Abstract
Background
Left atrial volume (LAV) is a predictor of prognosis in patients with heart failure.
Objective
We aimed to evaluate the determinants of LAV in patients with dilated cardiomyopathy (DCM).
Methods
Ninety patients with DCM and left ventricular (LV) ejection fraction ≤ 0.50 were included. LAV was measured with real-time three-dimensional echocardiography (eco3D). The variables evaluated were heart rate, systolic blood pressure, LV end-diastolic volume and end-systolic volume and ejection fraction (eco3D), mitral inflow E wave, tissue Doppler e´ wave, E/e´ ratio, intraventricular dyssynchrony, 3D dyssynchrony index and mitral regurgitation vena contracta. Pearson´s coefficient was used to identify the correlation of the LAV with the assessed variables. A multiple linear regression model was developed that included LAV as the dependent variable and the variables correlated with it as the predictive variables.
Results
Mean age was 52 ± 11 years-old, LV ejection fraction: 31.5 ± 8.0% (16-50%) and LAV: 39.2±15.7 ml/m2. The variables that correlated with the LAV were LV end-diastolic volume (r = 0.38; p < 0.01), LV end-systolic volume (r = 0.43; p < 0.001), LV ejection fraction (r = -0.36; p < 0.01), E wave (r = 0.50; p < 0.01), E/e´ ratio (r = 0.51; p < 0.01) and mitral regurgitation (r = 0.53; p < 0.01). A multivariate analysis identified the E/e´ ratio (p = 0.02) and mitral regurgitation (p = 0.02) as the only independent variables associated with LAV increase.
Conclusion
The LAV is independently determined by LV filling pressures (E/e´ ratio) and mitral regurgitation in DCM.
Keywords: Heart Atria; Organ Size; Cardiomyopathy, Dilated; Chagas Cardiomyopathy; Echocardiography, Three-Dimensional
Introduction
Left Atrial Volume (LAV) is a predictor of cardiovascular events in the general population1,2 and in patients with cardiac failure3-6. Moreover, LAV is associated with the presence of symptoms in these patients3.
Although left atrial dilatation is a marker of left ventricular7 (LV) diastolic dysfunction and can occur secondarily to mitral regurgitation, it is not clear what are the determinants of left atrial enlargement in patients with dilated cardiomyopathy (DCM). Thus, the objective of this study is to evaluate the determinants of LAV in patients with non-ischemic DCM and LV systolic dysfunction.
Methods
Patients
The study included 90 outpatients with DCM; 60 patients with idiopathic DCM (idiopathic defined as dilated cardiomyopathy in the absence of known causes that reslt in this condition; coronary artery disease was excluded by coronary angiography or epidemiology; primary valve disease was excluded by two-dimensional echocardiography; other causes of dilated cardiomyopathy were excluded according to epidemiological and clinical data), and 30 patients with Chagas cardiomyopathy (two positive tests for antibodies to Trypanosoma cruzi). Patients were consecutively recruited from a tertiary care center for patients with heart failure and cardiomyopathies. Inclusion criteria were age ≥ 18 years, functional class I, II or III (New York Heart Association), optimal medical treatment for heart failure, sinus rhythm, LV ejection fraction ≤ 0.50 (modified Simpson method) and echocardiography good image quality. Patients with primary valvular disease, hypertension, coronary artery disease, end-stage kidney disease or chronic obstructive pulmonary disease were excluded. All patients signed an informed consent form and the study was approved by the ethics committee of the institution.
The height and weight were obtained to calculate the body surface area. Heart rate and systolic and diastolic blood pressure were also recorded before the echocardiography.
Echocardiography and Tissue Doppler
All subjects underwent a two-dimensional echocardiography with Doppler in an IE33 device (Philips, Andover, Massachusetts) with a 1-5 MHz transducer under continuous electrocardiographic monitoring. The patients were studied in the left lateral decubitus position by the same echocardiographist. LV ejection fraction was estimated by the modified Simpson's method.
Mitral regurgitation was quantified by the vena contracta. LV diastolic function was assessed by analyzing the velocities of initial (E) and final (A) waves of the mitral inflow obtained from pulsed Doppler and by the velocity of the initial wave (e') of the septal mitral annulus obtained by tissue Doppler. These data were used to calculate the E/e' ratio as an estimate of filling pressures of LV8,9.
