Abstract
Objective. To evaluate the feasibility of an online training module, Certified Smoking Cessation Service Provider (CSCSP), developed for practicing pharmacists to equip pharmacy students with knowledge necessary for smoking cessation counseling and to assess the changes in student knowledge and skills regarding smoking cessation following training.
Design. Sixty third-year and 80 fourth-year pharmacy undergraduates (N=140) were given access to an online module, the main intervention in the study. Two linkable questionnaires were administered to assess students’ preintervention and postintervention knowledge. For the third-year students, an additional role-play training component was incorporated, and student skills were assessed during week 14 with an Objective Structured Clinical Examination (OSCE).
Assessment. Preintervention and postintervention knowledge assessments were completed by 130 (92.8%) students. Sixty-six students scored above 50% for the knowledge component postintervention, compared to 13 at preintervention, demonstrating significant improvement (x2(1, N=130)=32, p=0.003). All third-year students completed the intervention, and 66.7% were able to counsel excellently for smoking cessation, scoring more than 80%.
Conclusion. The CSCSP online module developed for practicing professionals was found suitable for equipping pharmacy undergraduates with knowledge on smoking cessation topics. The module, along with role-play training, also equipped students with knowledge and skills to provide smoking cessation counseling.
Keywords: smoking cessation, pharmacy undergraduates, active learning, Malaysia, pharmacy curricula
INTRODUCTION
Smoking is a major public health problem, causing an estimated 5 million people, including 10 thousand Malaysians,1 to die prematurely each year. Comprehensive evidence-based tobacco control programs that combine educational, clinical, regulatory, economic, and social strategies reduce the health burden of smoking.2 The Malaysian Quit Smoking Programme formulated a strategy to integrate smoking cessation programs into all relevant health care curricula, with the goal of providing comprehensive support for helping smokers quit.3
Internationally, the importance of such training is reflected in the recommendations that all health care students should receive education in the treatment of tobacco use and dependence during their professional training years.4-6 Nevertheless, studies repeatedly show that most students, including pharmacy undergraduates, lack the necessary knowledge and skills.6,7 We found only 13.4% of 127 students scored above 50% in the knowledge assessment of tobacco-related and smoking cessation counseling component from our preliminary study conducted among pharmacy students.8
In Malaysia, the bachelor of pharmacy degree is offered as a 4-year program consisting of an average of 150 credit hours whereby one credit hour involves approximately 40 hours of students learning time, which consists of face-to-face and self-directed learning time. A survey on the tobacco-related curricula among all the pharmacy schools across Malaysia found the median teaching duration for tobacco-related topics was around 2.75 hours for core courses and 2 hours for elective courses.8
Babar et al reported that opportunities exist for Malaysian pharmacists to render services in smoking cessation.9 Despite these opportunities, Malaysian pharmacists were not contributing optimally in this area.10,11 Lack of comprehensive tobacco-related courses and training in most universities’ curricula was cited as a major contributing factor, as well as lack of in-service training and continuing professional development (CPD) programs focusing on the subject.10 The latter issue was addressed through the initiation of the Certified Smoking Cessation Service Provider (CSCSP) program in 2004.The main objective of CSCSP was to provide Malaysian health care professionals with additional, specialized counseling skills to help smokers quit the habit. In August 2010, the online CSCSP module was launched to encourage more participation from practitioners by making the training available at their convenience.12
Several studies on web-based training for pharmacy students on smoking cessation counseling reported positive outcomes.13,14 Studies utilizing active-learning strategies to provide students with knowledge and skills for smoking cessation counseling also reported positive outcomes.15-17 However, none of these studies used modules developed for practicing health care professionals. In our study, the CSCSP module designed for practicing health care professionals was tested for its suitability to equip undergraduate pharmacy students with knowledge and skills at graduation to assist smokers with quitting.
We incorporated the online CSCSP module and role-playing into 2 courses engaging the third-year and fourth-year students at one institution. The main aim of this study was to evaluate the suitability of the module in providing pharmacy students with the knowledge necessary to provide smoking cessation counseling. We also evaluated third-year students’ skills pertaining to smoking cessation counseling following exposure to CSCSP and role-play.
