Abstract
Healthcare-seeking behaviours of HIV-infected mothers in sub-Saharan Africa are poorly characterized and typically focus on individual health conditions rather than overall health. We conducted a qualitative study to understand how HIV-infected mothers, their male partners, and their HIV-exposed infants seek medical services. We performed 32 in-depth interviews (17 female, 15 male) and four focus group discussions (FGDs) among HIV-infected postpartum women and their male partners in Nairobi, Kenya. We used a grounded theory approach to explore the paths followed for health-related concerns. Female participants reported that willingness to be tested for HIV influences whether women sought antenatal care and the type of facility they preferred for childbirth. The need for medical care outside regular clinic hours and securing safe transportation at night were also significant barriers to seeking care. Most men sought services from traditional healers and chemists before HIV diagnosis, and at governmental facilities afterwards. Both men and women sent infants to traditional healers for non-medical conditions such as bewitching and massage, but rarely for medical conditions. Strategies to reduce HIV-related stigma and fears in antenatal and maternity settings, increase access to care after-hours, and improve linkage to HIV care for men early in their infection are needed.
Keywords: HIV, maternal, health-seeking behaviours, male partners, infant
Background
Timely and appropriate HIV/AIDS related service provision is imperative to reduce the spread of HIV and its impact on HIV-infected individuals and family members. Utilisation of healthcare services is essential for HIV-infected women to minimize risk of mother-to-child HIV transmission (MTCT), monitor HIV disease progression, and treat opportunistic infections. Pregnant and breastfeeding women with HIV are a particular focus for health care service provision given the complicated cascade of events necessary for eliminating antepartum, delivery, and postpartum transmission of HIV to infants. Understanding healthcare-seeking behaviours of HIV-infected women and their male partners can inform best practices for delivering prevention of mother-to-child HIV transmission (PMTCT) services and implementing cutting edge treatments, such as pre-exposure prophylaxis (PrEP). Our previous studies have shown that antenatal care settings have proven useful as a venue for HIV prevention interventions (Farquhar et al., 2004; Farquhar et al., 2001; Gara, Pazvakavambwa, Maponga, & Gavaza, 2005; John, Farquhar, Kiarie, Kabura, & John-Stewart, 2008; Kiarie, Richardson, Mbori-Ngacha, Nduati, & John-Stewart, 2004; Orne-Gliemann et al., 2010).
In addition, survival of HIV-exposed children depends on infant access and timely receipt of PMTCT and other health care services (Ciampa et al., 2011). Less than 25% of HIV-exposed infants are tested for HIV early in life and receive the full cascade of services needed to keep them healthy (Ciampa et al., 2011; Sibanda, Weller, Hakim, & Cowan, 2013) Thus, understanding HIV-infected mothers’ attitudes to infant care is directly related to uptake of maternal and infant PMTCT services.
In Kenya, options for healthcare services include government operated healthcare facilities (ranging from dispensaries and clinics to tertiary hospitals), facilities with private medical providers (private for-profit, non-governmental, and faith based organizations), traditional healers, and traditional birth attendants (TBAs). Individuals using traditional methods may do so exclusively, or augment these services with private and/or government healthcare services; however, most Kenyans utilise government healthcare centres for their care (National Coordinating Agency for Population and Development [NCAPD], 2005).
Several studies in sub-Saharan Africa have been conducted on utilisation of specific types of medical services. In Kenya, researchers found that slum-dwelling women face transportation, financial, and poorly resourced facility-level barriers to optimal obstetric care service utilisation (Essendi, Mills, & Fotso, 2011). Accessing facility-based obstetrical care may also be challenging if family members, such as mother-in-laws, would prefer that women receive traditional services and are involved in making health care decisions (White, Dynes, Rubardt, Sissoko, & Stephenson, 2013). In addition, younger maternal age and rural residence have been linked to decreased PMTCT service utilisation (Delva et al., 2010). In Ethiopia, clinic distance, social support, and financial barriers were identified as major impediments to seeking HIV care and treatment (Gugsa, O’Malley, & Stewart, 2011; Talman, 2010). Other studies found that stigma and psychological distress were risk factors for morbidity, mortality, low antiretroviral adherence, poor service utilisation, and potential increased horizontal transmission of HIV (Pulerwitz, Michaelis, Lippman, Chinaglia, & Diaz, 2008; Rao, Feldman, Fredericksen, & al., 2011). However, little is known about the way in which HIV-infected individuals choose between available traditional and allopathic medical services, including barriers influencing those decisions in African settings. In order for medical services to meet the needs of impoverished, urban Kenyan women infected with HIV and their partners, it is important to understand how these individuals seek care for themselves and their HIV-exposed infants.