The intraventricular mechanical dyssynchrony of the LV was assessed by color tissue Doppler (color-TD). The volume sample was positioned in the LV six basal segments. The time interval between the beginning of the QRS of the electrocardiographic tracing to the systolic velocity peak of each segment10,11 was measured. The intraventricular delay was calculated by the maximum difference between the intervals of all segments11,12.
Real-time three-dimensional echocardiography
The real-time three-dimensional echocardiography (eco3D) was used to obtain the LAV and 3D dyssynchrony index of the LV. The same IE33 echocardiography device, with a X3 (1-3 MHz) matrix transducer, was used to acquire the full volume, real-time pyramidal volumetric data for four consecutive cardiac cycles. To ensure the inclusion of the entire volume of the LA and LV inside the pyramidal volume, data were acquired using the wide-angle mode, thus acquiring four wedge-shaped sub-volumes for a period of 5 seconds of apnea. The eco3D data were digitally stored and analyzed using the QLAB-Philips software (version 5.0; Philips Medical Systems). The three-dimensional echocardiographic images analysis was based on the apical window and semi-automatic tracing of the endocardial borders.
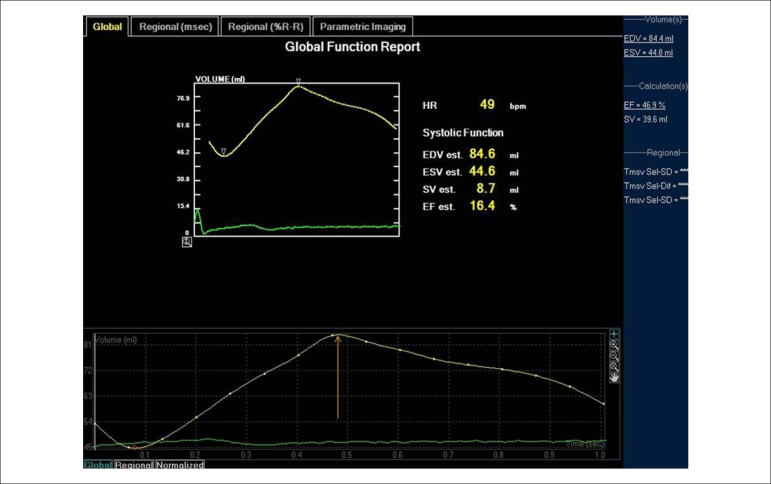
The analysis of the left atrium was performed by marking four points on the atrial surface of the mitral annulus: septal, lateral, anterior and inferior, and a fifth point in the left atrial roof. Subsequently, the endocardial surface was automatically outlined and could be visualized from different views. Manual modifications were made to correct the automatic tracing when necessary13 and then the software generate a variation curve of the LAV throughout the cardiac cycle (Figure 1). The LAV was considered the peak of the curve and the value was indexed by the body surface area (LAVi).
Figure 1.
Left atrium volume. The figure shows the variation of the left atrium volume during the cardiac cycle. The arrow indicates the maximum volume of the left atrium.
The LV analysis was performed by marking four points on the surface of the mitral annulus: anterior, inferior, lateral and septal, and a fifth point in the LV apex. Subsequently, the endocardial surface was automatically outlined and could be visualized from different views. Manual modifications were made to correct the automatic tracing when necessary14. The LV 3D dyssynchrony index was calculated from the standard deviation of the cardiac cycle fraction that each LV segment took to reach its minimum volume. The index is expressed as a percentage of the cardiac cycle duration15.
Statistical analysis
Statistical analysis was performed with SPSS 13.0 software (SPSS Inc, Chicago, IL). Continuous data are reported as mean ± SD and categorical data as percentage. The Kolmogorov-Smirnov test showed that the sample had normal distribution. Pearson´s correlation coefficient was used to identify the correlation of LAVi with heart rate, systolic blood pressure, LV end-diastolic and end-systolic volumes, LV ejection fraction, mitral inflow E wave velocity, e´ wave velocity, E/e´ ratio, intraventricular mechanical dyssynchrony of the LV, 3D dyssynchrony index and mitral regurgitation vena contracta.
A multiple linear regression model was performed, including LAVi as the dependent numerical variable and the variables correlated with it as predictive variables. The p-value was considered significant when < 0.05. The coefficient of variation was used to assess inter and intra-variability of the LAV measurement in a random sample of 20 patients.