DESIGN
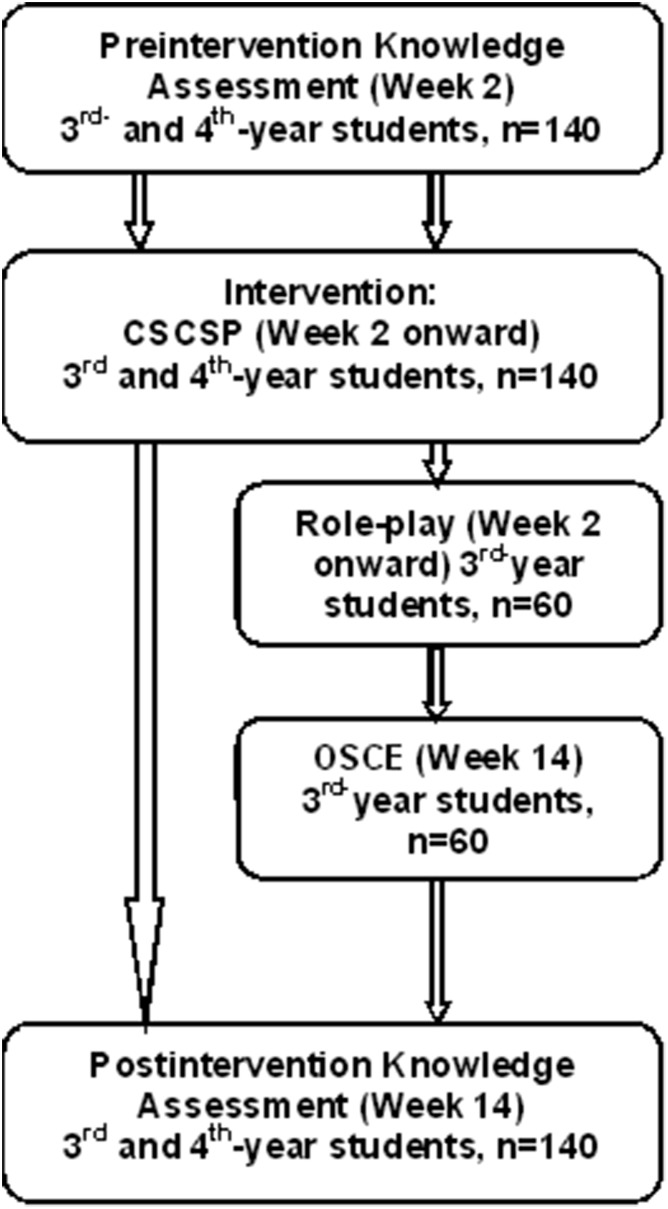
Pharmacy undergraduates for the academic year of 2011-2012 were recruited through convenience sampling from one institution. One hundred forty students were recruited, 60 third-year students and 80 fourth-year students. Third-year students had prior exposure to the basics of patient counseling, and fourth-year students had the opportunity to provide pharmaceutical care during their community and hospital rotations. The fourth-year students, who had exposure to tobacco-related topics the previous semester, were assessed only on the knowledge component while the third-year students, who had no prior exposure to tobacco-related topics, were assessed for knowledge and skills to provide smoking cessation counseling during the OSCE, as depicted in Figure 1. An exemption was obtained from the institutional review board where the study was conducted.
Figure 1.
Participation and Intervention by Year of Study (CSCSP=certified smoking cessation service provider; OSCE=objective structured clinical examination).
