Abstract
Background
The purpose of this investigation was to examine movement symmetry changes over the first 26 weeks following unilateral total knee arthroplasty in community environments using skin-mounted tibial accelerometers. Comparisons to healthy participants of similar age were also made.
Methods
Patients (N = 24) with unilateral knee osteoarthritis (mean (SD), 65.2 (9.2) years) scheduled to undergo total knee arthroplasty and a control group (N = 19 healthy people; mean (SD), 61.3 (9.2) years) were recruited. The total knee arthroplasty group participated in a standardized course of physical rehabilitation. Tibial acceleration data were recorded during a Stair Climb Test and 6-Minute Walk Test. Tibial acceleration data were reduced to initial peak acceleration for each step. An inter-limb absolute symmetry index of tibial initial peak acceleration values was calculated.
Findings
The total knee arthroplasty group had greater between limb asymmetry for tibial initial peak acceleration and initial peak acceleration absolute symmetry index values five weeks after total knee arthroplasty, during the Stair Climb Test and the 6-Minute Walk Test.
Interpretation
Tibial accelerometry is a potential tool for measuring movement symmetry following unilateral total knee arthroplasty in clinical and community environments. Accelerometer-based symmetry outcomes follow patterns similar to published measures of limb loading recorded in laboratory settings.
Keywords: total knee arthroplasty, movement symmetry, accelerometer, community environment
1. BACKGROUND
Improving lower limb movement symmetry is an important rehabilitation goal for patients recovering from unilateral total knee arthroplasty (TKA). Following unilateral TKA, patients have asymmetrical lower limb movements during tasks such as sit-stand transitions and walking, and this asymmetry is correlated with poor functional outcomes 1–4. To determine the impact of impaired movement symmetry on performance of functional tasks during daily activity, it is important to perform measurements in a natural living environment. Measurement of movement symmetry in community environments would serve to: 1) provide clinicians a practical method for assessing movement patterns and 2) serve as a means for providing patients with feedback on their movement patterns during functional activity.
Movement symmetry following TKA has often been measured in motion analysis laboratories equipped with cameras, electromyographic signal recording systems, and/or force platforms in a confined motion capture area 2,5–7. In addition, motion analysis systems have been used for providing feedback to patients during movement pattern re-training after lower limb joint surgeries 8–10. However, the equipment used to measure movement asymmetry and provide patients feedback during rehabilitation is not practical for common clinical use and difficult to use in community settings that patients encounter during daily living. Assessment of movement symmetry has historically been performed by motion capture and analysis of ground reaction forces. An alternative method that for measuring movement patterns is the use of accelerometers 11–13. Use of accelerometers to quantify movement patterns is a relatively inexpensive alternative which allows for assessing movements in community environments, and has established validity, with positive correlations to force-plate measurement systems 11,14–16
The purpose of this study was to examine use of portable, skin-mounted tibial accelerometers to measure changes in lower limb movement symmetry for patients with unilateral TKA during a Six-Minute Walk Test (6MWT) and Stair Climb Test (SCT). It was hypothesized that tibial acceleration would identify movement asymmetry in the TKA group compared to a group of healthy subjects (CTL) for both the 6MWT and SCT. It was also hypothesized that movement asymmetries measured by tibial acceleration would have a similar pattern to those measured in movement analysis laboratories, where asymmetry was greatest at 4–6 weeks after TKA and returned to preoperative levels by 26 weeks. Finally, it was expected that differences in tibial acceleration symmetry between the TKA and CTL groups would be greater during the SCT than the 6MWT, because the SCT test has a relatively higher loading demand.
2. MATERIALS & METHODS
Participants
This was an observational cohort study. Twenty-four people with knee osteoarthritis (OA) scheduled to undergo unilateral TKA. Participants in this study were control group subjects for ongoing investigations with standardized rehabilitation protocols from June 2006 to October 2012. Inclusion criteria were 1) age 50 to 85 years old and 2) ≤ half the level of pain on the non-surgical knee compared to the surgical knee before surgery (numerical pain rating scale of 0–10). Exclusion criteria were 1) uncontrolled hypertension, 2) uncontrolled diabetes, 3) BMI > 35 kg/m2, 4) neurologic impairment, or 5) other unstable lower-extremity orthopedic problems. The Colorado Multiple Institutional Review Board approved the studies, and written informed consent was obtained from all participants.