Results
Clinical data
The baseline clinical characteristics of the patients are shown in Table 1. The mean age was 53 ± 11 years and 63 (70%) patients were males. The etiology of the dilated cardiomyopathy was idiopathic dilated cardiomyopathy in 60 (67%) patients and Chagas cardiomyopathy in 30 (33%) patients. The functional class was I in 7 (8%) patients, II in 55 (61%) patients and III in 28 (31%) patients. All patients were receiving beta-blockers (76% carvedilol, 48 ± 6 mg/day, and 24% metoprolol, 178 ± 43 mg/day), ACE inhibitors (62% captopril, 133±24 mg/day, and 38 % enalapril 31 ± 10 mg/day) and furosemide (97 ± 62 mg/day). Of the 90 patients, 81 (90%) were using spironolactone and 20 (22%) used digoxin.
Table 1.
Baseline clinical characteristics of the patients
| n = 90 patients | |
|---|---|
| Age (years) | 53 ± 11 |
| Male gender (%) | 63 (70%) |
| BSA (kg/m2) | 1,73 ± 0.17 |
| HR (bpm) | 69 ± 12 |
| SBP (mmHg) | 109 ± 20 |
| DBP (mmHg) | 69 ± 14 |
| Idiopathic dilated cardiomyopathy (%) | 60 (67%) |
| Chagas cardiomyopathy (%) | 30 (33%) |
| FC I | 7 (8%) |
| FC II | 55 (61%) |
| FC III | 28 (31%) |
Values expressed as mean ± standard deviation or frequency (%). BSA: body surface area; FC: NYHA functional class; HR: heart rate; NYHA: New York Heart Association; DBP: diastolic blood pressure; SBP: systolic blood pressure.
Echocardiography data
Data from the two-dimensional Doppler echocardiography are shown in Table 2. The mean LV ejection fraction was 31.5 ± 8.0 % and the restrictive filling pattern was present in 24 (27%) patients. The mean E/e´ ratio was 17.3 ± 8.2, and the mean systolic pressure in the pulmonary artery was 43 ± 13 mmHg. Functional mitral regurgitation was present in 80 (89%) patients; the mean mitral regurgitation vena contracta was 0.43 ± 0.16; 18 (20%) patients had mild, 54 (60%), moderate and only 8 (9%) patients had severe mitral regurgitation. The intraventricular mechanical delay was 67 ± 43 ms and the 3D dyssynchrony index was 5.6 ± 5.3%.
Table 2.
Echocardiographic data
| n = 90 patients | |
|---|---|
| LA Diameter | 46.2 ± 5.6 mm |
| LAV - 3D | 67.9 ± 27.3 ml/m2 |
| LAVi - 3D | 39.2 ± 15.7 ml/m2 |
| LVEDV | 267 ± 103 ml |
| LVESV | 187 ± 86 ml |
| LVEF (%) | 31.5 ± 8.0 % |
| E wave | 78.2 ± 30.9 cm/s |
| A wave | 67.4 ± 31.7 cm/s |
| E/A ratio | 1.4 ± 1.5 |
| Restrictive filling pattern | 27% |
| e' wave | 4.9 ± 1.8 cm/s |
| E/e' ratio | 17.3 ± 8.2 |
| MR-VC | 0.43 ± 0.16 cm |
| PASP | 43 ± 13 mmHg |
| Intraventricular mechanical delay | 67 ± 43 ms |
| 3D dyssynchrony index | 5.6 ± 5.3% |
Values expressed as mean ± standard deviation or frequency (%). LA; left atrium; LVEF: left ventricular ejection fraction; PASP: pulmonary artery systolic pressure; LAV; left atrium volume; LAVi; left atrial volume indexed for body surface; MR-VC; mitral regurgitation vena contracta; LVEDV; end-diastolic volume of the left ventricle; LVESV; end-systolic volume of the left ventricle.
Echocardiographic data of the left atrium
The anteroposterior diameter of the left atrium was 46.2 ± 5.6 mm. The LAV evaluated by eco3D was 67.9 ± 27.3 ml and LAVi was 39.2 ± 15.7 mL/m2.
Correlations of the left atrium
The LAVi showed a weak to moderate correlation with the LV end-diastolic volume (r = 0.38; p < 0.01), with the LV end-systolic volume (r = 0.427; p < 0.001) and the LV ejection fraction (r = -0.362; p < 0.01), and moderate correlation with the E wave (r = 0.50; p < 0.01), E/e´ ratio (r = 0.51; p < 0.01) and mitral regurgitation vena contracta (r = 0.528; p < 0.01) (Table 3).
