Abstract
To evaluate the phenotype of macrophages in the cornea and conjunctiva of C57BL/6 mice with induced experimental dry eye. C57BL/6 mice exposed to desiccating stress (DS) were evaluated at 1, 5, and 10 days and C57BL/6 mice maintained in non-stressed environment were used as controls. Whole eyes and adnexa were excised for histology or used for gene expression analysis. Location and phenotype of macrophages infiltrating the cornea and conjunctiva was evaluated by immunofluorescence analysis. Quantitative polymerase chain reaction evaluated macrophage markers and T cell-related and inflammatory cytokine expression in cornea and conjunctiva. Immunofluorescence staining demonstrated that macrophages reside in the conjunctiva of control and dry eye mice and their number did not change with DS. Real-time RT-PCR demonstrated that the level of M1 macrophage marker, iNOS, increased prominently in the conjunctiva at DS 10 days. In contrast, there was a non-significant decrease of the M2 marker Arg1 with DS. The levels of inflammatory cytokine, IL-12a mRNA transcript in the conjunctiva increased significantly at DS1 and decreased at DS5, while levels of IL-18 were significantly increased at DS 10. Macrophages reside in the ocular surface tissues of C57BL/6 mice. Although the number of macrophages in the conjunctiva does not change, evidence of inflammatory M1 activation after desiccating stress was observed. Better understanding of phagocyte diversity and activation in dry eye disease provide a basis for the development of phagocyte-targeted therapeutic strategies.
Keywords: Dry eye disease, Macrophage phenotype, Desiccating stress, Ocular surface
Introduction
Dry eye disease (DED) is one of the most prevalent eye conditions that causes bothersome irritation and can possibly decrease quality of life. DED is not simply a disease of decreased tear production, but has a pathogenesis based on a T cell-mediated autoimmune response. DED has been demonstrated to cause inflammation on the ocular surface, evidenced by increased levels of inflammatory cytokines [interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF)-α] in the tear fluid and corneal and conjunctival epithelia and infiltration of the conjunctiva with CD4+ T cells (De Paiva et al. 2007; Pflugfelder 2003; Pflugfelder et al. 1999; Solomon et al. 2001; Stern et al. 2002). Macrophages interact intimately with CD4+ T cells, serving as both T cell-directed phagocytes and T cell-activating antigen-presenting cells (Zhou et al. 2012). Macrophages are heterogeneous, versatile cells that display remarkable phenotypic plasticity and functional diversity (Galli et al. 2011; Gordon and Taylor 2005; Sica and Mantovani 2012). Hence, activated macrophages often are classified in a spectrum of polarization states. Mirroring T helper type 1–T helper type 2 (TH1–TH2) polarization, two distinct states of polarized macrophage activation have been recognized: the classically activated (M1) macrophage phenotype and the alternatively activated (M2) macrophage phenotype (Galli et al. 2011; Gordon and Taylor 2005; Mantovani et al. 2002; Sica and Mantovani 2012). The M1 macrophages are induced by interferon (IFN)-γ or microbial stimuli [lipopolysaccharide (LPS)], and characterized by the expression of high levels of inducible nitric oxide synthase 2 (iNOS) (Mosser and Edwards 2008; Stout et al. 2005). Following activation, M1 macrophages secrete proinflammatory and T cell polarizing cytokines (IL-1β, TNF-α, IL-12 and IL-23) and chemokines (CXCL9 and CXCL10), and induce inflammation and tissue destruction (Mosser and Edwards 2008; Stout et al. 2005). In contrast, the M2 macrophages are driven by TH2 cytokines IL-4 and IL-13 and are characterized by high expression of mannose receptor (CD206) and production of IL-10, an anti-inflammatory cytokine that resolves inflammation and promotes wound healing (Mosser and Edwards 2008; Stout et al. 2005).
Cytokine expression patterns or the ratio of iNOS to arginase 1 (Arg1) gene expression is commonly used as readouts of macrophage phenotype and functional status (Chiang et al. 2008; Mosser 2003; Stout et al. 2005). However, these functional phenotypes are reversible.
Although mechanisms and molecules associated with macrophage plasticity and polarized activation have been studied in tumors, diseases of the central nervous system, or tissue transplantation (Biswas and Mantovani 2010; Oh et al. 2013; Sica 2010; Shechter and Schwartz 2013), there have been few studies on differentiation and distribution of macrophages in dry eye associated inflammation. Thus, we investigated the phenotype of macrophages in ocular surface tissues of experimental dry eye in mice. Greater understanding of macrophage plasticity and polarization in the ocular surface response to desiccating stress may provide a basis for macrophage-centered diagnostic and therapeutic strategies.
