Abstract
Objective. The Society for Hospital Medicine (SHM) conducted a survey of U.S. hospital systems to determine how nonphysician providers (NPPs) are utilized in interdisciplinary glucose management teams.
Methods. An online survey grouped 50 questions into broad categories related to team functions. Queries addressed strategies that had proven successful, as well as challenges encountered. Fifty surveys were electronically distributed with an invitation to respond. A subset of seven respondents identified as having active glycemic committees that met at least every other month also participated in an in-depth telephone interview conducted by an SHM Glycemic Advisory Panel physician and NPP to obtain further details. The survey and interviews were conducted from May to July 2012.
Results. Nineteen hospital/hospital system teams completed the survey (38% response rate). Most of the teams (52%) had existed for 1–5 years and served 90–100% of noncritical care, medical critical care, and surgical units. All of the glycemic control teams were supported by the use of protocols for insulin infusion, basal-bolus subcutaneous insulin orders, and hypoglycemia management. However, > 20% did not have protocols for discontinuation of oral hypoglycemic agents on admission or for transition from intravenous to subcutaneous insulin infusion. About 30% lacked protocols assessing A1C during the admission or providing guidance for insulin pump management. One-third reported that glycemic triggers led to preauthorized consultation or assumption of care for hyperglycemia.
Institutional knowledge assessment programs were common for nurses (85%); intermediate for pharmacists, nutritionists, residents, and students (40–45%); and uncommon for fellows (25%) and attending physicians (20%). Many institutions were not monitoring appropriate use of insulin, oral agents, or insulin protocol utilization. Although the majority of teams had a process in place for post-discharge referrals and specific written instructions were provided, only one-fourth were supported with written protocols to standardize medication, education, equipment, and follow-up instructions.
Conclusion. Inpatient glycemic control teams with NPPs often function in environments without a full set of measurement, education, standardization, transition, and order tools. Executive hospital leaders, community partners, and the glycemic control teams themselves need to address these deficiencies to optimize team effectiveness.
Given the national, and indeed global, epidemic of diabetes,1 it should not be surprising that there has also been a substantial increase in diabetes inpatient cases. From 1988 to 2009, the number of hospital discharges with a diabetes diagnosis doubled from ∼ 3 million to 6 million,2 representing a prevalence of 20–40% of all inpatients.3–5 Furthermore, there is a high reported incidence of unrecognized diabetes in the hospital setting, with rates ranging from 12 to 36%.4,5
National organizations have published guidance for the management of hyperglycemia in the hospital.6,7 These professional societies have strongly advocated for an integrated approach to delivery of inpatient and transitional care for diabetes and hyperglycemia, and a 2012 U.S. Supreme Court ruling confirming the legality of the Patient Protection and Affordable Care Act (ACA) of 2010 recently added strength to this recommendation.8,9 An important feature of the ACA is its call for integrated health care delivery across all settings to decrease hospital readmissions, among other outcomes.8 Hospital glycemic management services afford the opportunity to optimize inpatient glycemic control, enable identification and initiation of long-term diabetes management for those with previously unrecognized diabetes, and allow for the development of patient-friendly glycemic management discharge regimens for those with an established diagnosis of diabetes, thus contributing to prevention of readmissions and the comorbidities and high costs associated with diabetes complications.
Efforts to implement guideline-directed best practices for inpatients with hyperglycemia and coordinate their transitions of care6,7 are underway in numerous U.S. hospitals. Glycemic control teams inclusive of nonphysician providers (NPPs) are increasingly seen as a means to accelerate and reinforce practice guidelines and improve care. However, there has been little research into the structure or environment of these teams or their utility in care coordination and transitions across settings. Consequently, in 2012, the Society of Hospital Medicine (SHM) conducted a survey of U.S. hospital systems to better describe how NPPs are utilized on interdisciplinary glucose management teams and the environments in which they function. A secondary goal of the survey was to summarize best practices and strategies to optimize the effectiveness and efficiency of NPPs and their teams, as informed by the survey, interviews, and dialogue among the members of the SHM Glycemic Advisory Panel.
Methods
Project overview
The SHM advisory panel, which included two adult endocrinologists, one hospitalist, two nurse practitioners (NPs), and one physician assistant (PA), developed and conducted a survey of well-established interdisciplinary inpatient glycemic management teams. The goals of this survey were to 1) characterize team composition and the role of NPPs, 2) examine strategies and the availability of tools supporting delivery of glycemic management services, including protocols and triggers for management interventions and education of patients and providers, 3) delineate strategies and availability of tools supporting discharge planning and transitions of care, 4) establish which metrics were available to assist teams in tracking team progress and outcomes, and 5) inform the advisory panel as they formulated recommendations to optimize the effectiveness and efficiency of NPPs on glycemic control teams.
Survey and analysis methodology
Advisory panel members were selected based on their experience with inpatient glycemic management and involvement in regional or national collaborative efforts. An online survey was designed to capture detailed information related to the structure and functions of each site’s glycemic management team. Fifty questions were grouped into broad content categories related to aspects of team functionality. Queries addressed strategies that had proven successful, as well as challenges the teams had encountered.
