Abstract
Purpose
The purpose of this paper was to provide a description of the components of the PEDIATRIC PRO-SELF©: Pain Control Program.
Design and Methods
The Program, adapted from studies of this intervention in adults with cancer pain, was tested in two randomized clinical trials of acute pain management in pediatrics.
Results
Key strategies most effective for parents in the pediatric ambulatory surgery setting included use of an educational booklet and timer to facilitate adherence to the prescribed analgesic regimen, as well as interactive nursing support.
Practice Implications
The PEDIATRIC PRO-SELF©: Pain Control Program can be used with parents caring for children at home following tonsillectomy.
Search terms: Parent teaching, pediatric pain, postoperative pain, self-care, tonsillectomy
Education of parents in the pediatric ambulatory surgery setting focuses on the provision of information that enables the parent to anticipate events, to understand the meaning and purpose of these events, and to correct misinformation (LeRoy et al., 2003). Standard postoperative care instructions include key points for home care (e.g., diet, activity, incision care, pain management, when to contact the physician for problems, and follow-up appointment). However, the routine information provided on pain management is not adequate given the numerous reports on the undertreatment of postoperative pain in children following outpatient surgery (Gedaly-Duff & Ziebarth, 1994; Hamers & Abu-Saad, 2002; Helgadottir & Wilson, 2004; Homer, Swallow, & Semple, 2001; Huth & Broome, 2007; Sutters & Miaskowski, 1997; Vallee, Lafrenaye, Tetrault, Mayer, & Dorion, 2008; Warnock & Lander, 1998; Wiggins, 2009; Wilson & Helgadottir, 2006). Postoperative pain following outpatient tonsillectomy in children remains a significant problem and optimal use of pain medication is essential to prevent significant postoperative pain (Aguilera & Walker, 1999; Finley, McGrath, Forward, McNeill, & Fitzgerald, 1996; Hamers, Abu-Saad, van den Houten, & Halfens, 1998; Kankkunen, Vehvilainen-Julkunen, Pietila, Kokki, & Halonen, 2003; Nikanne, Kokki, & Tuovinen, 1999) and reduce associated complications including dysphagia, decreased oral intake, and dehydration (Abou-Jaoude et al., 2006; Baugh et al., 2011; Shah, Shahab, Robb, & Roy, 2001; Wiggins & Foster, 2007).
Two of the primary reasons for inadequate postoperative pain relief include inadequate prescription and insufficient administration of prescribed medications (Hamers et al., 1998; Kankkunen et al., 2003). As ambulatory programs expand, it is necessary to re-evaluate and explore alternative strategies for delivery of effective analgesia at home, including optimizing the choice of analgesic, the dosing schedule, and parental education to administer analgesics in a more effective manner (Wolf, 1999). With the large increases in the number of outpatient surgical procedures performed in children, parents need to be provided with more comprehensive information and taught the necessary skills to provide effective pain management at home. In this article, we report on one approach that was used as part of two randomized controlled trials (Sutters et al., 2004, 2010) that resulted in increased dosing of scheduled analgesics in children following tonsillectomy. Details and main findings from these two intervention studies are published elsewhere (Sutters et al., 2004, 2005, 2007, 2010). The purpose of this article is 2-fold. First, the article provides a detailed description of the components of the PEDIATRIC PRO-SELF©: Pain Control Program (PPPCP), an extension of the original PRO-SELF©: Pain Control Program (West et al., 2003) for parents and children, which can be used to help parents manage their child’s pain at home following tonsillectomy. Second, the article includes parents’ descriptions of their experiences with the PPPCP that serve to validate the program’s utility in this patient population.
BACKGROUND
Adherence to the prescribed medication regimen
The evaluation of adherence with an analgesic regimen in pediatrics is unique because one must consider both the parent, who is usually responsible for giving the medication, and the child, who may be reluctant to take pain medication due to unpleasant taste or pain that occurs with swallowing the medication, as in children following tonsillectomy. Physicians routinely prescribe analgesics for children’s pain management at home following ambulatory surgery, generally on an “as needed” basis. However, many parents are reluctant to treat their children with pain medication or to give adequate doses of medication to control pain, even when they recognize and believe that they have significant pain (Finley et al., 1996; Unsworth, Franck, & Choonara, 2007). The reasons for undertreatment of pain in children are multifactorial. However, failures are often related to parents’ lack of knowledge and understanding concerning appropriate actions to take for effective pain management (Seid & Varni, 1999) or their inability/unwillingness to sustain the postoperative pain management program at home.
Education and support strategies in the ambulatory surgery setting
The need for better instructions concerning pain management at home has become evident (Finley et al., 1996; Kotiniemi et al., 1997). Previous research identified that parents were anxious about postoperative pain and desired more explanation from medical and nursing staff (Thompson, Irwin, Gunawardene, & Chan, 1996). The provision of accurate information to clarify misconceptions provides psychological support in preparation for surgery and reduces parents’ stress levels (Whelan & Kirkby, 1998). Methods of pain alleviation should be taught to parents by the hospital staff prior to the child’s discharge home after day surgery (Kankkunen et al., 2003). However, limited nursing time places constraints on the education provided in the ambulatory surgery setting (Voepel-Lewis, Andrea, & Magee, 1992). Preoperative teaching, parent support, and postoperative instructions are completed in several hours or less. A variety of preparation methods that range from simple to complex, including educational handouts, books, movies, and preoperative tours, are utilized. In addition, parents have access to information through the Internet. Further research is needed to validate the optimal methods to provide information and advise parents on children’s postoperative pain management at home.
Many ambulatory surgery programs provide short-term follow-up with a phone call to the home on the day after surgery to assure that information and discharge instructions are understood. This interaction provides an opportunity to reinforce parental education and skills in the early postoperative period, which is the most critical time to intervene to obtain optimal pain relief. The overall goal is to provide parents with the knowledge and support that will enable them to achieve an optimal level of pain management for their child and minimize side effects.
THE PPPCP
Development
This adaptation of the PPPCP is based on work by Miaskowski and colleagues for adult oncology patients and their family caregivers to reduce pain from bone metastases (Dodd & Miaskowski, 2000; Kim et al., 2004; Larson, Dodd, & Aksamit, 1998; West et al., 2003). The original PRO-SELF©: Pain Control Program was designed to increase a patient’s ability to perform self-care through mastery of specific knowledge and skills and supportive care including skills training, reinforcement activities, and nurse coaching. While the content of the adult version of the PRO-SELF© Program needed to be completely revised, the skills training and nurse coaching that were fundamental components of the Program were retained in the pediatric version. The remainder of this article describes the adaptation of the PRO-SELF© Program for parents and children following ambulatory surgery for tonsillectomy.
