Abstract
Objective
To describe factors and provider characteristics associated with weight-related counseling practices among U.S. obstetrician-gynecologists (OB/GYNs).
Methods
Data were from a 2010 cross-sectional survey of 250 OB/GYNs. The OB/GYNs were asked how often they used pre-pregnancy body mass index (BMI) to determine the appropriate range of gestational weight gain (GWG), counseled pregnant patients on appropriate rate of GWG, and counseled postpartum patients on weight loss or maintenance. They were also asked how often they counseled pregnant and postpartum patients on five weight-related behaviors [consumption of Fruits and Vegetables (FV), Sugar-Sweetened Beverages (SSB), or high-fat or sugary foods, breastfeeding, and Physical Activity (PA)].
Results
Less than half of providers reported “always” using BMI to determine appropriate GWG (42%); however 65% reported “always” counseling about appropriate GWG rate. About one-third of providers reported counseling about postpartum weight loss or maintenance (38%).Providers reported counseling pregnant and postpartum patients on all weight-related behaviors only 58% and 27% of the time, respectively. Providers with normal BMI had a greater odds of counseling pregnant patients on FV consumption (adjusted odds ratio (aOR): 3.2; 95% confidence interval (CI): 1.5-7.0) and postpartum patients on FV (aOR: 1.9; 95% CI: 1.1-3.6) compared to overweight/obese providers. Providers who exercised regularly had a greater odds of counseling pregnant and postpartum patients on SSB (aOR: 2.2; 95% CI: 1.1-4.8, and aOR: 2.6; 95% CI: 1.4-4.9, respectively) compared to those providers not exercising regularly. Providers who used podcasts for continuing medical education(CME) had a greater odds of providing counseling on several behaviors, including postpartum patients on FV consumption (aOR: 3.1; 95% CI: 1.3-7.2).
Conclusions
Improvements can be made in weight-related counseling practices of OB/GYNs for both pregnant and postpartum patients. Strategies to improve counseling practices, such as podcasts for CME, could be investigated further.
Keywords: Pregnancy, Post-partum, Weight loss, Weight retention, Obesity, Counseling, Health behaviors, Women's health
Introduction
In the United States, 59% of women of reproductive age (20-39 years of age) are either overweight or obese (defined as body mass index (BMI) ≥ 25 kg/m2) [1]. Almost a third of women in this age group are obese (BMI ≥ 30 kg/m2). Among women delivering live born infants in 20 states in 2009, pre-pregnancy obesity prevalence was estimated at over 20% [2]. The prevalence of pre-pregnancy obesity in these 20 states displayed an increasing trend between 2003 and 2009 [2]. This is of concern since obesity is associated with an increased risk of preeclampsia, gestational diabetes, congenital anomalies, stillbirths and other adverse birth outcomes [3-6].
In addition to pre-pregnancy BMI, Gestational Weight Gain (GWG) may also influence pregnancy and birth-related outcomes [7,8]. In 2009, the Institute of Medicine (IOM) released revised guidelines for appropriate GWG based on pre-pregnancy BMI [9]. Preliminary estimates from births during 2010 indicate that nearly half of women have GWG in excess of these recommendations [10]. The American College of Obstetrics and Gynecology (ACOG) released guidelines on appropriate GWG and postpartum weight management [11]. Both of these guidelines emphasize the importance of healthy GWG based on pre-pregnancy BMI. In addition, these guidelines emphasize the role of providers in counseling women about behaviors that can aid in achieving appropriate GWG and rate during pregnancy. While there are currently no guidelines on postpartum weight loss, studies show that failure to return to pre-pregnancy weight by six months postpartum is an important predictor of long-term obesity [12].
A 2005 survey of 900 U.S. obstetricians and gynecologists (OB/GYNs) found that the majority of OB/GYNs counsel non-pregnant patients about diet, including specific strategies such as limiting portion size and increasing physical activity [13]. However, only 27% reported referring patients with obesity for behavioral therapy on a frequent basis. Moreover, whereas the majority of OB/GYNs counseled their pregnant patients on GWG, only 65% reported modifying that recommendation based on the patient's pre-pregnancy BMI [13]. A follow-up survey in 2007 demonstrated modest improvements in counseling rates for pregnant women [14]. A comparison of the two surveys also showed that counseling practices of OB/GYNs was associated with having familiarity with ACOG guidelines [15]. Previous studies have also shown that female providers and those providers with normal BMIs report higher rates of counseling [16,17,19].
The objectives of this study were to describe US OB/GYNs’ self-reported counseling practices in relation to the IOM and ACOG guidelines. Specifically, we sought to determine how frequently OB/GYNs used pre-pregnancy BMI to determine the appropriate GWG when counseling pregnant patients, how frequently they counseled pregnant patients on the appropriate rate of GWG, and how frequently they counseled postpartum patients on weight loss or weight maintenance. We also sought to determine whether they counsel pregnant and postpartum patients on specific weight-related behaviors. We examined predictors of these counseling practices including provider demographics, practice setting and personal engagement in health-related behaviors.
Methods
Data were obtained from Doc Styles 2010 -- a web-based panel survey developed by Porter Novelli designed to provide insight into health care provider attitudes, counseling behaviors and use of health information resources regarding a variety of adult and pediatric health issues [20-22]. In addition, the survey includes questions on the provider's height and weight, as well as other questions describing their demographics, health behaviors, and practice characteristics. The Centers for Disease Control and Prevention Human Subjects Review determined that these analyses were exempt from Human Subjects Review because this is a secondary data analysis using data without identifiers.