In this study, we used qualitative methods to describe healthcare-seeking behaviours, barriers and facilitators to seeking healthcare services, and rationale for the choice of healthcare providers among HIV-infected mothers, their male partners, and their HIV-exposed infants.
Methods
Study design and sampling methods
This study was nested within a double-blind, placebo-controlled, randomized clinical trial of valacyclovir suppressive therapy administered to HIV/herpes simplex virus type-2 (HSV-2) co-infected pregnant and postpartum women between 34 weeks gestation through 12 months postpartum conducted at the Mathare North City Council Clinic located in an urban slum in Nairobi, Kenya (Drake et al., 2012). This clinic offers ambulatory care consisting of preventive and curative services, such as antenatal care, family planning, infant vaccinations and growth monitoring, voluntary counselling and testing (VCT) for HIV, and PMTCT services.
A stratified, purposeful sampling strategy was used to identify trial participants eligible to be screened for study participation. Women were eligible for study screening if they were current participants in the trial between 9 and 12 months postpartum, or had exited the trial and were between 12 and 14 months postpartum, as of June 30, 2010. Among the 148 women enrolled in the trial, 77 women met these criteria. In order to maximize the opportunity for women to remain within the 9 to 12 month postpartum eligibility criteria at the time the study procedures were conducted, identification numbers of trial participants were ordered by ascending delivery date, and stratified by health status of infants (healthy or not healthy). Infants were classified as not healthy if they were deceased; experienced severe morbidities, such as HIV infection, pneumonia, malaria, meningitis; were hospitalized; or were wasted or stunted (defined as a weight-for-age Z-score or height-for age Z-score < −2), respectively, calculated from the 2006 World Health Organization reference population (World Heatlh Organization. WHO Child Growth Standards, 2006). Demographic characteristics of female study participants in the trial were linked by patient identifiers for women participating in the qualitative study; no demographics for male partners were collected.
All study procedures were reviewed and approved by the University of Washington Institutional Review Board and the Kenyatta National Hospital/University of Nairobi Ethics and Research Committee. Written informed consent was obtained for both male and female study participants.
Recruitment of female participants
Women were contacted sequentially by ascending delivery date within each infant health status strata to participate in either an in-depth interview (IDI) or a focus group discussion (FGD). Recruitment for participation in IDIs was prioritized before recruitment for participation in FGDs. Recruitment occurred either in the study clinic during a routine trial visit or by telephone. Women were contacted until 17 interviews were performed (8 with women of ill or deceased infants, and 9 with women of healthy children) and 19 women were scheduled for 2 female focus group discussions; 10 mothers of healthy infants in one FGD and 9 mothers of unhealthy infants in the other FGD.
Recruitment of male participants
Women who accepted or declined participation in IDIs and FGDs were asked whether they would like to ask their male partner to participate in an IDI or a FGD. Male partners who were unaware of the woman’s HIV status or participation in the randomized trial, as reported by women, or were <18 years of age were not eligible for study participation. Women were contacted in each infant health status strata in order of ascending delivery dates until 15 male partners participated in the IDIs and 16 men were scheduled to participate in one of two FGDs for males. One male FGD was conducted among men with healthy infants, and one with unhealthy infants.
Qualitative data collection and analysis
Given the exploratory nature of the study, we embarked upon qualitative analyses using a grounded theory approach (Glaser & Strauss, 1967; Strauss, 1987; Strauss & Corbin, 1990) in which no a priori hypotheses were defined, using a constant comparative method (Ayres, Kavanaugh, & Knafl, 2003; Green, 1998). As such, we designed IDI and FGD interview guides with open-ended questions aimed at collecting information about three themes (socioeconomic status, self-efficacy, and economic factors) and the impact of these factors on perceived access to, and use of, healthcare facilities. We explored these topics with HIV-infected postpartum women and their male partners, and inquired about healthcare access and use for their infants. We also asked interviewees about their healthcare-seeking behaviours and partner/family involvement in infant healthcare decisions. The average duration of IDIs and FGDs was 1 hour and 2.5 hours, respectively. Data gathered from interviews with women were analysed separately from that gathered from men, and a stratified analysis was conducted across sexes based on infant health status.