The goals of extending this nursing intervention to parents were to: (a) teach them the knowledge and skills needed to manage their child’s pain at home following tonsillectomy; (b) provide support and help parents with decision-making after their child was discharged home; and (c) coach parents to do the self-care activities for their child. Through written information and effective communication, parents are empowered to develop skills and knowledge in pain management, moving them toward independently providing care for their child (Jonas & Worsley-Cox, 2000). A total of 193 children 6 to 15 years of age and their parents were included in the two studies that tested the PPPCP (Sutters et al., 2004 [N = 80]; Sutters et al., 2010 [N = 113]). Both studies were approved by the institutional review board at the study site and at the University of California, San Francisco. As part of these randomized clinical trials, interview data were collected from children and their parents on the fourth day at home after surgery. Children’s accounts of their experiences with the PPPCP were reported previously (Sutters et al., 2007). Readers are referred to this article for a detailed description of the methods that were used to code parents’ home-interview data.
Theoretical framework for the intervention
The research was conceptualized within Orem’s (1991) general theory of nursing, which provides a useful framework for assisting parents to engage in self-care for their children. Orem’s self-care deficit theory focuses on an individual’s need for self-care to sustain life and health and to recover from disease or injury while coping with its effects (Closson, Mattingly, Finne, & Larson, 1994; Orem, 1991). Nursing actions taken to prevent or alleviate pain through provision of parental education and nurse coaching were viewed as components of Orem’s nursing systems.
Components of the PPPCP
The PPPCP was designed to provide parents of children undergoing tonsillectomy with the necessary knowledge and skills to manage their child’s postoperative pain at home and to coach them on how to optimize the prescribed analgesic regimen. As outlined in Table 1, the majority of the teaching focused on the implementation of the home analgesic regimen and the initial coaching occurred during the child’s postoperative recovery in the ambulatory surgery center. Reinforcement of the teaching and further coaching to promote parents’ adherence to the prescribed analgesic regimen occurred in the subsequent telephone calls on each of the first two postoperative days.
Table 1.
Components of the Pediatric PRO-SELF©: Pain Control Program
| Time period | Intervention |
|---|---|
| Preoperative—day of surgery | Nurse meets child and parents in ambulatory surgery preoperative area
|
| Postoperative—day of surgery | Nurse meets parents in the ambulatory surgery recovery area
|
| Postoperative day 1 | Nurse telephones parent
|
| Postoperative day 2 | Telephone call—same as postoperative day 1 |
| Postoperative day 4 | Home visit
|
Provision of information
Prior to the child’s discharge from ambulatory surgery, the research nurse used the PEDIATRIC PRO-SELF: Pain Control Booklet (i.e., the Booklet) as a guide to provide general postoperative care instructions (i.e., activity, diet, monitoring for postoperative bleeding and fever, follow-up) and as a template to guide education focused on pain management following tonsillectomy. The Booklet was developed, in part, from content included in the written postoperative discharge instructions distributed by participating pediatric ear, nose, and throat (ENT) surgeons at the study site. In addition, the Booklet included a pain management teaching guide presented in a question-and-answer format to provide information regarding the postoperative pain trajectory following tonsillectomy in children, the rationale for analgesic selection and scheduled analgesic administration, potential side effects, and “helpful hints” for giving pain medication to children. The content of the pain management teaching guide is summarized in Table 2.
Table 2.
Table of Contents and Excerpts from the Teaching Booklet
Postoperative instructions for tonsil and adenoid cases
|
|
Pain management The remainder of this booklet contains a list of the most common concerns/questions asked by parents about the management of their child’s pain following tonsillectomy. The information below may help you to understand the reasons for the pain treatment plan, the importance of following the instructions provided by your doctor and nurse, and some “helpful hints” for giving pain medicine to your child.
|
Pain medicines should be given on a regular schedule to “prevent” pain, rather than to “treat” pain. Prevention of pain is easier to do than chasing the pain after it occurs. Pain medicine needs to be given after surgery, even if the pain is not felt, to prevent the pain from coming back. Providing pain medicine “around-the-clock” may require waking a sleeping child. This is not easy to do, but it is necessary in order to provide a pain-free and restful sleep. Setting a timer during the day and an alarm clock during the night may help to remind you to give your child’s pain medicine on time. It’s important not to skip the nighttime dose(s), which may cause your child to wake up in pain in the morning.
|
| Good pain control is especially important in children following tonsillectomy because if your child has pain, he/she will not swallow or drink fluids and may become dehydrated or develop problems with infection or bleeding. If your child’s pain gets better or goes away during the first few days after surgery, it may be tempting to stop giving the pain medicine. However, stopping the pain medicine will allow the pain to come back. It is important to follow the prescription directions to be sure that your child is receiving the correct amount of pain medicine. |
|
Information included in the Booklet was derived from review of the literature that identified barriers to effective pain management in children (Finley et al., 1996; Forward, Brown, & McGrath, 1996; Gedaly-Duff & Ziebarth, 1994; Norinkavich, Howie, & Cariofiles, 1995; Sutters & Miaskowski, 1997; Warnock & Lander, 1998), the clinical practice guideline, Acute Pain Management: Operative or Medical Procedures and Trauma, which was developed by an expert panel convened by the Agency for Health Care Policy and Research (Acute Pain Management Guideline Panel, 1992), and recommendations from expert nurse clinicians. It was written at a ninth-grade reading level because an earlier study with a similar population found that the educational level of parents was at or above the ninth grade (Sutters, Levine, Dibble, Savedra, & Miaskowski, 1995). It was pilot-tested with parents of children undergoing tonsillectomy and found to be easy to follow and understand. Discharge instructions and review of the teaching booklet took between 15 and 20 min, and parents were provided with a copy of the teaching booklet to take home.
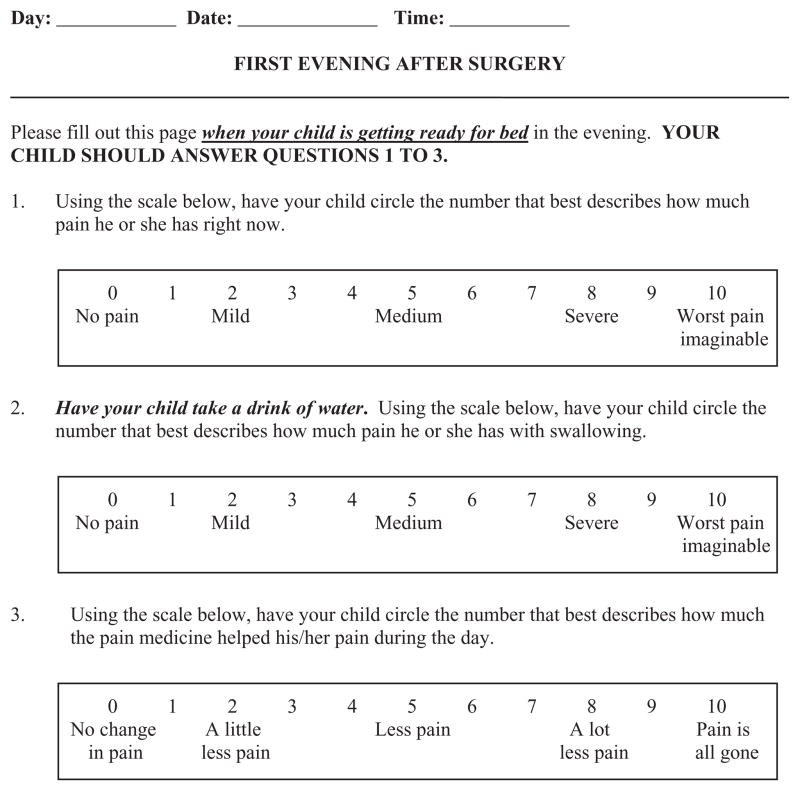
Medication record and digital timer
The research nurse taught the parents how to use the medication record to report information on the number and timing of analgesic doses that children received during the course of the study. As shown in Figure 1, the record was set up in a table format with four sections, beginning with the day of surgery through the third postoperative day. The instructions at the top of the medication record reminded parents not to give their child any pain medication other than what was prescribed. The research nurse recorded the day of the week, the date, the scheduled dosing times, and ordered dose volume (in milliliters). Parents circled the time that they gave each scheduled dose of medication. In the event that the dosing schedule was modified (e.g., excessive sedation resulting in a skipped dose, with subsequent breakthrough pain prior to the next scheduled dose requiring analgesic administration), parents were instructed to revise the dosing schedule by drawing a line through the previously written times and entering the new times at 4-hr intervals, beginning with the time of the dose just given. The content validity of the medication record was obtained by review and revision of the instrument by the investigators.
