Abstract
Objectives: Recently, photodynamic therapy (PDT) has been introduced as a new modality in oral bacterial decontamination. Current research aims to evaluate the effect of photodynamic killing of visible blue light in the presence of hydrogen peroxide, curcumin and erythrosine as potential oral photosensitizers on Porphyromonas gingivalis associated with periodontal bone loss and Fusobacterium nucleatum associated with soft tissue inflammation.
Materials and methods: Standard suspension of P. gingivalis and F. nucleatum were exposed to Light Emitting Diode (LED) (440–480 nm) in combination with erythrosine (22 µm), curcumin (60 µM) and hydrogen peroxide (0.3 mM) for 5 min. Bacterial samples from each treatment groups (radiation-only group, photosensitizer-only group and blue light-activated photosensitizer group) were subcultured onto the surface of agar plates. Survival of these bacteria was determined by counting the number of colony forming units (CFU) after incubation.
Results: Results for antibacterial assays on P. gingivalis confirmed that curcumin, Hydrogen peroxide and erythrosine alone exerted a moderate bactericidal effect which enhanced noticeably in conjugation with visible light. The survival rate of P. gingivalis reached zero present when the suspension exposed to blue light-activated curcumin and hydrogen peroxide for 2 min. Besides, curcumin exerted a remarkable antibacterial activity against F. nucleatum in comparison with erythrosine and hydrogen peroxide (P=0.00). Furthermore, the bactericidal effect of visible light alone on P. gingivalis as black-pigmented bacteria was significant.
Conclusion: Our result suggested that visible blue light in the presence of erythrosine, curcumin and hydrogen peroxide would be consider as a potential approach of PDT to kill the main gramnegative periodontal pathogens. From a clinical standpoint, this regimen could be established as an additional minimally invasive antibacterial treatment of plaque induced periodontal pathologies.
Keywords: Erythrosine, Periopathogenic bacteria, Visible blue light, Curcumin, Hydrogen peroxide, Oral antibacterial activity
1. Introduction
Periodontitis is a common disease, with a 5 to 30% prevalence in the adult population. It is an inflammatory process of periodontal tissues caused by bacterial infection which results in the destruction of periodontal connective tissue and resorption of alveolar bone. Porphyromonas gingivalis and Fusobacterium nucleatum strongly believed as major pathogens in the etiology of adult periodontitis 1). However, Antibacterial agents are also widely used, but problems with general efficacy due to access of topical agents to plaque and the possibility of development of bacterial resistance mean alternative strategies are desirable to control plaque and treat gingivitis and periodontal disease 2, 3).
One potential alternative antibacterial approach is Photodynamic Therapy (PDT) 4). Photodynamic inactivation represents a novel tool to combat multi-resistant and wild strain bacteria based on a very gentle procedure. Several studies have illustrated that PDT has a strong effect on a large number of oral gram positive and gram negative bacteria, using different photosensitizers and light sources 5, 6).
Photosensitizers, molecules that are chemically excited by light of specific wavelengths, may cause biological damage or lead to the generation of ROS capable of reacting and affecting biological systems. Although many of these dyes may have inherent antibacterial effects, it is generally only during irradiation that the photodynamic bactericidal effect is elicited 7).
Obviously, more immediate benefit could be attained from photosensitizers already available for use in the mouth. One such photosensitizer is erythrosine. Dental practitioners currently use erythrosine to stain and visualize dental plaque in the form of disclosing solution or tablets. Erythrosine has some reported antimicrobial activity against Gram-positive and Gramnegative oral bacteria 8, 9). However, erythrosine also belongs to a class of cyclic compounds called xanthenes, which absorb light in the visible region, and the ability of erythrosine to initiate photochemical reactions is well documented 10). Moreover, the results reported by Wood et al. pointed out that erythrosinemediated PDT is 5–10 times more effective than methylene blue (MB)-mediated PDT at killing Streptococcus mutans biofilm bacteria 11). Besides, he suggested that the region of maximal absorption by erythrosine is 500–550 nm which is near the wavelength range of visible blue light sources. This is extremely encouraging, as MB is an established and effective tumor 12) and antimicrobial photosensitizer 13, 14). Interestingly, there are few works to assess the potential antimicrobial activity of visible light-activated erythrosine on oral pathogenic bacteria.