Thirty-two IDIs and four FGDs (2 male and 2 female, with 7 to 10 participants in each FGD) were conducted at the Mathare North City Council Clinic between July and August 2010. Two Kenyan social scientists conducted the IDIs and one senior social scientist conducted all FGDs with the assistance of a note taker, who recorded impressions and non-verbal information observed. Prior to study commencement, IDI and FGD instruments were pilot tested to refine questions and ensure all staff understood what concepts each question aimed to ascertain. IDIs and FGDs were audio-recorded and conducted in Kiswahili, the language within which participants were most comfortable. Social scientists conducting IDIs were responsible for transcribing and translating their own interviews; similarly, the note taker present translated and transcribed FGDs. All transcription and English translation occurred within one week of the interview.
Transcripts were imported into Atlas.ti version 6.2, openly coded, and organized into themes representing healthcare-seeking behaviours of HIV-infected women, male partners, and their infants. A random selection of 25% of the interviews (N=8) was independently reviewed for themes by a second coder.
Results
Demographics of study participants
The median age of HIV-infected female IDI and FGD participants was 28 years (interquartile range [IQR] 24–33), 67% were married, and 28% were employed and a median monthly rent of US$20 (IQR $13–31). Median gravida was 2 (IQR 1–3) and 31 (86%) delivered in a facility (87% government facilities [55% at the maternity ward at Mathare North]), 13% at private facilities, and 4 (11%) at home. Among 15 male IDI participants, 12 (80%) disclosed their HIV positive status during interviews; HIV status was not disclosed during male FGDs to protect participant confidentiality. Among all 15 male and 17 female IDI participants (32 total), 4 (12%) had an infant die, and 6 (19%) had a severely ill infant during the first year of life, 1 of whom was HIV-infected.
Healthcare-seeking behaviours
Healthcare-seeking behaviours reported by parents of healthy infants were similar to those reported by parents of infants who were ill or subsequently died; therefore, we present themes that emerged from IDIs and FGDs for both groups combined.
HIV-infected peripartum women
Female FGD participants cited willingness to test for HIV as a key determinant of where women initiate antenatal care. Women willing to be tested were thought to prefer to receive care at government healthcare centres, whereas women not willing to be tested either do not seek antenatal care or visit TBAs for both antenatal care and delivery. While all FGD and IDI participants sought antenatal care from government healthcare centres, they also acknowledged supplementing care with visits to TBAs for services not performed at these facilities, such as ‘turning the baby’ (massaging the uterus to position the baby properly for delivery). One advantage women cited of attending a government healthcare centre for antenatal care was facility registration, which grants expedited access to the facility at the time of delivery.
Factors affecting delivery location included risk of adverse pregnancy outcomes and fear of MTCT; women in IDIs described choosing where to deliver after they knew their HIV status. Women with ‘low-risk’ pregnancies were more likely to deliver at government healthcare centres, whereas women with ‘high-risk’ pregnancies were more likely to deliver at the local tertiary government facility that exclusively provides maternity services following referral to these tertiary facilities by health care providers. Most study participants did not go to TBAs for their delivery for fear that they would transmit the HIV infection to their newborn. One female IDI participant stated:
If you deliver in a hospital the doctors will take good care of you and your baby, like me because I am HIV positive, if I go to traditional birth attendants, they help me deliver but they might mess up hence the baby might swallow some of my blood. But when you go to a doctor, first they will look at your files and during delivery they will take precautions so that the baby will be safe from infection during delivery.
Following delivery, women sought healthcare services from government healthcare centres, traditional healers, and local chemists depending on the illness type, time of illness onset, income, and health insurance status. Most women sought treatment for their own illnesses at government healthcare centres; however, women were more likely to report seeking care at private facilities if they had health insurance or a regular income. Women rarely went to traditional healers for standard postpartum medical care, but admitted seeking services for ‘illnesses that doctors cannot treat,’ such as mental illness, familial strife (e.g., husband’s heavy drinking or affairs), and bewitching. Women also reported that they sought healthcare services from a local chemist (pharmacy) if the illness was mild, it was late at night, or it was the weekend.
