Abstract
Background
Distal radius fractures are common, costly, and increasing in incidence. Percutaneous K-wire fixation and volar locking plates are two of the most commonly used surgical treatments for unstable dorsally displaced distal radius fractures. However, there is uncertainty regarding which of these treatments is superior.
Questions/purposes
We performed a meta-analysis of randomized controlled trials to determine whether patients treated with volar locking plates (1) achieved better function (2) attained better wrist motion, (3) had better radiographic outcomes, and (4) had fewer complications develop than did patients treated with K-wires for dorsally displaced distal radius fractures.
Methods
We performed a comprehensive search of MEDLINE (inception to 2014, October Week 2), EMBASE (inception to 2014, Week 42), and the Cochrane Central Register of Controlled Trials to identify relevant randomized controlled trials; we supplemented these searches with manual searches. We included studies of extraarticular and intraarticular distal radius fractures. Adjunctive external fixation was acceptable as long as the intent was to use only K-wires where possible and external fixation was used in less than 25% of the procedures. We considered a difference in the DASH scores of 10 as the minimal clinically important difference. We performed quality assessment with the Cochrane Risk of Bias tool and evaluated the strength of recommendations using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach. Seven randomized trials with a total of 875 participants were included in the meta-analysis.
Results
Patients treated with volar locking plates had slightly better function than did patients treated with K-wires as measured by their DASH scores at 3 months (mean difference [MD], 7.5; 95% CI, 4.4–10.6; p < 0.001) and 12 months (MD, 3.8; 95% CI, 1.2–6.3; p = 0.004). Neither of these differences exceeded the a priori-determined threshold for clinical importance (10 points). There was a small early advantage in flexion and supination in the volar locking plate group (3.7° [95% CI, 0.3°–7.1°; p = 0.04] and 4.1° [95% CI, 0.6°–7.6°; p = 0.02] greater, respectively) at 3 months, but not at later followups (6 or 12 months). There were no differences in radiographic outcomes (volar tilt, radial inclination, and radial height) between the two interventions. Superficial wound infection was more common in patients treated with K-wires (8.2% versus 3.2%; RR = 2.6; p = 0.001), but otherwise no difference in complication rates was found.
Conclusions
Despite the small number of studies and the limitations inherent in a meta-analysis, we found that volar locking plates show better DASH scores at 3- and 12-month followups compared with K-wires for displaced distal radius fractures in adults; however, these differences were small and unlikely to be clinically important. Further research is required to better delineate if there are specific radiographic, injury, or patient characteristics that may benefit from volar locking plates in the short term and whether there are any differences in long-term outcomes and complications.
Level of Evidence
Level I, therapeutic study.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-015-4347-1) contains supplementary material, which is available to authorized users.
Introduction
Distal radius fractures are common injuries with more than 600,000 occurring annually in the North American population [4]. The distributive pattern of these injuries is bimodal, affecting young (predominantly male) adults through high-energy mechanisms and elderly (predominantly female) adults through low-energy falls and osteoporosis [32]. Economic costs of distal radius fractures also are substantial—direct costs of care are more than USD 480 million in the United States annually; more than USD 170 million of these costs are borne by publically funded Medicare [39, 43]. As the population continues to age, the burden of distal radius fractures and the costs of care are expected to increase [33]. Unfortunately, the treatments for these injuries is controversial [22]. Therefore, determining effective evidence-based treatment of distal radius fractures is crucial.
There are multiple treatment options for patients with distal radius fractures, including closed reduction and cast immobilization, percutaneous K-wire fixation, fixation with volar or dorsal plates (locking or nonlocking), bridge plating, use of an external fixator, or a combination of these techniques. Although the best choice depends to some extent on the characteristics of the fracture (open/closed, nondisplaced/displaced, extra-/intraarticular), there is little high-quality evidence to inform this decision-making. For instance, clinical practice guidelines for distal radius fracture published by the American Academy of Orthopaedic Surgeons (AAOS) made 29 recommendations; however, none of these recommendations was given a “strong” rating owing to limited strength of the evidence [25].
Most randomized trials and all meta-analyses conducted to date have focused on comparisons between external fixators and internal plate fixation [17, 26, 45]. However, it is becoming less common for the majority of distal radius fractures to be treated with an external fixator because these devices can be bulky and inconvenient for patients and typically are reserved for more severe fracture types [32]. According to US Medicare data, internal fixation is the most common surgical intervention for distal radius fracture in the United States, followed closely by percutaneous pinning with K-wires [3]. To our knowledge, there have been no meta-analyses comparing these two common interventions despite multiple trials on the topic having been published [5, 12, 18, 21, 29, 30, 37].
The objective of this study therefore was to perform a systematic review and meta-analysis of randomized trials comparing K-wire fixation with volar locking plates for displaced distal radius fractures. The specific goals of this meta-analysis were to determine whether patients treated with volar locking plates (1) achieved better function, (2) attained better wrist motion, (3) had better radiographic outcomes, and (4) had fewer complications than did patients treated with K-wires for dorsally displaced distal radius fractures.
Materials and Methods
Search Strategy and Eligibility
Our systematic review was conducted and reported in accordance with PRISMA guidelines [31].