Porter Novelli utilized a physician sample drawn from the Epocrates Honors Panel, an opt-in, verified panel of over 275,000 medical practitioners across the nation. Respondents were selected to participate in this survey from a panel is drawn to match the American Medical Association's (AMA) master file proportions for age, gender, and region, but were not required to participate and could exit at any time. Respondents were paid an honorarium of $40-$60 for completing the survey. Respondents were screened to include only those who: practice in the United States; actively see patients; work in an individual, group, or hospital practice; and have been practicing for at least three years. No individual identifiers were included in the database. Quotas were set to reach 1,000 primary care physicians, 250 pediatricians, 250 OB/GYNs, 250 retail pharmacists, 250 nurse practitioners, and 150 registered dietitians; once the quotas were met, the survey was closed. For the purposes of this study, only the responses from the 250 OB/GYNs, who were asked our survey questions (Figure 1), were considered. To reach this quota, 431 OB/GYN invitations had to be sent, yielding an overall response rate of 51%.
Figure 1.
Survey questions regarding self-reported counseling practices on weight gain and behaviors among U.S. OB/GYNs-United States, Doc Styles, 2010.
The Doc Styles 2010 survey included 113 questions, some with multiple subparts, which could be selected to be viewed by all or only some of the health providers depending on applicability of question content. Our study asked five questions of OB/GYNs (Figure 1). The first three questions examined the frequency with which OB/GYNs or their staff (1) used pre-pregnancy BMI to modify GWG recommendations, (2) counseled pregnant patients on the appropriate rate of GWG, and (3) counseled postpartum patients on appropriate weight loss or weight maintenance. The possible answers to these three questions were meant to assess intensity of counseling and included “never, rarely, sometimes, often, or always.”The last two questions sought to determine whether OB/GYNs or their staff counseled their pregnant or postpartum patients on five weight-related behaviors (consumption of Fruits and Vegetables (FV), breastfeeding, consumption of high-fat or sugary foods, consumption of Sugar-Sweetened Beverages (SSBs),and Physical Activity (PA)).These questions on weight-related behavior counseling captured whether counseling was provided or not, and did not measure intensity. Respondents were allowed to select one or more behaviors or “none of these behaviors” for each question. The year 2010 was the first that these five questions were asked in the Doc Styles survey.
Bivariate analyses were conducted to explore associations between provider demographics and characteristics and counseling practices. Among these was the provider's BMI, categorized as either normal (BMI ≥ 18.5 kg/m2 and <25 kg/m2) or overweight/obese (BMI ≥ 25 kg/m2). Because there were only 4 respondents who were underweight (BMI <18.5 kg/m2), they were excluded from the analyses. Using podcasts for Continuing Medical Education (CME) was also investigated as a novel means by which providers might learn more about current guidelines as a means to improving their counseling practices. Finally, the provider's personal lifestyle behaviors were investigated as predictors of counseling patterns. Specifically, we examined whether providers who (1) consumed 5 cups of fruits/vegetables per day, 7 days a week compared to those who did not and, (2) engaged in physical activity to maintain an elevated heart rate for 30 minutes or more on >5 days per week compared to those who did not were more likely to counsel their patients on the selected measures.
For multivariate regression models, variables that were significant at p<0.05 in bivariate analyses were included. If a variable was significant in any of the bivariate analyses it was included in all of the multivariate regression models. We developed three sets of multivariate logistic regression models. We first examined the potential predictors of responding to“always”for all three questions regarding weight management practices; i.e., (1) using pre-pregnancy BMI to modify GWG recommendations, (2) counseling pregnant patients on the appropriate rate of GWG, and (3) counseling postpartum patients on appropriate weight loss or weight maintenance.
A second set of multivariate regression models examined potential predictors of counseling pregnant patients on each of the five weight-related behaviors. The third set of multivariate regression models examined potential predictors of counseling postpartum patients on each of the five weight-related behaviors.
Statistical analysis was completed using SPSS v.19 (IBAM Corp., Armonk, NY). We calculated means and frequencies of OB/GYN characteristics. We used chi-squared tests to explore bivariate relationships between OB/GYN characteristics and responses to questions on weight management practices and behavioral counseling.
Results
Of the 250 OB/GYNs who completed the survey, 55% were aged 45 years or older, 62% were male and 77% were non-Hispanic white (Table 1). These providers saw a mean of 107 patients per week and had been practicing medicine for an average of 16 years. About 80% worked in a group or hospital practice. Approximately 46% of OB/GYNs had a normal BMI and 53% had a BMI corresponding to overweight/obese. OB/GYNs ate 5 or more cups of fruits and vegetables on a median of 4 days/week; however, only 16% reported eating 5 or more cups of fruits and vegetables on each day of the week. Only 27% of OB/GYNs exercised for at least 30 minutes a day on ≥5 days/week. Only 12% of OB/GYNs reported using podcasts “always” or “often” for CME purposes.
Table 1.