Drawing from panel recommendations and a list of hospitals that had earned Joint Commission inpatient advanced certification in diabetes,10 SHM electronically distributed 50 surveys with an invitation to respond. A subset of seven respondents identified as having active glycemic committees that met at least every other month also participated in an in-depth telephone interview conducted by a panel physician and NPP to obtain further details. The survey and interviews were conducted from May to July 2012.
Results
Response rate and demographics
Nineteen hospitals’ or hospital systems’ teams completed and returned the survey, representing a 38% response rate. One responding hospital had Joint Commission inpatient diabetes certification. Among the core group responding, about half represented a single hospital and the balance represented two to five hospitals. The hospitals with responding teams were predominantly in urban settings. The majority were large (≥ 300 beds) teaching hospitals with an electronic medical record (EMR) system. About 60% used computerized provider order entry. Survey results for the entire cohort are shown in a supplemental appendix that can be accessed through the SHM website (http://www.hospitalmedicine.org/Web/Quality_Innovation/Implementation_Toolkits/Glycemic_Control/Web/Quality___Innovation/Implementation_Toolkit/Glycemic/Mentored_Implementation_Program.aspx#).
Survey findings
Glycemic management teams were interdisciplinary in composition.
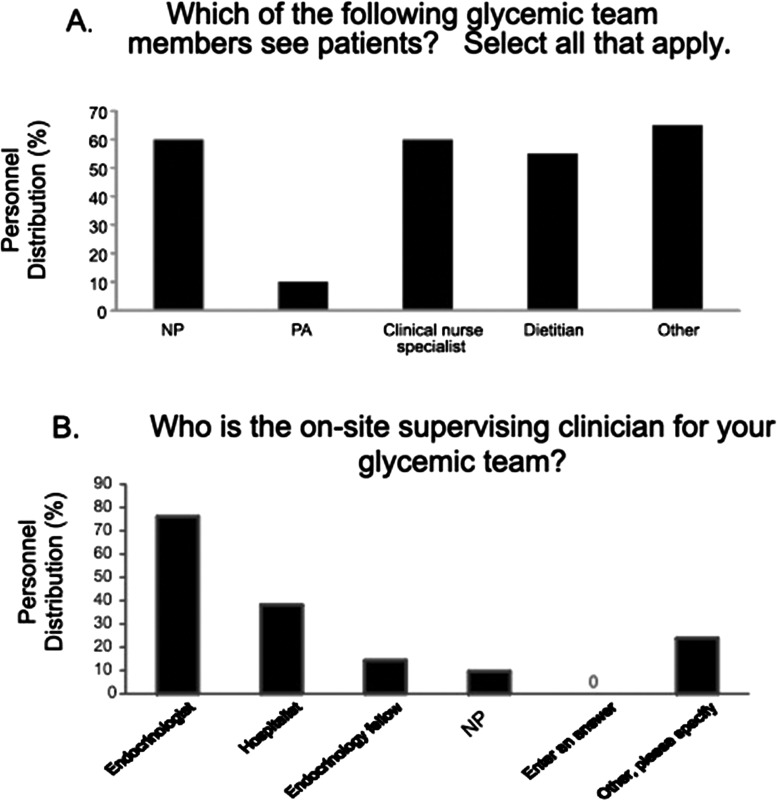
These were all well-established teams, 52% of which had been in existence for 1–5 years and the balance for > 5 years. All but one had a glycemic control committee that met regularly, with ∼ 60% convening monthly and most others meeting every other month or quarterly. Interdisciplinary team membership was a key feature of the teams, with the majority consisting of NPPs such as NPs or clinical nurse specialists (Figure 1A).
Figure 1.
Leadership patiernt care (A) and supervisory (B) roles and responsibilities of NPPs on glycemic management teams.
The leadership role was undertaken by one or more designated “glycemic champion(s),” typically a physician (hospitalist or endocrinologist), an NPP with expertise in diabetes management (NP or PA), or a registered nurse or registered dietitian who was a certified diabetes educator. The onsite supervising clinician for the majority of teams was an endocrinologist or hospitalist (Figure 1B). Other key team members included nurses, pharmacists, dietitians, quality improvement staff members, informatics specialists, graduate trainees (i.e., residents, interns, or endocrine fellows), surgeons, and anesthesiologists.
Glycemic management teams provided care throughout hospitals.
Nearly all (90–100%) of the teams served noncritical care and critical care medical and surgical units. Emergency departments, psychiatry units, obstetrics and gynecology units, and pediatrics units were also served by some teams to a lesser extent. Many teams saw patients for delivery of both medical care and education services.
NPPs provided evaluations and direct medical management recommendations.