Female IDI and FGD participants described several factors influencing which type of healthcare facility they selected for their care. Women valued the advice they received from healthcare providers, community health workers, and support group members at government healthcare centres. At both government healthcare centres and private clinics, women felt they received appropriate and effective treatment from healthcare workers for minor ailments. In addition, women perceived capacity to conduct laboratory tests as a benefit of seeking care at these facilities. In contrast, women reported being concerned that traditional healers distributed inappropriate ‘medicine’ and were unable to test for diseases such as malaria and tuberculosis. Female participants preferred government healthcare centres over private clinics and traditional healers due to less expensive fees, perception that non-government providers were driven by ‘money-seeking’ rather than improving patient health, and a general distrust of the traditional healers. One female IDI participant stated:
Those people can give you witchcraft in the name of medicine. I don’t trust their concoctions.
HIV-exposed infants
All female participants said they took their infants to government healthcare centres for medical care. One reason women preferred to take their infants to these facilities was that medications were often dispensed free of charge. Women said infants were taken to private facilities only if a problem occurred at night or on a weekend, or to a chemist (pharmacy) for mild health conditions (e.g., runny nose) or over-the-counter medications. When asked about factors that might prevent parents from taking their infant to the doctor, most women replied with statements echoing the following remark by a female IDI participant:
There is nothing that can prevent me from seeking medical attention when I really see my child is sick. There is nothing because the health of my baby is very important.
Some women also indicated utilising traditional healers for their infants’ care for medical problems and services not offered by allopathic providers but did not seek their assistance for infant illnesses or medication. For example, one woman sought a traditional healer to obtain herbs to bathe the infant, which was prescribed to counteract the father’s predilection for having many female sexual partners outside of marriage. Many women also described taking their infants to TBAs for massage. Mothers even refrained from using traditional healers for infant medical care when the infants’ fathers were traditional healers:
Interviewer: Why can’t you tell his father [who is a traditional healer] to give him some traditional medicines?
Female IDI Participant: What if they are strong and overpower him? I can’t give him such, he is still young. He cannot stand that medicine because of the dosage. You know you can think you know the dosage but you overdose him. How will you remove it and it is already in the body? So I can’t give him or tell him [husband] to give it.
Another male IDI participant said:
I fear them [traditional healers] because they have no experience to deal with children that is why I fear them.
When probed about hypothetical factors that may prevent parents from seeking care for their infant, such as time of day, lack of transportation, religious beliefs or cost, most parents agreed that a child being ill at night was the biggest barrier to seeking care when night-time travel and a lack of safe transportation created security concerns. Both male and female participants said employer permission, approval of others, traditional beliefs, religion, cost, and distance were not barriers to seeking care. Male and female participants also indicated that both partners were responsible for making financial and child healthcare decisions, and partner approval was not a barrier to seeking care. In addition, nearly all (97%) IDI participants felt that their infant’s sex was irrelevant when deciding whether to seek medical care, as indicated by the following exchange with a male IDI participant:
Interviewer: The way you make this boy’s decision when he is sick, would it be different if he was a girl?
Participant: It cannot be different. A baby is a baby.
Interviewer: Why no difference?
Participant: What for? She is mine. It is good even in a family whoever God gives you, it’s a baby. Even if it is a boy or a girl, all are children. Just rejoice for what you have got… It is God who gives, so a baby is a baby, you must love him or her.
One participant who did feel the infant’s sex was relevant when seeking health services believed care should be sought more quickly for boys than girls. This opinion was based on the perspective that girls are often married off to other families, while boys remain with their parents and are ultimately responsible for the well-being of their parents, siblings, and family home.
Male partners
The majority of men thought government healthcare centres provided the highest quality care and liked the variety of locations, easy access, and medical advice provided at these facilities; however, some men with regular income and/or health insurance also sought care at private clinics. While men appreciated longer operating hours and expedited services available at private clinics, they tended to avoid these clinics for reasons similar to those stated by female study participants: provider distrust and motivation from ‘money-seeking’ rather than improving patient health, and higher costs. Men also expressed concerns about private clinics offering sub-standard quality of care, lacking equipment to conduct laboratory testing for illnesses, and increasing risk of other illnesses and death.