Materials and Methods
Animals
This research protocol was approved by the Baylor College of Medicine Center for Comparative Medicine, and it conformed to the standards of the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research.
Six- to eight-week old of female C57BL/6 mice were purchased from The Jackson Laboratory (Bar Harbor, ME) for establishment of mouse colonies in our vivarium. They were housed in our vivarium in a pathogen-free environment that is managed by Baylor Center for Comparative Medicine. Mice were exposed to a 12-h light cycle while in the vivarium with timers controlling the light/dark cycle.
Induction of Desiccating Stress
C57BL/6 mice were exposed to desiccating stress (DS). DS was induced by subcutaneous injection of scopolamine hydrobromide (0.5 mg/0.2 ml; Sigma–Aldrich, St. Louis) four times a day (0800, 1100, 1400, 1700 hours), alternating flanks, for 1, 5 or 10 consecutive days (DS1, DS5, DS10), as previously described (Coursey et al. 2013; Dursun et al. 2002; Luo et al. 2004). Mice were placed in a cage with a perforated plastic screen on one side to allow airflow from a fan placed six inches in front of it for 16 h/day. Room humidity was maintained at 20–30 %. Control mice were maintained in a non-stressed environment at 50–75 % relative humidity without exposure to a forced air draft.
Histology and Immunofluorescent Staining
Immunofluorescence staining was performed to detect F4/80 (general macrophage marker) expression by infiltrating macrophages in corneal and conjunctival tissue sections. Eyes and adnexa from three mice of each group were surgically excised, embedded in optimal cutting temperature compound (VWR, Swannee, GA), and flash frozen in liquid nitrogen. Briefly, cryosections were fixed in methanol for 10 min, and permeabilized with 0.1 % Triton X-100 in phosphate buffer solution (PBS). After blocking with 20 % normal goat serum in PBS for 30 min, monoclonal rat antibody against F4/80 (Novus Biologicals, Littleton, CO) was applied, and the sections were incubated for 1 h at room temperature. After rinsing with PBS, Alexa-Fluor 488 conjugated goat anti-rat IgG (1:100 dilution) secondary antibodies were then applied, and the sections were incubated in a dark chamber for 1 h, and followed by nuclear counterstaining with Hoechst (Sigma-Aldrich, St. Louis, MO). Tissues without primary antibody were used as negative controls. The images were photographed using an epifluorescence microscope (Eclipse 400; Nikon, Garden City, NY). Positively stained cells were counted in the goblet cell rich area of the palpebral conjunctiva, over a length of at least 500 µm in the epithelium and to a depth of 75 µm below the epithelial basement membrane in the stroma for a distance of 500 µm using image-analysis software (NIS Elements Software, version 3.0; Nikon). Results were expressed as the number of positive cells per 100 µm.
RNA Isolation and Real-Time PCR
Total RNA from conjunctiva and corneal epithelium (individually collected and individually pooled) from C57BL/6 mice was extracted using a Qiagen MicroPlus RNA Isolation Kit (Qiagen, Valencia, CA, USA) according to the manufacturer’s instructions, measured by a NanoDrop ND-1000 Spectrophotometer (Thermo Scientific, Wilmington, DE, USA), and stored at −80 °C. One sample consisted of pooled samples of right and left eyes of the same animal. Samples were treated with DNase to prevent genomic DNA contamination according to the manufacturer’s instructions (Qiagen, Valencia, CA, USA).
First-strand complementary DNA was synthesized from 1 µg of total RNA using random hexamers and M-MuLV reverse transcriptase (Ready-To-Go You-Prime First-Strand Beads; GE Healthcare, Arlington Heights, NJ, USA), as previously described (Luo et al. 2004).