Table 3.
Left atrial volume correlation with clinical and echocardiographic variables
| Variable | R | p |
|---|---|---|
| HR | - | 0.44 |
| SBP | - | 0.21 |
| LVEDV | 0.38 | < 0.01 |
| LVESV | 0.43 | < 0.01 |
| LVEF | -0.36 | < 0.01 |
| E wave | 0.50 | < 0.01 |
| e' wave | - | 0.55 |
| E/e' ratio | 0.51 | < 0.01 |
| Intraventricular mechanical delay | - | 0.91 |
| MR-VC | 0.53 | < 0.01 |
| 3D dyssynchrony index | 0.15 | 0.09 |
HR: heart rate; LVEF: left ventricular ejection fraction; SBP: systolic blood pressure; MR-VC: mitral regurgitation vena contracta; LVEDV: end-diastolic volume of the left ventricle; LVESV: end-systolic volume of the left ventricle.
The multivariate analysis showed the E/e´ ratio (p = 0.02) and the mitral regurgitation vena contracta (p = 0.02) as the only variables independently associated with LAVi increase.
Inter and intra-observer variability
The inter and intra-observer variability coefficients for LAV were 8.9% and 3.7%, respectively.
Discussion
Increased LAVi is independently associated with LV filling pressures (E/e´ ratio) and mitral regurgitation. As far as we know, this is the first study to use eco3D to assess the determinants of LAV in patients with DCM and heart failure.
The eco3D is a more reliable method than the two-dimensional echocardiography to estimate LAV, and its accuracy is similar to that of nuclear magnetic resonance16.
It is well established that left atrial dilation is associated with poor prognosis and symptoms in patients with heart failure due to left ventricular systolic dysfunction3-6. Furthermore, it is known that diastolic dysfunction is a marker of disease severity and is associated with symptoms and prognosis in patients with DCM and heart failure17-19.
Left atrium and diastolic dysfunction
Echocardiographic assessment of diastolic dysfunction by mitral inflow and tissue Doppler reflects the instantaneous diastolic function. On the other hand, it was demonstrated that LAV reflects the diastolic function in the long-term20. In our study, it was demonstrated that LAV is strongly related to LV filling pressures (E/e´ ratio) in patients with DCM. Thus, the dilation of the left atrium and the diastolic dysfunction are also closely related in this population.
Left atrium and mitral regurgitation
The present study showed that the LAV is associated with mitral regurgitation. As the mitral regurgitation intensity increases, the LA dilates. This phenomenon is well known in primary mitral valve disease21, but the study was able to demonstrate that this phenomenon also occurs with functional mitral regurgitation.
Other causes of the left atrial dilation
Other mechanisms may be involved in left atrial dilation in patients with DCM. Atrial myopathy has been reported in a series of autopsies of idiopathic DCM, as well as in Chagas cardiomyopathy. Previous study showed that the left atrium is more affected in Chagas cardiomyopathy than in idiopathic DCM22, which shows greater impairment than ischemic cardiomyopathy23.
Interestingly, in this study, the diastolic and systolic volumes and LV ejection fraction showed weak to moderate correlation with left atrial dilation, but were not independently associated with left atrial dilatation in the multivariate analysis. These findings suggest that the myopathic process in the LV, which causes the dilation, does not have the same intensity in the left atrium.
Another mechanism possibly involved in left atrial dilatation is the inflammatory process that may be present in the DCM. Previous studies in patients with normal left ventricular function have demonstrated an association between inflammation and increased LAV24-25.
Limitations
It was not possible to perform the magnetic resonance imaging or autopsy in these patients, which could have provided other left atrial parameters, such as fibrosis extension26, which could also be related to the LAV increase.
It is important to remember that the initial velocity (E wave) of the transmitral diastolic flow is influenced by the degree of mitral regurgitation. Unfortunately, it is not possible to differentiate how much of the E-wave velocity is due to increased filling pressures and how much is due to mitral regurgitation.
The study also did not assess whether an inflammatory process was associated with the LAV increase, as it occurs in patients with preserved LV function24,25. Although it is important to remember that blood biomarkers show the instant inflammatory state, while the left atrium dilation is a continuous process.
Conclusion
The left atrial volume is independently determined by the left ventricular filling pressures (E/e´ ratio) and by mitral regurgitation in patients with non-ischemic dilated cardiomyopathy.