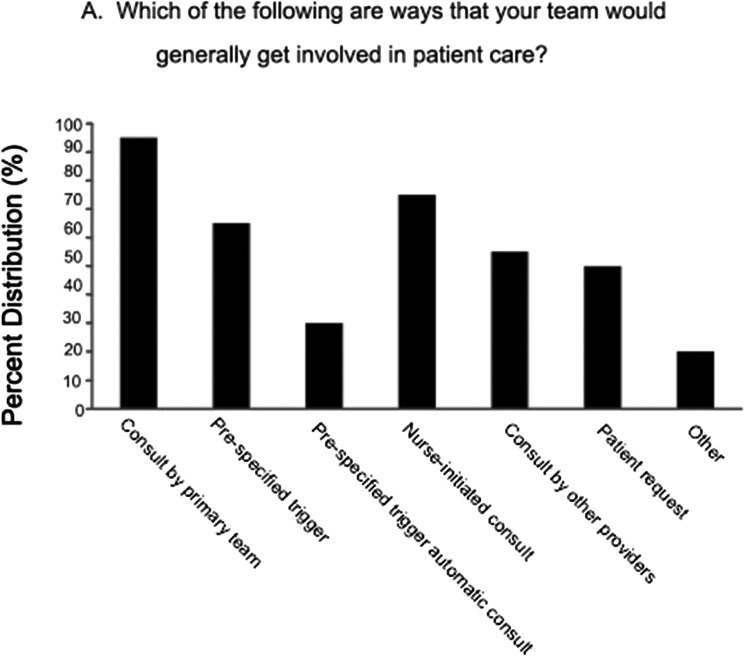
Fully 90% of the teams provided direct medical management, defined as active consultation or directly changing or recommending changes to patient orders. Figure 2A depicts the methods that triggered medical management interventions. Most common were direct requests for consultation from the primary inpatient team, nursing staff, or prespecified high or low glucose triggers that prompted calls to the primary team to provide suggestions. One-third of respondents reported that glycemic triggers led to preauthorized formal consultation or assumption of care for hyperglycemia. Patient requests and referrals from ancillary personnel could also trigger team involvement.
Figure 2.
Triggers for intervention and by glycemic management teams (A) and defined populations they serve (B).
Teams were asked if there were defined populations they routinely evaluated (Figure 2B). Routine consultation was common for patients with insulin pumps and for those with hypo- or hyperglycemia. Some teams routinely covered selected services or units.
Glycemic care recommendations were conveyed to the primary care team using various approaches. All used a consultation note and paging or direct communication by phone or in person. Sixty percent also communicated with patients’ nurses. Orders for management were written by just over half of the teams. The number of patients seen daily for medical management services varied, with half of teams seeing ≥ 11patients daily and the balance seeing from 1 to 10 patients daily. In just under half of the programs, the same NPPs performed both medical management and diabetes self-management education (DSME), which may explain the low numbers of patients being medically managed in some programs. Billing for glycemic management consultative services was performed either by physicians or NPPs. Forty percent of the responding programs did not bill for services rendered.
Many recommended best practices for safe and effective inpatient glycemic control were inconsistently supported by medical center protocols and order sets.
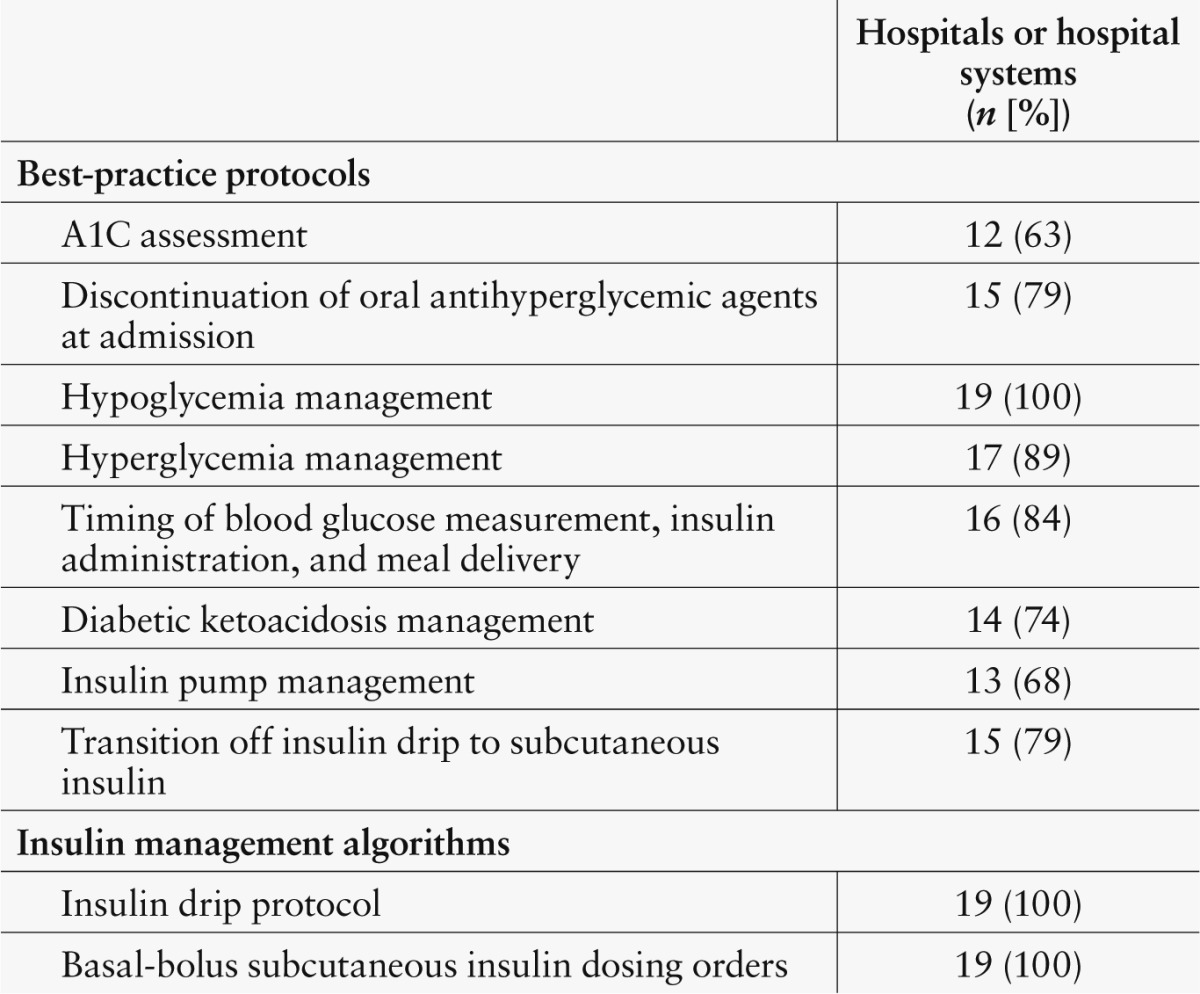