We performed a comprehensive search of three electronic medical databases: MEDLINE (inception to 2014, October Week 2), EMBASE (inception to 2014, Week 42), and the Cochrane Central Register of Controlled Trials (inception to Issue 9 of 12, September 2014) to identify relevant trials (Appendix 1. Supplemental material is available with the online version of CORR®). We also supplemented our search with manual review of recent conference abstracts (Orthopaedic Trauma Association 2012–2014 and AAOS annual meetings 2012–2014) and reference lists. Reference Manager Software Version 12 (Thomson Reuters, Philadelphia, PA, USA) was used to manage the search. Our inclusion criteria were randomized controlled trials that compared volar locking plates with K-wires for distal radius fractures. We did not distinguish between the type of K-wire technique used (such as Kapandji, interfragmentary, mixed, or other). We defined a volar locking plate as any plate applied to the volar aspect of the radius with screws that locked into a plate forming a fixed-angle construct, with or without adjunctive use of nonlocking screws. We included studies of extraarticular and intraarticular distal radius fractures. We attempted to collect outcome data for only K-wires used alone; however, if not reported independently, we accepted adjunctive external fixation as long as the intent was to use only K-wires where possible and external fixation was used in less than 25% of the total cases.
Study Selection and Data Extraction
Two reviewers (HC and YVK) screened all titles and abstracts for eligibility and conducted full-text reviews in duplicate. Discrepancies were resolved by consensus after discussion between the two reviewers. Data were collected using standardized data collection forms. We collected information pertaining to study characteristics, including publication year, study design, duration, location, number of centers, number of participants, mean age of participants, types of fractures included (AO type), and outcomes reported.
Data collection included functional outcome measures—specifically the Disabilities of the Arm, Shoulder, and Hand (DASH) and Patient Rated Wrist Evaluation (PRWE) questionnaires, which are the best available patient-reported outcome measurement instruments for distal radius fractures and have been recommended for functional outcome measurement [13]. We also collected reported data on grip strength, wrist ROM (flexion, extension, supination, pronation, ulnar deviation, radial deviation), complications, and radiographic outcomes. In cases in which wrist ROM was reported only as a percentage of the contralateral (normal) wrist, we converted percentages to a degree measurement based on normal physiologic ROM (normal values used: 85° flexion, 80° extension, 85° supination, 80° pronation, 35° ulnar deviation, and 20° radial deviation) [7, 28]. Means and standard deviations (SDs) were collected when reported; medians were used in place of means when the latter was not reported because these provide an acceptable alternate measurement for centrality [35]. Where data were reported only in graph format, GraphClick software [14] was used to extract the relevant values.
Quality Assessment
We assessed quality of each included study in duplicate using the Cochrane Risk of Bias tool [16] and reported this in chart format. In particular, this tool captures information on adequacy of randomization, allocation concealment, blinding, completeness of data collection, selective reporting, and other biases. Strength of recommendation for the functional outcome comparison was determined and reported using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach [15].
Statistical Analysis
Statistical analysis was performed using SPSS Software Version 21 (IBM Corp, Armonk, NY, USA) and Review Manager (RevMan) Version 5.3 software [36]. Mean differences were pooled for common outcomes scores reported across studies or standardized mean differences (SMDs) for outcome scores that differed across studies. We calculated heterogeneity between studies using the chi-square test and the I2 statistic. We considered either a chi-square value of p less than 0.1 or I2 statistic greater than 35% to represent significant heterogeneity. Outcomes with significant heterogeneity were pooled using a random-effects model; outcomes with low heterogeneity were pooled using a fixed-effects model.
Standard deviations were calculated for medians from ranges using described methods [19]. Where SDs or CIs were not reported, we imputed SDs using a trial-and-error process to reproduce reported p values. Differences in complication rates were compared using the chi-square statistical test. We considered a difference in DASH or quickDASH scores of 10 as the minimal clinically important difference (MCID) based on previously published studies and taking into consideration that reported values have not been evaluated specifically in patients with distal radius fractures [10, 38]. Given that normative data for these scoring instruments are sufficiently similar, and both are reported on a scale of 100, we pooled mean differences of these scores across all trials. We also performed a secondary analysis using SMDs, using 0.5 SDs as the MCID, as has been described as an appropriate threshold [34], to further corroborate our results. A p value less than 0.05 was used to infer statistical significance.
Literature Search
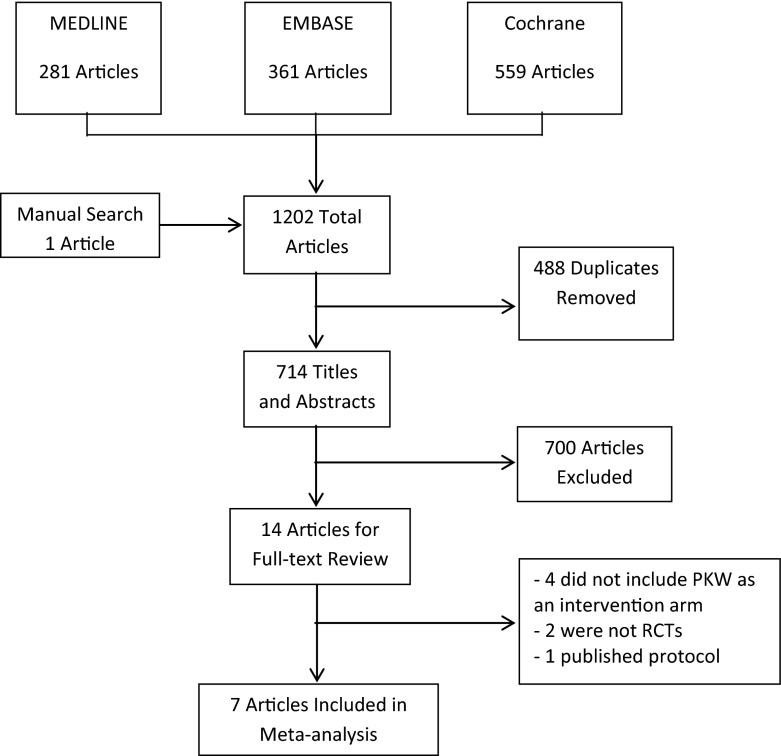
The search yielded 1202 citations (281 MEDLINE, 361 EMBASE, 559 Cochrane Library, one from other sources), of which we excluded 488 duplicates, leaving 714 for title and abstract screening. Fourteen articles met criteria for full-text review, and seven of these met inclusion criteria for our meta-analysis (Fig. 1).
