Abstract
Handovers permeate healthcare delivery systems. They are critical for patient safety and continuity of care, but also for logistics and clinical efficiency. Poor handovers can cause reduced efficiency, delayed discharge or time to operation, and contributes to patient harm.
The Objective was to conduct a human factors assessment (HFA) using a systems approach to study the handover process at an Orthopaedic unit, determine barriers to information transfer, and suggest improvements.
A direct observation model was used to help provide insights on the evening handover process. A Systems Engineering Initiative for Patient Safety (SEIPS) model was used to provide a framework. A total of ten handover sessions were observed and the junior doctors were interviewed using a semi-structured approach.
Participants had two chief centres of complaint: workspace and environmental issues (such as a small, hot, uncomfortable room), and the lack of the junior house officer at handover leading to ‘signal loss’ with respect to sick patients who may not be handed over fully. The process also lacked standardisation and structure compounding the potential loss of information.
Conclusion
Good handover remains a cornerstone of safe and effective clinical practice and continuity of care. This study has shown how an HFA can be useful in determining problems with the handover process locally. It suggests an approach for improvement and recommends better training at all levels in this aspect of patient care.
Keywords: Handover, Human Factors Assessment, SEIPS Model, Systems Approach, Communication, Patient Safety
Introduction
What are handovers and why are they important?
Clinical handover is defined as the – “transfer of professional responsibility and accountability for some or all aspects of care for a patient, or groups of patients, to another person or professional group on a temporary or permanent basis.”1 Handovers permeate healthcare delivery systems and occur at multiple points: shift changes, transfer of patients within hospitals (e.g. from theatre to recovery), patient transfer between hospitals, and from the community to the emergency department. Handovers are critical for a safe, reliable and efficient healthcare system.2 Poor handovers can cause a range of problems from reducing efficiency, delays in discharge or time to operation, and even contribute to patient harm as highlighted by Sir John Lilleyman, Medical Director of the National Patient Safety Agency (NPSA) – “Handover of care is one of the most perilous procedures in medicine, and when carried out improperly can be a major contributory factor to subsequent error and harm to patients.”1
Handovers, and indeed much of patient care, are an exercise in communication. Good handovers necessitate effective communication between people and teams. This is acknowledged in the General Medical Council's Good Medical Practice, in which doctors are to “keep colleagues well informed when sharing the care of patients”.3 The Institute of Medicine's sentinel reports: To Err is Human4 and Crossing the Quality Chiasm5 both emphasise the importance of continuity of care and robust information exchange between clinicians. The importance of handover is also emphasised in the UK Department of Health report: An Organisation with a Memory.6
Communication failures have been cited in several studies looking at causation of near misses.7,8 Previous studies examining handover in Medicine, Trauma and Orthopaedics, and General Surgery,9,10,11 have shown that current handover arrangements fall short of the ideal set out in the Safe Handover guidelines from the British Medical Association, NHS Modernisation Agency, and the NPSA.1
Handovers in Context, Internationally and in the UK
The ramification of this heightened awareness is that patient handover has been recognised internationally as a priority area for patient safety. Prevention of handover error is one of the five solution areas of the High 5s Initiative, established in 2006 through collaboration between the Commonwealth Fund and the World Health Organisation (WHO) to implement innovative patient safety solutions over five years.12 In 2007, effective communication during handover was listed as one of the National Patient Safety Goals by the Joint Commission on Accreditation of Healthcare Organisations.13 The UK, in particular, has much to gain from better handover practice. It has the second lowest ratio of doctors to patients in Europe, with 1.7/1000 compared with 3.0–5.0/1000 in many other countries in the European Union.22 In addition, the European Working Time Directives (EWTD) mandate of a 48-hour working week has necessitated multiple handovers of patients per day, both formally and informally. 14
Objectives
The objective of this study was to conduct a human factors assessment (HFA) using a systems approach of the handover process at the Orthopaedic Department at my hospital.15 Problems and barriers to information transfer would be determined using a SEIPS model to help structure the approach and suggest improvements.16
Methods
Setting
The study was conducted at the Trauma and Orthopaedics Department at Frimley Park Hospital NHS Foundation Trust in Frimley, Surrey, UK. The trust serves more than 400,000 people across North-East Hampshire, West Surrey, and East Berkshire, although its catchment for some services is much wider. In 2010–2011, the trust had over 100,000 Accident and Emergency Department (A&E) attendances for the first time.17 The Trauma and Orthopaedics department has 25 Consultant Surgeons and is one of the largest in the UK. There are three orthopaedic wards containing approximately 80 beds with additional patients sometimes outlying on other wards.