Personal and Professional Characteristics of Surveyed OB/GYNs.
| Characteristic | Proportions* (n=250) |
|---|---|
| Age (mean) | 46.6 |
| ≥ 45 years | 55.0 |
| Sex | |
| Male | 61.6 |
| Female | 38.4 |
| Race | |
| White | 77.2 |
| Non-White | 22.8 |
| Patients seen per week | |
| Mean | 107 |
| Median | 100 |
| Years practicing medicine | |
| Mean | 16 |
| Median | 15 |
| Work setting | |
| Individual Practice | 20.0 |
| Group practice | 69.2 |
| Hospital Clinic | 10.8 |
| Provider BMI, mean (kg/m2) | 25.6 |
| <18.5 kg/m2 | 1.6 |
| ≥ 18.5 kg/m2 , <25 kg/m2 | 45.6 |
| ≥ 25 kg/ m2 , <30 kg/ m2 | 38.8 |
| ≥ 30 kg/ m2, <35 kg/m2 | 10.4 |
| ≥ 35 kg/m2 | 3.6 |
| Eat at least5 cups of fruits and vegetables (days/week) | |
| Mean | 3.6 |
| Median | 4.0 |
| Eat at least 5 cups of fruits and vegetables 7 days/week | 16.4 |
| Exercise for at least 30 minutes (days/week) | |
| Mean | 3.2 |
| Median | 3.0 |
| Exercise for at least 30 minutes/day≥ 5 days/week | 26.8 |
| Uses podcasts for continuing medical education (always or often) | 12.4 |
This table provides a summary description of demographic and personal characteristics of obstetricians and gynecologists (OB/GYNs) who responded to the survey.
Proportions are displayed unless indicated otherwise.
BMI: Body mass index.
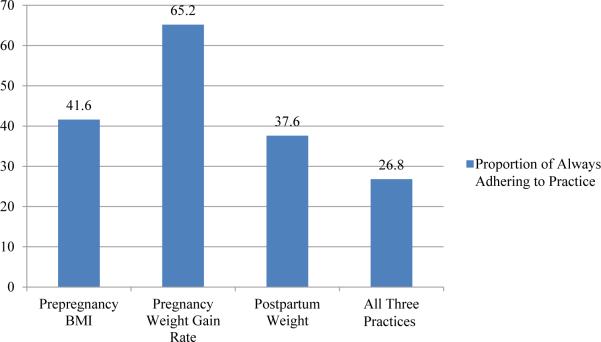
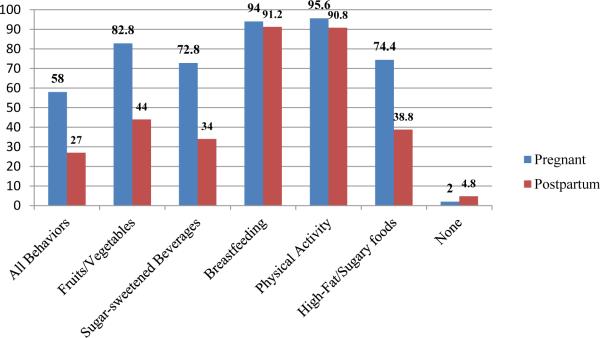
Forty-two percent (42%) of OB/GYNs responded they always used pre-pregnancy BMI to modify recommendations for GWG (Figure 2); 65% of OB/GYNs reported always counseling about appropriate rate of GWG. Finally, 38% of OB/GYNs reported always counseling postpartum patients on appropriate weight loss or maintenance. Overall, only 27% reported always adhering to all three weight management practices. For the specific weight-related behaviors (Figure 3), the frequency of “always” counseling pregnant patients exceeded 70% for each behavior. For counseling postpartum patients this ranged between 34% (counseling on SSB consumption) and 91% (breastfeeding and PA). Overall, approximately 58% of OB/GYNs provided counseling for pregnant patients on all of the behaviors, compared to 27% on all the behaviors for postpartum patients. By comparison, very few providers reported not counseling on any behaviors for pregnant (2%) and postpartum patients (4.8%).
Figure 2. Proportion of OB/GYNs Reporting “Always” Adhering to Specific Weight Management Practices.
The proportion of obstetricians and gynecologists (OB/GYNs) reporting “always” adhering to three weight management practices is shown. The specific questions on weight management practices were if the OB/GYN or practice: (1) Use pre-pregnancy BMI to modify recommendation for weight gain during pregnancy (Pre-pregnancy BMI)?; (2) Counsel pregnant patients on appropriate rate of weight-gain during pregnancy (Pregnancy Weight Gain Rate)?; (3) Counsel postpartum patients on appropriate weight loss or weight maintenance (Postpartum Weight)? The proportion responding “always” for all 3 practices is also shown.
Figure 3. Proportion of OB/GYN Providers Reporting Counseling Pregnant or Postpartum Patients on Five Specific Weight-Related Behaviors.
This figure depicts the proportion of obstetricians and gynecologists (OB/GYNs) who responded to ever counseling on each of these five weight-related behaviors and the proportions reporting counseling on all or none of the behaviors.
Logistic regression modeling revealed that providers with normal BMIs had a significantly greater odds than those with overweight/obesity of adhering to all three weight management practices (adjusted odds ratio (aOR): 2.6; 95% confidence interval (CI): 1.3-4.9) (Table 2). No other provider characteristics were significantly associated with adherence to the three weight management practices.
Table 2.