The distribution of practice protocols and insulin management algorithms across hospitals is shown in Table 1. All had insulin infusion protocols, basal-bolus subcutaneous insulin orders, and hypoglycemia management protocols in place. Some consensus-recommended best practices6,7 were not reliably supported by local protocols. More than 20% had no protocol prompting discontinuation of oral hypoglycemic agents on admission, and an equal number lacked a protocol for transition from insulin infusion to subcutaneous insulin. About one-third lacked protocols or policies prescribing assessment of A1C during the admission or providing guidance for insulin pump management.
Table 1.
Distribution of Best-Practice Protocols and Insulin Management Algorithms Across Hospitals and Hospital Systems
Glycemic management teams used multiple approaches for DSME.
Requests to provide education came in response to prespecified glycemic triggers or directly from nursing staff, providers, or patients. DSME services were provided routinely based on a variety of selection criteria, most commonly for patients with hyperglycemia, hypoglycemia, or insulin pumps. They were also unit based or service based. DSME was provided to fewer patients in intensive care units or emergency departments than in medical service wards and to about half of the patients in obstetrics and gynecology wards.
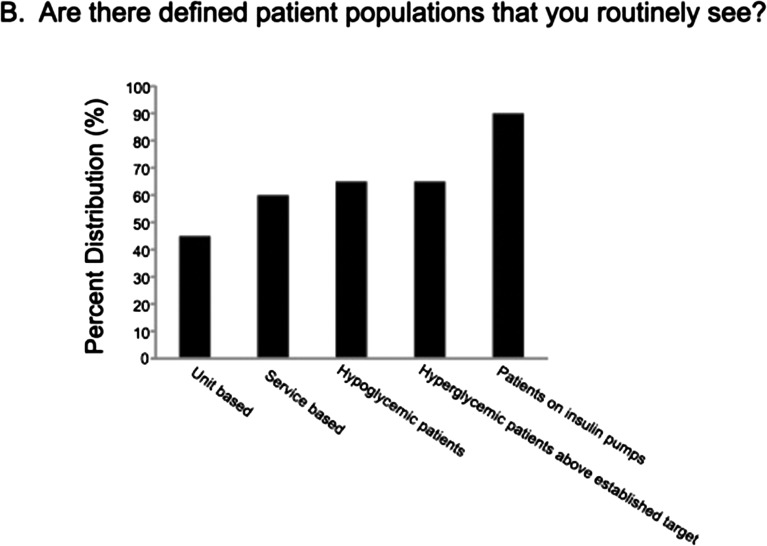
All hospitals reported delivering DSME via one-on-one education and provision of printed materials (Figure 3). About two-thirds also utilized online or video education tools. Less than 20% provided group DSME. Patient comprehension of DSME content was assessed using return demonstration, verbal assessment, or practice assessment. Written evaluation was less common. Education recommendations were most commonly provided in written form, by talking directly with a patient’s nurse, or by talking to the patient’s prescribing provider. Just under half of the time, the educator directly wrote teaching orders. Hospital teams did not bill for inpatient diabetes education.
Figure 3.
Multiple educational approaches for patients with diabetes.
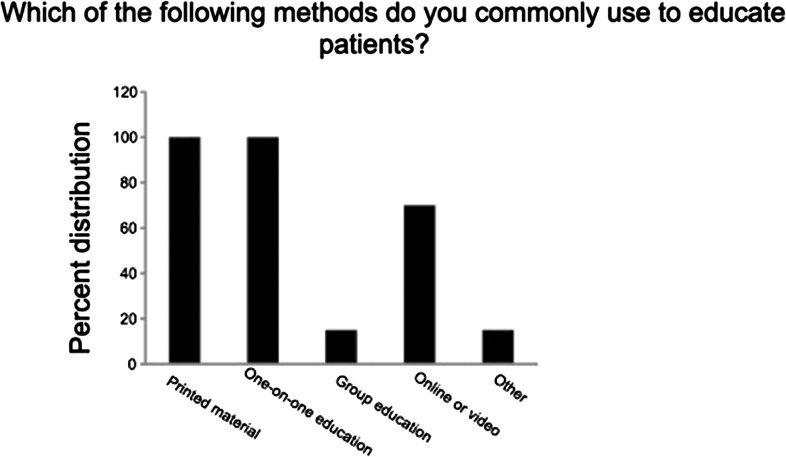
Professional education programs varied widely by the type of health care provider.