Figure 1.
Example of 1 Day from the Medication Record.
An additional component and support strategy of the PPPCP, which was not done in the original adult cancer pain study, included giving parents a battery-operated digital timer (Cook’s Club® Big Digit Digital Timer Clock, Cooks Club, Inc., Harrison, NJ, USA), with instructions to set it for 4 hr to remind them to give their child the pain medication.
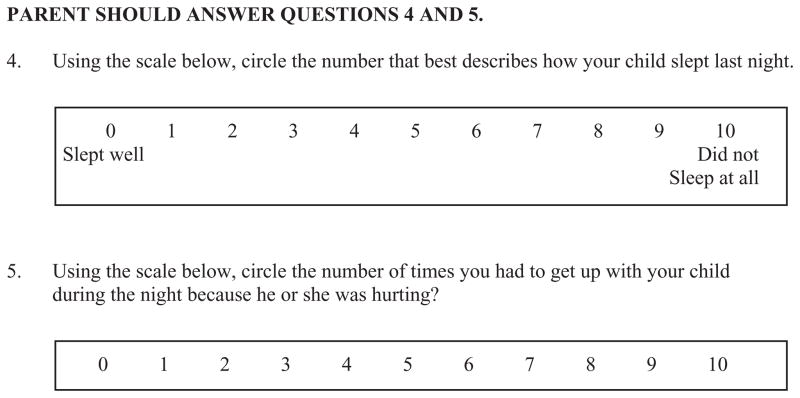
Pain Management Diary
The Pain Management Diary was modeled after that used in the original PRO-SELF©: Pain Control Program (West et al., 2003). The research nurse taught the parents how to use the Pain Management Diary, which parents completed twice a day, in the morning and at bedtime. The first page outlined the organization of the diary and provided written instructions on when to complete the respective sections. The pages were color-coded yellow for the portion of the diary that was completed in the morning and blue for the portion that was completed at night. Figure 2 illustrates the upper half of each page that was used to record the child’s self-reported pain intensity ratings with and without swallowing, and the child’s rating of pain relief from the analgesic medication. Parents were taught to obtain self-report ratings of their child’s pain and to complete this page of the diary when the child awoke each morning and each night at bedtime. Parents used the Pain Management Diary to determine if their child was in pain. However, analgesic administration was time-contingent and not linked to the child’s pain ratings.
Figure 2.
Example of 1 Day from the Home Diary—Pain Scores and Pain Relief Rating.
A descriptive numeric rating scale (NRS) was used for several reasons: (a) It was the tool currently being used in the clinical site where the study was conducted; (b) it was simple to administer, especially in a diary format; (c) it allowed for a greater dispersion of scores compared to some of the other pain rating scales; and (d) it did not require any special equipment. Since school-age children are able to provide valid and reliable self-reports of pain intensity (Franck, Greenberg, & Stevens, 2000; von Baeyer, 2006), pain ratings were obtained from the child rather than relying on parental assessment of the child’s pain. Parents were encouraged to have their children assist them to record their responses in the diary (i.e., circling their pain intensity and pain relief ratings on each of the respective 0 to10 NRS). Since pain intensity may vary between periods of rest and during swallowing, pain ratings for both conditions were recorded. The descriptive NRS is a simple, robust, and sensitive measure of pain intensity and is a valid measure of pain intensity in school-age children (Miro, Castarlenas, & Huguet, 2009; von Baeyer et al., 2009).
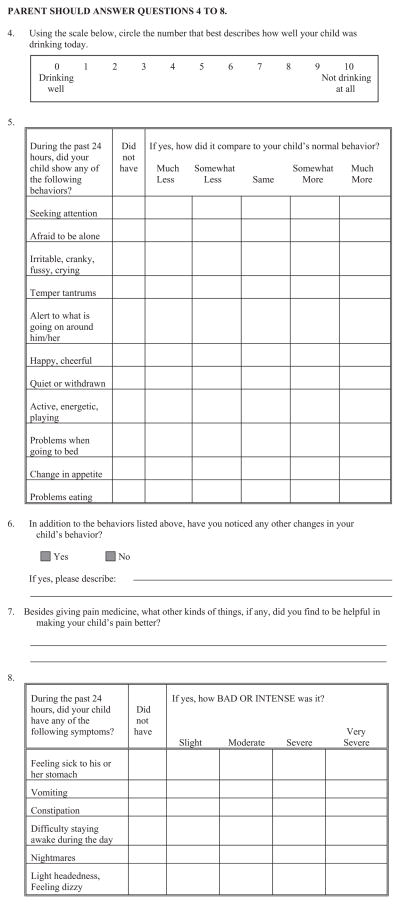
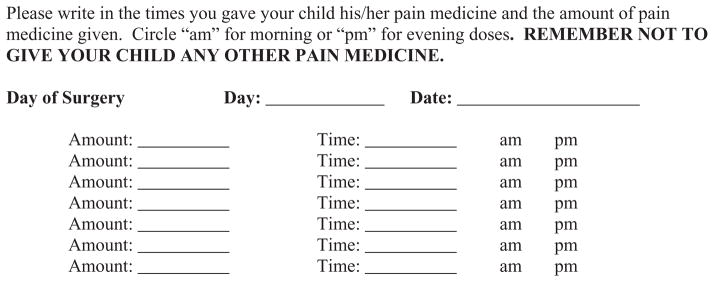
Because unrelieved pain can have deleterious effects on sleep, eating, and other behaviors, these parameters were assessed over the course of the study. Figure 3 illustrates the section of the Pain Management Diary that parents completed each morning (i.e., quality of sleep and interruption of sleep related to pain). Figure 4 illustrates the section of the diary that parents completed each evening (i.e., quality of fluid intake, behavioral changes, and analgesic side effects). Parents asked the children about their side effects and recorded them in the diary.
Figure 3.
Example of Pain Management Diary—Morning Questions.
Figure 4.
Example of Pain Management Diary—Evening Questions.