The structure and purpose of handovers in the Orthopaedic Department
Formal handover takes place twice a day at 08:00 and 20:00. The morning handover is multidisciplinary and involves discussing patients admitted in the previous 24-hour period. The evening handover is between the Senior House Officer (SHO) on-call for the day and the incoming night SHO. It purpose specifically is to inform the night SHO about:
-
1.
New patient admissions that day.
-
2.
Sick patients (e.g. to check haematological and radiological investigations, and review them later).
-
3.
Patients for operating theatre the next day (so the correct theatre list can be handed to theatre coordinators, patients can be prepared for theatre, fasted accordingly, given IV fluids, etc.).
-
4.
Patients waiting to be seen in A&E or who are expected to arrive or transfer from another hospital.
Observing handovers
A direct observation model was used to help provide insights on the handover process ‘up close’. Whilst handover was taking place, the author would observe the session and take notes. Such methodology is known to be effective and has been utilised by Catchpole et al. as means of identifying system failures in paediatric cardiac surgery.18,19 The focus of the study was evening handovers and 10 such sessions were observed. The aim was to see who attended, ask and observe what people do, ask participants what problems they face, and how the prevailing system could be improved using a semi-structured interview. Those questioned were invited to comment on the people, equipment, task, workspace, environment, organisation and asked to think about what differentiates a good handover from a bad handover. At the start of the observation period, an email was sent to all SHOs working in the Orthopaedic Department stating that handover would be observed and that this was not assessing individual performance. Observations were recorded in note format on an iPhone 4 or on a computer available in the same room. It was felt this would result in less Hawthorne effects than a clipboard. 20
Results
The prevailing handover process
The morning handover takes place in a large orthopaedic seminar room with AV facilities and good ventilation. There tended to be 10–15 people present, including; Orthopaedic Junior and Senior House Officers (JHO/SHO), Orthopaedic Specialist Registrars (SpR) and Consultants, a Trauma Coordinator, a Geriatric Medicine Consultant, and Physiotherapists. The evening handover session takes place in a small room (10 × 8 ft) with no window, ventilation, or airconditioning; attendance is more variable. Two doctors usually attend, the outgoing day SHO and incoming night SHO. They are not usually joined by the on-call SpR who is often in theatre or JHO whose shift finishes one hour earlier. In addition, to these formal handovers would be an informal ad hoc handover to the on-call JHO or SHO when staff who are not on-call leave at around 17:00. This pattern of working is illustrated below (Table 1).
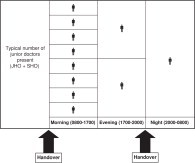
Table 1.
An illustration of the typical number of doctors present during a 24-hour period highlighting when handovers take place.
The on-call SHO for the day would typically be seeing new admissions via Accident and Emergency (A&E) and referrals from other specialties for inpatient consultations. The on-call JHO would be on the wards, managing patients and attending to anyone flagged by the nurses (using an early warning scoring system) as being unwell. In total 10 evening handovers were observed during March-April 2012 and 10 people were interviewed face to face at various times during this period (five SHOs and five JHOs). Table 2 provides the results of these observations and interviews.
Table 2.
Results of the observations and semi-structured interviews.