Fig. 1.
The flowchart shows the search and screening process for article inclusion. PKW = percutaneous K-wire fixation; RCTs = randomized controlled trials.
Publication Bias
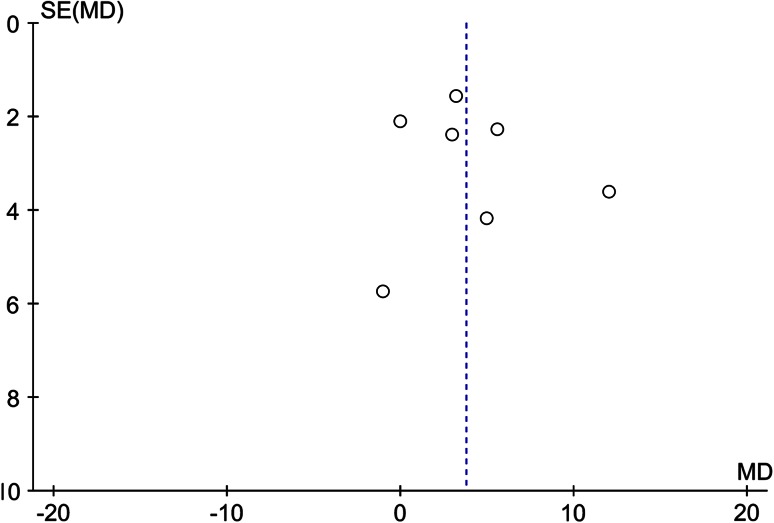
To assess publication (or positive-outcome bias), we constructed a funnel plot. Although the number of studies was small, we did not appreciate any asymmetry which would suggest publication bias (Fig. 2). A small group of positive industry-funded studies also can suggest publication bias [24]. If this were the case, we would expect results to positively favor the volar locking plate, as this represents a newer technology. We therefore assessed funding sources for each study. None of the studies were funded by industry, which further reinforced the lack of a publication bias.
Fig. 2.
There is no excessive asymmetry to suggest publication bias in the funnel plot. SE = standard error; MD = mean difference.
Study Characteristics
All seven studies included in this systematic review were parallel-group randomized controlled trials (Table 1). Six of these trials were conducted in Europe and one in North America. There was only one multicenter study, which was conducted in the United Kingdom and included 18 centers. Five studies reported final followup at 12 months and two reported final followup at 6 months. Six studies also reported intermediary followup data at 3 months or earlier. All trials reported less than 20% loss to followup, and in six of seven trials there was less than 10% loss to followup.
Table 1.
Study characteristics
| Study | Method | Location | Surgeon experience | Participants | Mean age (years; SD) | Fracture types in PKW group (AO classification) | Fracture types in VLP group (AO classification) | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Rozental et al. 2009 [37] | Parallel group, randomized controlled trial | USA | Fellowship-trained hand and upper extremity surgeons | 45 total; 22 PKW, 21 VLP 2/22 (9%) required external fixation in PP group |
PKW: 51 (NR), range, 19–77 VLP: 52 (NR), range, 24–79 |
A2: 4 A3: 2 C1: 6 C2: 9 |
A2: 2 A3: 8 C1: 2 C2: 11 |
DASH (3 weeks, 6 weeks, 12 weeks, 1 year) Wrist ROM Digit motion Grip strength Pinch strength Patient satisfaction Return to work Radiographic outcomes Complications |
| Marcheix et al. 2010 [29] | Parallel group, randomized controlled trial | France | NR | 103 total; 53 PKW, 50 VLP No external fixation |
PKW: 73 (11) VLP: 75 (11) |
A2: 1 A3: 22 C2: 23 C3: 6 |
A2: 0 A3: 17 C2: 25 C3: 8 |
DASH (12 weeks, 26 weeks) Herzberg score Wrist ROM Radiographic outcomes Complications |
| Hollevoet et al. 2011 [18] | Parallel group, randomized controlled trial | Belgium | University hospital surgeon (either consultants or trainees supervised by consultants) | 40 total; 20 PKW, 20 VLP No external fixation |
PKW: 66 (NR) VLP: 67 (NR) |
Frequencies by AO type NR 7 extraarticular, 13 intraarticular |
Frequencies by AO type NR 11 extraarticular, 9 intraarticular |
DASH (3 months, 1 year) Wrist ROM Grip strength Radiographic outcomes Complications |