Quantitative real-time PCR was performed with specific minor groove binder (MGB) probes (Taqman; Applied Biosystems) and PCR master mix (Taqman Gene Expression Master Mix), in a commercial thermocycling system (StepOnePlus Real-Time PCR System; Applied Biosystems). Murine MGB probes were NOS2 (iNOS, Mm00440485_m1), Arg1 (Mm00475988_m1), IL-9 (Mm00434304_m1), IL-4 (Mm00445259_m1), IL-13 (Mm00434204_m1), IL-18 (Mm 00434225_m1), and IL-12a (Mm00434165_m1). The hypoxanthine phosphoribosyltransferase 1 (HPRT-1) (Mm00446968_m1) gene was used as an endogenous reference for each reaction. The results of quantitative PCR were analyzed by the comparative Ct method in which the target of change =2−ΔΔCt and were normalized by the Ct value of HPRT-1 and the mean Ct of relative mRNA level in the normal control group (non-stressed) was used as the calibrator.
Statistical Analysis
One-way analysis of variance (ANOVA) with Tukey’s post hoc testing was used for statistical comparisons of multiple groups. P ≤ 0.05 was considered statistically significant. These tests were performed using GraphPad Prism 6.0 software (GraphPad Software Incorporation, San Diego, CA).
Results
Macrophage Infiltration in the Ocular Surface of Unstressed and Desiccating Stressed C57BL/6 Mice
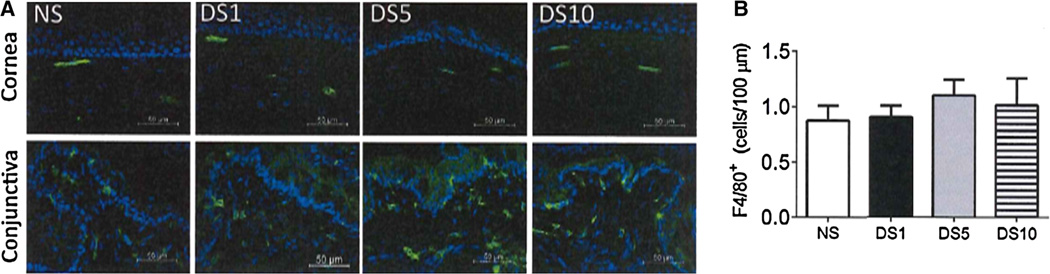
F4/80+ macrophages were detected in the conjunctival stroma and epithelium by immunofluorescence staining (Fig. 1a). These F4/80+ cells also infiltrated the subepithelial and stromal compartment of cornea (Fig. 1a), the number of F4/80+ cells in the cornea did not change with DS. The number of F4/80+ cells in the conjunctiva did not change with DS (Fig. 1b).
Fig. 1.
Histologic analysis of macrophage infiltration in the ocular surface of C57BL/6 mice after desiccation stress. a Representative images showed macrophage localization [F4/80 (green)] in the cornea and conjunctiva by immunofluorescence staining with Hoechst (blue) as nuclear counterstaining. b Macrophage density in the conjunctiva. NS non-stressed, DS1 desiccating stress (DS) day 1, DS5 DS day 5, DS10 DS day 10
Effects of Desiccating Stress on Expression of Macrophage Phenotype Markers in the Cornea and Conjunctiva of C57BL/6 Mice
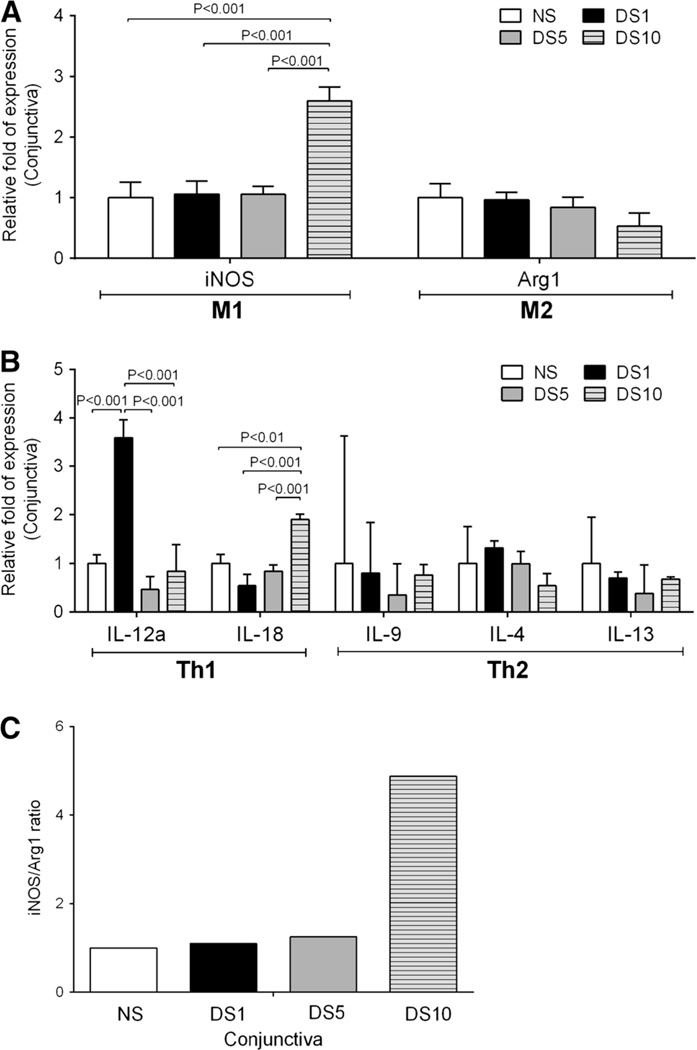