| Systems Approach Criteria | Observations (n = 10) | Comments from semi-structured interviews (n = 10; 5 SHOs, 5 JHOs) |
|---|---|---|
| People Present During Evening Handover | • 2 SHOs (75%) • 2 SHOs and a JHO (10%) • 2 SHOs and a SpR (10%) • 2 SHOs, JHO and SpR (5%) |
“Helpful to have a JHO and SpR present at the same handover so everyone is then on the same page.” (3/5 SHOs) |
| Equipment (Technology/Tools) | Two computers and a printer. | “The computer is not working.” (1/10) |
| Task and Job Design | • Handover of admitted patients (100% performed) • Flag sick patients (done only 20% of the time) |
“Sick patients often left out as the house officer is not here.” (3/5 SHOs) “What's going on – on the wards?” (3/5 SHOs) “We often find out about sick patients when we are called because they have got worse.” (3/5 SHOs) “Difficult to handover with the bleep going off again and again.” (2/5 SHOs) |
| Workspace | • 10 × 8 ft room located next to an Orthopaedic ward. • Messy workspaces with handover sheets from weeks (and months) gone by. |
“poor seating” (4/10) “lack of space and becomes crowded” (8/10) |
| Environment | • Thermal comfort – no air conditioning or window. • Overhead lighting was reasonable. • Noise and confidentiality issues – next to a busy corridor. • Slips, trips and falls – none witnessed but a risk in such a small room used by over 25 people (JHOs, SHOs, SpRs). |
“Uncomfortable seating and badly designed desk space.” (6/10) “Very hot!” (10/10) “You don’t feel like staying here long as its so uncomfortable.” (10/10) |
| Organisation | Team working, leadership and inclusion in decision making |
“I feel I should be at handover but I am supposed to finish at 7pm.” (2/5 JHOs) “If the SHO doesn’t answer their bleep when I call them at 7pm before I leave then how can I handover before I leave?” (2/5 JHOs)” “SpR is never here so we don’t have that senior leadership.” (1/5 SHOs)” |
Discussion
The results show that participants had two chief centres of complaint: workspace and environmental issues (a small, hot, uncomfortable room), and the lack of the JHO at handover leading to ‘signal loss’ with respect to sick patients. As an observer of this process, I also noticed that it lacks standardisation and structure with different people handing over in different ways. This can often mean that things are missed out (e.g. sick patients are not handed over).
Structure, standardisation, and checklists help to order complex clinical processes, improve efficiency and safety; for example, the WHO safer surgery checklist which recent research has shown can reduce mortality.21 Several others who have looked at handover seem to support this view. Ferran et al. studied data transfer between shifts at their Orthopaedic unit and found that standardised pro formas encourage filling of relevant fields and increases the data transferred.22 Al Benna et al. examined handover in burns units in the UK and recommended that handovers require a clear and structured format with succinct details to ensure satisfactory information exchange.23 Pfeffer et al. studied 1,130 handovers in a general medical team and found that use of a computerised pro forma and discussion at a handover meeting gave the highest percentage of adequate quality handovers.24
Guidance on safe handover such as Safe handover: safe patients points to numerous examples of good practice including; Hospital at night, intranet based patient lists, and specialty specific approaches.1 Another system of handover is: Think FIRST, developed within Paediatrics.25 Think FIRST is a pneumonic: Find out about; Incidents in the last shift, Risks in the new shift, Sick patients, and Team issues. Each system has its unique set of pros and cons. For instance, Sick patients are hard to talk about if the JHO hasn’t handed them over. This emphasises the need for handover systems to follow guidance. Crucially they must be adapted to local working patterns and conditions if they are to be usable, sustainable, and be respected for the efficiency and safety they deliver.
Fig 1.

Photo illustrating the problems with the workspace – very small and hot with a lack of proper desk space and seating, compounded by a cluttered work area.
Fig 2.
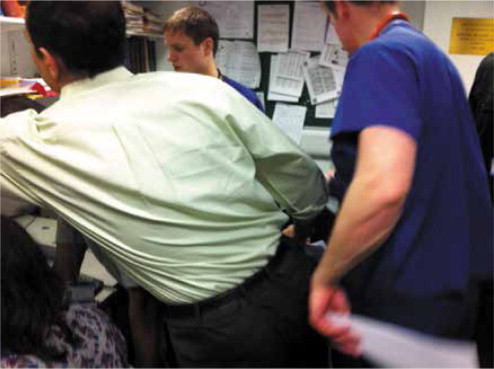
Another photo illustrating the problems with the workspace – very crowded.
Limitations
There were several limitations to this study. With only ten sessions observed, the study is statistically underpowered. However, it does provide a direction for future research inquiry. As people knew they were being observed and interviewed, potential Hawthorne effects may play a role here and people may not be as candid as they would normally. The informal handovers that occur at 17:00, when regular daytime staff leave, were not observed. This may represent an important area of ‘signal loss’. People also have limited time to speak or reflect during the course of a busy day. Approaching people face to face means they are less likely to not answer but will be more guarded than in an anonymous questionnaire. I do feel this personal touch added a lot to the data gathering success. However, such a study may be supplemented by approaching people about their thoughts on handover away from work, in a more social and relaxed setting.