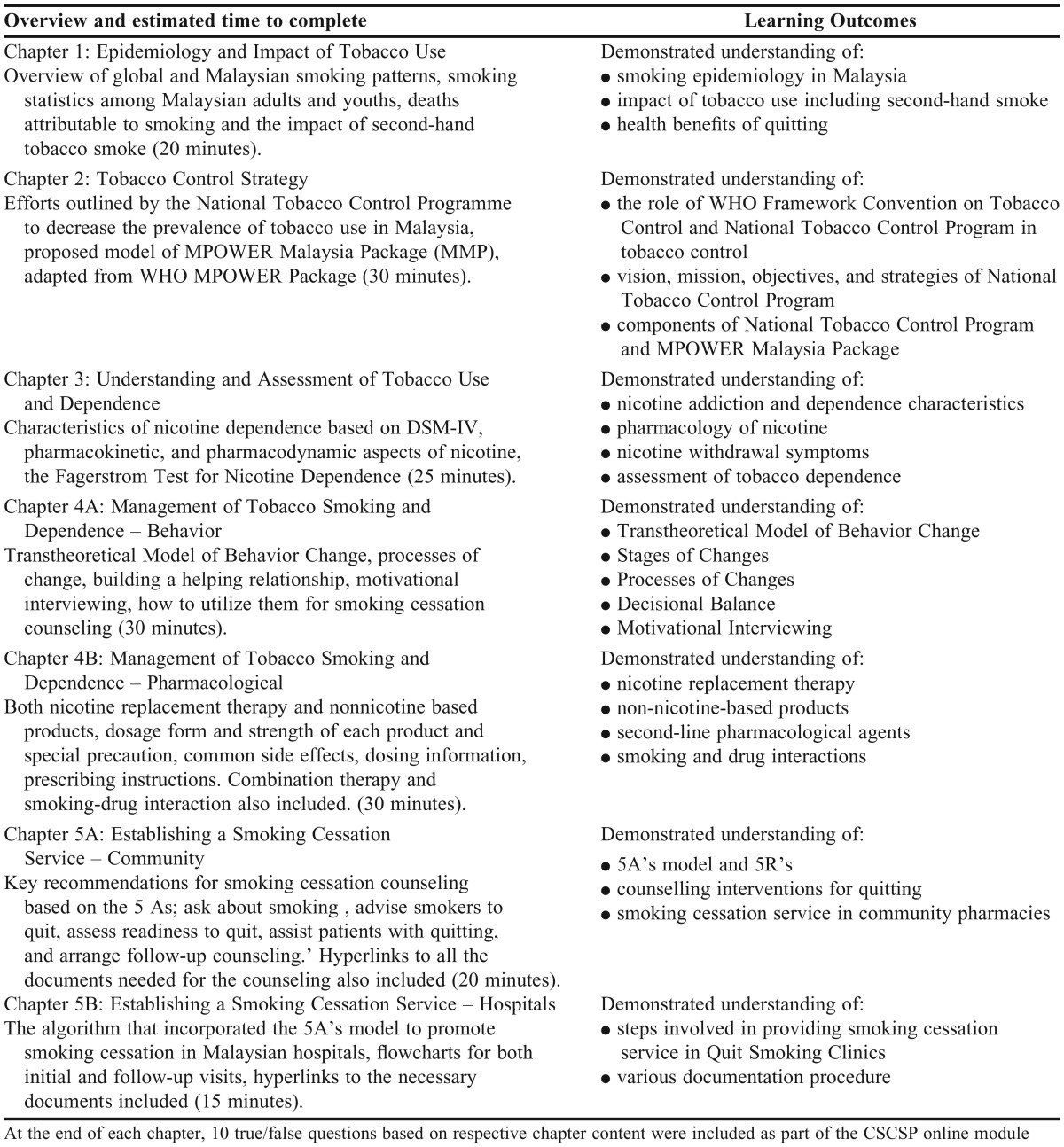
The existing CSCSP online module allowed convenient access for participants. The module could be easily integrated into the already tight curricula for the pharmacy program at this institution. A brief overview of the chapters, learning outcomes, and estimated time to complete each chapter in the module is outlined in Table 1. A pilot-test was administered to estimate the average time to complete the module; value, ease of use, comprehensiveness, quality, and module design were also assessed in the pilot-test. The training for the fourth-year students involved only CSCSP online intervention.
Table 1.
Overview and Learning Outcomes of the Chapters in the Certified Smoking Cessation Service Provider (CSCSP) Online Module
In addition to the online module, the third-year students were given access to 7 role-play scripts, which were uploaded to the learning management system of the institution. The scripts were developed based on the “5A’s” model for smoking cessation counseling (ask, advise, assess, assist and arrange follow-up)18 and incorporated scenarios at different difficulty levels. Skills were assessed through an OSCE for the third-year students only. The students were asked to practice the role-play scripts with group members as preparation for the OSCE, which was scheduled in week 14.