Curcumin a polyphenol found in turmeric absorbs blue light when solubilized, was shown to elicit several biological effects such as inhibition of tumorogenesis, anti-inflammatory activity and antibacterial properties 15). Several in vitro and in vivo studies have shown that curcumin alone is non-toxic, but highly antibacterial when light activated 16, 17). The high efficiency of curcumin as a photosensitizer is combined with a very good tolerability for curcumin after ingestion by humans, which has been explained by its low oral bioavailability 18). Araújo et al. have evaluated the effect of photo-activated curcumin on the bacterial content of saliva samples of 13 volunteers and have reported a significant reduction of salivary microorganisms 19). Paschoal et al. used a blue Light Emitting Diode (LED) to photo-activate curcumin placed in contact with plank-tonic cultures of Streptococcus mutans and reported a 70% reduction in bacterial viability after light exposure 20). Several studies investigate the possible bactericidal mechanism of light-activated curcumin and they pointed out that in the presence of light, curcumin can sensitize the formation of free radicals and ROS leading to phototoxic reactions. 21, 22). In addition, the results of a study conducted by Bruzell et al. pointed out that curcumin has a rather broad absorption peak in the range 300 – 500 nm (maximum ∼ 430 – 435 nm, depending on the preparation) and he suggested that the spectral overlap with a commercially available halogen lamp routinely used in dental light-curing is acceptable 23).
Hydrogen peroxide (H2O2) is used worldwide for cleaning wounds, removing dead tissue, or as an oral debriding agent, due to its strong oxidizing properties. Previous studies have indicated that the use of hydrogen peroxide associated with PDT gives increased killing of microorganisms 24). Besides, for all examined microorganisms, PDT in the presence of increasing hydrogen peroxide concentrations gave increased microbial killing in an H2O2 dose-dependent manner. The results of a study conducted by Feuerstein et al. indicated a synergistic antibacterial effect of noncoherent blue light, often used in restorative dentistry, and hydrogen peroxide (H2O2) on S. mutans under planktonic conditions was observed 25). The results of this study also suggested a potential bactericidal mechanism in which the synergistic effect on bacterial vitality is the result of the generation of the highly reactive hydroxyl radical (OH).
Visible light wavelengths, mostly in the presence of a chemical photosensitizer, have been studied as a potential means of affecting bacterial vitality 26–28). Recently, there are several reports on the bactericidal effect of visible light, most of them claiming the blue part (wavelength, 400–500 nm) to be responsible for killing various pathogens. For example, Feuerstein et al. showed that broadband blue light sources such as light emitting diode (LED) used in dentistry for curing resin-composite materials at 400–500nm exert a phototoxic effect on P. gingivalis and F. nucleatum 29). Meanwhile, irradiation of visible blue light is relatively in the maximum absorption range of these three mentioned sensitizers and as a result, it may bring about the maximum bactericidal effect. In addition, the involvement of ROS plays a major role in the phototoxic effect of visible light on bacteria 30). In this turn, this finding supports the hypothesis that the bactericidal effect of visible light that involves photo-oxidative reactions may enhance the potential bactericidal effects of these photosensitizers. Therefore, we hypothesized that the bactericidal activity of these three photosensitizers which we applied in the present study could be promoted maximally by visible blue light in the range of 400–500 nm exerted by hand held photopolymerize LED. This study aimed to carry out a preliminary assessment to examine the visible blue light-activated hydrogen peroxide, curcumin and erythrosine as potential oral photosensitizers on the viability of P. gingivalis associated with periodontal bone loss and F. nucleatum associated with soft tissue inflammation.
2. Materials and Methods
2.1. Bacteria and growth conditions
Fresh lyophilized Porphyromonas gingivalis (33277) and Fusobacterium nucleatum (25586) from the American Type Culture Collection (Rayen Biotechnology Co. Ltd., Tehran, Iran) were used. P. gingivalis and F. nucleatum were rehydrated in brain heart infusion (BHI) broth (Merck KGaA, Darmstadt, Germany) and incubated in an anaerobic jar at <1% O2 and 9–13% CO2 at 37°C. All the strains were subcultured twice before exposure to light. The bacterial concentration after 24 h incubation was standardized by dilution with sterile broth to OD650nm = 0.45, equivalent to ∼ 5×106 colony forming units (CFU).
2.2. Light source
The light source was equipped with a Light Emitting Diode (LED) in the wavelength range 440–480 nm (visible blue light) with an emission maximum at 460 nm (Starlight pro, Mectron, Italy). The device is routinely used in clinical light-curing of dental polymers, and is equipped with a light guide with an area of 0.7 cm2. The irradiation distribution of the light source is not fully homogenous at a few cm distances from the light guide. Therefore, the light guide was held close to the cell dish or plate and also, the distance between the light source tip and the exposed sample was fixed to obtain a constant power density. An average light power of 570 mW/cm2 was measured for LED using a power meter (Puyesh Tajhiz Sanat Pasargad Co., Tehran, Iran) over a spot of 0.7 cm diameter. To calculate power density, the average power was divided by the area of light spot. The light source is designed for irradiation purposes normally lasting less than 2min. For longer irradiation procedures, the device may become heated. Therefore, a maximum of approximately 5 min irradiation time was chosen for our experiments.