The group of healthy individuals was recruited from the community with the intent of having a group similar in age (50–85 years) and sex distribution to the TKA group. In addition to the exclusion criteria for the TKA group, volunteers for the healthy group were excluded if they had knee pain > 2/10 on an intermittent basis, had any knee pain with regular activity, and did not exercise at least three days per week.
Intervention
Within 2 weeks following baseline testing, all TKA group participants received a unilateral TKA. Rehabilitation following TKA included acute (2–4 days), home-based (1–2 weeks) and outpatient (1.5–2.5 weeks) intervention phases before a final 26-week follow-up testing session 17. All treatment sessions were performed by a physical therapist.
Outcome Measures
Participants performed all testing in the stairwell and hallway of an office building. The two functional outcome measures were: 1) a Stair Climb Test (SCT) and 2) the 6-Minute Walk Test (6MWT). TKA group participants were tested 1–2 weeks before surgery and at 5 (range 4–6) and 26 weeks after surgery. Not all time-points were tested for each participant in the TKA group, as accelerometer testing was a secondary outcome measure and primary outcomes were prioritized for participants who could not complete the entire testing protocol. In addition, participants were not tested at 26 weeks after surgery in one study. Healthy group participants were tested once to provide reference data collected during the SCT (n=12) and 6MWT (n=19). Sample sizes are reported for each time point in the results section.
Tibial Acceleration
Acceleration along the tibial longitudinal axis was measured using skin-mounted triaxial accelerometers (Delsys, Boston, MA, USA) (range ± 10g) (Figure 1). Accelerometers were rectangular in shape with a mass of 4 g, and were dimensionally 20 × 33 × 5 mm. An accelerometer was placed on the anteromedial surface of each tibia (66% height from inferior medial malleolus and knee medial joint line) before participants performed the two functional outcome tests. The longitudinal accelerometer axis was visually aligned along the tibial longitudinal axis and mounted with adhesive tape and an elastic wrap. Firm tension of the elastic wrap was used to preload the skin to damp potential artifact introduced by soft tissue between the tibia and the accelerometer 18. Data were recorded (1000 Hz) with a portable biosignal monitor (Delsys, Boston, MA, USA) worn on a waist belt.
Figure 1.
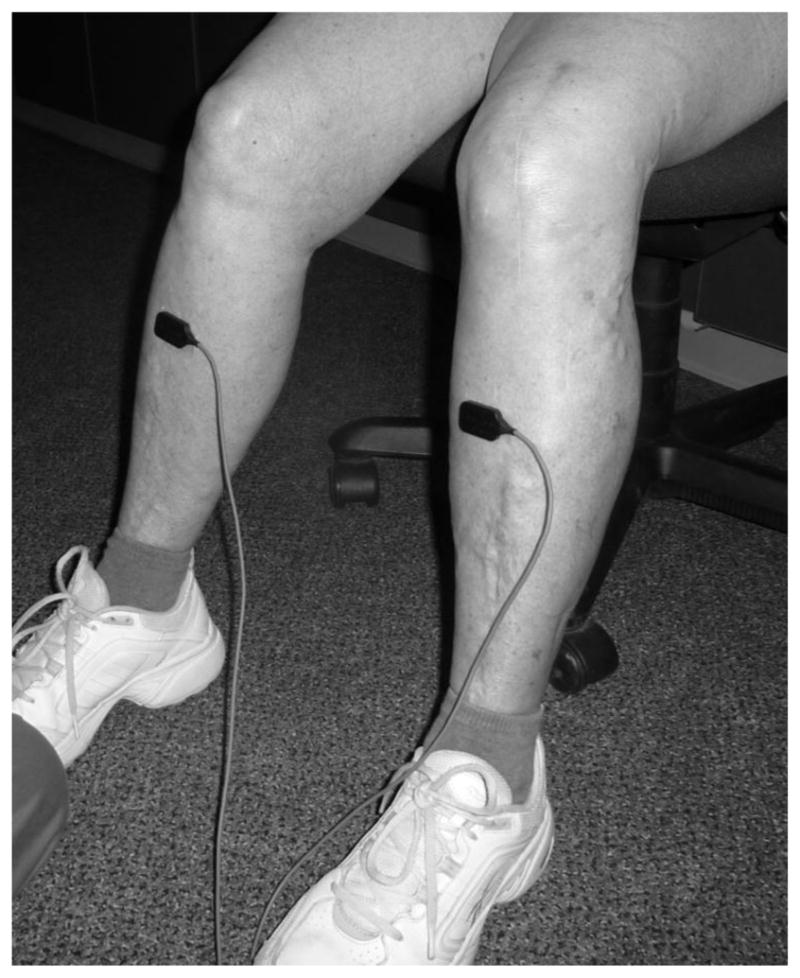
Accelerometers attached to the tibia.