Regardless of whether men sought care at private or government facilities, they were more likely to initiate or be taken for care with chemists and/or traditional healers than women and infants. However, the reasons men sought care from traditional healers were similar to those reported by women. The predominant factors driving men to seek care from traditional healers included provider accessibility, specialization in treatment of conditions not offered by allopathic providers (e.g., bewitching), and the broad spectrum of advice on both medical and psycho-social issues. One male IDI participant indicated traditional healers are valued for filling the gap between services provided by hospitals and the needs of the community, particularly for services related to mental illness:
Perhaps you can have disease related to mind insanity - let’s say you have such a disease and you are told somebody can treat it, you can try if the hospital fails.
Males described changes in provider preferences after the onset of HIV symptoms and diagnosis. Male partners who disclosed their HIV positive status during IDIs said they sought relief from mild health conditions and opportunistic infections by visiting traditional healers and/or chemists before they knew their status. These HIV-infected men began seeking care at government healthcare centres when they became sicker or ran out of money. Most HIV-infected men learned their status at government healthcare centres while others got tested as part of couple’s HIV counselling and testing, where couples are counselled and tested for HIV together at the clinic. Some men avoided seeking care with traditional healers if their illness was too severe to be adequately treated, but instead went to government facilities for medical help, and ultimately HIV testing. These men continued to seek services from government healthcare centres for ongoing HIV care and treatment.
Discussion
In our study, HIV-infected women and male partners of HIV-infected women demonstrated individual trajectories as they navigated the healthcare system. We found acceptance of HIV testing to be an important determinant of seeking antenatal care in medical clinics. Unlike women, who often learned their HIV status through antenatal testing, men became aware of their status when they eventually sought formal medical services after long periods of illness and exhausting other forms of medical care, including chemists and traditional healers. Similar to women, HIV-infected men tended to remain in HIV care and treatment programs after initiating care and only sought alternative providers for medical conditions and services considered outside the scope of allopathic medicine. Men were also committed to ensuring their infants received only formal medical services and sought services for their infants rapidly, even for minor illnesses.
Female study participants chose to seek antenatal services at a government healthcare centre, in order to be registered with the facility and to expedite registration at facilities prior to delivery. Fear of being turned away in labour, or of their newborn being cared for by an unskilled provider that would place the baby at increased risk of HIV infection, also drove their decision-making.
Turan et al. (Turan, Miller, Bukusi, Sande, & Cohel, 2008) suggest fear associated with HIV testing affects uptake of labour and delivery services since women often learn their HIV status through HIV testing integrated into antenatal care programs. Fear may be one factor that contributes to the lack of improvement in maternal health in sub-Saharan Africa. Our findings support this hypothesis: female participants reported that women who were afraid of being tested stayed clear of the government healthcare centres; they either did not seek antenatal care or sought it from a TBA. Although women can opt-out of HIV testing during antenatal care in Kenya, women did not mention this option and may not be aware of this choice or feel licensed to opt-out.
In Kenya, over 80% of pregnant women were offered HIV testing services during pregnancy in 2010 (Organization, HIV/AIDS, & Fund, 2011), and many women in this study also learned of their HIV positive status through antenatal testing. This approach of ‘bundling’ services has been very successful at identifying infections, linking women into HIV care and treatment, and PMTCT. In contrast, uptake of HIV testing among men is low; men are typically not engaged in regular medical care and often do not seek out HIV testing, or fail to link to care and treatment after testing positive. To make it easier for HIV-infected women to share their status and gain support from male partners, Kenya and several other sub-Saharan African countries have incorporated couple counselling into antenatal care, thus promoting HIV testing of both partners simultaneously and mutual disclosure of status. Yet, uptake of couple counselling remains <20% in the majority of antenatal settings (Osoti, Han, Kinuthia, & Farquhar, 2014). Strategies to improve male involvement in antenatal care, such as making clinics male-friendly and home-based HIV counselling and education of male and female partners together, may improve maternal and infant health. (Aluisio et al., 2011). Male HIV testing through couple counselling could also result in earlier HIV diagnosis, linkage to care, and improved health outcomes for men (Osoti et al., 2014).