Footnotes
Author contributions
Conception and design of the research:Mancuso FJN, Almeida DR, Poyares D, Oliveira WA, Campos O. Acquisition of data:Mancuso FJN, Almeida DR, Storti LJ, Brito FS. Analysis and interpretation of the data: Mancuso FJN, Moisés VA, Oliveira WA, Campos O. Statistical analysis:Mancuso FJN, Moisés VA. Writing of the manuscript:Mancuso FJN, Storti LJ, Campos O. Critical
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Tsang TS, Barnes ME, Gersh BJ, Takemoto Y, Rosales AG, Bailey KR, et al. Prediction of risk for first age-related cardiovascular events in an elderly population: the incremental value of echocardiography. J Am Coll Cardiol. 2003;42(7):1199–1205. doi: 10.1016/s0735-1097(03)00943-4. [DOI] [PubMed] [Google Scholar]
- 2.Tsang TS, Abhayaratna WP, Barnes ME, Miyasaka Y, Gersh BJ, Bailey KR, et al. Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J Am Coll Cardiol. 2006;47(5):1018–1023. doi: 10.1016/j.jacc.2005.08.077. [DOI] [PubMed] [Google Scholar]
- 3.Acartuk E, Koc M, Bozkurt A, Unal I. Left atrial size may predict exercise capacity and cardiovascular events in patients with heart failure. Tex Heart Inst. 2008;35(2):136–143. [PMC free article] [PubMed] [Google Scholar]
- 4.Nunes MCP, Barbosa MM, Ribeiro AL, Colosimo EA, Rocha MO. Left atrial volume provides independent prognostic value in patients with Chagas cardiomyopathy. J Am Soc Echocardiogr. 2009;22(1):82–88. doi: 10.1016/j.echo.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Rossi A, Cicoira M, Zanolla L, Sandrini R, Golia G, Zardini P, et al. Determinants and prognostic value of left atrial volume in patients with dilated cardiomyopathy. J Am Coll Cardiol. 2002;40(8):1425–1430. doi: 10.1016/s0735-1097(02)02305-7. [DOI] [PubMed] [Google Scholar]
- 6.Suh IW, Song JM, Lee EY, Kang SH, Kim MJ, Kim JJ, et al. Left atrial volume measured by real-time 3-dimensional echocardiography predicts clinical outcomes in patients with severe left ventricular dysfunction and in sinus rhythm. J Am Soc Echocardiogr. 2008;21(5):439–445. doi: 10.1016/j.echo.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90(12):1284–1289. doi: 10.1016/s0002-9149(02)02864-3. [DOI] [PubMed] [Google Scholar]
- 8.Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30(6):1527–1533. doi: 10.1016/s0735-1097(97)00344-6. [DOI] [PubMed] [Google Scholar]
- 9.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10(2):165–193. doi: 10.1093/ejechocard/jep007. [DOI] [PubMed] [Google Scholar]
- 10.Bax JJ, Bleeker GB, Marwick TH, Molhoek SG, Boersma E, Steendijk P, et al. Left ventricular dyssynchrony predicts response and prognosis after cardiac resynchronization therapy. J Am Coll Cardiol. 2004;44(9):1834–1840. doi: 10.1016/j.jacc.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 11.Gorcsan J, III, Abraham T, Agler DA, Bax JJ, Derumeaux G, Grimm RA, et al. American Society of Echocardiography: Echocardiography for Cardiac Resynchronization Therapy: Recommendations for Performance and Reporting-A Report from the American Society of Echocardiography Dyssynchrony Writing Group Endorsed by the Heart Rhythm Society. J Am Soc Echocardiogr. 2008;21(3):191–212. doi: 10.1016/j.echo.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Penicka M, Bartunek J, De Bruyne B, Vanderheyden M, Goethals M, De Zutter M, et al. Improvement of left ventricular function after cardiac resynchronization therapy is predicted by tissue Doppler imaging echocardiography. Circulation. 2004;109(8):978–983. doi: 10.1161/01.CIR.0000116765.43251.D7. [DOI] [PubMed] [Google Scholar]