After data collection, accelerometer data were filtered (Butterworth, 4th order, cutoff 40Hz) and voltage converted to gravitational units. Initial peak acceleration (IPA) was calculated from the acceleration signals during the four middle steps of ascending and descending the stairs and of the first and last minute of the 6MWT for each leg. IPA was the peak tibial acceleration after foot contact. The average IPA value over the four steps was used for analysis for each condition. To account for acceleration due to gravity, acceleration was measured along the vertical axis of the tibia with the participant standing in an upright posture prior to functional testing. This stationary acceleration measurement was subtracted from the acceleration values recorded during movement. In this way, the influence of gravity on the acceleration signal was accounted for in the natural orientation of the tibia when the participant was standing.
An absolute symmetry index 19 was calculated to compare the absolute differences in IPA between limbs (Equation 1). An absolute symmetry index value of zero would indicate perfect symmetry.
| (Equation 1) |
where IPAL = average initial peak acceleration for left limb and IPAR = average initial peak acceleration for right limb
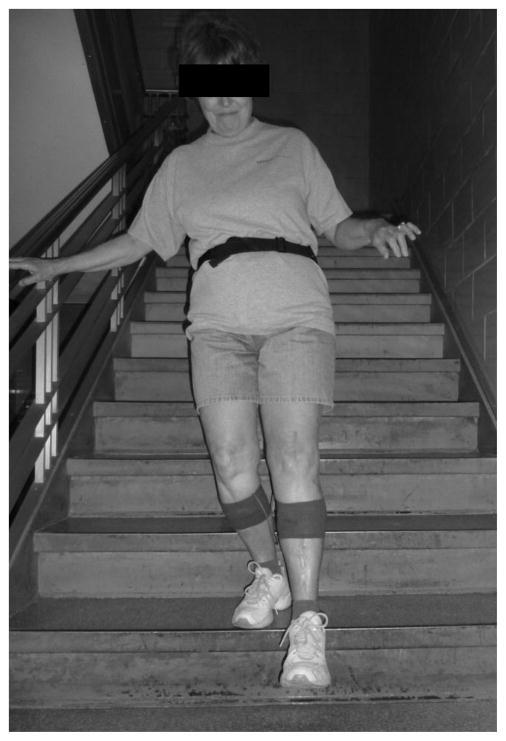
Stair Climb Test
Subjects were positioned at the base of a 10-step stairwell in an office building and instructed to ascend and descend the stairs “as quickly as possible, but safely” (Figure 2). Subjects were allowed to perform any step pattern desired (including stepping on each step with both feet, alternating foot contacts each step, or skipping steps). If needed, subject were allowed to use a cane or a handrail in the stairwell during stair walking for balance control. Subjects performed two trials of the SCT with the second trial used for time as well as accelerometer data analysis. The timed stair walking test has been shown to be a reliable and valid measure of physical function for people with and without knee OA 20,21.
Figure 2.
Participant performing Stair Climb Test with accelerometers attached to the tibia.