| McFadyen et al. 2011 [30] | Parallel group, randomized controlled trial | United Kingdom | Senior orthopaedic consultant for most cases (74% VLP; 62% PKW). Trainees or associate specialists for other cases | 56 total; 29 PKW, 27 VLP No external fixation |
PKW: 65 (NR), range, 18–80 VLP: 61 (NR), range, 26–80 |
Only Type A fractures, frequencies NR | Only Type A fractures, frequencies NR | QuickDASH (3 months, 6 months) Gartland and Werley score Wrist ROM Grip strength Radiographic outcomes Complications |
| Karantana et al. 2013 [21] | Parallel group, randomized controlled trial | United Kingdom | Senior orthopaedic consultant surgeons from tertiary center | 130 total; 64 PKW, 66 VLP 11/64 (17%) required external fixation in PP group |
PKW: 51 (16) VLP: 48 (15) |
A3: 28 C2: 30 C3: 6 |
A3: 27 C2: 37 C3: 2 |
QuickDASH (6 weeks, 12 weeks, 1 year) PEM EQ-5DTM Wrist ROM Grip strength Radiographic outcomes Complications |
| Goehre et al. 2014 [12] | Parallel group, randomized controlled trial | United Kingdom | Experienced senior orthopaedic surgeons | 40 total; 19 PKW; 21 VLP No external fixation |
PKW: 73.8 (8.9) VLP: 71.3 (5.7) |
A2: 6 A3: 9 C1: 4 |
A2: 4 A3: 14 C1: 3 |
DASH (3 months, 6 months, 12 months) PRWE Castaing score Wrist ROM Grip strength Radiographic outcomes Complications |
| Costa et al. 2014 [5] | Parallel group, randomized controlled trial | United Kingdom | Multiple surgeons from multiple different centers (68% had performed > 20 prior VLPs; 74% had performed > 20 prior PKWs) | 461 total; 230 PKW; 231 VLP No external fixation |
PKW: 59.7 (16.4) VLP: 58.3 (14.9) |
A2: 73 A3: 84 B1: 1 B2: 1 B3: 1 C1: 33 C2: 26 C3: 7 |
A2: 73 A3: 78 B1: 4 B2: 1 B3: 0 C1: 30 C2: 34 C3: 11 |
DASH (12 months) PRWE EQ-5DTM Complications |
PKW = percutaneous K-wires; VLP = volar locking plate; PP = percutaneous pins; NR = not reported; PEM = Patient Evaluation Measure; PRWE = Patient Rated Wrist Evaluation.
All trials included only dorsally displaced distal radius fractures. Six trials included patients with extraarticular and intraarticular distal radius fractures; one trial included patients with only extraarticular fractures. Two trials included patients who received supplemental external fixation because of residual instability after K-wire fixation (9% of patients receiving K-wire fixation in one trial, 17% of patients in the second trial; this represented less than 3% of all patients analyzed in the K-wire group). All studies except one excluded patients with polytrauma or multiple injuries. Costa et al. [5] did not explicitly exclude these high-energy injuries; however, “fall” was reported as the mechanism of injury in 98% (451 of 461) of distal radius fractures included in their study.
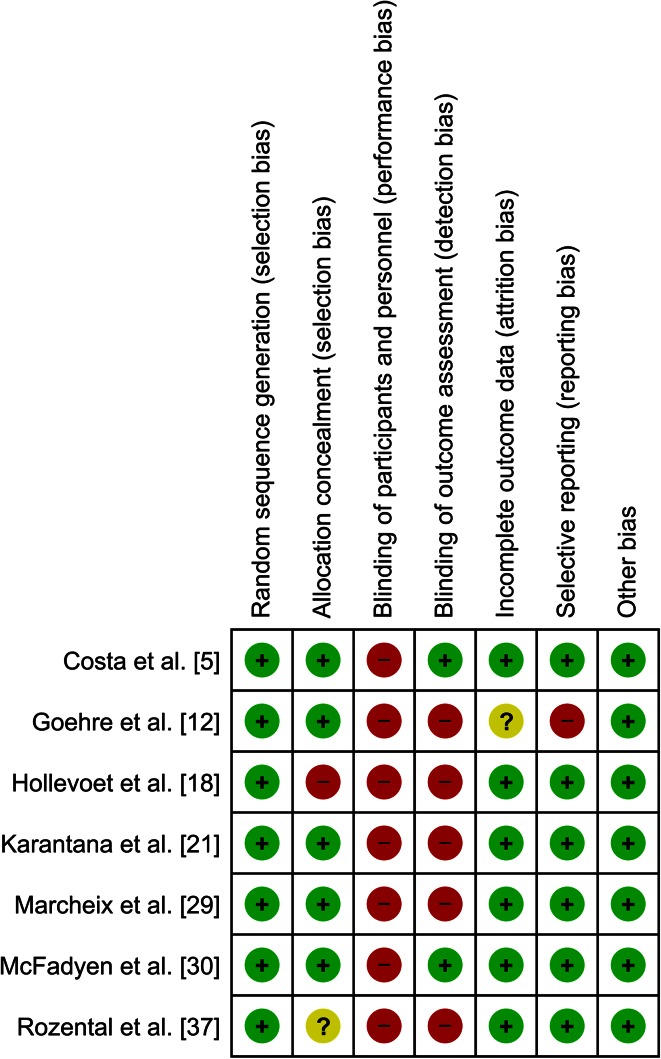
Risk of Bias
None of the trials reported any attempt to blind surgeons or patients. Outcome assessors were blinded in two trials. One study had a risk of selective reporting bias. The majority of trials were at low risk of bias in terms of random sequence generation, allocation concealment, completeness of followup, selective reporting, or other biases (Fig. 3).
Fig. 3.
The risk of bias for each trial included in the meta-analysis using the Cochrane Risk of Bias tool is shown.