Logistic Regression Model of “Always” Using Prepregnancy BMI to Modify Gestational Weight Gain (GWG) Recommendations, Counseling Pregnant Patients on the Appropriate rate of GWG and Counseling Postpartum Patients on Weight Loss or Maintenance.
| Independent Variable | %† | aOR | 95%CI |
|---|---|---|---|
| Sex | |||
| Male | 21 | – | |
| Female | 36 | 1.7 | 0.9–3.3 |
| Body Mass Index (BMI)* | |||
| Overweight/Obese | 20 | – | |
| Normal | 61 | 2.6 | 1.3–4.9 |
| Exercises at least 30 min on ≥5 days/week | |||
| No | 23 | – | |
| Yes | 36 | 1.7 | 0.9–3.4 |
| Consumes at least 5 cups fruits/vegetables 7 days/week | |||
| No | 26 | – | |
| Yes | 30 | 0 8 | 0.3–1.8 |
| Podcasts for CME | |||
| Less than often | 26 | – | |
| Always, Often | 35 | 2.1 | 0.8–5.0 |
| Work setting | |||
| Individual | 24 | – | |
| Group/Hospital | 28 | 1.0 | 0.5–2.3 |
| Years In Practice | |||
| < 15 | 31 | – | |
| ≥ 15 | 22 | 0.7 | 0.4–1.3 |
| Number of Patients/Week | |||
| < 100 | 25 | – | |
| ≥ 100 | 30 | 1.5 | 0.8–2.8 |
Logistic regression modeling results for predictors of obstetricians and gynecologists always using body mass index (BMI) to modify gestational weight gain recommendations, counseling pregnant patients on the appropriate rate of gestational weight gain, and counseling postpartum patients on weight loss/maintenance. Statistically significant results are set in bold.
Percent (%) represent the proportion of respondents in that category who provided counseling.
Body mass index defined as normal (BMI ≥18.5 kg/m2 and <25 kg/m2) or overweight/obese (BMI ≥25 kg/m2)
aOR: adjusted odds ratio; CI: confidence interval; CME: continuing medical education.
In general, providers who had a normal BMI and maintained a healthier lifestyle had greater odds than their counterparts of counseling their pregnant and postpartum patients on weight-related behaviors (Tables 3 and 4, respectively). There were notable differences between the counseling of pregnant and postpartum patients including, for example: the use of podcasts always/often for CME was associated with counseling on healthier behaviors only for postpartum patients. Because of the very high prevalence of counseling on breastfeeding and PA (Figure 3) and resultant small sample sizes of non-counseling physicians, regression models are not reported for these two behaviors for pregnant and postpartum patients; although combined models with all behaviors are reported.
Table 3.
Logistic Regression Models for Counseling Pregnant Patients on Specific Health Behaviors
| Fruit and Vegetable Intake | Sugar Sweetened Beverage Intake | High-fat or Sugary Food Intake | All Weight-Related Behaviors | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| %† | aOR | 95%CI | % | aOR | 95%CI | % | aOR | 95%CI | % | aOR | 95%CI | |
| Sex | ||||||||||||
| Male | 82 | – | 71 | – | 74 | – | 58 | – | ||||
| Female | 85 | 1.9 | 0.9–4.6 | 73 | 1.2 | 0.6–2.3 | 76 | 1.3 | 0.7–2.6 | 59 | 1.3 | 0.7–2.4 |
| Body Mass Index* | ||||||||||||
| Overweight/Obese | 76 | – | 70 | – | 72 | – | 56 | – | ||||
| Normal | 88 | 3.2 | 1.5–7.0 | 74 | 1.4 | 0.8–2.7 | 76 | 1.1 | 0.6–2.0 | 60 | 1.5 | 0.8–2.6 |
| Exercises ≥30 min on ≥5 days/week | ||||||||||||
| No | 81 | – | 69 | – | 69 | – | 53 | – | ||||
| Yes | 88 | 1.8 | 0.8–4.6 | 84 | 2.2 | 1.1–4.8 | 88 | 2.8 | 1.2–6.5 | 73 | 2.5 | 1.3–4.9 |
| Consumes ≥5 cups fruits or vegetables 7 days/week | ||||||||||||
| No | 81 | – | 72 | – | 73 | – | 57 | – | ||||
| Yes | 93 | 2.8 | 0.8–9.9 | 78 | 1.2 | 0.5–2.7 | 83 | 1.4 | 0.6–3.4 | 66 | 1.2 | 0.6–2.5 |
| Podcasts for CME | ||||||||||||
| Less than often | 80 | – | 72 | – | 73 | – | 58 | – | ||||
| Always, Often | 86 | 1.8 | 0.5–6.5 | 77 | 1.2 | 0.5–3.1 | 84 | 1.9 | 0.7–5.5 | 65 | 1.3 | 0.6–2.9 |
| Worksetting | ||||||||||||
| Individual | 83 | – | 68 | – | 72 | – | 56 | – | ||||
| Group/Hospital | 84 | 1.1 | 0.5–2.7 | 74 | 1.5 | 0.7–3.0 | 75 | 0.3 | 0.6–2.6 | 59 | 1.2 | 0.6–2.4 |
| Years In Practice | ||||||||||||
| < 15 | 81 | – | 69 | – | 72 | – | 57 | – | ||||
| ≥ 15 | 84 | 1.2 | 0.6–2.5 | 77 | 1.4 | 0.8–2.6 | 77 | 1.2 | 0.7–2.3 | 61 | 1.2 | 0.7–1.9 |
| Number of Patients/Week |
||||||||||||
| < 100 | 81 | – | 70 | – | 70 | – | 56 | – | ||||
| ≥ 100 | 85 | 1.3 | 0.6–2.8 | 77 | 1.3 | 0.7–2.5 | 81 | 1.7 | 0.9–3.2 | 61 | 1.1 | 0.6–1.9 |
Logistic regression modeling results for predictors of obstetricians and gynecologists counseling pregnant patients on specific behaviors: fruit and vegetable and sugar sweetened beverage intake, and high-fat or sugary food intake. A combined model for counseling on all of the specific behaviors, including breastfeeding and PA, is also depicted. Statistically significant results are set in bold.