Healthcare-seeking behaviours changed significantly after HIV disease onset and/or diagnosis. Prior to knowing their status, male partners were more willing to delay seeking care until their symptoms escalated, and they treated their symptoms with medications dispensed by a local chemist. After HIV diagnosis, both men and women promptly sought care at government healthcare centres and did not delay seeking care for their infants. Since chemists and traditional healers are frequently utilised by men and women prior to HIV testing and diagnosis, including these providers in HIV prevention, testing, and treatment efforts could be an innovative means of developing effective programs to impact uptake of HIV testing. For example, chemists could refer clients seeking medical advice for illnesses often recognized as consistent with HIV infection or traditional healers/TBAs could promote HIV testing as an approach to early diagnosis and linkage to care.
Key determinants of healthcare-seeking behaviours among HIV-infected peripartum women and their male partners included facility location, cost, perceived quality of medical advice and treatment, and trust of providers. These determinants were similar to those reported by Fonck et al. (2011) on health-seeking behaviours of sexually transmitted diseases patients in Nairobi: location of services and cost were strongly associated with selection of healthcare providers (Fonck et al., 2001). Thus, in order to enhance service utilisation among HIV-infected women and their families, facilities need to be conveniently located and offer low cost services and effective treatment. In addition, ensuring providers are adequately trained to offer high quality medical services, including training in strengthening patient-provider communication, will also be important to meet the needs of this vulnerable population.
While men and women primarily attending government or private clinics felt the services they received adequately met their needs, many participants felt that other services could only be provided by traditional healers (such as bewitching and spousal infidelity) and women described augmenting their care with traditional providers for these services. While women in our study did not report visiting TBAs for postpartum services, 25% of women in the larger trial from which our study participants were recruited delivered at a non-governmental facility (4% specifically with a TBA) despite receiving antenatal care and HIV testing at a governmental facility (Drake et al., 2012). Another study conducted in Kenya found that women sought postpartum, in-home services from TBAs (Cotter, Hawken, & Temmerman, 2006). These contradictory findings suggest there is variation in the use of traditional services and allopathic medical care across studies.
Mothers and male partners interviewed in this study uniformly said that they did and would proceed directly to government health facilities at the first sign of illness in their infants, and were also capable of accurately perceiving infant illnesses severity. However, they also acknowledged that their intentions may be influenced by logistical barriers to promptly receiving care, such as securing safe transportation at night, which may result in delaying medical care for infants until advanced signs and symptoms develop. Infants are also particularly vulnerable and may face rapid decompensation; thus even if they are brought to care quickly, they may still do poorly.
Our study has several strengths. We conducted both IDIs and FGDs with a large number of participants, included both HIV-infected women and their male partners, and obtained information about healthcare-seeking behaviours for women, men, and for their HIV-exposed infants. This holistic approach provided family-centric information about treatment seeking patterns in Kenya. The study instruments were designed to elucidate themes related to healthcare-seeking behaviour and utilisation, including directed probes to follow-up with responses from study participants. In addition, interviews were conducted by native Kiswahili speakers who were familiar with local culture and customs. This study is also subject to several limitations. First, female participants were already enrolled within a larger study of women seeking care from a Nairobi-based government facility, and were receiving monetary compensation for study involvement and free medical care for themselves and their infants. Male participants were referred through these women, and were only eligible for study participation if they were aware of the women’s HIV positive status, and may have been more likely to be involved in the formal medical system. In the larger trial cohort, over half of the women did not disclose their HIV status to their partners after diagnosis and through 12 months postpartum (Roxby et al., 2013). Therefore, our results may not be generalizable to HIV-infected women who have not disclosed their HIV status (and their male partners), women and their male partners who have not sought formal medical care, women who opt to use TBAs for antenatal and delivery services, or men and women in other areas of Kenya.
Our study provides insight into the way in which HIV-infected women, and their male partners and infants, utilise alternative services in conjunction with allopathic medicine. Understanding barriers to families seeking care, including HIV testing and care, and access points with different provider types may help guide development of novel strategies to improve linkage to, and retention, in HIV care and treatment programs.