Content validity of the questions was determined by review of a panel of expert clinicians and by the investigators. Similar questions were used in a previous telephone survey (Sutters & Miaskowski, 1997), as well as in a pilot study of the diary that found that parents were able to provide valid and reliable responses to queries regarding specific parameters of their children’s recovery following tonsillectomy.
The behavioral checklist was used to record the presence or absence of specific child behaviors, which were then compared to the child’s normal behavior using a 5-level Likert-type scale that ranged from much less to much more. The list of behaviors was derived from postoperative behavioral changes that were reported in previous studies (Kotiniemi, Ryhanen, & Moilanen, 1996, 1997; Reid, Hebb, McGrath, Finley, & Forward, 1995).
The side-effects checklist contained six items and was developed based on a review of the literature on side effects of analgesic medications. This checklist was used in the original PRO-SELF© study of adults with cancer pain (Villars et al., 2007). The parent was asked to indicate the presence or absence of each side effect and to rate its severity using a 4-level Likert scale that ranged from 1 slight to 4 very severe. The content validity of the adapted instrument was established by a panel of experts in pediatric pain management. We tested the internal consistency reliability of the side effects checklist in a pilot study with participants who were not receiving adequate doses of analgesics to produce the expected level of side effects and found that its Cronbach’s alpha ranged from .71 to .82. Parents reported that it took approximately 10 min to complete the Pain Management Diary each day.
Teaching and nurse coaching
Dimensions of skills enhancement that were the focus of the teaching and nurse coaching included: (a) doing the skill correctly; (b) doing the skill consistently and in a timely manner; and (c) being able to evaluate whether the prescribed activity is effective (Larson et al., 1998). Initial parental instruction, followed by supportive, interactive care through nurse coaching was an integral aspect of the Program. Most of the coaching took place during the daily telephone calls on the first 2 days following surgery. The phone calls established a relationship between the parent and the nurse that offered supportive nursing care through encouragement and problem-solving assistance, and provided parents with the opportunity to enhance their self-care abilities.
The research nurse called at a prearranged time, reviewed the child’s pain scores for the previous 24 hr, and verified that the child was taking the pain medication. Earlier teaching was reviewed, re-education was provided as needed, the rationale for adhering to the prescribed scheduled analgesic dosing regimen was reinforced, and strategies to support and facilitate medication administration were reiterated if the nurse ascertained that the parent was having difficulties. Parents were instructed to contact their physician for questions unrelated to pain management. If parents reported that their child had unrelieved pain following administration of the prescribed analgesic, the research nurse contacted the surgeon to change the pain medication. In general, the daily telephone calls were focused and required only brief interaction between the parent and research nurse. In addition to the scheduled calls, parents were encouraged to call the research nurse for any questions/concerns or to validate their interventions. At the time of the home visit on the fourth postoperative day, parents were instructed to change the analgesic regimen to as-needed dosing only and transition to acetaminophen alone, based on the child’s self-report of pain intensity. This instruction was in accordance with the hospital’s standard procedure.
Research nurse training
The same research nurse provided the educational intervention to each participant. The research nurse was experienced in pediatric surgery, including tonsil and adenoid procedures. The research nurse received a 6-hr orientation to the study, teaching materials, and data collection procedures. This orientation provided the nurse with information on how to advise parents around common pain management issues that might arise. The research nurse was instructed to advise parents to contact their child’s physician directly for questions or concerns related to other postoperative care issues.
FINDINGS
Implementation and evaluation
The effectiveness of the PPPCP was tested in two randomized clinical trials with parents of children who underwent tonsillectomy with or without adenoidectomy (Sutters et al., 2004, 2005, 2007, 2010). Patients were randomized to receive either standard care (i.e., routine postoperative education and “as needed” analgesic dosing), standard care and “around-the-clock” (ATC) dosing, or the PPPCP (i.e., one that combined ATC dosing of analgesics, with parent postoperative education and nurse coaching targeted at decreasing barriers to effective pain control in the home). The two clinical trials were similar in design but evaluated the effectiveness of two different combination opioid/nonopioid analgesic medications (i.e., acetaminophen and codeine and acetaminophen and hydrocodone).
In both studies, children in the ATC groups received significantly higher doses of analgesic than children in the PRN group. However, no significant differences were found in the doses of analgesic administered per day between the ATC groups with and without nurse coaching (Sutters et al., 2004, 2010). Parents who were instructed to give the analgesic medication every 4 hr adhered to the prescribed analgesic regimen regardless of the coaching intervention. Nevertheless, study findings demonstrated that parents benefited from other components of the PPPCP.
Use of the teaching booklet
Analysis of the data from both studies found that the majority of parents in the experimental groups (i.e., ATC with and without nurse coaching) indicated that the teaching booklet and Pain Management Diary helped them to manage their child’s pain (i.e., 90% and 92%, respectively). Parents reported that the printed information was valuable and was used extensively as a reference. Comments regarding the teaching booklet included, “Everything was there that we needed to refer back to if we had any questions.” “The teaching booklet was really good because there’s a lot of things in there that I had no idea was going to happen because this was the first time I ever had to deal with any type of surgery with one of my children.” “Any time I had a question, I had the book to refer back to, so that’s why I didn’t page you.” “The day of surgery, everything was kind of overwhelming so it was good to have that to refer back to. I didn’t remember it all.”
Parents who reported that they did not use the teaching booklet indicated that the information provided prior to surgery and/or at the time of the child’s discharge from the hospital was sufficient. Several parents indicated that they were nurses, or had immediate family members who were nurses, and were already knowledgeable about the procedure and how to care for the child after surgery. One parent stated, “I recently had my tonsils out, so I knew what to expect and didn’t need it, but for someone who’s never had to go through this, I think it would be very helpful.”
Interestingly, several parents commented on the need for additional information. For example, one parent commented, “I would check the booklet before I called the nurse, and like with the patches in her throat, it didn’t say anything there … so of course I asked you about it.” Another parent commented about needing more information on whether or not to continue medications that were previously being taken (e.g., asthma/allergy medications). They were told to hold these medications on the morning of surgery and were never told to resume them until the research nurse instructed them to do so on the first postoperative day. Another parent commented, “I think they should be more specific on soft foods, and how long he is gonna be eating cold stuff, for the next 10 days? How are we supposed to know?” Another parent commented, “She’s 14 and I thought … you know, she’s pretty self-sufficient, but she regressed. She wanted me more, she wanted me there, she did other behaviors you know of younger children, and I was surprised by that.”
Use of the diary
Several parents reported that by tracking pain in the home log they could identify problems that needed follow-up as well as monitor improvements in symptoms. Comments included, “Writing down when she had the medicine and everything kind of helped me keep track of how often she was having it, and when the pain medicine would kind of wear off, and how much time she had left for the next one. It helped keep track of how much pain she was having.” “It helped me to be aware of what other symptoms she might have, and it helped me to remember when to give her more medicine.”