Percent (%) represent the proportion of respondents in that category who provided counseling on the specific measure.
Body mass index defined as normal (BMI ≥18.5 kg/m2 and <25 kg/m2) or overweight/obese (BMI ≥25 kg/m2)
aOR: adjusted odds ratio; CI: confidence interval; CME: continuing medical education.
Table 4.
Logistic Regression Models for Counseling Postpartum Patients on Specific Health Behaviors.
| Fruit and Vegetable Intake | Sugar Sweetened Beverage Intake | High-fat or Sugary Food Intake | All Weight-Related Behaviors | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| %† | aOR | 95%CI | % | aOR | 95%CI | % | aOR | 95%CI | % | aOR | 95%CI | |
| Sex | ||||||||||||
| Male | 45 | – | 36 | – | 44 | – | 28 | – | ||||
| Female | 42 | 1.0 | 0.5–1.8 | 31 | 0.9 | 0.5–1.7 | 30 | 0.7 | 0.4–1.3 | 25 | 0.9 | 0.5–1.9 |
| Body Mass Index* | ||||||||||||
| Overweight/Obese | 37 | – | 32 | – | 31 | – | 25 | – | ||||
| Normal | 49 | 1.9 | 1.1–3.6 | 35 | 1.3 | 0.7–2.3 | 46 | 2.1 | 1.1–3.9 | 29 | 0.7 | 0.4–1.3 |
| Exercises ≥30 min on ≥5 days/week | ||||||||||||
| No | 40 | – | 28 | – | 32 | – | 22 | – | ||||
| Yes | 54 | 1.8 | 1.0–3.4 | 51 | 2.6 | 1.4–4.9 | 57 | 3.1 | 1.6–5.8 | 40 | 2.2 | 1.1–4.3 |
| Consumes ≥5 cups fruits or vegetables 7 days/week | ||||||||||||
| No | 39 | – | 31 | – | 36 | – | 27 | – | ||||
| Yes | 68 | 3.4 | 1.6–7.3 | 49 | 1.7 | 0.8–3.6 | 51 | 1.6 | 0.7–3.3 | 44 | 2.1 | 1.0–4.6 |
| Podcasts for CME | ||||||||||||
| Less than often | 41 | – | 31 | – | 35 | – | 24 | – | ||||
| Always, Often | 68 | 3.1 | 1.3–7.2 | 55 | 2.7 | 1.2–6.1 | 68 | 3.5 | 1.5–8.2 | 48 | 3.2 | 1.4–7.8 |
| Worksetting | ||||||||||||
| Individual | 44 | – | 28 | – | 34 | – | 18 | – | ||||
| Group/Hospital | 46 | 1.2 | 0.6–2.3 | 36 | 1.6 | 0.8–3.5 | 40 | 1.6 | 0.8–3.5 | 30 | 2.6 | 1.1–6.3 |
| Years In Practice | ||||||||||||
| < 15 | 43 | – | 35 | – | 37 | – | 25 | – | ||||
| ≥ 15 | 45 | 0 9 | 0.5–1.6 | 33 | 1.0 | 0.5–1.7 | 41 | 1.00 | 0.6–1.7 | 29 | 1.1 | 0.6–2.1 |
| Number of Patients/Week | ||||||||||||
| < 100 | 46 | – | 36 | – | 36 | – | 26 | – | ||||
| ≥ 100 | 41 | 0.6 | 0.4–1.1 | 33 | 0.9 | 0.5–1.7 | 43 | 1.1 | 0.6–1.9 | 28 | 0.9 | 0.5–1.7 |
Logistic regression modeling results for predictors of obstetricians and gynecologists counseling postpartum patients on specific behaviors: fruit and vegetable and sugar sweetened beverage intake and high-fat or sugary food intake. A combined model for counseling on all of the specific behaviors, including breastfeeding and PA, is also depicted. Statistically significant results are set in bold.
Percent (%) represent the proportion of respondents in that category who provided counseling.
Body mass index defined as normal (BMI ≥18.5 kg/m2 and <25 kg/m2) or overweight/obese (BMI ≥25 kg/m2)
aOR: adjusted odds ratio; CI: confidence interval; CME: continuing medical education.
Providers with a normal BMI had greater odds than those with overweight/obesity of counseling pregnant patients on FV consumption (aOR: 3.2; 95% CI: 1.5-7.0) (Table 3). Providers who exercised at least 30 minutes/day on ≥ 5 days a week had greater odds of counseling pregnant patients on SSB (aOR: 2.2; 95% CI: 1.1-4.8) and high-fat or sugary food consumption (aOR: 2.8; 95% CI: 1.2-6.5) and all weight-related behaviors (aOR: 2.5; 95% CI: 1.3-4.9) compared to providers who exercised less. A provider's personal level of exercise was not associated with counseling pregnant patients on physical activity. There were no associations for providers who consumed ≥ 5 cups of fruits or vegetables each day of the week or who used podcasts for CME always/often with counseling pregnant patients.