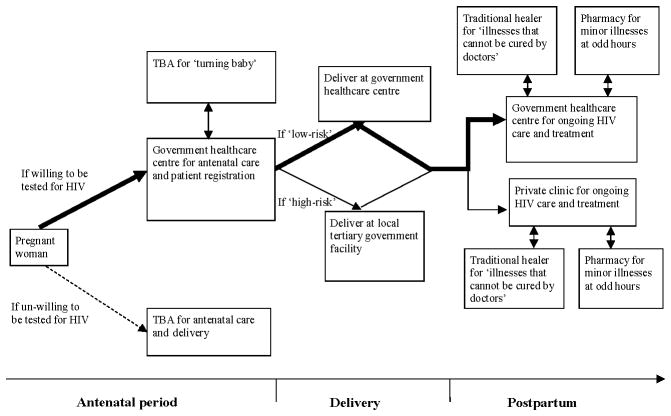
Figure 1.
Service utilisation patterns among HIV-infected mothers in the peripartum period. Line density reflects proportion of women. TBA=traditional birth attendant.
Footnotes
Disclosure statement
The authors have no disclosures or conflicts of interests.
References
- Aluisio A, Richardson BA, Bosire R, John-Stewart G, Mbori-Ngacha D, Farquhar C. Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV-free survival. J Acquir Immune Defic Syndr. 2011;56(1):76–82. doi: 10.1097/QAI.0b013e3181fdb4c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres L, Kavanaugh K, Knafl KA. Within-Case and Across-Case Approaches to Qualitative Data Analysis. Qualitative Health Research. 2003;13(6):871–883. doi: 10.1177/1049732303013006008. [DOI] [PubMed] [Google Scholar]
- Ciampa PJ, Burlison JR, Blevins M, Sidat M, Moon TD, Rothman RL, Vermund SH. Improving retention in the early infant diagnosis of HIV program in rural Mozambique by better service integration. J Acquir Immune Defic Syndr. 2011;58(1):115–119. doi: 10.1097/QAI.0b013e31822149bf. [DOI] [PubMed] [Google Scholar]
- Cotter K, Hawken M, Temmerman M. Low use of skilled attendants’ delivery services in rural Kenya. J Health Popul Nutr. 2006;24(4):467–471. [PMC free article] [PubMed] [Google Scholar]
- Delva W, Yard E, Luchters S, Chersich M, Muigai E, Oyier V, Temmerman M. A Safe Motherhood Project in Kenya: assessment of antenatal attendance, service provision and implications for PMTCT. Trop Med Int Health. 2010;15(5):584–591. doi: 10.1111/j.1365-3156.2010.02499.x. [DOI] [PubMed] [Google Scholar]
- Drake AC, Roxby AL, Ongecha-Owuor F, Kiarie J, John-Stewart G, Wald A, Farquhar C. Valacyclovir Suppressive Therapy Reduces Plasma and Breast Milk HIV-1 RNA Levels during Pregnancy and Postpartum: a Randomized Trial. Journal of Infectious Diseases. 2012;205(3):366–375. doi: 10.1093/infdis/jir766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essendi H, Mills S, Fotso J. Barriers to formal emergency obstetric care services’ utilization. Journal of Urban Health. 2011;88(Supp 2):S356–369. doi: 10.1007/s11524-010-9481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, John-Stewart GC. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37(5):1620–1626. doi: 10.1097/00126334-200412150-00016. 00126334-200412150-00016 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar C, Mbori-Ngacha DA, Bosire RK, Nduati RW, Kreiss JK, John GC. Partner notification by HIV-1 seropositive pregnant women: association with infant feeding decisions. AIDS. 2001;15(6):815–817. doi: 10.1097/00002030-200104130-00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonck K, Mwai C, Rakwar J, Kirui P, Ndinya-achola J, Temmerman M. Healthcare-seeking behavior and sexual behavior of patients with sexually transmitted diseases in Nairobi, Kenya. Sexually Transmitted Diseases. 2001;28(7):367–371. doi: 10.1097/00007435-200107000-00002. [DOI] [PubMed] [Google Scholar]
- Gara CP, Pazvakavambwa I, Maponga CC, Gavaza P. An investigation of the factors influencing the choice of infant feeding methods among urban Zimbabwean women in the context of HIV transmission. Cent Afr J Med. 2005;51(1–2):1–4. [PubMed] [Google Scholar]
- Glaser B, Strauss A. The discovery of grounded theory. Chicago: Aldine Publishing; 1967. [Google Scholar]
- Green J. Commentary: Grounded theory and the constant comparative method. British Medical Journal. 1998;316(7137):1064–1065. [PubMed] [Google Scholar]