To investigate the macrophage phenotype, we compared expression of macrophage phenotype markers in the conjunctiva and corneal epithelium of C57BL/6 mice in non-stressed conditions and after at 1, 5 and 10 days after desiccating stress. Real-time RT-PCR demonstrated that the level of M1 macrophage marker, iNOS, increased significantly in the conjunctiva at DS10. In contrast, Arg1, a marker of M2 macrophages, showed a gradual non-significant decrease with DS (Fig. 2a). Expression of Th1 and Th2 associated cytokine transcripts in the conjunctiva was also evaluated (Fig. 2b). A significant increase in IL-12a was noted at DS1 and decreased to baseline levels at DS5 (Fig. 2b), while levels of IL-18 were significantly increased at DS10. No significant change in levels of IL-9, IL-4, and IL-13 transcripts in the conjunctiva was noted.
Fig. 2.
Quantitative gene analysis of mRNA transcripts in the conjunctiva of C57BL/6 mice after desiccation stress. a Relative fold of expression of M1 and M2 macrophage markers in conjunctiva of C57BL/6 mice at desiccating stress 1, 5, and 10 days. Bar graphs show mean ° SEM of one representative experiment with 7–10 samples/time point (experiment was repeated twice with similar results). One sample consisted of pooled right and left conjunctivas of the same animal. b Relative fold of expression of T cell-related cytokines and inflammatory cytokines. c iNOS to Arg1 ratio in the conjunctiva of C57BL/6 mice after desiccation stress. NS non-stressed, DS1 desiccating stress (DS) day 1, DS5 DS day 5, DS10 DS day 10, iNOS inducible nitric oxide synthase (NOS2), Arg1 arginase 1, IL-9 interleukin-9
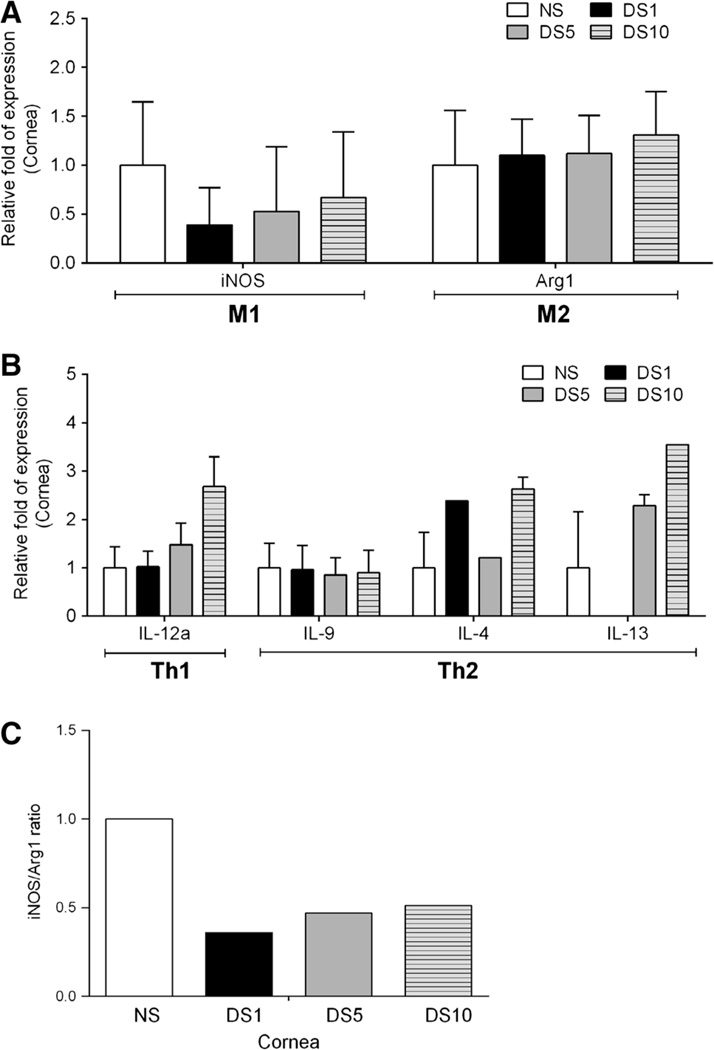
In the cornea of C57BL/6 mice, there was no change in the levels of iNOS, Arg1, IL-4, IL-9, and IL-13 transcripts with DS (Fig. 3). Increased expression of IL-12a in the cornea was noted with DS, but this did not reach significance (Fig. 3b). iNOS and Arg1 are known to utilize l-arginine as a common substrate, and they are considered signature enzymes of M1 and M2 macrophages, respectively. We calculated the ratio of iNOS to Arg1 to determine the predominant macrophage phenotype in non-stressed mice at each time point after induction of DS. Our results presented in Fig. 2c show greater iNOS to Arg1 ratio in the conjunctiva at DS10, whereas this ratio decreased in the cornea with DS (Fig. 3c).
Fig. 3.
Quantitative gene analysis of mRNA transcripts in the cornea of C57BL/6 mice after desiccation stress. a Relative fold of expression of M1 and M2 macrophage markers in cornea of C57BL/6 mice at desiccating stress 1, 5, and 10 days. Bar graphs show mean ± SEM of one representative experiment with 7–10 samples/time point (experiment was repeated twice with similar results). One sample consisted of pooled right and left cornea of the same animal. b Relative fold of expression