6-Minute Walk Test
The 6MWT was performed in a hallway of the office building with a linoleum-tiled floor, 30.5 m (100 ft.) in length. Instructions to the participants were to walk “as far as possible”, covering the maximum amount of distance, in the 6-minute time frame. Participants were allowed to rest as needed during timing, although the timer did not stop during any rest periods. The total distance covered in the 6 minutes was used as the outcome measure. Accelerometer data were analyzed during 4 steps in the middle of the first and last minute of the test. The 6MWT has been shown to be a valid and reliable outcome measure for older adults with and without lower extremity orthopedic problems, such as knee OA and TKA 22–24.
Statistical Analysis
The sample size estimate was based on five-week post-TKA IPA absolute symmetry index values (mean ± SD) during stair ascent for the first 10 participants. With a targeted 2:1 allocation ratio (TKA:CTL) and a difference in IPA symmetry index of 30 (SD = 40 for the TKA group and 10 for the CTL group), having 20 subjects in the TKA group and 10 in the CTL would provide 80% power to detect group differences, with alpha level at 0.05 using a 2-group t test. To account for potential dropout and missed test points, we targeted minimum sample sizes of 22 and 11 for the TKA and CTL groups, respectively.
Baseline characteristics for the two groups were compared using independent t tests for continuous variables or likelihood ratio chi-square tests for categorical variables. Comparison of IPA values between limbs at each time point was made using paired t tests. Comparison of IPA absolute symmetry index values between the TKA and CTL groups and within the TKA group between time points was based on contrasts estimated from a linear mixed-model regression. Due to multiple comparisons, the False Discovery Rate method was used to control the proportion of erroneous significances 25,26. The adjusted p values from the false discovery rate method were used to assess significance of differences between means.
3. RESULTS
Baseline Characteristics
The TKA and healthy CTL groups were comparable in age, sex distribution, and anthropometric measures (Table 1).
Table 1.
Baseline characteristics of TKA and Control groups
| Characteristic | TKA | CTL | P-value |
|---|---|---|---|
| Age (years) | 65.2 (9.2) | 61.3 (9.2) | 0.183 |
| Sex | Women (n = 13) Men (n = 11) |
Women (n= 10) Men (n = 9) |
0.920 |
| Height (m) | 1.71 (0.11) | 1.66 (0.26) | 0.423 |
| Body mass (kg) | 84.5 (12.9) | 78.5 (17.9) | 0.210 |
Data are mean (SD), except for sex, which is presented as number of women and men.
Outcome Measures
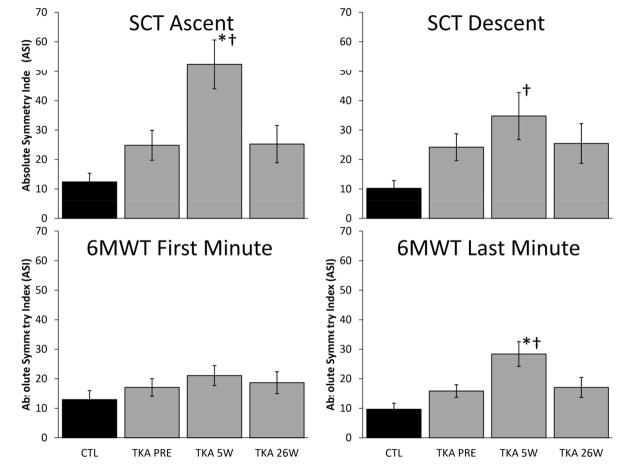
Absolute symmetry index values for tibial IPA are graphed for each condition at all time points in Figure 3. Group means for tibial IPA at all time points for each condition are presented in Table 2. IPA absolute symmetry index mean was greater for the TKA group at the five-week time point compared to the pre-operative time point for SCT ascent (p = 0.01) and last minute of the 6MWT (p = 0.02), with IPA being most asymmetrical during the SCT ascent. The TKA group IPA absolute symmetry index mean was greater at the five-week time point compared to the CTL group during the SCT ascent (p = 0.001), SCT descent (p = 0.02), and last minute of the 6MWT (p = 0.01). SCT times and 6MWT distances are presented in Table 3.
Figure 3.
Instantaneous Peak Acceleration Absolute Symmetry Index Values Across all Time Points.