The Pain Management Diary served as a useful communication tool between family caregivers. Parents commented, “The home log was great especially when there are different caregivers, when she goes to Grandma’s or when her Dad is watching her, then we know what’s been done.” “I had everything documented and jotted down and I could sit back and remember how things went the day before and know how they were resting, how they were feeling, and I had a concrete way of letting you know how they were feeling each time.” Parents reported that the Pain Management Diary was useful in tracking the child’s recovery and improvement. For example, one parent commented, “It helped me make sure I stayed on track. Made me keep that schedule in my head cause I had to write it down. And it was really easy to remember because you’re always writing it down, and then it just kind of set in cause you know, they always tell you to write it.” Another parent commented, “It was encouraging to watch it go from you know, really painful and then the next couple of days she’d tell me that she’s getting better. Maybe it’s because when you look back you see, this is what I was going through on this day, and look at how much better it’s gotten. It kind of reminds you of how much better things are going.”
Use of the medication diary and digital timer
Parents commented on the benefit of the Pain Management Diary to the child. For example, one parent reported, “I think it helped him more than it helped me, cause when he’s had surgery before, he could never really say how much it hurt, but with the chart I think he thought that yes, it was okay that he could hurt. I think he kind of got excited to do it … he’d say, ‘did you wanna know this is how I’m feeling right now?’ ”
Parents commented specifically on the usefulness of the medication log and the digital timer, “It was very helpful because with my busy life, you get, you know, side tracked, so having the time clock and the log we were able to really keep track on how much and when it was given.” “I liked it because it let me know when I was supposed to give it (pain medicine) to him. It kept me on top of his pain because his pain wouldn’t flare up again you know because after 4 hr it would get worse, and I didn’t want him to be uncomfortable.” “Giving the pain medicine every 4 hr was no problem with your little alarm clock.” “Without the timer, I think I would have got confused. To wake me up in the night, that really helped me every 4 hr.” “It helped me to keep track of the time, what time I needed to do it.” “It was very useful because a lot of times during the night I couldn’t remember. I was afraid that I wouldn’t remember because I was so out of it myself from sleep deprivation that it helped me to write it down. Then in the morning I saw that, oh yeah, okay I gave it at that time.”
Evidence of skills development
Evidence of skill development was noted in parents’ responses during the telephone calls and home interviews. For example, one parent commented, “Sometimes I missed two doses, she woke up hurting. I couldn’t bring myself to wake her up you see cause she was sleeping so soundly, but I did find that if I would wake her up at 5:45 then she wouldn’t wake up in pain.” Another parent stated:
Make sure they don’t skip their medicine because that was when we had the hard time in the middle of the night the first night we came home. We let him go and we didn’t wake him up to take it and he woke up screaming in the middle of the night. That was a pretty bad situation because it was really hard to calm him down. And it was really hard to get him to take it when he was at that point of screaming and hollering, and screaming it hurts, it hurts. He was like, I said he was beyond … you know like they say the pain was beyond manageability because once it starts … so, I’m all for keeping it on a regular schedule.
Many parents shared tips on giving the medication, as well as other specific interventions that were helpful in managing their child’s pain, or things to avoid that made their child’s pain worse. Comments included, “At night when I’d wake him up, that was the only time he looked like he wanted to gag, and I think he was just confused … more asleep than awake. So, I’d make him take a drink of something else first and then take his medicine.” “Before giving the medicine, he would take some sips of ice water and then a little bit of medicine … another sip, about a teaspoon at a time.” In addition, parents identified things to avoid that made their child’s pain worse. One parent commented, “Don’t let them in front of a fan. I think it caused her more pain on the second day because it was hot, and we put the fan directly on her, and her throat was constantly sore.”
Parents’ commented on the child’s skill development as well:
At first it was kind of difficult cause we had to, you know wake up and give it, give it to him and everything, but after we got into kind of like a routine of doing it, it became easier and easier that he had to do it. So, on some occasions he would remind me, ‘mom it’s time for my medicine’ because the timer would be going off. At the end, when he knew he would take his medicine, he was actually doing it himself, and he was more comfortable because he knew how much he would take, and he’d swallow so it wouldn’t hurt him instead of me just trying to guess if I was giving it to him.
Parents provided evidence of skill building with regard to nonpharmacologic interventions. Although the teaching booklet included instructions for diet and activity, it did not specifically address nonpharmacologic pain management strategies. Many parents reported distraction as an effective approach. One parent reported, “It definitely seemed to work a lot better keeping him involved in something, you know, talking, watching TV, or playing a game or something … keeping his mind off his pain.” Another parent commented, “Me and her dad talked to her and tried to make her laugh and smile. When she smiled, then that’s when she forgot about her pain.” Cold fluids or external cold were identified by many parents as an effective pain relief strategy. For example, one parent recommended “frozen peas as an ice pack.” Another parent commented, “Cold things were the one thing that really helped relieve the pain. Whether we kept ice in her cup when she had juice, and so forth and so on.”
Parents demonstrated critical thinking skills in evaluating potential causes for side effects such as nausea. One parent commented, “There’s the possibility of the erythromycin causing him to be so nauseous, as well as giving the codeine, we weren’t sure which one or if both were causing side effects. Billy was changed to Cefprozil and the vomiting stopped.” The parents questioned why the physician would prescribe a medication that would have such harsh side effects if not taken with food when their child had just had a tonsillectomy and was not able to eat well.
Evidence of nurse coaching
The nurse-parent interactions during the phone calls on postoperative days 1 and 2 were reported by parents to be helpful, useful, and informative. Comments included, “It was good to have a nurse call and answer concerns.” “I liked to be in contact with the nurses because if I had any questions, they answered them. They said if he’s uncomfortable, go ahead and give the pain medicine 15 to 20 min ahead of schedule, that was very useful.” “It was helpful in a lot of ways, like I didn’t know what to do about his stomach pain, I was so scared.” Parents also described the emotional support that the calls from the research nurse provided. One parent commented, “When she called me, I knew she was caring, and I felt like she was concerned.” Another parent commented, “I look forward to the calls because it helps me, it tells me you’re concerned really about the patient you know, when he comes home. Most of the time when the kids come home, that’s it, you don’t have anybody.” One parent commented on the benefit to the child, “He’d say, ‘mom the nurse called me today’ and you know, he was all excited about that. So that alone, knowing that you’re still caring and you’re concerned about him, that was really good.”
DISCUSSION
The findings from our two randomized clinical trials (Sutters et al., 2004, 2005, 2007, 2010) demonstrated the feasibility of adapting the PRO-SELF©: Pain Control Program to parents caring for children, ages 6 to 15 years, at home following outpatient surgery. Education is key to preparing parents as participants in their child’s care, and ambulatory surgery nurses play a pivotal role. It is imperative that parents have the essential information, skills, and support to carry out effective pain management for their child. Findings from our two studies suggested that when scheduled analgesic administration is prescribed, along with written instructions that detail the expected pain trajectory, rationale for a time-contingent analgesic dosing regimen, and strategies to facilitate analgesic administration, analgesic administration at home is improved, with or without the nurse coaching intervention.