of T cell-related cytokines and inflammatory cytokines. In results of IL-4 and IL-13, there was 1/5 less only sample to amplify at DS1, DS5, and DS10. c iNOS to Arg1 ratio in the cornea of C57BL/6 mice after desiccation stress. NS non-stressed, DS1 desiccating stress (DS) day 1, DS5 DS day 5, DS10 DS day 10, iNOS inducible nitric oxide synthase (NOS2), Arg1 arginase 1, IL-9 interleukin-9
Discussion
Macrophages are very flexible in adapting their transcription profile to changes in their microenvironment (Stout et al. 2005). Our results demonstrated that after subjecting C57BL/6 mice to desiccating stress, there was no change in number of macrophages, but increased production of M1 macrophage markers in the conjunctiva. Also, the expression of inflammatory cytokines IL-18 and IL-12 that are produced by activated M1 macrophages was found to increase in the conjunctiva.
Desiccating stress, factors that disrupt tear film stability and increase tear osmolarity, can induce ocular surface damage and initiate an inflammatory cascade that generates innate and adaptive immune responses (Stevenson et al. 2012). In our study, transiently increased IL-12 expression was noted after exposure to desiccating stress. IL-12 expression peaked one day after exposure to desiccating stress. The transient appearance of IL-12 would suggest that although the number of macrophages did not change in the early period of DS, there is a shift toward M1 phenotype that may be induction of the Th1 response and increased IFN-γ production that we have previously reported (De Paiva et al. 2007).
Macrophages can also be polarized into an “M2-like” state, which shares some but not all the signature features of M2 cells (Biswas and Mantovani 2010). For example, various stimuli, such as antibody immune complexes together with LPS or IL-1, transforming growth factor-β and IL-10, give rise to M2-like functional phenotypes that share properties with IL-4 or IL-13-activated macrophages (such as high expression of mannose receptor, IL-10 and angiogenic factors) (Mantovani et al. 2004). Adipose tissue macrophages from obese mice have a mixed profile, with upregulation of several M1 and M2 gene transcripts (Shaul et al. 2010). In our study, there was an increase in levels of M1 macrophage markers in the conjunctiva in response to DS. This study suggests there is plasticity of macrophage functional state on the ocular surface with a shift towards M1 shortly after exposure to desiccating environmental conditions (Biswas and Mantovani 2010; Mosser and Edwards 2008).
