To the Editor:
Choledochocele is a cystic dilatation of the intraduodenal portion of the common bile duct that can protrude into the duodenum. Although often classified as type III biliary cyst, choledochocele has distinctive demographic and anatomic features, and is associated with a lower risk of malignancy as compared to other types of choledochal cysts. Patients with this condition present with biliary colic, cholangitis, or pancreatitis.1,2 Until recently, transduodenal cyst excision with or without sphincterotomy had been the treatment of choice.3 At present, however, endoscopic sphincterotomy and cyst unroofing have become the treatment of choice.4 We present a case of choledochocele associated with acute pancreatitis that was treated with endoscopic sphincterotomy and cyst unroofing.
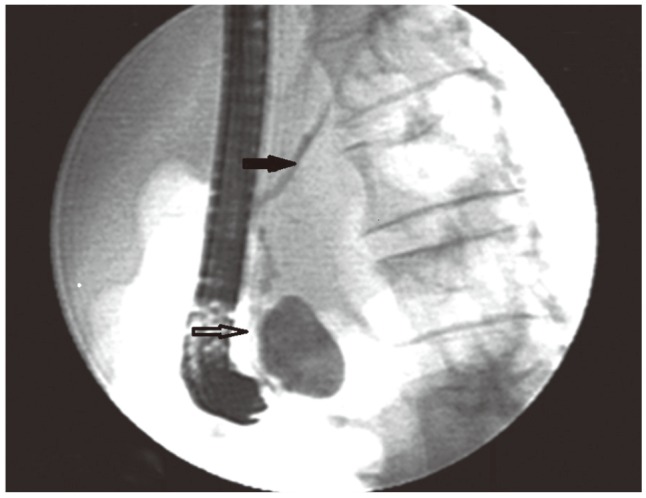
A 38-year-old woman with a 24-hour history of severe abdominal pain, nausea, and vomiting was admitted to our clinic. On physical examination, mild upper abdominal tenderness was observed. On admission, her amylase level was 3,262 IU/L (reference range, 25 to 125) and her C-reactive protein level was 64 mg/dL (reference range, 0 to 0.8). Transabdominal ultrasonography and magnetic resonance cholangiopancreatography (MRCP) revealed a dilated main pancreatic duct, mild peripancreatic fluid collection, and a cystic lesion 4 cm in diameter that was localized to the second portion of the duodenum. Furthermore, MRCP revealed that the cyst had the same intensity as the biliary tract and that the cyst communicated with the main pancreatic duct and common bile ducts (Fig. 1). Duodenoscopy revealed a soft and pedicular mass covered with normal duodenal mucosa, approximately 4×3×3 cm in size, in the medial wall of the duodenum. Cholangiography revealed an intraduodenal cyst communicating with the common bile duct and main pancreatic duct (Fig. 2). The patient had no other symptoms during the 6-month follow-up.
Fig. 1. A magnetic resonance cholangiopancreatography image showing that the cyst had the same intensity as the biliary tract and that the cyst communicated with the main pancreatic duct and common bile duct.
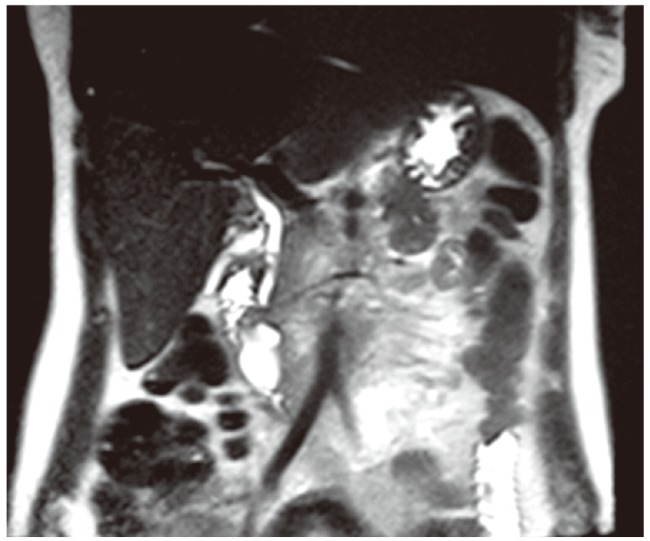
Fig. 2. An endoscopic retrograde cholangiopancreatography image showing communication between the cystic dilatation of the intraduodenal common bile duct (white arrow) and the pancreatic duct (black arrow).
In conclusion, choledochocele should be considered as a differential diagnosis of duodenal cystic lesion. Endoscopic unroofing may be considered as a simple and safe treatment option for choledochocele.
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Khandelwal C, Anand U, Kumar B, Priyadarshi RN. Diagnosis and management of choledochal cysts. Indian J Surg. 2012;74:29–34. doi: 10.1007/s12262-011-0388-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012;18:4801–4810. doi: 10.3748/wjg.v18.i35.4801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Can MF, Kaymakçioğlu N, Yağci G, Görgülü S, Tufan T. An adult choledochocele case presented with gastric outlet obstruction: a rare presentation. Turk J Gastroenterol. 2006;17:70–73. [PubMed] [Google Scholar]
- 4.Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol. 2014;12:196–203. doi: 10.1016/j.cgh.2013.04.037. [DOI] [PubMed] [Google Scholar]