2.3. Erythrosine
1% (w/v) erythrosine powder (Sigma Ltd, Poole, UK) was used and dissolved in distilled water to reach the final concentration of 22 µm, where the filter was sterilized to obtain clear and homogenous solution.
2.4. Curcumin
Curcumin (Zingiberaceae-ginger F. curcuma longa L. as authenticated by Dr. Davari Nejad, Department of Botany, Ferdowsi University, Mashhad, Iran) was used as aphotosensitizer because it absorbs blue light (absorption range 400–460 nm). To circumvent the relative insolubility of curcumin in non-organic solvents, a stock solution (1 mM) was prepared by dissolving the powder in 99.5% ethanol. Stock solution was further diluted to the concentrations to be tested by adding NaCl 0.9%; maximal ethanol concentration in bacterial cultures was less than 3% (v/v) (60 µM curcumin samples). The solution was stored in the refrigerator and protected from light until usage.
2.5. Hydrogen peroxide (H2O2)
Hydrogen peroxide (Sigma-Aldrich Co., Germany) was used at final concentrations of 0.3 mM. This concentration is significantly lower than the Minimum Inhibitory concentration for P. gingivalis and F. nucleatum reported by Mckenzie et al. in 2012 31).
2.6. Lethal photosensitization of bacteria
Colonies of P. gingivalis and F. nucleatum from Mueller-Hinton (MH) Agar plates were suspended in BHI broth, and bacterial density was visually adjusted to a turbidity of 0.5 McFarland standard reagents. The exact density (CFU/mL) of each suspension was verified on MH agar plates. P. gingivalis and F. nucleatum solutions were prepared for five 96-well (7mm diameter) flat-bottom plates with lids (Orange Scientific, Belgium) as follow: visible light + erythrosine (LED+ ER+), visible light + curcumin (LED+ CUR+), visible light + Hydrogen peroxide (LED+ H2O2+), erythrosine (LED− ER+), curcumin (LED− CUR+), Hydrogen peroxide (LED− H2O2+) and visible light without photosensitizer (LED+). In each study well of plates, 175 µL of P. gingivalis or F. nucleatum suspension plus 175 µL of each three photosensitizers added. In the group of visible light without photosensitizer (LED+), 175 µL of the sterile phosphate-buffered saline (PBS) was added to equalize the level of the walls. Samples were then kept in the dark for 5 min before irradiation. Samples of bacteria in suspension were exposed in a laminar flow hood (Besat, Tehran, Iran) under dark aseptic and aerobic conditions to the maximum output of each light source. The treatment was performed under aerobic condition since the result of a study strongly recommended that the mechanism of phototoxicity of blue light on periopathogenic bacteria is oxygen dependent, which might result mainly in the formation of hydroxyl radicals 32). Light devices were fixed in vertical positions at the level of the wells. To prevent light transmission into neighbouring wells, 15 wells of each plate, with 2-well distance between them, were selected and plates were covered with a black shield with an orifice corresponding to the diameter of the wells. Every sample was exposed 1, 2, 3, 4 and 5 min to light source, bacterial strain and medium combinations, equivalent to flounce of 34–172 J/cm2 using LED.
2.7. Determination of bacterial survival
After exposure of the bacteria in suspension to different treatment, samples were diluted 1:10 for six executive times in sterile broth. Then, triplicates of 10 µL were applied to the agar plates. Survival of these bacteria was determined by counting the number of colony forming units (CFU) after incubation. P. gingivalis and F. nucleatum were cultured under anaerobic condition at 37°C until bacteria colonies were visible (1–5 days). The percentage of surviving bacteria was calculated in relation to the control non-exposed samples under similar experimental conditions. All the experiments in which the results of the treated samples differed from those of the control were repeated at least five times.
2.8. Statistical methods
To assess the effect of bacterial strains, light source, photosensitizer and the length of exposure to light on bacterial survival, multiway analysis of variance (ANOVA) was applied. The one-sample t-test was used to determine whether the change in bacterial count was significant. All the applied tests were two-tailed, and a P value of ≤ 0.05 was considered statistically significant.