Results
Functional Outcomes
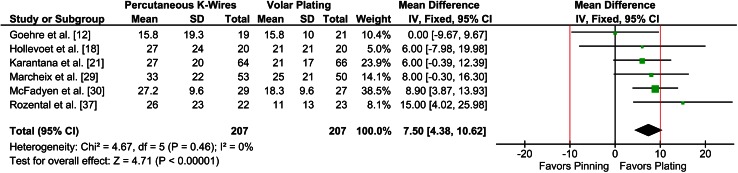
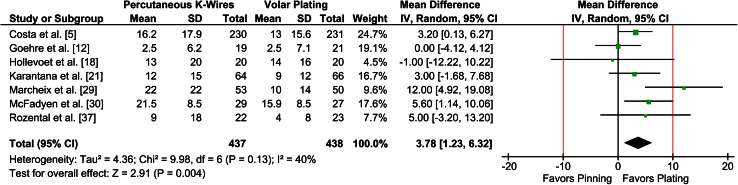
Patients treated with volar locking plates had slightly better DASH scores than did patients treated with K-wires at 3 months and at final followup. At 3-month followup, the mean DASH score was 7.5 points lower (ie, better) in the volar locking plate group (six trials, 414 participants; 95% CI, 4.4–10.6; p < 0.001) (Fig. 4). The upper threshold of the 95% CI crossed the MCID of 10, and therefore we were unable to rule out a clinically important difference at 3 months. At final followup (6 or 12 months), the mean DASH score was only 3.8 points lower in the volar locking plate group (seven trials, 875 participants; 95% CI, 1.2–6.3; p = 0.004) (Fig. 5). The upper threshold of the 95% CI was less than 10, suggesting that this was unlikely to be a clinically important difference at final followup. These conclusions were consistent when SMDs were used for analysis (3-month SMD, 0.42; 95% CI, 0.22–0.61; p < 0.001); 6- or 12-month SMD, 0.29; 95% CI, 0.11–0.46; p = 0.001). Removal of the two trials from the analysis that did not follow patients to 1 year (ie, 6-month followup only) did not substantially change the results (mean difference [MD], 2.3; 95% CI, 0.3–4.4; p = .03). Based on GRADE, there was low confidence in the 3-month estimate of effect and moderate confidence in the 6- to 12-month estimate of effect (Table 2). There were a total of 875 participants for which these data were available. There were no differences found between K-wires and volar locking plates in terms of the PRWE score at either 3 months or final followup (6 months or 1 year) in either of the two trials that reported on this endpoint [5, 12].
Fig. 4.
The individual and pooled 3-month mean differences in DASH scores and 95% CIs are shown in the forest plot. The minimum clinically important difference is indicated by the red lines. IV = inverse variance.
Fig. 5.
The individual and pooled 6- and 12-month mean differences in DASH scores, along with 95% CIs, are shown in the forest plot. The minimum clinically important difference is indicated by the red lines. IV = inverse variance.
Table 2.
GRADE summary of findings
| Volar locking plate compared with percutaneous K- wires for displaced distal radius fracture Bibliography (systematic reviews) | ||||
|---|---|---|---|---|
| Outcomes | Number of participants (studies) followup |
Quality of the evidence (GRADE) | Anticipated absolute effects | |
| Risk with percutaneous K-wires | Risk difference with volar locking plate | |||
| Function at 3 months assessed with DASH followup: 3 months | 414 (6 RCTs) 3 months |
⊕⊕◯◯ Low1,2 |
The mean function at 3 months in the control group was 27.4 | MD 7.5 lower (4.4 lower to 10.6 lower) |
| Function at 6–12 months (final function) assessed with DASH followup: range, 6–12 months | 875 (7 RCTs) 6–12 months |
⊕⊕⊕◯ Moderate1 |
The mean function at 6–12 months in the control group was 15.5 | MD 3.8 lower (1.2 lower to 6.3 lower) |
1Lack of blinding of outcome assessors in most trials; 2 high imprecision in pooled estimate; the risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI); RCTs = randomized controlled trials; MD = mean difference. GRADE Working Group grades of evidence: High quality = We are very confident that the true effect lies close to that of the estimate of the effect; Moderate quality = We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; Low quality = confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect; Very low quality = We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.
Wrist ROM
Flexion and supination were slightly greater in the volar locking plate group at 3 months (four trials, 3.7° [95% CI, 0.3°–7.1°, p = 0.04] and 4.1° [95% CI, 0.6°–7.6°, p = 0.02] greater, respectively), but not at final followup. There were no differences in wrist extension, pronation, radial deviation, or ulnar deviation at 3 months or final followup. Wrist ROM was reported as an outcome in five trials [12, 18, 21, 29, 37], four of which reported sufficient information to enable pooling. Radial deviation and ulnar deviation were reported in only two of these trials [12, 37].
Radiographic Outcomes
There were no differences in radiographic outcomes at the latest reported followup between the two interventions. Among trials that reported sufficient information for meta-analysis, there were no differences in volar tilt (four trials, 0.1° greater in K-wire group; 95% CI, −4.6° to 4.9°; p = 0.96), radial inclination (four trials, 0.4° greater in K-wire group; 95% CI, −0.9° to 1.7°; p = 0.58), or radial height (three trials, 0.4 mm greater in K-wire group; 95% CI, −0.3 mm to 1.0 mm; p = 0.31) at final followup. Of the two trials that could not be included in meta-analysis, one reported better volar tilt, radial height, and radial inclination with the volar locking plate but did not report absolute values [30]; the other trial reported a greater median volar tilt in the K-wire group (4° vs 0° in volar locking plate group) but did not provide any data to estimate variance (eg, SD, interquartile range) or statistically analyze the data. Only one study reported articular step-off postoperatively [21], and it detected no difference between the two interventions. Radiographic outcomes were reported in six of the seven trials.
Complications
There were more total complications in the K-wire group than in the volar locking plate group. This difference was driven predominantly by a difference in superficial wound infections (8.2% versus 3.2%; RR = 2.6; p = 0.001), all of which were treated successfully with oral antibiotics. There were no differences in the risks of any of the other reported complications (deep infection, neurologic injury, tendon rupture, or reoperations) between the two groups (Table 3). In total, there were 102 complications reported in the K-wire group and 66 reported in the volar locking plate group. All trials reported complications.