Written materials are by far the most frequently used tools for parental education. They provide a standardized teaching format for the nurse to use to give discharge instructions. In addition, they can be taken home (Lea & Phippen, 1992) and serve as a resource for parents to use at home. Study findings validated the utility of the teaching booklet written at an appropriate reading level that included detailed information about pain management to increase parents’ knowledge about pain management and to serve as a mechanism for nursing staff to standardize discharge teaching regarding pain management. Findings from our research and other investigations (Seid & Varni, 1999) indicate that when parents have a clear understanding of pain management and the provision of adequate pain relief, they report high satisfaction and improved outcomes (e.g., increased analgesic consumption, decreased pain). However, future studies need to evaluate other methods of education for both parents and children (e.g., DVDs, CDs).
In addition, the use of a digital timer, which is readily available in most homes, was identified by parents as a valuable tool to keep track of scheduled dosing times. Finally, the Pain Management Diary helped parents to think about their child’s pain, their responses to the analgesic regimen, and to identify other observed/reported symptoms that the child experienced during their early postoperative recovery. The use of a diary provided more accurate information than methods that rely on recall because it increases the validity and reliability of the data recorded (Gill, Shand, Fuggle, Dugan, & Davies, 1997; Jeffries, Huth, & Daraiseh, 2009; Maikler, Broome, Bailey, & Lea, 2001).
The majority of teaching for the PPPCP occurred in the hospital, prior to the child’s discharge from ambulatory surgery. The mean length of time required to provide discharge instructions including expanded pain management information was approximately 20 min. Although this amount of time may represent an increase over what is routinely spent in providing postoperative discharge instructions to parents in the ambulatory surgery setting, it represents a critical component of patient care, and efforts to insure this outcome should justify the additional time required.
An important finding from our investigations is that nurse coaching did not impact analgesic administration (Sutters et al., 2004, 2010). Parents instructed to give pain medication ATC, with or without nurse coaching, gave more medication than parents instructed to administer the analgesic on an as-needed basis. Detailed postoperative instructions regarding pain management resulted in greater adherence to postoperative analgesic administration compared to children whose parents received standard postoperative instructions. Similar to findings from other studies (Huth, 1999; Kankkunen, Vehvilainen-Julkunen, & Pietila, 2002), telephone calls from the research nurse were upheld as a measure of support for parents, as well as an opportunity for parents to validate their decision-making regarding their child’s pain management. Several parents commented that they were glad to know that the nurse was available and could be contacted if they had questions or concerns. Parents’ adherence with completing the diary (93.5% adherence rate) was attributed to the follow-up telephone calls by the research nurse.
The first step in influencing outcomes is to identify areas in which family caregivers perceive problems after discharge (Closson et al., 1994). Similar to reports from previous research (Kankkunen et al., 2003), our findings indicated that parents’ perceptions and use of analgesics were not related to an underestimation of pain but rather to difficulties associated with adherence to a frequent dosing schedule, nighttime dosing, oral ingestion/sore throat, nausea interfering with oral intake, and child refusal to take them. Additional research is needed to identify strategies to address/overcome these risks to nonadherence with prescribed therapeutic regimens.
Although scheduled analgesic dosing reduced children’s pain intensity scores following tonsillectomy, it did not completely alleviate the children’s postoperative pain. Similar to findings from other research (Kankkunen, Vehvilainen-Julkunen, Pietila, & Halonen, 2003), our study findings demonstrated that parents identified a number of helpful adjunctive comfort and pain relief measures used at home, which could easily be incorporated into written educational materials and addressed as part of the routine discharge instructions provided by nursing staff. Further research is needed to evaluate the effectiveness of these methods for acute pain relief in children following tonsillectomy and to evaluate how parents are guided to use nonpharmacological methods to relieve acute postoperative pain.
How Do I Apply This Evidence to Nursing Practice?
Parents need specific education regarding their child’s postoperative pain management at home. Nurses play a critical role in providing them with useful information and support that will influence their decision-making and participation in care. Practice implications include identification of key strategies of the PRO-SELF©: Pain Control Program that were most effective for parents in the pediatric ambulatory surgery setting. In conjunction with optimizing the analgesic dosing schedule, nurses need to (a) use an educational booklet to increase parent’s knowledge about pain management strategies; (b) provide a timer to insure adherence with the prescribed analgesic regimen; (c) provide a Pain Management Diary to track analgesic dosing, the child’s pain intensity scores, and other symptoms; and (d) provide interactive nursing support. Although nurse coaching was not found to be an important strategy that impacted analgesic administration, the nurse-parent interaction that occurred during the postoperative phone calls was useful in providing support, validating parental decision-making, and promoting completion of the Pain Management Diary.
Acknowledgments
This research was supported by a grant from the National Institute of Nursing Research (NR04826, NCT00251628). The authors would like to acknowledge the support and assistance of the surgeons, pharmacists, nurses, and other staff at our study site as well as our project staff. We are especially grateful to all the children and parents who participated in the two studies.
Footnotes
Disclosure: The authors report no actual or potential conflicts of interest.
Contributor Information
Kimberly A. Sutters, Clinical Nurse Specialist, Surgical Services, Pain Management, Children’s Hospital Central California, Madera, and Assistant Adjunct Professor, School of Nursing, University of California, San Francisco.
Marilyn C. Savedra, Professor Emerita, School of Nursing, University of California, San Francisco.
Christine Miaskowski, Professor and Associate Dean for Academic Affairs, American Cancer Society Clinical Research Professor, Sharon A. Lamb Endowed Chair, School of Nursing, University of California, San Francisco, California, USA.