Macrophages might exert direct cytotoxicity and act as effector immune cells by producing reactive nitrogen species (Biswas and Mantovani 2010; Sica and Mantovani 2012). M1 macrophages express high levels of iNOS that compete with Arg1 for l-arginine, the common substrate of both enzymes (Cho et al. 2014). iNOS converts l-arginine to nitric oxide (NO), competing with Arg1, which converts NO into urea and ornithine (Cho et al. 2014). By inhibiting iNOS, Arg1 may promote the M2 phenotype and contributes to the suppression of the M1 phenotype (Cho et al. 2014). Our data show the level of iNOS and the ratio of iNOS to Arg1 gradually increased in the conjunctiva with desiccating stress, peaking at DS10.
Previous report stated that local depletion of peripheral conjunctival antigen-presenting cells using subconjunctival injection of clodronate blocked the ability of dry eye specific CD4+ T cells to accumulate within ocular surface tissues and did not induce robust production of proinflammatory cytokines (Schaumburg et al. 2011). Depleting dendritic cell and macrophages will turn off the immune response of dry eye. Complete understanding of macrophage biology and mechanisms underlying macrophage differentiation and phenotypic maturation might provide novel therapeutic targets for preventing ocular surface inflammation in response to DS.
In conclusion, our results show that C57BL/6 mice have macrophages residing in the conjunctiva and cornea. Although there is no change of number of macrophages after DS, inflammatory M1 activation was observed. Better understanding of phagocyte diversity and activation in dry eye disease may show efficacy for phagocyte-targeted therapeutic strategies.
Acknowledgments
This work was supported by NIH Grant EY11915 (S. C. Pflugfelder), NEI/NIH Core Grant EY-002520RPB, Oshman Foundation, William Stamps Farish Fund, Hamill Foundation. This paper was also supported by research funds of Chonbuk National University in 2012.
Footnotes
Conflict of Interest All the authors declare that they have no conflict of interest.
Contributor Information
In-Cheon You, Department of Ophthalmology, Research Institute of Clinical Medicine of Chonbuk National University, Chonbuk National University Medical School and Hospital, Chonbuk National University, Jeonju, Jeonbuk, Korea; Department of Ophthalmology, Ocular Surface Center, Cullen Eye Institute, Baylor College of Medicine, Houston, TX, USA.
Terry G. Coursey, Department of Ophthalmology, Ocular Surface Center, Cullen Eye Institute, Baylor College of Medicine, Houston, TX, USA
Fang Bian, Department of Ophthalmology, Ocular Surface Center, Cullen Eye Institute, Baylor College of Medicine, Houston, TX, USA.
Flavia L. Barbosa, Department of Ophthalmology, Ocular Surface Center, Cullen Eye Institute, Baylor College of Medicine, Houston, TX, USA
Cintia S. de Paiva, Department of Ophthalmology, Ocular Surface Center, Cullen Eye Institute, Baylor College of Medicine, Houston, TX, USA
Stephen C. Pflugfelder, Email: stevenp@bcm.edu, Department of Ophthalmology, Ocular Surface Center, Cullen Eye Institute, Baylor College of Medicine, Houston, TX, USA; Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, 6565 Fannin Street, NC 505, Houston, TX 77030, USA.