Table 3.
Common complications
| Complication | Percutaneous K-wires | Volar locking plate | p value |
|---|---|---|---|
| Superficial infection | 36 | 14 | 0.001 |
| Deep infection | 2 | 2 | 1.00 |
| Neurologic injury* (carpal tunnel) | 33 (22) | 32 (28) | 0.89 (0.39) |
| Tendon rupture† | 6 | 6 | 1.00 |
| Reoperations | 14 | 17 | 0.59 |
* Includes transient nerve palsies; †does not include tendinitis.
Discussion
Distal radius fractures are common and costly injuries [4, 32, 39]. With unstable dorsally displaced fractures requiring surgical intervention, the optimal surgical treatment option remains equivocal. Clinical practice guidelines have bemoaned the lack of high-quality evidence to inform orthopaedic practice in this area [22, 25]. Despite this lack of evidence, there has been a large shift in the treatment of dorsally displaced distal radius fractures toward the use of the volar locking plates, especially among younger orthopaedic surgeons [20, 23]. To our knowledge, there have been no published meta-analyses to date comparing volar locking plates with K-wires for dorsally displaced distal radius fractures. In our meta-analysis of 875 patients, we found lower (ie, better) DASH scores with use of volar locking plates at 3 months and 12 months. Although we cannot exclude the possibility of a small clinically important difference at 3 months, the magnitude of improvement by 12 months is most likely imperceptible to patients.
An important limitation of our review is that followup of all included trials was limited to a maximum of 1 year and in some trials just 6 months. This followup interval is not long enough for development of posttraumatic arthritis, one of the long-term complications of a malreduced articular surface. One of the potential advantages of volar plating is that the fracture can be reduced under direct observation leading to more accurate articular reduction in AO Types B and C fractures. Studies with longer-term followup will be necessary to determine whether there is a difference in clinical symptoms of posttraumatic arthritis between these two treatment modalities. Included trials, in general, had low risk of bias—with the exception of blinding, which is difficult given the nature of the interventions. However, given that both interventions were surgical, the presence of a “placebo bias” is less likely. The inclusion of patients with adjunctive external fixation in the K-wire group is a potential limitation. However, only two trials included patients with external fixation and a small proportion required this adjunct (< 3% of all patients treated with K-wires). If K-wires alone would have led to a poorer outcome in these patients treated with adjunctive external fixation, then this meta-analysis potentially may be underestimating the benefit of the volar locking plate in some situations. However, given the small number of patients, the degree of this underestimate is expected to be minimal. Differences resulting from adjunctive treatments that were not reported consistently across trials (eg, use of bone graft) is another limitation to this meta-analysis.
Another important limitation relates to the external validity—or generalizability—of the findings of this review. The results of this meta-analysis are most applicable to the low-to-moderate energy dorsally displaced distal radius fracture (with or without an intraarticular component), which is reducible under fluoroscopy and allows for good purchase of bone with K-wires. Extreme cases of either high-energy trauma (eg, motor vehicle accidents) or very low-energy trauma in patients with osteoporosis are either underrepresented or excluded entirely in the trials constituting our meta-analysis. Therefore we cannot make any definitive conclusions regarding these subgroups.
We found that use of volar locking plates for displaced distal radius fractures showed a small improvement in DASH scores at 3 months (MD, 7.5; 95% CI, 4.4–10.6; p < 0.001) and 12 months (MD, 3.8; 95% CI, 1.2–6.3; p = 0.004) compared with K-wires. Uncertainty in the estimate precludes the conclusion that there is no clinical advantage at 3 months postoperatively; however, by 1 year the magnitude of this difference was less than our a priori-established MCID on the DASH scale of 10 points [10, 38]. This represents the best (ie, lowest risk of bias) estimate of functional differences in the literature to date, as we were able to pool the results of seven recent and good quality RCTs to achieve a large sample size. Our endeavor was facilitated by the use of a common and recommended functional outcome instrument across all RCTs, the DASH questionnaire. Inconsistent and varying use of outcome instruments has presented limitations to previous meta-analyses in the orthopaedic and distal radius literature [2, 17]. Future trials must continue to use common outcome instruments to allow for meaningful meta-analysis.
Our analysis also found small early advantages in flexion and supination in the volar locking plate group (3.7° and 4.1° greater, respectively) at 3-month followup, but these differences disappeared at final followup. Not all trials standardized postoperative protocols for both groups (eg, patients treated with volar locking plates were allowed to mobilize at 1 week in three trials versus 6 weeks for patients with K-wires), which may have contributed to the finding that volar locking plates lead to improved DASH scores, flexion, and supination at 3 months. However, patients treated with volar locking plates typically are permitted earlier mobilization [42], and it would be reasonable to expect this to contribute to some the early advantage in ROM. Furthermore, the three trials that standardized postoperative protocols showed possible early improvements as well; therefore, the early improvements seen with volar locking plates may not be entirely attributable to reduced immobilization times as has been suggested [27].
There were no differences in radiographic alignment (volar tilt, radial inclination, and radial height, or articular incongruity) between the two interventions. The relationship between radiographic outcomes—including articular incongruity—and clinical outcomes is controversial [11]. In terms of short-term outcomes, small amounts of radial shortening (as little as 3 mm) have been shown to negatively affect function [1, 41]. However, the distal radius appears to be relatively tolerant to changes in volar tilt, with no apparent functional deficits with even a small amount of dorsal angulation [44]. In terms of long-term outcomes, an articular step-off of 2 mm has been shown to result in radiographic signs of arthritis. However, this has not consistently translated into poorer clinical outcomes [6, 11]. Therefore, small differences in radiographic outcomes are likely not clinically important.