Abbreviations: SCT, Stair Climb Test; 6MWT, Six-Minute Walk Test; CTL, Control group; TKA, Total Knee Arthroplasty group; PRE, Pre-operative time point; 5W, Five Week time point; 24W, 24 Week time point.
* difference from pre-operative measurement for TKA group, P<0.05; † difference between TKA group and CTL group.
Table 2.
Instantaneous Peak Accelerations at all Time Points for Both Groups
|
|
||||||||
|---|---|---|---|---|---|---|---|---|
| CTL | TKA Pre-Operative | TKA 5 Weeks Post-Operative | TKA 26 Weeks Post-Operative | |||||
|
| ||||||||
| Right Limb | Left Limb | Surgical Limb | Non-Surgical Limb | Surgical Limb | Non-Surgical Limb | Surgical Limb | Non-Surgical Limb | |
| SCT | (n = 12) | (n = 22) | (n = 21) | (n = 17) | ||||
|
| ||||||||
| IPA: Ascent (g) | 2.61 (0.43) | 2.61 (0.54) | 2.11 (0.79) | 2.19 (0.73) | 1.28 (0.73) | 1.92 (0.85) | 2.45 (0.58) | 2.65 (0.59) |
| IPA: Descent (g) | 2.51 (0.62) | 2.53 (0.64) | 2.10 (0.81) | 2.35 (0.80) | 1.41 (0.70) | 1.94 (0.92) | 2.38 (0.64) | 2.57 (0.54) |
|
| ||||||||
| 6MWT | (n = 19) | (n = 21) | (n = 22) | (n = 16) | ||||
|
| ||||||||
| IPA: Minute 1 (g) | 2.33 (0.60) | 2.33 (0.58) | 2.23 (0.69) | 2.07 (0.64) | 1.55 (0.60) | 1.70 (0.71) | 2.41 (0.51) | 2.28 (0.58) |
| IPA: Minute 6 (g) | 2.39 (0.48) | 2.30 (0.44) | 2.24 (0.67) | 2.04 (0.62) | 1.50 (0.63) | 1.66 (0.72) | 2.47 (0.48) | 2.30 (0.61) |
NOTE. Values are mean (SD).
Abbreviations: SCT, Stair Climb Test; 6MWT, Six-Minute Walk Test; CTL, Control group; TKA, Total Knee Arthroplasty group.
Table 3.
Stair Climb Test and 6-Minute Walk Test outcomes
| Outcome | CTL | TKA Pre-Operative | TKA 5 Weeks Post-Operative | TKA 26 Weeks Post-Operative |
|---|---|---|---|---|
| SCT (s) | 9.8 ± 2.0 | 11.9 ± 6.7 | 23.1 ± 8.8 | 11.9 ± 2.6 |
| 6MWT (m) | 592.2 ± 97.6 | 482.1 ± 91.0 | 421.0 ± 102.9 | 535.9 ± 62.0 |
NOTE. Values are mean ± SD.
Abbreviations: SCT, Stair Climb Test; 6MWT, Six-Minute Walk Test; CTL, Control group; TKA, Total Knee Arthroplasty group.
4. DISCUSSION
Results of this study illustrate the use of portable, skin-mounted accelerometers to measure tibial movement symmetry during functional task performance in a community environment. Use of such devices has promise for clinical application to assess movement asymmetries during rehabilitation following unilateral TKA, and potentially movement deviations with other clinical populations. The results also demonstrate a consistent pattern of absolute symmetry index means being greater for the TKA group at all time points than the CTL group.
Similar to previous studies using motion analysis laboratories, the data from this study indicate that patients with unilateral TKA have asymmetrical movement patterns during the rehabilitation phase following surgery 1,2,5. For example, using a stair case instrumented with force plates and an 8-camera motion analysis system, Mandeville and colleagues 27 demonstrated that patients have reduced surgical knee extension moments during stair climbing at six months following surgery compared to a healthy age-matched control group. Stacoff and colleagues 5 also used a motion analysis lab to examine inter-limb loading symmetry during stair ascent and descent for patients 1–3 years after unilateral TKA. Their findings were that patients demonstrated asymmetry of loading, characterized by decreased loading on the surgical limb compared to the non-surgical limb during weight acceptance phase of stair ascent and descent. Similar inter-limb loading asymmetry has been shown for patients within the first year after unilateral TKA for tasks such as sit-stand 1,2 and level ground walking 2,28. The consistency of findings with the current and previous studies, all concluding that lower limb movement asymmetry is important, suggests the potential utility of accelerometers for clinical applications such as movement pattern measurement and feedback to patients during rehabilitation.