Suggestions for improvement
The current handover process could be improved but requires a broad based approach. Structural constraints should be taken up with management and dealt with (e.g. space and thermal comfort). This requires a coherent voice and support from all parts of the department. A standardised protocol for handover should be developed in consultation with local clinical leads and junior doctors – identifying barriers together and working towards a practical solution. Such efforts should build upon the recommendations set out in the Safe handover: safe patients guide which should be circulated throughout the department.1 In addition, changes should respect the principles of choice architecture,26 that have already been highlighted in recent quality improvement studies.27,28 Essentially we need to make it easier well-meaning people to do the right thing.
Senior clinicians and champions for safer practice together with proactive managers should take the lead in seeing such changes through – taking juniors and their senior colleagues with them. Handover training should be incorporated into hospital induction and postgraduate curricula. Indeed, Safe handover: safe patients proposes that: “Postgraduate deans and the medical royal colleges should include effective handover practice as an essential criterion for granting educational approval of a training grade post.”1 Handover training should also be incorporated into undergraduate curricula.29
Conclusion
Good handover remains a cornerstone of safe and effective clinical practice, and continuity of care. This is especially so in a climate of: increasing patient turnover, shift patterns of working, restricted working hours, an ageing society resulting in a greater proportion of patients with multiple comorbidities, and rising public demands for a safe high quality service. Further research is needed on how we can best stimulate improvements in handover practice and develop specialty specific and locally acceptable standards.
Ethical approval
Not required.
Conflict of interest
Nil.
Author contribution
Single author paper.
Funding
None received.
Open Access: This article is published Open Access at annalsjournal.com. It is distributed under the AMS terms and conditions, which permits unrestricted non commercial use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Footnotes
Provenance and Peer Review
Unsolicited and externally peer-reviewed
References
- 1.British Medical Association, National Patient Safety Agency, NHS Modernisation Agency. Safe handover: safe patients. Guidance on clinical handover for clinicians and managers, 2005 [online]. Available online at: http://www.saferhealthcare.org.uk/IHI/Products/Publications/safehandoversafepatients.htm2005(accessed5April2012).
- 2.Manser T., Foster S. Effective handover communication: an overview of research and improvement effort. Best Pract Res Clin Anaesthesiol. 2011;25(2):181–191. doi: 10.1016/j.bpa.2011.02.006. Jun. [DOI] [PubMed] [Google Scholar]
- 3.Good Medical Practice. General Medical Council, London, 2006. Available at: http://www.gmc-uk.org/guidance/good_medical_practice/GMC_GMP.pdf(accessed5April2012).
- 4.Institute of Medicine. To Err is Human: Building A Safer Health System [online]. Available at: http://www.iom.edu/Reports/1999/To-Err-is-Human-Building-A-Safer-Health-System.aspx(accessed5April2012).
- 5.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century [online]. Available at: http://www.iom.edu/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx(accessed5April2012).
- 6.Donaldson L. An organisation with a memory. Department of Health. Available at: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4065086.pdf(accessed5April2012).
- 7.Giraud T., Dhainaut J.F., Vaxelaire J.F., Joseph T., Journois D., Bleichner G. Iatrogenic complications in adult intensive care units: a prospective two-center stud. Crit Care Me. 1993;21:40–51. doi: 10.1097/00003246-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Tourgeman-Bashkin O., Shinar D., Zmora E. Causes of near misses in critical care of neonates and childre. Acta Paedia. 2008;97(3):299–303. doi: 10.1111/j.1651-2227.2007.00616.x. [DOI] [PubMed] [Google Scholar]
- 9.Roughton V., Severs M. The junior doctor handover: current practices and future expectation. J Royal College Physicians Londo. 1996;30:213–214. [PMC free article] [PubMed] [Google Scholar]
- 10.Todkode M., O’Riordan B., Bartholmes L. That's all I got handed over: missed opportunities and opportunity for near misses in Wale. BM. 2006;332:610. doi: 10.1136/bmj.332.7541.610-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Todkode M., O’Riordan B., Bartholmes L. Near-misses and missed opportunities: poor patient handover in general surger. Ann R Coll Surg Engl (Suppl. 2008;90:96–98. [Google Scholar]
- 12.High 5s. High 5s project action on patient safety [online]. Available at: https://www.high5s.org/pub/Manual/TrainingMaterials/High5sProjectOverviewFactSheet.pdf.2006 (accessed5April2012).