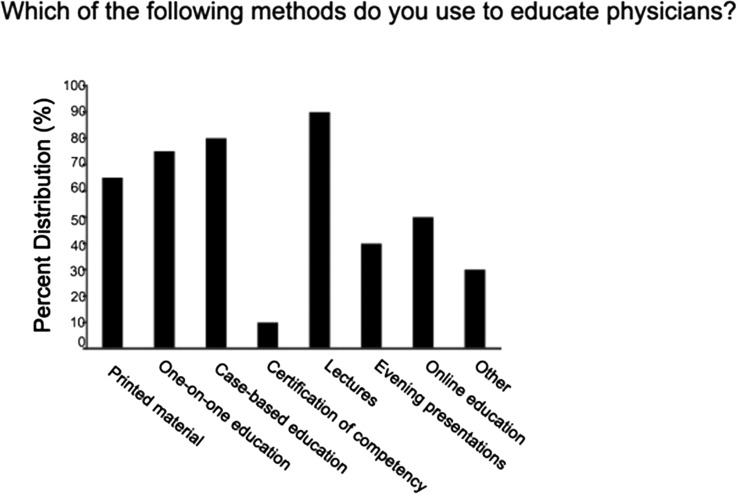
A wide variety of approaches ranging from printed materials to lectures to online learning centers were used to educate physicians (Figure 4). Just two hospitals had implemented prescriber certification of glycemic management competency, whereas 12 had such certification in place for nurses.
Figure 4.
Multiple educational approaches for physicians.
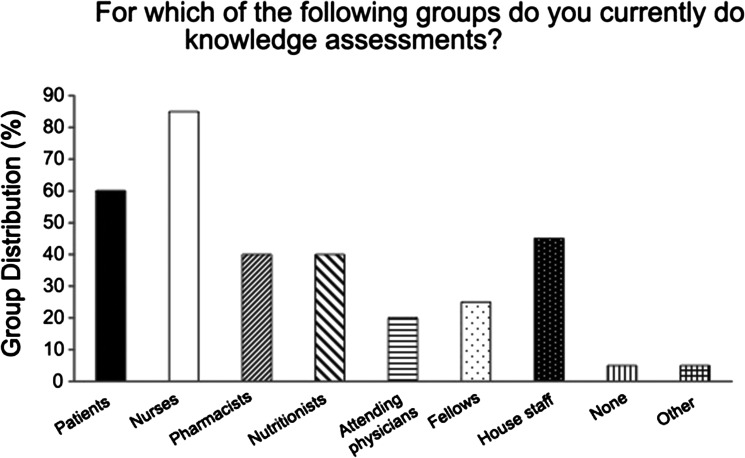
Nursing staff education was most commonly provided through lectures and printed materials. Nursing education instructors provided oversight for nursing education in all hospitals, with physicians and NPs supporting the effort ∼ 30% of the time. Knowledge assessment was conducted for nurses at 85% of responding facilities; for pharmacists, nutritionists, and residents or medical students at 40–45% of the facilities; for fellows at 25% of the facilities; and for attending physicians at 20% of facilities (Figure 5). One system had developed online diabetes training modules that were required for medical residents and provided continuing medical education credits for attending physicians.
Figure 5.
Diabetes knowledge assessments for health care providers.
The metrics and assessment tools available to glycemic management teams varied, and measures were not routinely shared with leadership.
The availability of metrics and analysis of outcomes for assessing the impact of team interventions varied widely. Tracking parameters differed based on accessibility of data. The majority of teams obtained metrics and outcomes from their hospital electronic data repositories, including the EMR, the laboratory database (incorporating laboratory and downloaded point-of-care blood glucose meter measurements), hospital outcomes databases, and third-party data collectors. Heterogeneity in metrics and outcomes tracked was reported, with > 15 measures being cited overall. The parameters tracked by the responding hospitals are detailed in Table 2. A large proportion of respondents reported that they are not currently monitoring appropriate use of insulin or oral agents, protocol utilization, or a number of other clinically relevant parameters.
Table 2.