3. Results
Effect of different treatments and exposure time on bacterial growth
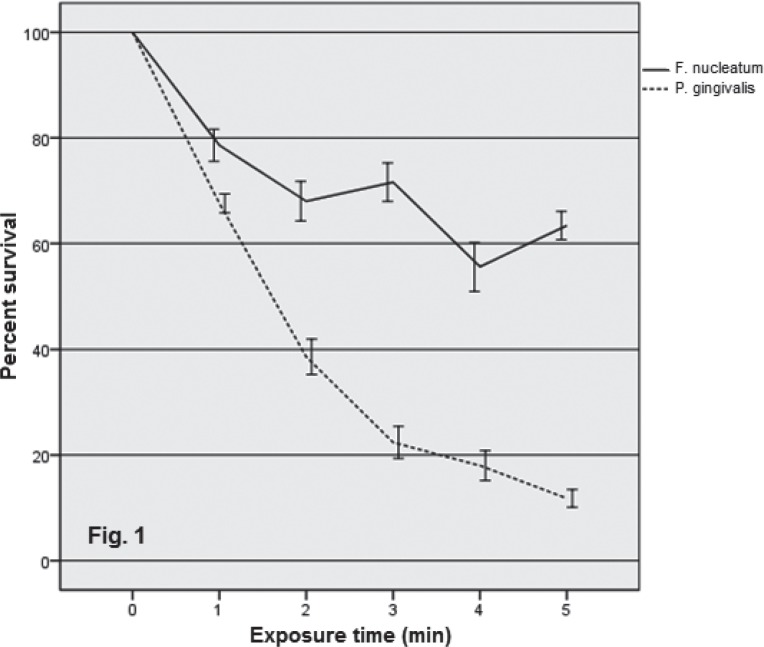
Viability was assessed after different treatments were applied to bacteria under same conditions and is expressed by percent survival of bacteria in suspension. To assess the effect of exposure time and different treatments on bacterial survival, multiway analysis of variance (ANOVA) was applied which its results (P=0.00 for both bacteria species) suggested that the both factors including the exposure time and treatment were significantly effective to reduce the viability of bacteria. Besides, to achieve the optimal treatment and exposure time for each bacteria species, the t-test was used when multiple pairwise comparisons were made. Exposure to visible blue light in the presence of these three photosensitizers reduced the viability of P. gingivalis and F. nucleatum noticeably, which was positively affected by exposure time. The reduced viability of P. gingivalis exposed to blue light alone for 3 min was significantly higher in comparison with F. nucleatum that may point out the potential susceptibility of P. gingivalis as black-pigmented bacteria possess endogenous porphyrins to visible light (Fig. 1).
Fig. 1:
Effect of visible blue light on viability of both species examined in suspension during 5 min irradiation. Error bars indicate the SD.
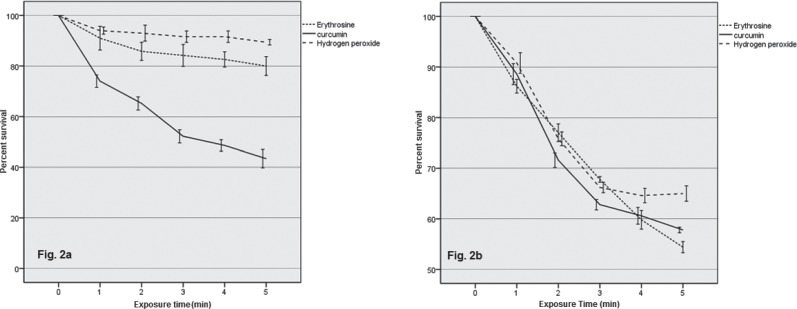
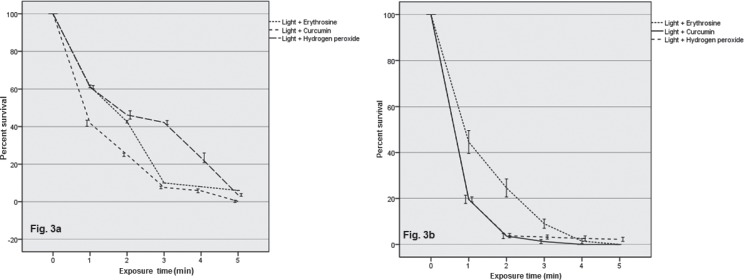
Results for antibacterial assays on P. gingivalis confirmed that curcumin, Hydrogen peroxide and erythrosine alone exerted a moderate bactericidal effect which enhanced noticeably in conjugation with visible light. For instance, the viability of P. gingivalis decreased to approximately 60% when these three photosensitizers applied alone on the suspension of both species examined for 5 min (Fig. 2b). Besides, the survival rate of P. gingivalis reached zero present when the suspension exposed to blue light-activated curcumin and hydrogen peroxide for 2 min. However, erythrosine-mediated photodynamic therapy killed approximately the whole population of this bacteria species during 4 min (Fig. 3b).
Fig. 2:
Effect of photosensitizers on viability of F. nucleatum (a) and P. gingivalis (b) in suspension during 5 min exposure. Error bars indicate the SD.
Fig. 3.
Effect of blue light-activated hydrogen peroxide, curcumin and erythrosine on survival rate of F. nucleatum (a) and P. gingivalis (b) in suspension during 5 min irradiation. Error bars indicate the SD.