Changes in participant knowledge were assessed using the same set of 14 multiple-choice questions. Preintervention knowledge was assessed in the second week prior to CSCSP access, while postintervention knowledge was assessed at week 14. A linkable questionnaire was aligned to the chapters in the CSCSP module to assess students’ tobacco-related and smoking cessation counseling knowledge. Two questions per chapter covered the essential topics of the module and only correct answers were given points. These questions were pretested with 9 students. The average difficulty index for all 14 questions was 0.45, determined by calculating the average ratio of correct answers to all questions attempted by students. A question was considered difficult if the index was below 0.30. Index value above 0.70 indicated an easy question. Ideally, the difficulty index should be in the range of 0.50 to 0.60.19
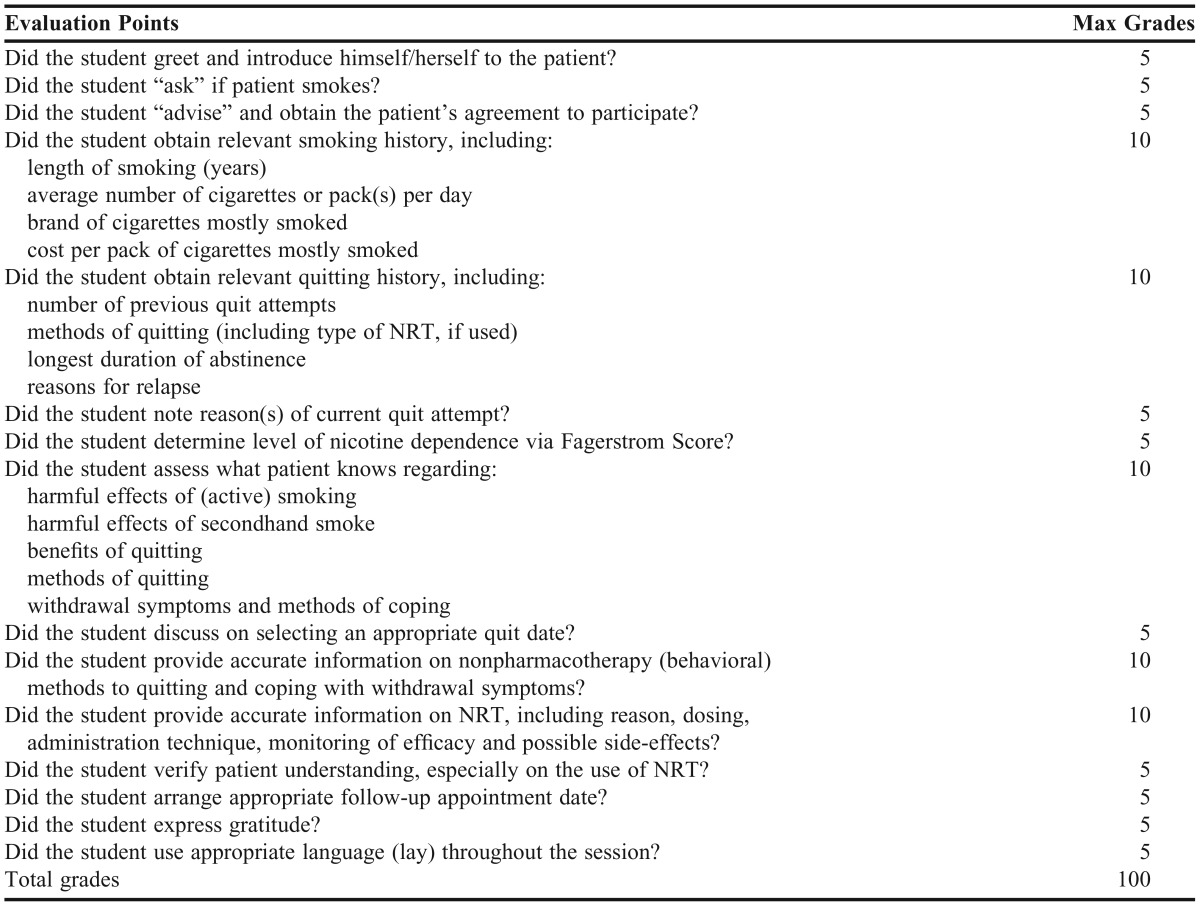
The rubric for awarding points for the counseling skill component during the OSCE was adapted from the CSCSP attachment checklist (Table 2). This rubric was mainly based on the 5A’s model for smoking cessation counseling; other relevant criteria for general counseling skills were also included. In dealing with patients, students were encouraged to use layman’s terms rather than medical terminology. Examiners at each of the 3 stations assessed the students’ skills using the grading rubrics, adapted to the respective cases at their station. Two faculty members developed 3 cases, one of which included a smoker, for the OSCE. The cases and the grading rubrics were reviewed for content and clarity by 2 other faculty members, and changes suggested were incorporated and reviewed a final time. Only one of the 3 cases included assessed students’ skills at smoking cessation counseling; the remaining 2 assessed students’ability to counsel for the correct usage of peak flow meter and inhalers. Participants were required to ask all patients about smoking. Three laboratory technicians were recruited to play the role of patients and were instructed not to provide information unless they clearly understood the students’ requests.