Providers with a normal BMI had greater odds than those with overweight/obese of counseling postpartum patients on FV consumption (aOR: 1.9; 95% CI: 1.1-3.6) and consumption of high-fat or sugary foods (aOR: 2.1; 95% CI: 1.1-3.9) (Table 4). Providers who exercised at least 30 minutes/day on ≥ 5 days a week had greater odds of counseling postpartum patients on SSB consumption (aOR: 2.6; 95% CI: 1.4-4.9), high-fat or sugary food consumption (aOR 3.1; 95% CI: 1.6-5.8) and all weight-related behaviors (aOR: 2.2; 95% CI: 1.1-4.3) compared to providers who exercised less. Providers who consumed at least 5 cups of fruits or vegetables each day of the week had greater odds of counseling postpartum patients on FV consumption (aOR: 3.4; 95% CI: 1.6-7.3) compared to providers consuming less FV. Providers who used podcasts always/often for CME had greater odds of counseling postpartum patients on FV (aOR: 3.1; 95% CI: 1.3-7.2), SSB (aOR: 2.7; 95% CI: 1.2-6.1) and high-fat or sugary consumption (aOR: 3.5; 95% CI: 1.5-8.2) and all weight-related behaviors (aOR: 3.2; 95% CI: 1.4-7.8), compared to those using podcasts less often. Providers who worked in a group or hospital setting had greater odds of counseling postpartum patients on all weight-related behaviors (aOR: 2.6; 95% CI: 1.1-6.3) compared to those working in individual practices.
Discussion
The IOM report, the ACOG committee opinion, and experts provide recommendations on screening for obesity and weight management during pregnancy and through the postpartum period [10,11,23-25]. Research has shown, however, that providers experience barriers to effective screening and weight management including awareness of guidelines and time constraints [26,27]. Other barriers include the provider's perception that he/she may not be effective in counseling [28] or that there are no effective treatments for women of reproductive age with overweight or obesity [13,26]. However, appropriate training has been shown to improve counseling skills and provider self-efficacy [25,26]. Furthermore, there is evidence that counseling women of reproductive age on increasing FV consumption, increasing PA and reducing consumption of less healthy foods and beverages may optimize gestational weight gain and postpartum weight retention [30,31].
Similar to the two ACOG surveys conducted in 2005 and 2007 where nearly two-thirds of OB/GYNs reported using BMI “most of the time” or “often” to provide specific recommendations for gestational weight gain [13,14], we found that our 2010 study suggests that 71% of OB/GYNs “always” or “often” used the woman's pre-pregnancy BMI in their counseling of GWG. Approximately 65% of providers in our sample reported counseling on the appropriate rate of GWG. Our study also observed a similar proportion of OB/GYNs who reported counseling postpartum patients on weight loss: 75% compared to 67% and 72% in the ACOG surveys [13,14]. We did find that providers with normal BMIs had greater odds than those with overweight/obesity to adhere to all three weight management practices.
Regarding specific health behavior counseling for pregnant patients, our study asked about counseling on consumption of FV, sugar sweetened beverages and high-fat or sugary foods as well as counseling on breastfeeding and PA in a single survey. We found that 80% of OB/GYNs report ever counseling pregnant patients on FV consumption, breastfeeding and PA more each. However, only 58% of respondents reported always counseling on all five health behaviors. For postpartum patients, a much smaller proportion of OB/GYNs reported counseling on the specific health behaviors. The notable exceptions were breastfeeding and PA for which 91% of respondents reported ever counseling on each of these behaviors. This is important because breastfeeding may be an important corollary strategy to postpartum weight management [18]. We found that only 27% of OB/GYNs reported counseling on all of the health behaviors for postpartum patients.
To our knowledge, our study was unique in investigating specific behavior counseling rates associated with OB/GYN personal health behaviors. We found that providers who consumed at least 5 cups of FV 7 days/week had greater odds of counseling only for FV consumption for postpartum patients. In comparison, providers who exercised at least 30 minutes/day on >5 days/week had greater odds of counseling on several other behaviors. Unlike other studies, we did not find that years in practice (a proxy for years since residency) or volume of patients were associated with counseling practices. Our findings on practice setting are in contrast to previous studies that have compared physicians in private practice to those in other settings and found either a higher likelihood of providers in private settings than those in academic or hospital settings to counsel patients on healthier behaviors [17] or no differences between groups [16]. One study did find that physicians in non-academic hospital settings were less likely than those in other settings (including academic, private and community settings) to counsel their patients on healthier food behaviors [29]. The reasons for our finding are unclear, but may include that group and hospital-based practices have more resources to incorporate best counseling practices into their clinical practices. However, caution must be used when interpreting these comparisons because these studies included (a) OB/GYNs with other physicians, and (b) other practice sites (e.g., academic), thus making comparisons with our categorization of settings difficult.
Awareness of specific counseling guidelines has been associated with lifestyle counseling, as has use of new sources of medical knowledge [15,16,33]. In our study we examined the use of podcasts as a novel means of CME to enable providers to be more up to date with recent recommendations and counseling practices. In the models examining “always” adhering to the three weight management practices there was no association with the use of podcasts. However, in the models examining “always” counseling of health behaviors, we found that the use of podcasts was associated with counseling postpartum patients on FV, SSB and high-fat or sugary foods consumption, and on all weight related behaviors. However, the question on use of podcasts only asked about their use for CME in general and not for counseling on topics related overweight or obesity in specific. Therefore, the associations we report need to be explored further. Specifically, future studies can investigate the association of provider characteristics on weight management and counseling practices. Furthermore, future studies can assess strategies to improve counseling and patient engagement, e.g., motivational interviewing, in regards to GWG and postpartum weight management. The use of novel means of CME, such as podcasts, can also be explored in interventional studies.