Superficial infections were more frequent in patients treated with K-wires, but otherwise no differences in complication rates were found between the two treatments. It has been argued that in the absence of convincing evidence of superiority of volar locking plates, economic considerations should drive clinical decision-making and policy in the treatment of dorsally displaced distal radius fractures [8, 9, 40]. However, a robust economic analysis will need to consider differences in costs associated with complications (eg, antibiotic treatment for superficial infections) in addition to differences in costs of the implants, length of surgery, requirement for adjunctive treatments (eg, external fixation, casting), and postoperative protocols (eg, clinic visits, radiographs) [8].
We found that volar locking plates result in lower (ie, better) DASH scores compared with K-wires for dorsally displaced distal radius fractures in adults. However, these differences were small and likely to have been imperceptible to the patient, since they were smaller than the predefined MCID. Further research is required to better delineate if there are specific radiographic, injury, or patient characteristics that may benefit from volar locking plates in the short term. Further, the incidence of posttraumatic arthritis would not have been detected at the short-term followups in the studies included in this meta-analysis. Therefore, future research must evaluate if there are any differences in outcomes and complications between these two interventions in the long term.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at McMaster University, Hamilton, Ontario, Canada.
References
- 1.Aro HT, Koivunen T. Minor axial shortening of the radius affects outcome of Colles’ fracture treatment. J Hand Surg Am. 1991;16:392–398. doi: 10.1016/0363-5023(91)90003-T. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry H, Simunovic N, Petrisor B. Cochrane in CORR®: surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults (review) Clin Orthop Relat Res. 2015;473:17–22. doi: 10.1007/s11999-014-4018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung KC, Shauver MJ, Yin Y, Kim M, Baser O, Birkmeyer JD. Variations in the use of internal fixation for distal radius fracture in the United States Medicare population. J Bone Joint Surg Am. 2011;93:2154–2162. doi: 10.2106/JBJS.J.012802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 5.Costa ML, Achten J, Parsons NR, Rangan A, Griffin D, Tubeuf S, Lamb SE, DRAFFT Study Group Percutaneous fixation with Kirschner wires versus volar locking plate fixation in adults with dorsally displaced fracture of distal radius: randomised controlled trial. BMJ. 2014;349:g4807. doi: 10.1136/bmj.g4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diaz-Garcia RJ, Chung KC. Common myths and evidence in the management of distal radius fractures. Hand Clin. 2012;28:127–133. doi: 10.1016/j.hcl.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dincer F, Samut G. Physical examination of the hand. In: Duruoz MT, ed. Hand Function. A Practical Guide to Assessment. New York, NY: Springer; 2014:23–40.
- 8.Dzaja I, MacDermid JC, Roth J, Grewal R. Functional outcomes and cost estimation for extra-articular and simple intra-articular distal radius fractures treated with open reduction and internal fixation versus closed reduction and percutaneous Kirschner wire fixation. Can J Surg. 2013;56:378–384. doi: 10.1503/cjs.22712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farner S, Malkani A, Lau E, Day J, Ochoa J, Ong K. Outcomes and cost of care for patients with distal radius fractures. Orthopedics. 2014;37:e866–e878. doi: 10.3928/01477447-20140924-52. [DOI] [PubMed] [Google Scholar]
- 10.Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the Disabilities of the Arm, Shoulder and Hand outcome measure (DASH) and its shortened version (QuickDASH) J Orthop Sports Phys Ther. 2014;44:30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 11.Giannoudis PV, Tzioupis C, Papathanassopoulos A, Obakponovwe O, Roberts C. Articular step-off and risk of post-traumatic osteoarthritis: evidence today. Injury. 2010;41:986–995. doi: 10.1016/j.injury.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Goehre G, Otto W, Schwan S, Mendel T, Vergroesen PP, Lindemann-Sperfeld L. Comparison of palmar fixed-angle plate fixation with K-wire fixation of distal radius fractures (AO A2, A3, C1) in elderly patients. J Hand Surg Eur. 2014;39:249–257. doi: 10.1177/1753193413489057. [DOI] [PubMed] [Google Scholar]
- 13.Goldhahn J, Beaton D, Ladd A, Macdermid J, Hoang-Kim A, Distal Radius Working Group of the International Society for Fracture Repair (ISFR) International Osteoporosis Foundation (IOF) Recommendation for measuring clinical outcome in distal radius fractures: a core set of domains for standardized reporting in clinical practice and research. Arch Orthop Trauma Surg. 2014;134:197–205. doi: 10.1007/s00402-013-1767-9. [DOI] [PubMed] [Google Scholar]
- 14.GraphClick. Arizona Software. Available at: http://www.arizona-software.ch/graphclick/. Accessed November 3, 2014.