Table 2.
Objective Structured Clinical Examination (OSCE) Grading Rubrics
During the second week of the semester, preintervention knowledge was assessed among all participating students. Following this, students were given access to the module. An OSCE was conducted in week 14 of the semester for the third-year students, during which their smoking cessation counseling skills were assessed. At the end of week14, a linkable questionnaire using the same set of 14 multiple-choice questions to assess postintervention knowledge was made available to participants. The preintervention and postintervention knowledge assessment was conducted by distributing the questionnaire in-person.
Paired t tests were used to analyze knowledge scores before and after the intervention, and chi-square tests determined the change in proportion of students scoring above 50%. The knowledge scores were subjected to a 2-way analysis of variance (ANOVA) for the module intervention (before, after) and role-play intervention (exposed, not exposed) to determine the impact of the interventions on changes in knowledge scores. Descriptive statistics were computed as percentages for the OSCE based on the grades awarded for the skill assessment.
EVALUATION AND ASSESSMENT
The preintervention and postintervention survey instruments were completed by 130 students, yielding a 92.9% overall response rate, of which 77 were fourth-year students and 53 were third-year students. The mean age and its standard deviation for participating students were 22.5(0.6) for fourth-year students and 21.1(0.7) for third-year students. The majority of the participants were female—75% of the fourth-year students (n=58) and 72% of the third-year students (n=38).
There was significant improvement in preintervention to postintervention mean knowledge scores among all students, with slightly higher improvement among third-year students, who had exposure to the role-play intervention (Table 3). The number of students who scored above 50% for the knowledge component improved significantly from 13 at preintervention to 66 at postintervention: x2(1, N=130)=32, p=0.003. The lowest grades were obtained for questions pertaining to pharmacology of nicotine and behavioral changes, yielding difficulty indices of 0.20 and 0.15, respectively, at preintervention. These improved to 0.87 and 0.78, respectively, following the online module intervention. The highest preintervention scores were obtained for questions on nicotine withdrawal and second-hand smoke health effect, yielding the difficulty indices of 0.80 and 0.74, respectively, with slight improvement noticed for both at postintervention. The average difficulty index for the remaining questions improved fairly from 0.30 at preintervention to 0.70 at postintervention.
Table 3.