Our study was limited by the fact that the respondent population was derived from quota sampling. Previous ACOG surveys [13,14] involved between 787 and 900 OB/GYNs who were a part of a collaborative research network and reported to be representative of practicing OB/GYNs across the nation. Since our sample was self-selected it may not be nationally representative. However, our findings on the use of BMI for counseling on GWG are similar to those of the previous ACOG surveys. Our respondent pool may have been too small to find any significant associations between certain counseling practices as noted above. The questions we asked aligned very closely with recently released guidelines and recommendations about weight-related counseling, so a social desirability bias may have influenced some of the respondents. For example, this may have overestimated the proportion of physicians reporting “always” counseling. In this study we were unable to differentiate OB/GYNs who practice gynecology only, thus we may have misclassified some respondents as non-frequent counselors when they in fact donot routinely provide care to pregnant and postpartum patients in their practice. Also our study did not assess several factors that might contribute to lower counseling rates, including the providers’ perceived self-efficacy and use of counseling skills such as motivational interviewing [24]. Similar considerations might explain why some associations, e.g., with providers’ exercise habits and use of podcasts, were found for counseling of postpartum patients, but not pregnant patients.
Conclusion
Providing support and guidance to OB/GYNs may help to improve counseling about weight management to pregnant and postpartum women. Instituting best practice training and tools, such as motivational interviewing and electronic record prompts, respectively, could be useful for providers to increase their perceived self-efficacy. Furthermore, using novel means of keeping providers aware of guidelines and the efficacy of clinical interventions could be useful as well. Specific training on healthy lifestyle behaviors can be systematically included in OB/GYN residency programs and standardized such that future work forces are prepared to counsel around these issues.
Acknowledgments
Funding Sources
This work was made possible through The CDC Experience Applied Epidemiology Fellowship, a public/private partnership supported by a grant to the CDC Foundation from External Medical Affairs, Pfizer Inc.
Abbreviations
- ACOG
American College of Obstetricians and Gynecologists
- aOR
adjusted Odds Ratio
- BMI
Body Mass Index
- FGP
Family or General Practitioner
- IOM
Institute of Medicine
- OB/GYNs
Obstetricians and Gynecologists
- OR
Odds Ratio
- CI
Confidence Interval
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher SC, Kim SY, Sharma AJ, Rochat R, Morrow B. Is obesity still increasing among pregnant women? Prepregnancy obesity trends in 20 states, 2003-2009. Prev Med. 2013;56:372–378. doi: 10.1016/j.ypmed.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Chaar D, Finkelstein SA, Tu X, Fell DB, Gaudet L, et al. The impact of increasing obesity class on obstetrical outcomes. J Obstet Gynaecol Can. 2013;35:224–233. doi: 10.1016/S1701-2163(15)30994-4. [DOI] [PubMed] [Google Scholar]
- 4.Rankin J, Tennant PW, Stothard KJ, Bythell M, Summerbell CD, et al. Maternal body mass index and congenital anomaly risk: a cohort study. Int J Obes (Lond) 2010;34:1371–1380. doi: 10.1038/ijo.2010.66. [DOI] [PubMed] [Google Scholar]
- 5.Scott-Pillai R, Spence D, Cardwell CR, Hunter A, Holmes VA. The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004-2011. BJOG. 2013;120:932–939. doi: 10.1111/1471-0528.12193. [DOI] [PubMed] [Google Scholar]
- 6.Stillbirth Collaborative Research Network Writing Group Association between stillbirth and risk factors known at pregnancy confirmation. JAMA. 2011;306:2469–2479. doi: 10.1001/jama.2011.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hinkle SN, Sharma AJ, Swan DW, Shieve LA, Ramakrishnan U, et al. Excess gestational weight gain is associated with child adiposity among mothers with normal and overweight prepregnancy weight status. J Nutr. 2012;142:1851–1858. doi: 10.3945/jn.112.161158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonald SD, Han Z, Mulla S, Lutsiv O, Lee T, et al. High gestational weight gain and the risk of preterm birth and low birth weight: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2011;33:1223–1233. doi: 10.1016/S1701-2163(16)35107-6. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine . Weight gain during pregnancy: reexamining the guidelines. National Academies press; Washington DC: 2009. [PubMed] [Google Scholar]
- 10.IOM (Institute of Medicine) and NRC (National Research Council) Leveraging action to support dissemination of the pregnancy weight gain guidelines: Workshop summary. The National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
- 11.American College of Obstetricians and Gynecologists ACOG Committee opinion no. 548: weight gain during pregnancy. Obstet Gynecol. 2013;121:210–212. doi: 10.1097/01.aog.0000425668.87506.4c. [DOI] [PubMed] [Google Scholar]