References
- Abou-Jaoude PM, Manoukian JJ, Daniel SJ, Balys R, Abou-Chacra A, Nader ME, Schloss MD. Complications of adenotonsillectomy revisited in a large pediatric case series. Journal of Otolaryngology. 2006;35(3):180–185. [PubMed] [Google Scholar]
- Acute Pain Management Guideline Panel. AHCPR Pub No. 92-0032. Rockville, MD: Agency for Health Care Policy and Research. Public Health Service, U.S. Department of Health and Human Services; 1992. Acute pain management: Operative or medical procedures and trauma. Clinical practice guideline. [Google Scholar]
- Aguilera IM, Walker RW. Tears at bedtime. British Journal of Anaesthesia. 1999;83(2):358–359. doi: 10.1093/bja/83.2.358-a. [DOI] [PubMed] [Google Scholar]
- Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ, Patel MM. Clinical practice guidelines: Tonsillectomy in children. Otolaryngology and Head and Neck Surgery. 2011;144:S1–S30. doi: 10.1177/0194599810389949. [DOI] [PubMed] [Google Scholar]
- Closson BL, Mattingly LJ, Finne KM, Larson JA. Telephone follow-up program evaluation: Application of Orem’s self-care model. Rehabilitation Nursing. 1994;19(5):287–292. doi: 10.1002/j.2048-7940.1994.tb00824.x. [DOI] [PubMed] [Google Scholar]
- Dodd MJ, Miaskowski C. The pro-self program: A self-care intervention program for patients receiving cancer treatment. Seminars in Oncology Nursing. 2000;16:300–308. doi: 10.1053/sonu.2000.16586. [DOI] [PubMed] [Google Scholar]
- Finley G, McGrath P, Forward S, McNeill G, Fitzgerald P. Parents’ management of childrens’ pain following “minor” surgery. Pain. 1996;64(1):83–87. doi: 10.1016/0304-3959(95)00091-7. [DOI] [PubMed] [Google Scholar]
- Forward SP, Brown TL, McGrath PJ. Mothers’ attitudes and behavior toward medicating children’s pain. Pain. 1996;67:469–474. doi: 10.1016/0304-3959(96)03149-1. [DOI] [PubMed] [Google Scholar]
- Franck LS, Greenberg CS, Stevens B. Pain assessment in infants and children. Pediatric Clinics of North America. 2000;47(3):487–512. doi: 10.1016/S0031-3955(05)70222-4. [DOI] [PubMed] [Google Scholar]
- Gedaly-Duff V, Ziebarth D. Mothers’ management of adenoid-tonsillectomy pain in 4- to 8-year-olds: A preliminary study. Pain. 1994;57:293–299. doi: 10.1016/0304-3959(94)90004-3. [DOI] [PubMed] [Google Scholar]
- Gill LJ, Shand PAX, Fuggle P, Dugan B, Davies SC. Pain assessment for children with sickle cell disease: Improved validity of diary keeping versus interview ratings. British Journal of Health Psychology. 1997;2:131–140. [Google Scholar]
- Hamers JPH, Abu-Saad HH. Children’s pain at home following (adeno) tonsillectomy. European Journal of Pain. 2002;6:213–219. doi: 10.1053/eujp.2001.0326. [DOI] [PubMed] [Google Scholar]
- Hamers JPH, Abu-Saad HH, van den Houten MA, Halfens RJG. Are children given insufficient pain-relieving medication postoperatively? Journal of Advanced Nursing. 1998;27(1):37–44. doi: 10.1046/j.1365-2648.1998.00493.x. [DOI] [PubMed] [Google Scholar]
- Helgadottir HL, Wilson ME. Temperament and pain in 3- to 7-year-old children undergoing tonsillectomy. Journal of Pediatric Nursing. 2004;19(3):204–213. doi: 10.1016/j.pedn.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Homer JJ, Swallow J, Semple P. Audit of pain management at home following tonsillectomy in children. Journal of Laryngology and Otology. 2001;115:205–208. doi: 10.1258/0022215011907208. [DOI] [PubMed] [Google Scholar]
- Huth M. A response to Seid & Varni [Peer commentary on the journal article “Pediatric day surgery outcomes management: The role of preoperative anxiety and a home pain management protocol”] Journal of Child and Family Nursing. 1999;2(4):273–275. Retrieved from http://www.nursingcenter.com/library/journalissue.asp?Journal_ID=54031&Issue_ID=55039. [PubMed] [Google Scholar]
- Huth MM, Broome ME. A snapshot of children’s postoperative tonsillectomy outcomes at home. Journal for Specialists in Pediatric Nursing. 2007;12(3):186–195. doi: 10.1111/j.1744-6155.2007.00111.x. [DOI] [PubMed] [Google Scholar]
- Jeffries A, Huth M, Daraiseh N. Podium presentation at the 118th Annual Meeting of the Ohio Academy of Science. Springfield, OH: Wittenberg University; 2009. Use of a home diary to assess children’s pain after tonsillectomy. [Google Scholar]
- Jonas D, Worsley-Cox K. Information giving can be painless. Journal of Child Health Care. 2000;4(2):55–58. doi: 10.1177/136749350000400202. [DOI] [PubMed] [Google Scholar]
- Kankkunen K, Vehvilainen-Julkunen K, Pietila AM, Halonen P. Parents’ use of nonpharmacological methods to alleviate children’s postoperative pain at home. Journal of Advanced Nursing. 2003;41(4):367–375. doi: 10.1046/j.1365-2648.2003.02536.x. [DOI] [PubMed] [Google Scholar]
- Kankkunen K, Vehvilainen-Julkunen K, Pietila AM, Kokki H, Halonen P. Parents’ perceptions and use of analgesics at home after children’s day surgery. Paediatric Anaesthesia. 2003;13:132–140. doi: 10.1046/j.1460-9592.2003.00998.x. [DOI] [PubMed] [Google Scholar]
- Kankkunen PM, Vehvilainen-Julkunen KM, Pietila AMK. Children’s postoperative pain at home: Family interview study. International Journal of Nursing Practice. 2002;8:32–41. doi: 10.1046/j.1440-172x.2002.00341.x. [DOI] [PubMed] [Google Scholar]
- Kim JE, Dodd M, West C, Paul S, Facione N, Schumacher K, Miaskowski C. The PRO-SELF pain control program improves patients’ knowledge of cancer pain management. Oncology Nursing Forum. 2004;31(6):1137–1143. doi: 10.1188/04.ONF.1137-1143. [DOI] [PubMed] [Google Scholar]
- Kotiniemi LH, Ryhanen PT, Moilanen IK. Behavioural changes following routine ENT operations in two-to-ten year old children. Paediatric Anaesthesia. 1996;6:45–49. doi: 10.1111/j.1460-9592.1996.tb00352.x. [DOI] [PubMed] [Google Scholar]
- Kotiniemi LH, Ryhanen PT, Moilanen IK. Behavioural changes in children following day-case surgery: A 4-week follow-up of 551 children. Anaesthesia. 1997;52:970–976. doi: 10.1111/j.1460-9592.1996.tb00352.x. [DOI] [PubMed] [Google Scholar]
- Kotiniemi LH, Ryhanen PT, Valanne J, Jokela R, Mustonen A, Poukkula E. Postoperative symptoms at home following day-case surgery in children: A multicentre survey of 551 children. Anaesthesia. 1997;52(10):963–969. doi: 10.1111/j.1365-2044.1997.202-az0337.x. [DOI] [PubMed] [Google Scholar]
- Larson PJ, Dodd MJ, Aksamit I. A symptom-management program for patients undergoing cancer treatment: The PRO-SELF Program. Journal of Cancer Education. 1998;13(4):248–252. doi: 10.1080/08858199809528554. [DOI] [PubMed] [Google Scholar]
- Lea SG, Phippen ML. Client education in the ambulatory surgery setting. Seminars in Perioperative Nursing. 1992;1(4):203–223. [PubMed] [Google Scholar]
- LeRoy S, Elixson EM, O’Brien P, Tong E, Turpin S, Uzark K. Recommendations for preparing children and adolescents for invasive cardiac procedures. A statement from the American Heart Association Pediatric Nursing Subcommittee of the Council on Cardiovascular Nursing in Collaboration With the Council on Cardiovascular Diseases of the Young. Circulation. 2003;108:2550–2564. doi: 10.1161/01.CIR.0000100561.76609.64. [DOI] [PubMed] [Google Scholar]