On the other hand, curcumin exerted a remarkable antibacterial activity against F. nucleatum in comparison with erythrosine and hydrogen peroxide suggested a statistically meaningful difference (P=0.00, t-test) (Fig. 2a). This result is in agreement with the finding of a study that indicated curcumin possesses antibacterial property against a number of Gram positive and Gram negative bacteria (37). Furthermore, the viable population of F. nucleatum reduced to 10% after 3 min when the suspension of bacteria exposed to blue light-activated curcumin or erythrosine while visible light-activated hydrogen peroxide led to 60% and 98% drop in survival rate of F. nucleatum after 3 and 5 min respectively (Fig. 3a).
We compared the bactericidal effect of photosensitizers that applied alone with blue light-activated ones. In this case, our results suggested a statistically meaningful difference (P=0.00 for erythrosine and H2O2, P=0.04 for curcumin, t-test) and consequently, this finding indicates a synergic antibacterial effect between blue light and these sensitizers on viability of P. gingivalis and F. nucleatum. Moreover, our results suggested that the maximum bactericidal effect of visible blue light-activated curcumin, erythrosine and hydrogen peroxide examined could be achieved for both species by optimal exposure time of 3 min which clearly is of clinical value of this antimicrobial regimen. In addition, we found that these photo-activated compounds we applied in our study may represent the potential photosensitizers of choice for clinical PDT of periodontal infections.
4. Discussion
Currently, there is considerable interest in the use of locally applied antimicrobial agents in the treatment of periodontitis 33). A major advantage of this approach over the systemic administration of such agents is that it minimizes disruption of the normal microflora at other body sites, so helping to avoid opportunistic infections at these sites. However, the low capability of these agents to penetrate the deep layers of the biofilm is considered a pivotal factor in this effect while it is conceivable that light energy has the capability to penetrate the deeper layers of the biofilm relatively more than chemical agents do. Besides, the other serious problem with this approach is the difficulty in maintaining therapeutic levels of the agent for a sufficient period of time due to elution of the agent by gingival crevicular fluid 34). The use of PDT, however, is not beset by such problems, as the photosensitizer needs to be retained in the periodontal pocket for only a short time. This is extremely encouraging, as the results of our study showed a significant bactericidal effect of visible blue light-activated erythrosine, curcumin and hydrogen peroxide on two main periopathogenic species for 3 min.
Bacteria species such as Porphyromonas and Prevotella endogenously synthetize porphyrines which absorb at wavelength similar to visible blue light used in this study 35). Soukos et al. claimed that broadband light (380 to 520 nm) rapidly and selectively kills oral black-pigmented bacteria (BPB) in pure cultures and in dental plaque samples obtained from human subjects with chronic periodontitis and they hypothesize that this killing effect is a result of light excitation of their endogenous porphyrins 36). Besides, the results of a study pointed out that those Bacteria which possess high amounts of endogenous photosensitizers can easily be destroyed with visible light 37). This result are in agreement completely with our findings that the irradiation of blue light after 3 min resulted in significant reduction of viability of P. gingivalis comparing with F. nucleatum. However, it was beyond the scope of the present study to test the role of this photosensitizer in phototoxicity of blue light on bacteria.
One of the photosensitizer that was used in this study was oral plaque disclosing agent or erythrosine. To our knowledge, there are rare reports of the use of erythrosine as a photosensitizer in the mouth. Clearly, erythrosine has an advantage over other photosensitizers in development, as it already targets dental plaque and has full approval for use in the mouth. To determine the phototoxic effect of erythrosine as sensitizer, we observed that the survival rate of both species examined exposed to blue light in conjugation with erythrosine, decreased noticeably to nearly zero percent following 4 min irradiation. Interestingly, these results completely are in agreement with the findings of a study that demonstrated the efficacy of erythrosine in sensitizing of non-oral microbes to killing by light 38).
Curcumin features many of the attributes of an ideal photosensitizer for photokilling of pathogens: it is very small, has the ability to form singlet oxygen in an aprotic environment and features excellent biocompatibility 19). In this study, we found potential antibacterial effect of curcumin on two main gram-negative periopathogenic bacteria since it reduced the survival rate of these species by nearly 50 percent. This result is in agreement with the finding of a study that indicated curcumin possesses antibacterial property against a number of Gram positive and Gram negative bacteria 39). The survival rate of P. gingivalis and F. nucleatum reached zero present when the suspension exposed to blue light- activated curcumin up to 2 min (68 J/cm2) and 3 min(102 J/cm2) respectively. Interestingly, the results of a study of a study suggested that Exposure of planktonic cultures of S. mutans to 2 µM of photo-activated curcumin reduced the population of live cells by 95.5% after 2 min irradiation 40). Recently, Mandroli and Bhat showed that curcumin exerted an antibacterial activity against standard strains of most prevalent organisms of deep carious lesions namely Streptocuccus mutans, Lactobacillus casei, Actinomyces viscosus and most prevalent strains of root canal bacteria namely Porphyromonas gingivalis, Prevotella intermedia41).