- 12.Adegboye A, Linne YM, Lourenco PM. Diet or exercise, or both, for weight reduction in women after birth. Cochrane Database Syst Rev. 2013;23:CD005637. doi: 10.1002/14651858.CD005627.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Power ML, Cogswell ME, Schulkin J. Obesity prevention and treatment practices of U.S. obstetrician-gynecologists. Obstet Gynecol. 2006;108:961–968. doi: 10.1097/01.AOG.0000233171.20484.db. [DOI] [PubMed] [Google Scholar]
- 14.Power ML, Cogswell ME, Schulkin J. US obstetrician-gynaecologist's prevention and management of obesity in pregnancy. J Obstet Gynaecol. 2009;29:373–377. doi: 10.1080/01443610902946911. [DOI] [PubMed] [Google Scholar]
- 15.Cogswell ME, Power ML, Sharma AJ, Schulkin J. Prevention and management of obesity in nonpregnant women and adolescents: beliefs and practices of U.S. obstetricians and gynecologists. J Womens Health (Larchmt) 2010;19:1625–1634. doi: 10.1089/jwh.2009.1838. [DOI] [PubMed] [Google Scholar]
- 16.Livaudais JC, Kaplan CP, Haas JS, Pérez-Stable EJ, Stewart S, et al. Lifestyle behavior counseling for women patients among a sample of California physicians. J Womens Health (Larchmt) 2005;14:485–495. doi: 10.1089/jwh.2005.14.485. [DOI] [PubMed] [Google Scholar]
- 17.Frank E, Segura C, Shen H, Oberg E. Predictors of Canadian physicians’ prevention counseling practices. Can J Public Health. 2010;101:390–395. doi: 10.1007/BF03404859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neville CE, McKinley MC1, Holmes VA1, Spence D2, Woodside JV1. The relationship between breastfeeding and postpartum weight change-a systematic review and critical evaluation. Int J Obes (Lond) 2014;38:577–590. doi: 10.1038/ijo.2013.132. [DOI] [PubMed] [Google Scholar]
- 19.Wilkinson SA, Poad D, Stapleton H. Maternal overweight and obesity: a survey of clinicians’ characteristics and attitudes, and their responses to their pregnant clients. BMC Pregnancy Childbirth. 2013;13:117. doi: 10.1186/1471-2393-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldstein IM, Foltz JL, Onufrak S3, Belay B3. Health-promoting environments in U.S. medical facilities: physician perceptions, DocStyles 2012. Prev Med. 2014;67:65–70. doi: 10.1016/j.ypmed.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 21.Fang J, Cogswell ME, Keenan NL, Merritt RK. Primary health care providers’ attitudes and counseling behaviors related to dietary sodium reduction. Arch Intern Med. 2012;172:76–78. doi: 10.1001/archinternmed.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiang N, Wethington H, Onufrak S, Belay B. Characteristics of US Health Care Providers Who Counsel Adolescents on Sports and Energy Drink Consumption. Int J Pediatr. 2014;2014:987082. doi: 10.1155/2014/987082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siega-Riz AM, Deierlein A, Stuebe A. Implementation of the new institute of medicine gestational weight gain guidelines. J Midwifery Womens Health. 2010;55:512–519. doi: 10.1016/j.jmwh.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Zera C1, McGirr S, Oken E. Screening for obesity in reproductive-aged women. Prev Chronic Dis. 2011;8:A125. [PMC free article] [PubMed] [Google Scholar]
- 25.ACOG District IX/CA: Postpartum visit algorithm: overweight/obesity. Interconception Care Project for California [Google Scholar]
- 26.Shaw KA, Caughey AB, Edelman AB. Obesity epidemic: how to make a difference in a busy OB/GYN practice. Obstet Gynecol Surv. 2012;67:365–373. doi: 10.1097/OGX.0b013e318259ee6a. [DOI] [PubMed] [Google Scholar]
- 27.Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202:135. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: pediatricians’ self-efficacy, barriers, resources, and advocacy. Ambul Pediatr. 2005;5:150–156. doi: 10.1367/A04-104R.1. [DOI] [PubMed] [Google Scholar]
- 29.Polacsek M, Orr J, Letourneau L, Rogers V, Holmberg R, et al. Impact of a primary care intervention on physician practice and patient and family behavior: keep ME Healthy---the Maine Youth Overweight Collaborative. Pediatrics. 2009;123:S258–S266. doi: 10.1542/peds.2008-2780C. [DOI] [PubMed] [Google Scholar]
- 30.Kinnunen TI1, Raitanen J, Aittasalo M, Luoto R. Preventing excessive gestational weight gain--a secondary analysis of a cluster-randomised controlled trial. Eur J Clin Nutr. 2012;66:1344–1350. doi: 10.1038/ejcn.2012.146. [DOI] [PubMed] [Google Scholar]
- 31.Phelan S, Phipps MG, Abrams B, Darroch F, Grantham K, et al. Does behavioral intervention in pregnancy reduce postpartum weight retention? Twelve-month outcomes of the Fit for Delivery randomized trial. Am J Clin Nutr. 2014;99:302–311. doi: 10.3945/ajcn.113.070151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frank E, Wright EH, Serdula MK, Elon LK, Baldwin G. Personal and professional nutrition-related practices of US female physicians. Am J Clin Nutr. 2002;75:326–332. doi: 10.1093/ajcn/75.2.326. [DOI] [PubMed] [Google Scholar]
- 33.Frank E, Bhat Schelbert K, Elon L. Exercise counseling and personal exercise habits of US women physicians. J Am Med Womens Assoc. 2003;58:178–184. [PubMed] [Google Scholar]