- 15.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group. Cochrane Statistical Methods Group The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoang-Kim A, Scott J, Micera G, Orsini R, Moroni A. Functional assessment in patients with osteoporotic wrist fractures treated with external fixation: a review of randomized trials. Arch Orthop Trauma Surg. 2009;129:105–111. doi: 10.1007/s00402-008-0661-3. [DOI] [PubMed] [Google Scholar]
- 18.Hollevoet N, Vanhoutie T, Vanhove W, Verdonk R. Percutaneous K-wire fixation versus palmar plating with locking screws for Colles’ fractures. Acta Orthop Belg. 2011;77:180–187. [PubMed] [Google Scholar]
- 19.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hull P, Baraza N, Whalley H, Brewster M, Costa M. Dorsally displaced fractures of the distal radius: a study of preferred treatment options among UK trauma and orthopaedic surgeons. Hand Surg. 2010;15:185–191. doi: 10.1142/S0218810410004801. [DOI] [PubMed] [Google Scholar]
- 21.Karantana A, Downing ND, Forward DP, Hatton M, Taylor AM, Scammell BE, Moran CG, Davis TR. Surgical treatment of distal radial fractures with a volar locking plate versus conventional percutaneous methods: a randomized controlled trial. J Bone Joint Surg Am. 2013;95:1737–1744. doi: 10.2106/JBJS.L.00232. [DOI] [PubMed] [Google Scholar]
- 22.Koval K, Haidukewych GJ, Service B, Zirgibel BJ. Controversies in the management of distal radius fractures. J Am Acad Orthop Surg. 2014;22:566–575. doi: 10.5435/JAAOS-22-09-566. [DOI] [PubMed] [Google Scholar]
- 23.Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius: the evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90:1855–1861. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 24.Lexchin J, Bero LA, Djulbegovic B, Clark O. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ. 2003;326:1167–1170. doi: 10.1136/bmj.326.7400.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lichtman DM, Bindra RR, Boyer MI, Putnam MD, Ring D, Slutsky DJ, Taras JS, Watters WC, 3rd, Goldberg MJ, Keith M, Turkelson CM, Wies JL, Haralson RH, 3rd, Boyer KM, Hitchcock K, Raymond L. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180–189. doi: 10.5435/00124635-201003000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Li-hai Z, Ya-nan W, Zhi M, Li-cheng Z, Hong-da L, Huan Y, Xiao-xie L, Pei-fu T. Volar locking plate versus external fixation for the treatment of unstable distal radial fractures: a meta-analysis of randomized controlled trials. J Surg Res. 2015;193:324–333. J Hand Surg Eur Vol. 2014;39:249–257. [DOI] [PubMed]
- 27.Lozano-Calderon SA, Souer S, Mudgal C, Jupiter JB, Ring D. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008;90:1297–1304. doi: 10.2106/JBJS.G.01368. [DOI] [PubMed] [Google Scholar]
- 28.Magee DJ. Forearm, wrist and hand. Orthopedic Physical Assessment. St Louis, MO: Saunders; 2008:396–470.
- 29.Marcheix PS, Dotzis A, Benko PE, Siegler J, Arnaud JP, Charissoux JL. Extension fractures of the distal radius in patients older than 50: a prospective randomized study comparing fixation using mixed pins or a palmar fixed-angle plate. J Hand Surg Eur. 2010;35:646–651. doi: 10.1177/1753193410364179. [DOI] [PubMed] [Google Scholar]
- 30.McFadyen I, Field J, McCann P, Ward J, Nicol S, Curwen C. Should unstable extra-articular distal radial fractures be treated with fixed-angle volar-locked plates or percutaneous Kirschner wires? A prospective randomised controlled trial. Injury. 2011;42:162–166. doi: 10.1016/j.injury.2010.07.236. [DOI] [PubMed] [Google Scholar]
- 31.Moher D, Liberatri A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nana AD, Joshi A, Lichtman DM. Plating of the distal radius. J Am Acad Orthop Surg. 2005;13:159–171. doi: 10.5435/00124635-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin. 2012;28:113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 35.Pinto RZ, Maher CG, Ferreira ML, Ferreira PH, Hancock M, Oliveira VC, McLachlan AJ, Koes B. Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis. BMJ. 2012;344:e497. doi: 10.1136/bmj.e497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Review Manager (RevMan) Version 5.3. Copenhagen, The Netherlands: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. Available at: http://tech.cochrane.org/revman. Accessed April 30, 2015.
- 37.Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation: a prospective randomized trial. J Bone Joint Surg Am. 2009;91:1837–1846. doi: 10.2106/JBJS.H.01478. [DOI] [PubMed] [Google Scholar]
- 38.Schmitt JS, Di Fabio RP. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol. 2004;57:1008–1018. doi: 10.1016/j.jclinepi.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 39.Shauver MJ, Yin H, Banerjee M, Chung KC. Current and future national costs to medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36:1282–1287. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 40.Shyamalan G, Theokli C, Pearse Y, Tennent D. Volar locking plates versus Kirschner wires for distal radial fractures: a cost analysis study. Injury. 2009;40:1279–1281. doi: 10.1016/j.injury.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 41.Slutsky DJ. Predicting the outcome of distal radius fractures. Hand Clin. 2005;21:289–294. doi: 10.1016/j.hcl.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 42.Smith DW, Brou KE, Henry MH. Early active rehabilitation for operatively stabilized distal radius fractures. J Hand Ther. 2004;17:43–49. doi: 10.1197/j.jht.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 43.US Department of Health & Human Services, Agency for Healthcare Research and Quality. Welcome to H-CUPnet. Available at: http://hcupnet.ahrq.gov/. Accessed November 3, 2014.
- 44.Warwick D, Field J, Prothero D, Gibson A, Bannister GC. Function ten years after Colles’ fracture. Clin Orthop Relat Res. 1993;295:270–274. [PubMed] [Google Scholar]
- 45.Wei DH, Poolman RW, Bhandari M, Wolfe VM, Rosenwasser MP. External fixation versus internal fixation for unstable distal radius fractures: a systematic review and meta-analysis of comparative clinical trials. J Orthop Trauma. 2012;26:386–394. doi: 10.1097/BOT.0b013e318225f63c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.