- Gugsa S, O’Malley G, Stewart G. Determinants of retention and clinical response 6 months after initiation of antiretroviral treatment in Ethiopian public HIV treatment program. International Training and Education Center (I-TECH); 2011. Under Review. [Google Scholar]
- John FN, Farquhar C, Kiarie JN, Kabura MN, John-Stewart GC. Cost effectiveness of couple counselling to enhance infant HIV-1 prevention. Int J STD AIDS. 2008;19(6):406–409. doi: 10.1258/ijsa.2008.007234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiarie JN, Richardson BA, Mbori-Ngacha D, Nduati RW, John-Stewart GC. Infant feeding practices of women in a perinatal HIV-1 prevention study in Nairobi, Kenya. J Acquir Immune Defic Syndr. 2004;35(1):75–81. doi: 10.1097/00126334-200401010-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization, W. H., HIV/AIDS, J. U. N. P. o., & Fund, U. N. C. s. Toward Universal Access: Scaling up Priority HIV/AIDS Interventions in the Health Sector. 2011. [Google Scholar]
- Orne-Gliemann J, Tchendjou PT, Miric M, Gadgil M, Butsashvili M, Eboko F, Dabis F. Couple-oriented prenatal HIV counseling for HIV primary prevention: an acceptability study. BMC Public Health. 2010;10:197. doi: 10.1186/1471-2458-10-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osoti A, Han H, Kinuthia J, Farquhar C. Role of male partners in the prevention of mother-to-child HIV transmission. Research and Reports in Neonatology. 2014;4:131–138. [Google Scholar]
- Pulerwitz J, Michaelis A, Lippman S, Chinaglia M, Diaz J. HIV-related stigma, service utilization, and status disclosure among truck drivers crossing the Southern borders in Brazil. AIDS Care. 2008;20(7):764–770. doi: 10.1080/09540120701506796. [DOI] [PubMed] [Google Scholar]
- Rao D, Feldman B, Fredericksen R, et al. A Structural Equation Model of HIV-Related Stigma, Depressive Symptoms, and Medication Adherence. AIDS and Behavior. 2011 doi: 10.1007/s10461-011-9915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roxby AC, Matemo D, Drake AL, Kinuthia J, John-Stewart GC, Ongecha-Owuor F, Farquhar C. Pregnant women and disclosure to sexual partners after testing HIV-1-seropositive during antenatal care. AIDS Patient Care STDS. 2013;27(1):33–37. doi: 10.1089/apc.2012.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibanda EL, Weller IV, Hakim JG, Cowan FM. The magnitude of loss to follow-up of HIV-exposed infants along the prevention of mother-to-child HIV transmission continuum of care: a systematic review and meta-analysis. AIDS. 2013;27(17):2787–2797. doi: 10.1097/QAD.0000000000000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss A. Qualitative analysis for social scientists. Cambridge: Cambridge University Press; 1987. [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. London: Sage; 1990. [Google Scholar]
- Talman A. Predictors of Patient Retention and Mortality in the First Six Months after Initiating Antiretroviral Therapy at Felege Hiwat Referral Hospital, Bahir Dar, Ethiopia. University of Washington; 2010. [Google Scholar]
- Turan J, Miller S, Bukusi E, Sande J, Cohel C. HIV/AIDS and maternity care in Kenya: how fears of stigma and discrimination affect uptake and provision of labor and delivery services. AIDS Care. 2008;20(8):938–945. doi: 10.1080/09540120701767224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White D, Dynes M, Rubardt M, Sissoko K, Stephenson R. The influence of intrafamilial power on maternal health care in Mali: perspectives of women, men and mothers-in-law. Int Perspect Sex Reprod Health. 2013;39(2):58–68. doi: 10.1363/3905813. [DOI] [PubMed] [Google Scholar]
- World Heatlh Organization. WHO Child Growth Standards. 2006 Retrieved from http://www.who.int/childgrowth/standards/en/