In the current investigation, we found an insignificant antibacterial effect of H2O2 against F. Nucleatum; however, the survival rate of this species reached zero percent when exposed to blue light-activated hydrogen peroxide for 5 min. on the other hand, H2O2-mediated PDT kill the whole population of P. gingivalis in suspension up to 2 min (68 J/cm2) irradiation which may show the more potential susceptibility of this species comparing to F. Nucleatum. These results are partly in agreement with the finding of Feuerstein et al. who showed that the combination of visible blue light exposure for 20 s (23 J/cm2) and a concentration of 0.3 mM H2O2 yielded 96% growth inhibition of S. mutans, whereas, when they were applied separately, bacterial growth was decreased by 3% when exposed to light and by 30% in the presence of H2O2 42).
The result of our study confirmed that the bactericidal effects of blue light-activated hydrogen peroxide, curcumin and erythrosine decreased moderately during the last minutes of irradiation (Fig. 3a, b). This fact can be explained not only by the limited numbers of photosensitizer's molecules but also by the limited reactive oxygen species (ROS) generating capacity. Moreover, the photodynamic process also leads to diminish photosensitizer level due to the photobleaching 11). Metcalf et al. observed that the fractionation of white light during the erythrosine-mediated PDT of S. mutans biofilm grown in vitro results in increased cell killing compared with continuous irradiation. This may be due to the replenishment, during dark periods, of target molecules (such as oxygen) for the excited photosensitizer and any photosensitizer concentration gradient might be equilibrated during dark periods 43). Therefore, we concluded that the maximum bactericidal effect of these treatments above for both species examined could be achieved by optimal exposure time of 3 min. However, for the longer exposure duration, we suggest to increase the concentration of the photosensitizer or consider a dark period in which the general replenishment of target molecules (such as oxygen) or redistribution of the photosensitizer would be happened.
The argument that the mechanism of killing of P. gingivalis by blue light is not photochemical but heat induced 44) is not inline with the result of a study where the authors indicated that toxic ROS are possibly generated. In the present investigation, we found that when using lethal light doses (up to 172 J/cm2) an increase in the temperature of the bacteria suspension was recorded but did not reached 27°C under the experimental conditions. Thus, this result probably may not support a rise in temperature as the killing mechanism involved; Perhaps, in clinical condition, the increased temperature duo to the light exposure may be reduced in the presence of some factors such as saliva.
5. Conclusion
We conclude that the blue light source, which is used to photopolymerize dental composite material, in conjugation with hydrogen peroxide, curcumin and erythrosine as potential oral photosensitizers could serve for significant reduction of main periopathogenic bacteria. The encouraging results of this preliminary study suggest that an in vivo investigation of this novel approach are worth undertaken to determine the efficacy of visible blue light-mediated PDT in the presence of these three photosensitizers on periopathogenic species and periodontal inflammatory signs and establish as an additional minimally invasive antibacterial treatment of plaque induced periodontal pathologies such as gingivitis and periodontitis.
Acknowledgements
This experiment is supported by the Dental Research Center of the Mashhad University of Medical Sciences, Mashhad, Iran. We also wish to thanks Dr. Yasaman Maleki for her invaluable input in statistical analysis of the date.
Conflict of interest
The authors report no conflicts of interest.