- Maikler VE, Broome ME, Bailey P, Lea G. Childrens’ and adolescents’ use of diaries for sickle cell pain. Journal for Specialists in Pediatric Nursing. 2001;6(4):161–169. doi: 10.1111/j.1744-6155.2001.tb00240.x. [DOI] [PubMed] [Google Scholar]
- Miro J, Castarlenas E, Huguet A. Evidence for the use of a numerical rating scale to assess the intensity of pain. European Journal of Pain. 2009;13(10):1089–1095. doi: 10.1016/j.ejpain.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Nikanne E, Kokki H, Tuovinen K. Postoperative pain after adenoidectomy in children. British Journal of Anaesthesia. 1999;82(6):886–889. doi: 10.1093/bja/82.6.886. [DOI] [PubMed] [Google Scholar]
- Norinkavich KM, Howie G, Cariofiles P. Quality improvement study of day surgery for tonsillectomy and adenoidectomy patients. Pediatric Nursing. 1995;21(4):341–344. [PubMed] [Google Scholar]
- Orem DE. Nursing: Concepts of practice. 4. New York: Mosby-Year Book; 1991. [Google Scholar]
- Reid GJ, Hebb JP, McGrath PJ, Finley GA, Forward SP. Cues parents use to assess postoperative pain in their children. Clinical Journal of Pain. 1995;11:229–235. doi: 10.1097/00002508-199509000-00011. [DOI] [PubMed] [Google Scholar]
- Seid M, Varni JW. Pediatric surgery outcomes management: The role of preoperative anxiety and a home pain management protocol. Journal of Clinical Outcomes Management. 1999;6(2):24–30. [Google Scholar]
- Shah C, Shahab R, Robb P, Roy D. Role of a home care team in paediatric day-case tonsillectomy. Journal of Laryngology and Otology. 2001;115:39–43. doi: 10.1258/0022215011906975. [DOI] [PubMed] [Google Scholar]
- Sutters KA, Levine JD, Dibble S, Savedra M, Miaskowski C. Analgesic efficacy and safety of single-dose intramuscular ketorolac for postoperative pain management in children following tonsillectomy. Pain. 1995;61:145–153. doi: 10.1016/0304-3959(94)00166-C. [DOI] [PubMed] [Google Scholar]
- Sutters KA, Miaskowski C. Inadequate pain management and associated morbidity in children at home following tonsillectomy. Journal of Pediatric Nursing. 1997;12(3):178–185. doi: 10.1016/S0882-5963(97)80075-9. [DOI] [PubMed] [Google Scholar]
- Sutters KA, Miaskowski C, Holdridge-Zeuner D, Waite S, Paul S, Savedra M, Lanier B. A randomized clinical trial of the effectiveness of a scheduled analgesic dosing regimen for the management of postoperative pain in children following tonsillectomy. Pain. 2004;110(1–2):49–55. doi: 10.1016/j.pain.2004.03.008. [DOI] [PubMed] [Google Scholar]
- Sutters KA, Miaskowski C, Holdridge-Zeuner D, Waite S, Paul S, Savedra M, Lanier B. Time-contingent dosing of an opioid analgesic following tonsillectomy does not increase moderate to severe side effects in children. Pain Management Nursing. 2005;6(2):49–57. doi: 10.1016/j.pmn.2005.01.001. [DOI] [PubMed] [Google Scholar]
- Sutters KA, Miaskowski C, Holdridge-Zeuner D, Waite S, Paul S, Savedra M, Lanier B. Children’s expectations of pain, perceptions of analgesic efficacy, and experiences with nonpharmacologic pain management strategies at home following tonsillectomy. Journal for Specialists in Pediatric Nursing. 2007;12(3):139–148. doi: 10.1111/j.1744-6155.2007.00107.x. [DOI] [PubMed] [Google Scholar]
- Sutters KA, Miaskowski C, Holdridge-Zeuner D, Waite S, Paul S, Savedra M, Mahoney K. A randomized clinical trial of the efficacy of scheduled dosing of acetaminophen and hydrocodone for the management of postoperative pain in children following tonsillectomy. Clinical Journal of Pain. 2010;26(2):95–103. doi: 10.1097/AJP.0b013e3181b85f98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson N, Irwin MG, Gunawardene WMS, Chan L. Pre-operative parental anxiety. Anaesthesia. 1996;51:1008–1012. doi: 10.1111/j.1365-2044.1996.tb14992.x. [DOI] [PubMed] [Google Scholar]
- Unsworth V, Franck LS, Choonara I. Parental assessment and management of children’s postoperative pain: A randomized clinical trial. Journal of Child Health Care. 2007;11(3):186–194. doi: 10.1177/1367493507079558. [DOI] [PubMed] [Google Scholar]
- Vallee E, Lafrenaye S, Tetrault JP, Mayer S, Dorion D. Pain management after tonsillectomy: Morphine is not enough. Journal of Otolaryngology: Head and Neck Surgery. 2008;37(2):279–284. doi: 10.2310/7070.2008.0059. [DOI] [PubMed] [Google Scholar]
- Villars P, Dodd M, West C, Koetters T, Paul SM, Schumacher K, Miaskowski C. Differences in the prevalence and severity of side effects based on type of analgesic prescription in patients with chronic cancer pain. Journal of Pain and Symptom Management. 2007;33(1):67–77. doi: 10.1016/j.jpainsymman.2006.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voepel-Lewis T, Andrea CM, Magee SS. Parent perceptions of pediatric ambulatory surgery: Using family feedback for program evaluation. Journal of Post Anesthesia Nursing. 1992;7:106–114. [PubMed] [Google Scholar]
- von Baeyer CL. Children’s self-reports of pain intensity: Scale selection, limitations, and interpretation. Pain Research & Management. 2006;11(3):157–162. doi: 10.1155/2006/197616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA. Three new datasets supporting the use of the numerical rating scale (NRS-11) for children’s self-reports of pain intensity. Pain. 2009;143:223–227. doi: 10.1016/j.pain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Warnock FF, Lander J. Pain progression, intensity, and outcomes following tonsillectomy. Pain. 1998;75:37–45. doi: 10.1016/S0304-3959(97)00202-9. [DOI] [PubMed] [Google Scholar]
- West CM, Dodd MJ, Paul SM, Schumacher K, Tripathy D, Koo P, Miaskowski C. The PRO-SELF©: Pain control program—An effective approach for cancer pain management. Oncology Nursing Forum. 2003;30(1):65–73. doi: 10.1188/03.ONF.65-73. [DOI] [PubMed] [Google Scholar]
- Whelan TA, Kirkby RJ. Advantages for children and their families of psychological preparation for hospitalization and surgery. Journal of Family Studies. 1998;4(1):35–51. doi: 10.5172/jfs.4.1.35. [DOI] [Google Scholar]
- Wiggins SA. Family exemplars during implementation of a home pain management intervention. Issues in Comprehensive Pediatric Nursing. 2009;32:160–179. doi: 10.3109/01460860903281341. [DOI] [PubMed] [Google Scholar]
- Wiggins SA, Foster RL. Pain after tonsillectomy and adenoidectomy: “Ouch it did hurt bad. Pain Management Nursing. 2007;8(4):156–165. doi: 10.1016/j.pmn.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Wilson ME, Helgadottir HL. Patterns of pain and analgesic use in 3- to 7-year-old children after tonsillectomy. Pain Management Nursing. 2006;7(4):159–166. doi: 10.1016/j.pmn.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Wolf AR. Tears at bedtime: A pitfall of extending paediatric day-case surgery without extending analgesia. British Journal of Anaesthesia. 1999;82(3):319–320. doi: 10.1093/bja/82.3.319. [DOI] [PubMed] [Google Scholar]