Metrics and Outcomes Available to Inpatient Glycemic Management Teams
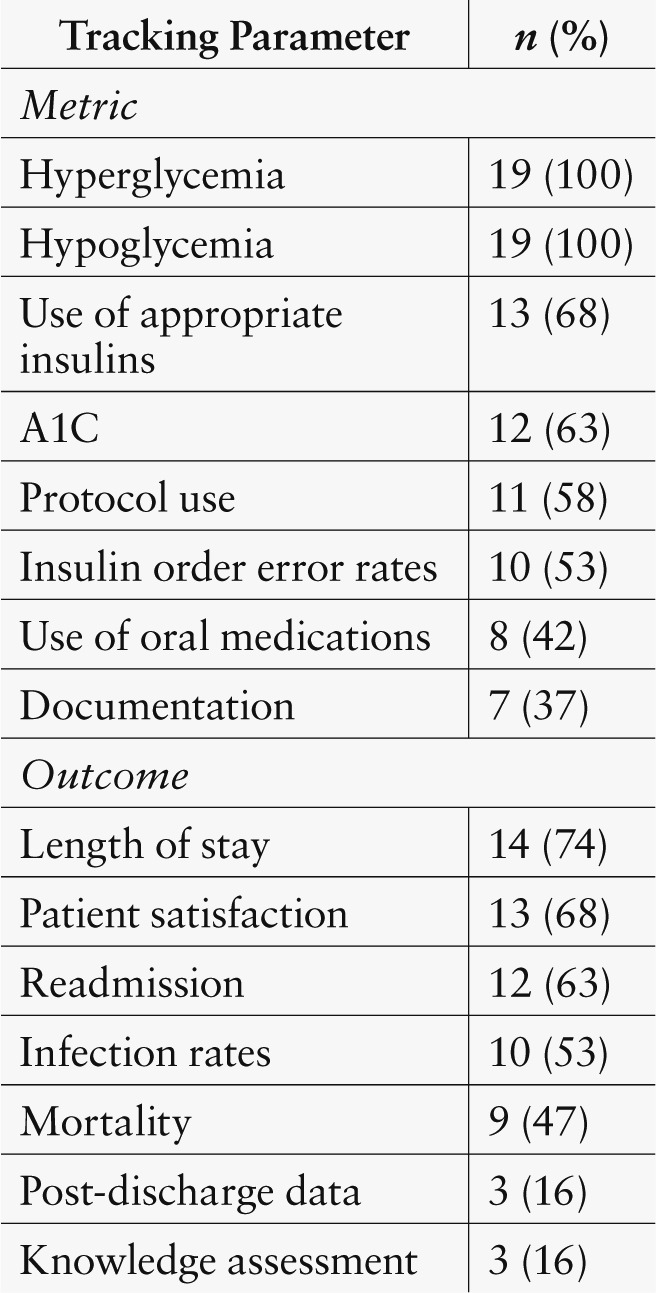
Glycemic targets for critical and noncritical care units were generally consistent with consensus statement target ranges (e.g., 140–180 mg/dl).11–14 Metrics and outcomes were shared with the hospital glycemic committee, nursing staff, and physicians by the majority of respondents. Only about one-third of the hospitals were reporting metrics and outcomes to corporate suite executive teams, and one shared results with patients.
Performance-based incentives based on metrics were given to physicians at 21% of responding hospitals, management at 11%, hospitals at 16%, and corporate suite executives at 5%. It was not a goal of this survey to examine glycemic control metrics results because this will be the topic of another SHM publication. However, the heterogeneity of methods to track glycemic control and hypoglycemia was apparent.
Effective transitions to outpatient care were a challenge for glycemic management teams.
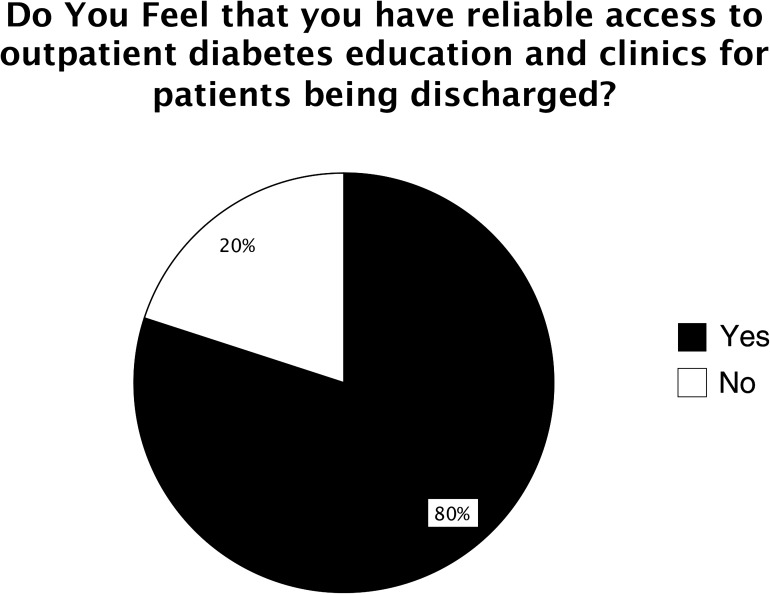
Many responding facilities reported facing limitations to reliable access to outpatient diabetes care programs as part of the transition to outpatient care (Figure 6). Less than 20% of teams reported tracking any glycemic control or A1C parameters after discharge, but two-thirds reported monitoring readmission rates. Although the majority of teams had a process in place for post-discharge referrals and provided patients with specific written instructions, only about one-fourth had written protocols to standardize medication, education, equipment, and follow-up instructions. Although most teams offered access to post-discharge DSME and clinic services, 21% did not have reliable access to these resources, and about one-third did not feel that they have dependable access to diabetes supplies and medications for their patients.
Figure 6.
Limitations to reliable access to transition of care resources in the outpatient setting.