Preintervention and Postintervention Knowledge Scoresa
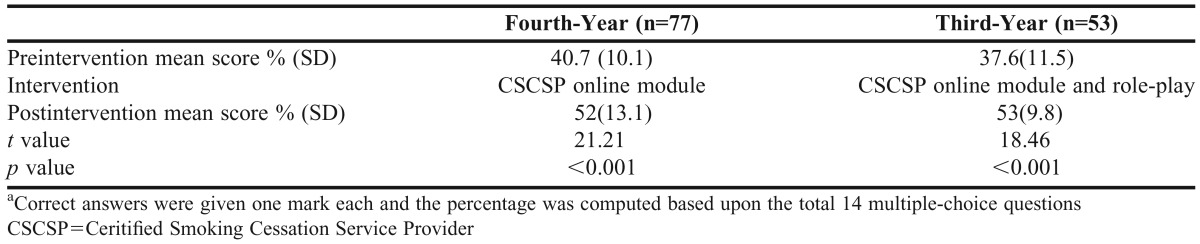
From the results of the 2-way ANOVA, the main effect of the module intervention was significant with higher knowledge scores at postintervention (M=52.5%, SD=11.9) than at preintervention (M=39.4%, SD=10.8). The interaction effect was significant, F (1,128)=5.81, p=0.017, indicating the impact of the module intervention was slightly greater among students who also had exposure to the role-play intervention. However, the main effect of the role-play intervention was not significant in terms of knowledge score improvement: F (1, 128)=1.59, p=0.112.
Sixty third-year students completed the OSCE, a 100% response rate, which resulted from this component being included as part of the continuous assessment for the semester. Approximately 66.7% of students were able to counsel excellently for smoking cessation, scoring more than 80%.The lowest grades obtained were 45%, while the highest were 95%. Almost all students performed the first 2A’s (ie, ask and advise). Approximately two thirds managed to proceed smoothly to the next steps, (ie, assess, assist, and arrange follow-up). Apart from the 5A-based tasks, which accounted for 85% of the total grades, students were also assessed on their general counseling skills, such as using layman terms and expressing gratitude to the patients for their time and willingness to participate and listen, which are considered good counseling practices.
DISCUSSION
Our findings indicated that students’ knowledge pertaining to smoking cessation counseling improved following the CSCSP online intervention. This is consistent with the findings of Brown and Janke, who reported significant improvement for knowledge scores, (from preintervention of 36.3% to 84.5% at postintervention) following a web-based training.13 Although the mean improvement of knowledge score in our study was less than that noted in Brown and Janke’s study, the difference could be explained by the 12-week lapse between intervention knowledge assessments in our study vs the 2 to 3 weeks between assessments in the Brown and Janke study.
Although the fourth-year students in our study had exposure to tobacco-related topics the previous semester, the preintervention knowledge scores were relatively low with a mean of 40.7 (10.1%). This suggests that continuous emphasis on training regarding the importance of tobacco-related and smoking cessation counseling should be placed throughout the undergraduate program, and faculty members involved should view this training as a process rather than one-time event. Follow up is therefore necessary.
We found the third-year students had slightly higher improvement in the knowledge component. However, the knowledge assessment in this study was aligned to the content of the CSCSP module, which may explain the reason for the role-play intervention alone not contributing significantly to the knowledge score gain. Yet, active learning such as role-play improves students’ confidence and skill in providing smoking cessation counseling, and the active-learning process involving role-play did contribute to their ability to provide smoking cessation counseling, assessed during the OSCE.15,16 In our study, two-thirds of the third-year students were able to provide smoking cessation counseling appropriately following the module and role-play interventions, corroborating findings from other studies.15-17
In this study, a major limitation was that we did not know if students accessed the CSCSP online module. The module was incorporated as optional reading material, and its content was not assessed as part of their final examination. However, an effort was made to encourage students to use the module and the multiple-choice questionsin the knowledge assessment were aligned to the module content. A question could have been included in the questionnaire to ascertain whether students had accessed the module. Another limitation was that students’ skills to counsel before the role-play and CSCSP interventions were not determined. Lastly, since the sample was obtained from only one institution, the generalizability of the findings is limited. Moreover, the study lacked a control group and a large sample size.
SUMMARY
The Certified Smoking Cessation Service Provider (CSCSP), an online module developed for practicing professionals, was found suitable in equipping pharmacy undergraduates with knowledge on smoking cessation topics. Students’ counseling skills were encouraging following role-play training and CSCSP intervention. Students should be given continuous encouragement and opportunities throughout the undergraduate program to practice such skills and reinforce the knowledge obtained. Training for smoking cessation counseling should be seen as an ongoing process rather than as one-time event.
ACKNOWLEDGMENTS
The authors would like to thank the students who participated in this study for their contribution, the Malaysian Academy of Pharmacy, and the Malaysian Pharmaceutical Society for their support.