References
- 1: Norkiewicz DS, Breault LG, Wonderlich ST, Malone KH. The use of chemotherapeutic agents in localized periodontal pockets. Mil Med 2001;166(11):940-946. [PubMed] [Google Scholar]
- 2: Robinson C, Kirkham J, Percival R, Shore RC, Bonass WA, Brookes SJ, Kusa L, Nakagaki H, Kato K, Nattress B. A method for the quantitative sitespecific study of the biochemistry within dental plaque biofilms formed in vivo. Caries Res 1997;31(3):194-200. [DOI] [PubMed] [Google Scholar]
- 3: Sreenivasan P, Gaffar A. Antiplaque biocides and bacterial resistance: a review. J Clin Periodontol 2002;29(11):965-974. [DOI] [PubMed] [Google Scholar]
- 4: Wainwright M. Photodynamic antimicrobial chemotherapy (PACT). J Antimicrob Chemother 1998;42:13-28. [DOI] [PubMed] [Google Scholar]
- 5: George S, Hamblin MR, Kishen A. Uptake pathways of anionic and cationic photosensitizers into bacteria. Photochem Photobiol Sci 2009;8(6):788-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6: Mang TS, Tayal DP, Baier R. Photodynamic therapy as an alternative treatment for disinfection of bacteria in oral biofilm. Lasers Surg Med 2012;44(7):588-596. [DOI] [PubMed] [Google Scholar]
- 7: Kolenbrander PE. Oral microbial communities: biofilms, interactions, and genetic systems. Annu Rev Microbiol 2000;54:413-437. [DOI] [PubMed] [Google Scholar]
- 8: Begue WJ, Bard RC, Koehne GW. Microbial inhibition by erythrosine. J Dent Res 1966;45:1464-1467. [DOI] [PubMed] [Google Scholar]
- 9: Marsh PD, Bevis RA, Newman HN, Hallsworth AS, Robinson C, Weatherell JA, Pitter AF. Antibacterial activity of some plaque-disclosing agents and dyes. Caries Res 1989;23:348-350. [DOI] [PubMed] [Google Scholar]
- 10: Tran J, Olmsted J., III Intramolecular triplet-triplet energy transfer from xanthene dyes to an anthyrl substituent. J Photochem Photobiol A Chem 1993;71:45-49. [Google Scholar]
- 11: Wood S, Metcalf D, Devine D, Robinson C. Erythrosine is a potential photosensitizer for the photodynamic therapy of oral plaque biofilms. J Antimicrob Chemother 2006;57:680-684. [DOI] [PubMed] [Google Scholar]
- 12: Orth K, Beck G, Genze F, Rück A. Methylene blue mediated photodynamic therapy in experimental colorectal tumours in mice. J Photochem Photobiol B 2000;57(22-3):186-192. [DOI] [PubMed] [Google Scholar]
- 13: Capella MAM, Menzies S. Synergism between electrolysis and methylene blue photodynamic action in Escherichia coli. Int J Radiat Biol 1992;62:321-6. [DOI] [PubMed] [Google Scholar]
- 14: Usacheva MN, Teichert MC, Biel MA. Comparison of the methylene blue and toluidine blue photobactericidal efficacy against gram-positive and gram-negative microorganisms. Lasers Med Surg 2001;29:165-173. [DOI] [PubMed] [Google Scholar]
- 15: Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J 2013;15(1):195-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16: Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, Ko JY, Lin JT, Lin BR, Ming-Shiang W, Yu HS, Jee SH, Chen GS, Chen TM, Chen CA, Lai MK, Pu YS, Pan MH, Wang YJ, Tsai CC, Hsieh CY. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res 2001;21(4B):2895-2900. [PubMed] [Google Scholar]
- 17: Deodhar SD, Sethi R, Srimal RC. Preliminary study onantirheumatic activity of curcumin (diferuloyl methane). Indian J Med Res 1980;71:632-634. [PubMed] [Google Scholar]
- 18: Hatcher H, Planalp R, Cho J, Torti FM, Torti SV. Curcumin: from ancient medicine to current clinical trials. Cell Mol Life Sci 2008;65(11):1631-1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19: Araújo NC, Fontana CR, Gerbi MEM, Bagnato VS. Overall-mouth disinfection by photodynamic therapy using curcumin. Photomed Laser Surg 2012;30(2):96-101. [DOI] [PubMed] [Google Scholar]
- 20: Paschoal MA, Tonon CC, Spolidório DM, Bagnato VS, Giusti JS, Santos-Pinto L. Photodynamic potential of curcumin and blue LED against Streptococcus mutans in a planktonic culture. Photodiagnosis Photodyn Ther 2013;10(3):313-319. [DOI] [PubMed] [Google Scholar]
- 21: Chignell CF, Bilski P, Reszka KJ, Motton AG, Sik RH, Dahl TA. Spectral and photochemical properties of curcumin. Photochem Photobiol 1994;59(3):295-302. [DOI] [PubMed] [Google Scholar]
- 22: Khopde SM, Priyadarsini KI, Palit DK, Mukherjee T. Effect of solvent on the excited-state photophysical properties of curcumin. Photochem Photobiol 2000;72(5):625-631. [DOI] [PubMed] [Google Scholar]
- 23: Bruzell EM, Morisbak E, Tonnesen HH. Studies on curcumin and curcuminoids. XXIX. Photoinduced cytotoxicity of curcumin in selected aqueous preparations. Photochem Photobiol Sci 2005;4(7):523-530. [DOI] [PubMed] [Google Scholar]