- 13.Joint Commission on Accreditation of Healthcare Organisations. JCAHO National patient safety goals for 2007 [online]. Available at: http://www.patientsafety.gov/TIPS/Docs/TIPS_JanFeb07.pdf(accessed5April2012). [PubMed]
- 14.Council Directive 93/104/EC. Official Journal of the European Community 1993;L307:18-24.
- 15.Reason J. Safety in the operating theatre – Part 2: Human error and organisational failure. Qual Saf Health Car. 2005;14:56–61. [PMC free article] [PubMed] [Google Scholar]
- 16.Carayon P., Schoofs Hundt A., Karsh B.T., Gurses A.P., Alvarado C.J., Smith M., Flatley Brennan P. Work system design for patient safety: the SEIPS mode. Qual Saf Health Care. 2006;15(Suppl 1):i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frimley Park NHS Foundation Trust. Annual Report and Accounts 2010-2011 [online]. Available from: www.frimleypark.nhs.uk/images/stories/about_us/publications/Annual_ Report_2010-11.pdf(accessed17July2012).
- 18.Catchpole K.R., Giddings A.E., de Leval M.R., Peek G.J., Godden P.J., Utley M., Gallivan S., Hirst G., Dale T. Identification of systems failures in successful paediatric cardiac surger. Ergonomics. 2006;15(5-6):567–588. doi: 10.1080/00140130600568865. 49. [DOI] [PubMed] [Google Scholar]
- 19.Catchpole K.R., Giddings A.E., Wilkinson M., Hirst G., Dale T., de Leval M.R. Improving patient safety by identifying latent failures in successful operation. Surgery. 2007;142(1):102–110. doi: 10.1016/j.surg.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 20.Adair G. The Hawthorne effect: a reconsideration of the methodological artefact. Appl Psycho. 1984;69(2):334–345. [Google Scholar]
- 21.van Klei W.A., Hoff R.G., van Aarnhem E.E., Simmermacher R.K., Regli L.P., Kappen T.H., van Wolfswinkel L., Kalkman C.J., Buhre W.F., Peelen L.M. Effects of the introduction of the WHO “Surgical Safety Checklist” on in-hospital mortality: a cohort stud. Ann Surg. 2012;255(1):44–49. doi: 10.1097/SLA.0b013e31823779ae. [DOI] [PubMed] [Google Scholar]
- 22.Ferran N.A., Metcalfe A.J., O’Doherty D. Standardised proformas improve patient handover: Audit of trauma handover practic. Patient Saf Surg. 2008;25(2):24. doi: 10.1186/1754-9493-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Benna S., Al-Ajam Y., Alzoubaidi D. Burns surgery handover study: Trainees’ assessment of current practice in the British Isle. Burn. 2009;35(4):509–512. doi: 10.1016/j.burns.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 24.Pfeffer P.E., Nazareth D., Main N., Hardoon S., Choudhury A.B. Are weekend handovers of adequate quality for the on-call general medical team. Clin Med. 2011;11(6):536–540. doi: 10.7861/clinmedicine.11-6-536. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macauley C and Rees C. Think FIRST! [online]. Available at: http://blogs.bmj.com/agentsforchange/files/2010/07/think-first.pdf(accessed5April2012).
- 26.Sunstein C., Thaler R. Yale University Press; New Haven: 2008. Nudge: Improving Decisions about Health Wealth, and Happiness. [Google Scholar]
- 27.Agha RA, Camm CF, Edison E and Browning N. Improving Compliance with Statins in Patients with Peripheral Arterial Disease: A Quality Improvement Study. Annals of Medicine and Surgery 2012; 1(1) (In Press). [DOI] [PMC free article] [PubMed]
- 28.Agha RA, Edison E, Camm CF, Cheng L, Gajendragadkar P and Borland C. Improving Compliance with NICE Guidelines on Parkinson's Disease: A Quality Improvement Study. Annals of Medicine and Surgery 2012; 1(1) (In Press). [DOI] [PMC free article] [PubMed]
- 29.McGlynn M.C., Scott H.R., Thomson C., Peacock S., Paton C. How we equip undergraduates with prioritisation skills using simulated teaching scenario. Med Teach. 2012;34(7):526–529. doi: 10.3109/0142159X.2012.668235. [DOI] [PubMed] [Google Scholar]