REFERENCES
- 1.Ministry of Health. Clinical Practice Guidelines: Treatment of Tobacco Smoking and Dependence. Ministry of Health Malaysia and Academy of Medicine; 2003.
- 2.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2007. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; October 2007.
- 3.Zain Z. Malaysian Smoking Cessation Programme and Smoke-Free Air Laws. Asia Pacific Regional Conference; Kuala Lumpur: 2007. [Google Scholar]
- 4.Raw M, Anderson P, Batra A, et al. WHO evidence based recommendations on the treatment of tobacco dependence. Tob Control. 2001;11:44–46. doi: 10.1136/tc.11.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence: clinical practice guideline.US Department of Health and Human Services. Public Health Service. 2000 [Google Scholar]
- 6.Warren CW, Jones Sinha DN, Lee J, Lea V, Jones NR. Tobacco use and cessation counseling among pharmacy students. J Behav Health. 2013;2(1):8–18. [Google Scholar]
- 7.Hudmon KS, Bardel K, Kroon LA, Fenlon CM, Corelli RL. Tobacco education in US schools of pharmacy. Nicotine Tob Res. 2005;7(2):225–232. doi: 10.1080/14622200500055392. [DOI] [PubMed] [Google Scholar]
- 8.Simansalam S, Mohamed MHN. Equipping pharmacy undergraduates with knowledge and skills on smoking cessation intervention: Findings from environmental scan of universities curricula and assessment of students’ knowledge. Malaysian J Pharm. 2011;1(9):399. [Google Scholar]
- 9.Babar Z, Bukhari NI, Sarwar W, Efendie B, Pereira R, Mohamed MH. A preliminary study on the effect of pharmacist counseling on awareness of and willingness to quit smoking in malaysian Population. Pharm World Sci. 2007;29(3):101–103. doi: 10.1007/s11096-005-2905-4. [DOI] [PubMed] [Google Scholar]
- 10.Awaisu A, Mohamed MHN, Noordin NM, et al. Potential impact of a pilot training program on smoking cessation intervention for tuberculosis DOTS providers in Malaysia. J Public Health. 2010;18(3):279–288. [Google Scholar]
- 11.Lee ML, Hassali MA, Shafie AA, Abd Aziz A. M. Challenges of pharmacist-managed smoking cessation services—a viewpoint. Nicotine Tob Res. 2011;13(6):504–505. doi: 10.1093/ntr/ntr052. [DOI] [PubMed] [Google Scholar]
- 12. Malaysian Academy of Pharmacy, Malaysian Pharmaceutical Society. http://www.acadpharm.org.my/index.cfm?&menuid=2. Accessed on March 3, 2015.
- 13.Brown MC, Janke KK. Impact of an internet-based smoking cessation educational module on pharmacists’ knowledge and practice. Am J Pharm Educ. 2003;67(4) Article 107. [Google Scholar]
- 14.Schmelz AN, Nixon B, McDaniel A, Hudmon KS, Zillich AJ. Evaluation of an online tobacco cessation course for health professions students. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740236. Article 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hudmon KS, Kroon LA, Corelli RL, et al. Training future pharmacists at a minority educational institution: Evaluation of the Rx for Change tobacco cessation training program. Cancer Epidemiol Biomarkers Prev. 2004;13(3):477–481. [PubMed] [Google Scholar]
- 16.Corelli RL, Kroon LA, Chung EP. Statewide evaluation of a tobacco cessation curriculum for pharmacy students. Prev Med. 2005;40(6):888–895. doi: 10.1016/j.ypmed.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Saba M, Bittoun R, Saini B. A workshop on smoking cessation for pharmacy students. Am J Pharm Educ. 2013;77(9) doi: 10.5688/ajpe779198. Article 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rx for Change: Clinician-assisted tobacco cessation. Smoking Cessation Leadership Center. http://rxforchange.ucsf.edu/curricula/ask_advise.php. Accessed on 5 Oct 2014.
- 19.Ananthakrishnan N. Item analysis-validation and banking of MCQs. In N. Ananthkrishnan, K.R. Sethuraman & S. Kumar. Medical Education Principles and Practice. Pondichery: JIPMER; 2000:131–137.