- 24: McCullagh C, Robertson PKJ. Photo-dynamic biocidal action of methylene blue and hydrogen peroxide on the cyanobacterium Synechococcus leopoliensis under visible light irradiation. J Photochem Photobiol 2006;83(1):63-68. [DOI] [PubMed] [Google Scholar]
- 25: Feuerstein O, Moreinos D, Steinberg D. Synergic antibacterial effect between visible light and hydrogen peroxide on Streptococcus mutans. J Antimicrob Chemother 2006;57(5): 872-876. [DOI] [PubMed] [Google Scholar]
- 26: O'Neill JF, Hope CK, Wilson M. Oral bacteria in multispecies biofilms can be killed by red light in the presence of toluidine blue. Lasers Surg Med 2002;31(2):86-90. [DOI] [PubMed] [Google Scholar]
- 27: Konig K, Teschke M, Sigusch B, Glockmann E, Eick S, Pfister W. Red light kills bacteria via photodynamic action. Cell Mol Biol 2000;46:1297-1303. [PubMed] [Google Scholar]
- 28: Komerik N, MacRobert AJ. Photodynamic therapy as an alternative antimicrobial modality for oral infections. J Environ Pathol Toxicol Oncol 2006;25(1-2):487-504. [DOI] [PubMed] [Google Scholar]
- 29: Feuerstein O, Persman N, Weiss EI. Phototoxic effect of visible light on Porphyromonas gingivalis and Fusobacterium nucleatum: an in vitro study. Photochem Photobiol 2004;80(3):412-415. [DOI] [PubMed] [Google Scholar]
- 30: Lubart R, Lipovski A, Nitzan Y, Friedmann H. a possible mechanism for the bactericidal effect of visible light. Laser Ther 2011;20(1):17-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31: McKenzie ME, Johnson NA, Aruni W, Dou Y, Masinde G, Fletcher HM. Differential response of Porphyromonas gingivalis to varying levels and duration of hydrogen peroxide-induced oxidative stress. Microbiology 2012;158(Pt 10):2465-2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32: Feuerstein O, Ginsburg I, Dayan E, Veler D, Weiss E. Mechanism of visible light phototoxicity on Porphyromonas gingivalis and Fusobacterium nucleatum. Photochem Photobiol 2005;81:1186-1189. [DOI] [PubMed] [Google Scholar]
- 33: Slots J, Jorgensen MJ. Effective, safe, practical and affordable periodontal antimicrobial therapy: where are we going, and are we there yet? Periodontol 2000, 2002;28:298-312. [DOI] [PubMed] [Google Scholar]
- 34: Oosterwaal PJ, Mikx FH, Renggli HH. Clearance of a topically applied fluorescein gel from periodontal pockets. J Clin Periodontol 1990;17(9):613-615. [PubMed] [Google Scholar]
- 35: Shah HN, Bonnett R, Mateen B, Williams RAD. The porphyrin pigmentation of subspecies of Bacteroides melaninogenicus. Biochem J 1979;180(1),45-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36: Soukos NS, Som S, Abernethy AD, Ruggiero K, dunham J, Lee C, Doukas AG, Goodson JM. Phototargeting oral black-pigmented bacteria. Antimicrob agents Chemother 2005;49:1391-1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37: Lubart R, Lipovski A, Nitzan Y, Friedmann H. a possible mechanism for the bactericidal effect of visible light. Laser Ther 2011;20(1):17-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38: Krasnoff SB, Faloon D, Williams JE, Gibson DM. Toxicity of xanthene dyes to entomopathogenic fungi. Biocont Sci Tech 1999;9:215-225. [Google Scholar]
- 39: Negi PS, Jayaprakasha GK, Jagan Mohan Rao L, Sakariah KK. Antibacterial activity turmeric oil: a byproduct from curcumin manufacture. J Agric Food Chem 1999;47(10):4297-4300. [DOI] [PubMed] [Google Scholar]
- 40: Manoil D, Filieri A, Gameiro C, Lange N, Schrenzel J, Wataha JC, Bouillaguet S. Flow cytometric assessment of Streptococcus mutans viability after exposure to blue light-activated curcumin. Photodiagnosis and Photodyn ther 2014;11(3):372-379. [DOI] [PubMed] [Google Scholar]
- 41: Mandroli PS, Bhat K. An in-vitro evaluation of antibacterial activity of curcumin against common endodontic bacteria. J Applied Pharmaceutical Sci 2013;3(10):106-108. [Google Scholar]
- 42: Branco MR1, Marinho HS, Cyrne L, Antunes F. Decreased of H2O2 plasma membrane permeability during adaptation of H2O2 in Saccharomyces cerevisiae. J Biol Chem 2004;279(8):6501-6506. [DOI] [PubMed] [Google Scholar]
- 43: Metcalf D, Robinson C, devine D, Wood S. Enhancement of erythrosine-mediated photodynamic therapy of Streptococcus mutans biofilms by light fractionation. J Antimicrob Chemother 2006;58:190-92. [DOI] [PubMed] [Google Scholar]
- 44: Izzo AD, Walsh JT. Light induced modulation of Porphyromonas gingivalis growth. J Photochem Photobiol 2004;77:63-69. [DOI] [PubMed] [Google Scholar]