Movement asymmetry after TKA, characterized by decreased loading of the surgical limb compared to the non-surgical limb, has been suggested to relate to the higher incidence of knee and hip pathologies of the contralateral limb after unilateral TKA 28. There have also been links between lower limb movement asymmetry and limitations in functional performance 1–3. In light of these findings, it has been suggested that targeting the quality of movement symmetry could be an approach to improving rehabilitation outcomes after unilateral TKA 2,8. However, the tools for measuring movement asymmetry must be feasible in clinical and community settings to target this movement limitation.
Previous researchers have demonstrated tibial accelerometers as valid tools for measuring limb accelerations and for estimating joint loading at the knee 11. Liikavainio and colleagues 11 used skin-mounted tibial accelerometers on healthy young men to demonstrate high repeatability of IPA measures during walking on level surfaces. In addition, tibial acceleration measures were found to be highly correlated with maximal loading rates measured from vertical ground reaction forces via a force plate during walking 11. O’Leary and colleagues, 12 amongst others, 29,30 have used tibial mounted accelerometers to measure impact loading for runners. Relative to knee osteoarthritis and TKA, use of tibial accelerometry has not been widely reported. Turpin and colleagues 13 have used tibial accelerometers to measure limb accelerations during walking with knee OA to examine the affects of cushioned shoe insoles.
One advantage of skin-mounted tibial accelerometers is portability. The tibial accelerometers used in this study were mounted to the tibia on each limb and wired to a data collection unit that the participants wore on a waist-belt. This set-up allowed patients to perform the SCT and 6MWT in a community environment. Using these methods, clinicians could test patients in rehabilitation clinic, home, or other community settings.
As a measurement of asymmetry, accelerometers may also have value in biofeedback training. Previous studies have provided promising results of movement training strategies to improve symmetry of movement for select patient populations 8,10,31. In regard to TKA rehabilitation, McClelland and colleagues 8 have demonstrated use of a force plate system to provide feedback on lower limb weight-bearing during exercise and activity. A limitation to use of force plates is that patients must either hit the plates during dynamic activity, or perform activity where the feet remain relatively stationary on the plates (e.g. squat or lunge activities). A value in using tibial accelerometers is that foot contacts are not limited to placement on the measurement devices. Thus, using tibial-mounted accelerometers can provide patient feedback during training of dynamic activities in community settings.
Study Limitations
Despite the portability, there are limitations to similar use of accelerometers in clinical settings. For example, accelerometers must be placed on the participant’s tibias in a reproducible manner to monitor changes in measures over time. Proper mounting requires time for accurate measurement as well as securing the devices to the skin. In addition, the accelerometers used in this study were wired to the recording device worn around the waist. As with other motion analysis systems, use of a waist belt device may have altered the patient’s movement patterns. Future study is needed to assess the effectiveness of wireless accelerometer systems. Also, the accelerometer system used in this study did not allow real-time feedback to the patient regarding tibial accelerations. Future development is needed to create a system to process the tibial acceleration signals and provide visual or auditory feedback to the patient, so that clinical implementation is feasible for biofeedback training. This system could be further refined by integrating additional movement sensors, such as pressure transducers to assess pressure distribution along the sole of the foot, as has previously been performed in patients with knee OA 32. This addition could, in turn, expand the ability to detect and assess movement asymmetry. It is also important for future work to focus on validating tibial accelerometer measures of movement symmetry against other gold standard measurement systems for movement (such as instrumented three-dimensional motion analysis with video) and force (such as force plates).
