA shortens the foot lever, similar to high heels, creating a smaller effective moment arm about the ankle.20 These changes highlight the complex, interacting factors that must be considered when tuning orthoses.
Conclusion
This case study illustrates how musculoskeletal modeling can be used to evaluate the role of individual muscles during walking, informing orthotic design to improve gait. We quantified changes in musculotendon lengths, kinematics, and kinetics when wearing an AFO-FC. The AFO-FC reduced gastrocnemius length but did not improve knee extension in stance compared to shoes alone and the PLS AFO. However, overall gait improved with the AFO-FC, including faster walking speed and reduced stiff-knee gait. Further studies are needed to determine if changes in gastrocnemius operating length and effects on joint moments during gait are consistent across multiple subjects and evaluate differences between orthotic designs. We believe that finding the balance between optimizing musculotendon operating lengths and lower extremity joint moments can help improve orthotic designs.
Acknowledgments
We wish to thank Donald McGovern, CPO, for his orthotic expertise in this case study and Rebecca Stine, MS, for data collection and processing. We also acknowledge use of the Jesse Brown VA Medical Center Motion Analysis Research Laboratory.
Funding: This case study was funded by National Institutes of Health (NIH) under Grant No. K12HD073945 (Principle Investigator: Katherine Steele) and in part by the National Institute on Disability and Rehabilitation Research (NIDRR) of the U.S. Department of Education under Grant No. H133E080009 (Principle Investigators: Steven Gard and Stefania Fatone). The opinions contained in this publication are those of the grantee and do not necessarily reflect those of the Department of Education.
Footnotes
Conflict of interest: The authors declare no conflict of interest.
References
- 1.Wade DT, Hewer RL. Functional abilities after stroke: measurement, natural history and prognosis. J Neurol Neurosur Ps. 1987;50:177–82. doi: 10.1136/jnnp.50.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butler PB, Farmer SE, Stewart C, Jones PW, Forward M. The effect of fixed ankle foot orthoses in children with cerebral palsy. Disabil Rehabil Assist Technol. 2007;2(1):51–8. doi: 10.1080/17483100600662009. [DOI] [PubMed] [Google Scholar]
- 3.Jagadamma KC, Owen E, Coutts FJ, Herman J, Yirrell J, Mercer TH, et al. The effects of tuning an ankle-foot orthosis footwear combination on kinematics and kinetics of the knee joint of an adult with hemiplegia. Prosthet Orthot Int. 2010;34(3):270–6. doi: 10.3109/03093646.2010.503225. [DOI] [PubMed] [Google Scholar]
- 4.Owen E. Shank angle to floor measures of tuned ‘ankle-foot orthosis footwear combinations’ used with children with cerebral palsy, spina bifida and other conditions. Gait Posture. 2002;16:S132–3. [Google Scholar]
- 5.Butler PB, Nene AV. The biomechanics of fixed ankle foot orthoses and their potential in the management of cerebral palsied children. Physiotherapy. 1991;77:81–8. [Google Scholar]
- 6.Owen E. Proposed clinical algorithm for deciding the sagittal angle of the ankle in an ankle-foot orthosis footwear combination. Gait Posture. 2005;22S:38–9. [Google Scholar]
- 7.Owen E. A clinical algorithm for the design and tuning of ankle-foot orthosis footwear combinations (AFOFCs) based on shank kinematics. Gait Posture. 2005;22S:36–7.8. [Google Scholar]
- 8.Owen E. The point of ‘point-loading rockers’ in ankle-foot orthosis footwear combinations used with children with cerebral palsy, spina bifida and other conditions. Gait Posture. 2004;20S:S86. [Google Scholar]
- 9.Owen E. The importance of being earnest about shank and thigh kinematics especially when using ankle-foot orthoses. Prosthet Orthot Int. 2010;34(3):254–69. doi: 10.3109/03093646.2010.485597. [DOI] [PubMed] [Google Scholar]
- 10.Bowers R, Ross K. Development of a best practice statement on the use of ankle-foot orthoses following stroke in Scotland. Prosthet Orthot Int. 2010;34:245–53. doi: 10.3109/03093646.2010.486392. [DOI] [PubMed] [Google Scholar]
- 11.Olney SJ, Richards C. Hemiparetic gait following stroke. Part I: Characteristics. Gait Posture. 1996;4(2):136–48. [Google Scholar]
- 12.Katherine MS, Ajay S, Jennifer LH, Michael SS, Scott DL. Muscle contributions to support and progression during single-limb stance in crouch gait. J Biomech. 2010;43:2099–105. doi: 10.1016/j.jbiomech.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stauffer RN, Chao EY, Györy AN. Biomechanical gait analysis of the diseased knee joint. Clin Orthop Relat Res. 1977;126:246–55. [PubMed] [Google Scholar]
- 14.Kadaba MP, Ramakrishnan HK, Wooten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8(3):383–92. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 15.Delp SL, Anderson FC, Arnold AS, Loan P, Habib A, John CT, et al. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans Biomed Eng. 2007;54(11):1940–50. doi: 10.1109/TBME.2007.901024. [DOI] [PubMed] [Google Scholar]
- 16.Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Trans Biomed Eng. 1990;37(8):757–67. doi: 10.1109/10.102791. [DOI] [PubMed] [Google Scholar]
- 17.Arnold AS, Liu MQ, Schwartz MH, Ounpuu S, Delp SL. The role of estimating muscle-tendon lengths and velocities of the hamstrings in the evaluation and treatment of crouch gait. Gait Posture. 2006;23(3):273–81. doi: 10.1016/j.gaitpost.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal-Harding KJ, Schwartz MH, Delp SL. Variation of hamstrings lengths and velocities with walking speed. J Biomech. 2010;43(8):1522–6. doi: 10.1016/j.jbiomech.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu MQ, Anderson FC, Schwartz MH, Delp SL. Muscle contributions to support and progression over a range of walking speeds. J Biomech. 2008;41(15):3243–52. doi: 10.1016/j.jbiomech.2008.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas MC, Barbara C. The effects of heel height and ankle-foot-orthosis configuration on weight line location: A demonstration of principles. Orthotics Prosthet. 1976;30(4):43–6. [Google Scholar]
- 21.Zajac FE, Gordon ME. Determining muscle's force and action in multi-articular movement. Exerc Sport Sci Rev. 89(17):187–230. [PubMed] [Google Scholar]
- 22.Anderson FC, Arnold AS, Pandy MG, Goldberg SR, Delp SL. Human Walking. 3rd. Williams and Wilkins; 2006. Simulation of walking; pp. 195–210. [Google Scholar]