Uneven coverage on weekends and nights was described as a challenge to providing reliable glycemic management expertise to support transitions to the outpatient setting. With regard to the scope of coverage hours provided by NP or PA team members, only about 30% provided night coverage, and < 20% provided around-the-clock coverage or rotated call duties with physician team members. Only one-third of NPPs provide weekend coverage.
Discussion
The overall goals of this SHM survey on hospital glycemic management practices were to assess the structure, function, and environment of NPPs and their teams in medical management, education, and transition of care roles; identify potential areas for improvement; and summarize best practices and strategies to optimize the effectiveness and efficiency of NPPs and their teams, as informed by the survey, interviews, and dialogue among the membership of the SHM Glycemic Advisory Panel.
To our knowledge, this is the first survey addressing this topic. The results showed that NPPs were integral health care providers in inpatient glycemic management teams. NPPs were perceived as being valued members of the glycemic management team. NPs and PAs were directly responsible for evaluating, managing, and often providing diabetes education to hospitalized patients. In addition to these direct care responsibilities, NPPs also participated in administrative duties such as monthly committee meetings, establishment of patient care protocols, and education of nursing staff, pharmacists, and ordering providers. However, despite the extensive roles they play, these inpatient glycemic management teams with NPPs often function in environments lacking a full complement of organizational, measurement, education, standardization, transition, and order set tools.
Important gaps in care and infrastructure
Administrative leadership was not regularly updated about glycemic team efforts or metrics, with correspondingly low (5%) rates of corporate suite executives having any incentive aligned with glycemic control priorities. Although all of the surveyed teams implemented insulin drip protocols, subcutaneous basal-bolus insulin order sets, and hypoglycemia management protocols, important protocols affecting diabetic ketoacidosis management, insulin pumps, transitions, and discontinuation of oral hypoglycemic agents were often lacking (Table 1). Measures related to many of these same issues and outcomes that can be influenced by glycemic control teams were also frequently not available to these teams, potentially hampering their effectiveness or even awareness of problems (Table 2).
NPPs and their teams were involved in a wide variety of educational efforts, but survey results indicated that nurses commonly underwent knowledge assessments, whereas physicians did not. This is an area of medical education that is clearly lacking for physicians who continue to have knowledge deficits related to insulin and diabetes management in general.15 Sites that had strong nursing and pharmacy partners in education seemed to function the best, allowing more direct patient management and systems improvement time for the NPPs on the glycemic control team.
The importance of optimizing anti-hyperglycemic agent therapy regimens and adequate DSME to improve self-care management is highlighted by recent surveillance data revealing a prominent role of hypoglycemic adverse drug events as a precipitant to emergency department visits, admissions, and readmissions in patients ≥ 65 years of age.16 NPPs and glycemic control teams have the potential to smooth transitions of care, reduce readmissions, and improve long-term glycemic control,17 but the infrastructure and gaps in care revealed through this survey were perhaps most pervasive in this area, with many sites having lapses in protocol guidance, measurement, night and weekend coverage, availability of community follow-up, and institutional prioritization in these areas.
Advisory panel recommendations
After deliberation over survey and interview results, the SHM glycemic control advisory panel presents the following recommendations to enhance the effectiveness and efficiency of NPPs and their glycemic control teams. These recommendations are aligned with those of the American Diabetes Association and American Association of Clinical Endocrinologists6 and the Joint Commission certification program for inpatient diabetes management.10 However, we suggest that these more comprehensive recommendations may be necessary to realize the full potential of these teams (Table 3).
Table 3.
Recommended Structure, Protocols, Metrics, and Strategies for Hospital Glycemic Teams

Structure and administrative support.
The glycemic management team should function as a core component of a comprehensive glycemic control effort, with regular meetings of an interdisciplinary steering committee. Engagement from medical staff, hospital executives, and units should be secured by feedback on performance, awareness and education campaigns, assignment of administrative liaisons, and aligned incentives.18 Administrative support should be manifest by a regular review of progress, information technology and standardization resources, performance incentives, and enforcement of educational standards.
Education and direct patient care issues.
Glycemic management team NPPs should provide direct patient care, as well as educational services. To maximize the impact of this relatively small, specialized management team, other providers such as bedside nurses, diabetes resource nurses, and pharmacists should be utilized for basic patient education and to facilitate adoption and reinforcement of protocols and order sets. The glycemic management team NPPs should direct their educational efforts to particularly high-risk patients and spend time educating and creating and reinforcing protocols with other members of the overall glycemic management effort. DSME programs should incorporate teach-back techniques and be sensitive to patients’ goals, health literacy and numeracy, and psychosocial issues to enhance patients’ understanding and activation.19
The core glycemic management team’s triggers for involvement in patient management should include proactive monitoring for glycemic outliers and protocol nonadherence, as well as direct consultation from primary teams, nurses, and patients. Staff educational programs with assessment of knowledge of concepts and protocols should include physicians, as well as nurses and other providers.
Best-practice protocols, clinical decision support, and measures.
A full complement of best-practice protocols should be designed, implemented with clinical-decision support at the point of care, monitored, maintained, and revised as needed. Protocols and related order sets, educational materials, and transition tools reinforce best practices with front-line providers, reduce variation, and allow the core team to focus on patients more in need of their expertise and direct involvement. Protocols should include the full range of topics described in Table 1.