5. CONCLUSIONS
In summary, this study provides an example of using tibial accelerometry to measure movement symmetry following unilateral TKA. Decreased movement symmetry during functional tasks such as stair walking for people following TKA is linked to poorer results on common physical performance measures, such as the stair climb time. Developing accelerometer-based systems to measure lower limb movement symmetry during stair and overground walking can assist clinicians in both measuring movement symmetry as well as providing patient feedback during movement retraining following TKA.
Highlights.
Movement symmetry 26 weeks following total knee arthroplasty was examined.
Tibial accelerometers were used during a Stair Climb Test and 6-Minute Walk Test.
Comparisons to healthy participants of similar age were made.
The total knee arthroplasty group had greater between limb asymmetry.
Acknowledgments
The authors acknowledge Dana Judd, DPT, PhD; Mitchell Luce, DPT; Emily Rogers, DPT; and Christy Schlottman for protocol implementation and subject testing support. We also acknowledge the patient participants for volunteering their time.
ACKNOWLEDGEMENT OF FINANCIAL SUPPORT: Sponsored by the Foundation for Physical Therapy and the National Institutes of Health (grant nos. K23-AG029978, R01-HD065900, T32-AG00279).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Christiansen CL, Bade MJ, Judd DL, Stevens-Lapsley JE. Weight-bearing asymmetry during sit-stand transitions related to impairment and functional mobility after total knee arthroplasty. Arch Phys Med Rehabil. 2011;92:1624–9. doi: 10.1016/j.apmr.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083–90. doi: 10.1016/j.orthres.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Boonstra MC, Schwering PJ, De Waal Malefijt MC, Verdonschot N. Sit-to-stand movement as a performance-based measure for patients with total knee arthroplasty. Phys Ther. 2010;90:149–56. doi: 10.2522/ptj.20090119. [DOI] [PubMed] [Google Scholar]
- 4.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon) 2008;23:320–8. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stacoff A, Kramers-de Quervain IA, Luder G, List R, Stussi E. Ground reaction forces on stairs. Part II: knee implant patients versus normals. Gait Posture. 2007;26:48–58. doi: 10.1016/j.gaitpost.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Yoshida Y, Zeni J, Snyder-Mackler L. Do patients achieve normal gait patterns 3 years after total knee arthroplasty? J Orthop Sports Phys Ther. 2012;42:1039–49. doi: 10.2519/jospt.2012.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christiansen CL, Stevens-Lapsley JE. Weight-bearing asymmetry in relation to measures of impairment and functional mobility for people with knee osteoarthritis. Arch Phys Med Rehabil. 2010;91:1524–8. doi: 10.1016/j.apmr.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClelland J, Zeni J, Haley RM, Snyder-Mackler L. Functional and biomechanical outcomes after using biofeedback for retraining symmetrical movement patterns after total knee arthroplasty: a case report. J Orthop Sports Phys Ther. 2012;42:135–44. doi: 10.2519/jospt.2012.3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White SC, Lifeso RM. Altering asymmetric limb loading after hip arthroplasty using real-time dynamic feedback when walking. Arch Phys Med Rehabil. 2005;86:1958–63. doi: 10.1016/j.apmr.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Isakov E. Gait rehabilitation: a new biofeedback device for monitoring and enhancing weight-bearing over the affected lower limb. Eura Medicophys. 2007;43:21–6. doi: 10.3928/01477447-20141023-56. [DOI] [PubMed] [Google Scholar]
- 11.Liikavainio T, Bragge T, Hakkarainen M, Jurvelin JS, Karjalainen PA, Arokoski JP. Reproducibility of loading measurements with skin-mounted accelerometers during walking. Arch Phys Med Rehabil. 2007;88:907–15. doi: 10.1016/j.apmr.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 12.O’Leary K, Vorpahl KA, Heiderscheit B. Effect of cushioned insoles on impact forces during running. J Am Podiatr Med Assoc. 2008;98:36–41. doi: 10.7547/0980036. [DOI] [PubMed] [Google Scholar]