- 13.Anwar AM, Soliman OI, Geleijnse ML, Nemes A, Vletter WB, tenCate FJ. Assessment of left atrial volume and function by real-time three-dimensional echocardiography. Int J Cardiol. 2008;123(1):155–161. doi: 10.1016/j.ijcard.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 14.Gerard O, Billon AC, Rouet JM, Jacob M, Fradkin M, Allouche C. Efficient model-based quantification of left ventricular function in 3D echocardiography. IEEE Trans Med Imaging. 2002;21(9):1059–1068. doi: 10.1109/TMI.2002.804435. [DOI] [PubMed] [Google Scholar]
- 15.Kapetanakis SMT, Siva A, Gall N, Cooklin M, Monaghan MJ. Real-time three-dimensional echocardiography: a novel technique to quantify global left ventricular mechanical dyssynchrony. Circulation. 2005;112(7):992–1000. doi: 10.1161/CIRCULATIONAHA.104.474445. [DOI] [PubMed] [Google Scholar]
- 16.Keller AM, Gopal AS, King DL. Left and right atrial volume by freehand three-dimensional echocardiography: in vivo validation using magnetic resonance imaging. Eur J Echocardiogr. 2000;1(1):55–65. doi: 10.1053/euje.2000.0010. [DOI] [PubMed] [Google Scholar]
- 17.Packer M. Abnormalities of diastolic function as a potential cause of exercise intolerance in chronic heart failure. Circulation. 1990;81(Suppl III):III78–III86. [PubMed] [Google Scholar]
- 18.Pinamonti B, Di Lenarda A, Sinagra G, Camerini F. Restrictive ventricular filling pattern in dilated cardiomyopathy assessed by Doppler echocardiography: clinical, echocardiographic and hemodynamic correlation and prognostic implication. Heart Muscle Disease Study Group. J Am Coll Cardiol. 1993;22(3):808–815. doi: 10.1016/0735-1097(93)90195-7. [DOI] [PubMed] [Google Scholar]
- 19.Xie GY, Berk MR, Smith M, Gurley JC, DeMaria A. Prognostic value of Doppler transmitral flow patterns in patients with congestive heart failure. J Am Coll Cardiol. 1994;24(1):132–139. doi: 10.1016/0735-1097(94)90553-3. [DOI] [PubMed] [Google Scholar]
- 20.Appleton CP, Jensen JL, Hatle LK, Oh JK. Doppler evaluation of left and right ventricular diastolic function: a technical guide for obtaining optimal flow velocity recordings. J Am Soc Echocardiogr. 1997;10(3):271–292. doi: 10.1016/s0894-7317(97)70063-4. [DOI] [PubMed] [Google Scholar]
- 21.Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al. American Society of Echocardiography Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16(7):777–802. doi: 10.1016/S0894-7317(03)00335-3. [DOI] [PubMed] [Google Scholar]
- 22.Mancuso FJN, Almeida DR, Moises VA, Oliveira WA, Mello ES, Poyares D, et al. Left atrial dysfunction in Chagas cardiomyopathy is more severe than in idiopathic dilated cardiomyopathy: a study with real-time three-dimensional echocardiography. J Am Soc Echocardiogr. 2011;24(5):526–532. doi: 10.1016/j.echo.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 23.Ohtani K, Yutani C, Nagata S, Koretsune Y, Hori M, Kamada T. High prevalence of atrial fibrosis in patients with dilated cardiomyopathy. J Am Coll Cardiol. 1995;25(5):1162–1169. doi: 10.1016/0735-1097(94)00529-y. [DOI] [PubMed] [Google Scholar]
- 24.Rao AK, Djamali A, Korcarz CE, Aeschlimann SE, Wolff MR, Stein JH. Left atrial volume is associated with inflammation and atherosclerosis in patients with kidney disease. Echocardiography. 2008;25(3):264–269. doi: 10.1111/j.1540-8175.2007.00589.x. [DOI] [PubMed] [Google Scholar]
- 25.Barberato SH, Bucharles SGE, Souza AM, Constantini CO, Constantini CRF, Pecoitz R., Filho Associação entre marcadores de inflamação e aumento do átrio esquerdo em pacientes de hemodiálise. Arq Bras Cardiol. 2013;100(2):141–146. [Google Scholar]
- 26.Sara L, Szarf G, Tachibana A, Shiozaki AA, Villa AV, Oliveira AC, et al. Sociedade Brasileira de Cardiologia II Diretriz de Ressonância Magnética e Tomografia Computadorizada Cardiovascular da Sociedade Brasileira de Cardiologia e do Colégio Brasileiro de Radiologia. Arq Bras Cardiol. 2014;103(6) supl. 3:1–86. doi: 10.5935/abc.2014S006. [DOI] [PubMed] [Google Scholar]