References
- Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol. 2010;11:889–896. doi: 10.1038/ni.1937. [DOI] [PubMed] [Google Scholar]
- Chiang CS, Chen FH, Hong JH, et al. Functional phenotype of macrophages depends on assay procedures. Int Immunol. 2008;20:215–222. doi: 10.1093/intimm/dxm137. [DOI] [PubMed] [Google Scholar]
- Cho DI, Kim MR, Jeong HY, et al. Mesenchymal stem cells reciprocally regulate the M1/M2 balance in mouse bone marrow-derived macrophages. Exp Mol Med. 2014;46:e70. doi: 10.1038/emm.2013.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coursey TG, Gandhi NB, Volpe EA, et al. Chemokine receptors CCR6 and CXCR3 are necessary for CD4(+) T cell mediated ocular surface disease in experimental dry eye disease. PLoS One. 2013;8:e78508. doi: 10.1371/journal.pone.0078508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Paiva CS, Villarreal AL, Corrales RM, et al. Dry eye-induced conjunctival epithelial squamous metaplasia is modulated by interferon-gamma. Invest Ophthalmol Vis Sci. 2007;48:2553–2560. doi: 10.1167/iovs.07-0069. [DOI] [PubMed] [Google Scholar]
- Dursun D, Wang M, Monroy D, et al. A mouse model of keratoconjunctivitis sicca. Invest Ophthalmol Vis Sci. 2002;43:632–638. [PubMed] [Google Scholar]
- Galli SJ, Borregaard N, Wynn TA. Phenotypic and functional plasticity of cells of innate immunity: macrophages, mast cells and neutrophils. Nat Immunol. 2011;12:1035–1044. doi: 10.1038/ni.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- Luo L, Li DQ, Doshi A, et al. Experimental dry eye stimulates production of inflammatory cytokines and MMP-9 and activates MAPK signaling pathways on the ocular surface. Invest Ophthalmol Vis Sci. 2004;45:4293–4301. doi: 10.1167/iovs.03-1145. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Sozzani S, Locati M, et al. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23:549–555. doi: 10.1016/s1471-4906(02)02302-5. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Sica A, Sozzani S, et al. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25:677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- Mosser DM. The many faces of macrophage activation. J Leukoc Biol. 2003;73:209–212. doi: 10.1189/jlb.0602325. [DOI] [PubMed] [Google Scholar]
- Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8:958–969. doi: 10.1038/nri2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh JY, Lee HJ, Ko AY, et al. Analysis of macrophage phenotype in rejected corneal allografts. Invest Ophthalmol Vis Sci. 2013;54:7779–7784. doi: 10.1167/iovs.13-12650. [DOI] [PubMed] [Google Scholar]
- Pflugfelder SC. Anti-inflammatory therapy of dry eye. Ocul Surf. 2003;1:31–36. doi: 10.1016/s1542-0124(12)70005-8. [DOI] [PubMed] [Google Scholar]
- Pflugfelder SC, Jones D, Ji Z, et al. Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjögren’s syndrome keratoconjunctivitis sicca. Curr Eye Res. 1999;19:201–211. doi: 10.1076/ceyr.19.3.201.5309. [DOI] [PubMed] [Google Scholar]
- Schaumburg CS, Siemasko KF, de Paiva CS, et al. Ocular surface APCs are necessary for autoreactive T cell-mediated experimental autoimmune lacrimal keratoconjunctivitis. J Immunol. 2011;187:3653–3662. doi: 10.4049/jimmunol.1101442. [DOI] [PubMed] [Google Scholar]
- Shaul ME, Bennett G, Strissel KJ, et al. Dynamic, M2-like remodeling phenotypes of CD11c+ adipose tissue macrophages during high-fat diet-induced obesity in mice. Diabetes. 2010;59:1171–1181. doi: 10.2337/db09-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechter R, Schwartz M. Harnessing monocyte-derived macrophages to control central nervous system pathologies: no longer ‘if’ but ‘how’. J Pathol. 2013;229:332–346. doi: 10.1002/path.4106. [DOI] [PubMed] [Google Scholar]
- Sica A. Role of tumour-associated macrophages in cancer-related inflammation. Exp Oncol. 2010;32:153–158. [PubMed] [Google Scholar]
- Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122:787–795. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon A, Dursun D, Liu Z, et al. Pro- and anti-inflammatory forms of interleukin-1 in the tear fluid and conjunctiva of patients with dry-eye disease. Invest Ophthalmol Vis Sci. 2001;42:2283–2292. [PubMed] [Google Scholar]
- Stern ME, Gao J, Schwalb TA, et al. Conjunctival T-cell subpopulations in Sjögren’s and non- Sjögren’s patients with dry eye. Invest Ophthalmol Vis Sci. 2002;43:2609–2614. [PubMed] [Google Scholar]
- Stevenson W, Chauhan SK, Dana R. Dry eye disease: an immune-mediated ocular surface disorder. Arch Ophthalmol. 2012;130:90–100. doi: 10.1001/archophthalmol.2011.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout RD, Jiang C, Matta B, et al. Macrophages sequentially change their functional phenotype in response to changes in microenvironmental influences. J Immunol. 2005;175:342–349. doi: 10.4049/jimmunol.175.1.342. [DOI] [PubMed] [Google Scholar]
- Zhou D, Chen YT, Chen F, et al. Critical involvement of macrophage infiltration in the development of Sjögren’s syndrome-associated dry eye. Am J Pathol. 2012;181:753–760. doi: 10.1016/j.ajpath.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]