- 13.Turpin KM, De Vincenzo A, Apps AM, et al. Biomechanical and clinical outcomes with shock-absorbing insoles in patients with knee osteoarthritis: immediate effects and changes after 1 month of wear. Arch Phys Med Rehabil. 2012;93:503–8. doi: 10.1016/j.apmr.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 14.Rowlands AV, Stiles VH. Accelerometer counts and raw acceleration output in relation to mechanical loading. J Biomech. 2012;45:448–54. doi: 10.1016/j.jbiomech.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Stiles VH, Griew PJ, Rowlands AV. Use of accelerometry to classify activity beneficial to bone in premenopausal women. Med Sci Sports Exerc. 2013 doi: 10.1249/MSS.0b013e31829ba765. [DOI] [PubMed] [Google Scholar]
- 16.Neugebauer JM, Hawkins DA, Beckett L. Estimating youth locomotion ground reaction forces using an accelerometer-based activity monitor. PLoS One. 2012;7:e48182. doi: 10.1371/journal.pone.0048182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther. 2012;92:210–26. doi: 10.2522/ptj.20110124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forner-Cordero A, Mateu-Arce M, Forner-Cordero I, Alcantara E, Moreno JC, Pons JL. Study of the motion artefacts of skin-mounted inertial sensors under different attachment conditions. Physiological measurement. 2008;29:N21–31. doi: 10.1088/0967-3334/29/4/N01. [DOI] [PubMed] [Google Scholar]
- 19.Herzog W, Nigg BM, Read LJ, Olsson E. Asymmetries in ground reaction force patterns in normal human gait. Med Sci Sports Exerc. 1989;21:110–4. doi: 10.1249/00005768-198902000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Lin YC, Davey RC, Cochrane T. Tests for physical function of the elderly with knee and hip osteoarthritis. Scand J Med Sci Sports. 2001;11:280–6. doi: 10.1034/j.1600-0838.2001.110505.x. [DOI] [PubMed] [Google Scholar]
- 21.LeBrasseur NK, Bhasin S, Miciek R, Storer TW. Tests of muscle strength and physical function: reliability and discrimination of performance in younger and older men and older men with mobility limitations. J Am Geriatr Soc. 2008;56:2118–23. doi: 10.1111/j.1532-5415.2008.01953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parent E, Moffet H. Preoperative predictors of locomotor ability two months after total knee arthroplasty for severe osteoarthritis. Arthritis Rheum. 2003;49:36–50. doi: 10.1002/art.10906. [DOI] [PubMed] [Google Scholar]
- 23.Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:70–80. doi: 10.1053/apmr.2002.27337. [DOI] [PubMed] [Google Scholar]
- 24.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–37. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 25.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Statist Soc. 1995;57:289–300. doi: 10.2307/2346101. [DOI] [Google Scholar]
- 26.Benjamini Y, Yekateuli D. The control of false discovery rate in multiple testing under dependency. Annal Statist. 2001;29:1165–88. doi: 10.2307/2674075. [DOI] [Google Scholar]
- 27.Mandeville D, Osternig LR, Chou LS. The effect of total knee replacement on dynamic support of the body during walking and stair ascent. Clin Biomech (Bristol, Avon) 2007;22:787–94. doi: 10.1016/j.clinbiomech.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Milner CE, O’Bryan ME. Bilateral frontal plane mechanics after unilateral total knee arthroplasty. Arch Phys Med Rehabil. 2008;89:1965–9. doi: 10.1016/j.apmr.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 29.Olin ED, Gutierrez GM. EMG and tibial shock upon the first attempt at barefoot running. Hum Mov Sci. 2013;32:343–52. doi: 10.1016/j.humov.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech (Bristol, Avon) 2011;26:78–83. doi: 10.1016/j.clinbiomech.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cowey A. The Ferrier Lecture 2004 what can transcranial magnetic stimulation tell us about how the brain works? Philos Trans R Soc Lond B Biol Sci. 2005;360:1185–205. doi: 10.1098/rstb.2005.1658. WHHTQC6LRA3GK9Y3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liikavainio T, Isolehto J, Helminen HJ, et al. Loading and gait symmetry during level and stair walking in asymptomatic subjects with knee osteoarthritis: importance of quadriceps femoris in reducing impact force during heel strike? The Knee. 2007;14:231–8. doi: 10.1016/j.knee.2007.03.001. [DOI] [PubMed] [Google Scholar]