Uncontrolled hyper- and hypoglycemia rates, timeliness of hypoglycemia management, and recurrent hypoglycemia rates should be tracked by the team on a monthly basis to prioritize interventions and assess intended and unintended consequences of interventions. Principles for measurement have been described,20,21 and outsourcing of these metrics and benchmarking with SHM or other organizations is now available as a low- or no-cost option to building the reports.22–24 Surrogate measures for hypoglycemia (e.g., the use of 50% dextrose) are poor substitutes for more accurate tracking of hypoglycemic events. Tracking patterns in insulin and oral hypoglycemic agent use, A1C testing, and the outcomes included in Table 2 are also recommended. Day-to-day identification of glycemic outliers and patients who are potentially “off protocol” is also recommended.
Transitions of care and care coordination.
Transitions and care coordination should be high priorities for NPPs and inpatient glycemic control teams. Coordination with larger institutional efforts to reduce readmissions and improve transitions of care is necessary. Protocols outlining transition to the outpatient setting should take into account patient history, preferences, fiscal constraints, psychosocial issues, A1C, and community resources available for follow-up. Community partnerships, innovation, longitudinal case management or pharmacy follow-up, expedited outpatient follow-up, post-discharge phone contact, and home care nurses should all be considered for high-risk patients. Outpatient DSME and access to diabetes medications and supplies after discharge should be secured in advance, if possible. On a public policy level, exploration of payment models that allow for billing of diabetes management, diabetes education, and care coordination services should be explored.
Conclusions
The results of this survey revealed that well-established glycemic control teams incorporating NPPs provide valuable services, but often have gaps in infrastructure and reliable assurance of glycemic management best practices across the spectrum of care settings. To some extent, gaps in care reflect opportunities for the glycemic care team members themselves, whereas in others cases (e.g., unreliable access to post-discharge diabetes supplies and medications), some changes in organizational structure, institutional prioritization, and community support services are needed to close the gaps.
The limitations of this survey merit discussion. Only 38% of hospitals and hospital systems invited to complete the survey did so. It is possible that glycemic management team practices at the participating sites differed from those at sites that did not respond. Although there have been viewpoints advocating for surveys to assess nonresponse bias,25 we did not obtain information regarding practices for glycemic management at the nonrespondent hospitals, and their reasons for electing not to participate were not assessed. In addition, the surveys and telephone interviews relied almost exclusively on self-reporting. On the other hand, any selection bias would tend to minimize the gaps in infrastructure and care that were revealed by the survey because this select group of medical centers likely represent better-than-average performers.
Our recommendations and strategies to optimize the effectiveness and efficiency of these teams rely to some degree on our internal dialogue and experience, rather than on a level of evidence obtained through randomized, controlled trials. However, they are aligned with the recommendations of others6,7,10,18 and are grounded in large-scale collaborative improvement cohorts involving a wide variety of hospitals.26 In the next phase of our efforts, we will work with a cohort of sites with glycemic control teams and NPPs in an attempt to gauge the impact of implementing these recommendations to address gaps in the optimal care of inpatients with hyperglycemia.
References
- 1.Centers for Disease Control and Prevention: National diabetes fact sheet : national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, Ga, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 2.Centers for Disease Control and Prevention : Diabetes data and trends, diabetes surveillance system: number (in thousands) of hospital discharges with diabetes as any-listed diagnosis, United States, 1980–2005. Available from http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed 5 June 2014
- 3.Fraze T, Jiang HJ, Burgess J: Hospital stays for patients with diabetes, 2008. AHRQ Healthcare Cost and Utilization Project. Statistical Brief #93. August 2010. Available from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb93.pdf. Accessed 28 November 2012 [PubMed]
- 4.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE: Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87:978–982, 2002 [DOI] [PubMed] [Google Scholar]
- 5.Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE: Unrecognized diabetes among hospitalized patients. Diabetes Care 21:246–249, 1998 [DOI] [PubMed] [Google Scholar]
- 6.Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE: American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care 32:1119–1131, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, Seley JJ, Van den Berghe G: Management of hyperglycemia in hospitalized patients in non-critical care setting: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97:16–38, 2012 [DOI] [PubMed] [Google Scholar]
- 8.Patient Protection and Affordability Care Act (H.R.3590) Available from http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf. Accessed 5 June 2014.
- 9.National Federation of Independent Business et al v. Sebelius, Secretary of Health and Human Services, et al. (No. 11–393, argued 26–28 March 2012; decided 28 June 2012. Available from http://www.supremecourt.gov/opinions/11pdf/11-393c3a2.pdf. Accessed 5 June 2014
- 10.Joint Commission : Inpatient advanced certification in diabetes. Available from http://www.jointcommission.org/certification/inpatient_diabetes.aspx. Accessed 20 November 2012
- 11.NICE-SUGAR Study Investigators : Intensive versus conventional glucose control in critically ill patients. N Engl J Med 360:1283–1297, 2009 [DOI] [PubMed] [Google Scholar]
- 12.Krinsley JS, Aarti G: Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med 35:2262–2267, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Inzucchi SE, Siegel MD: Glucose control in the ICU: how tight is too tight? N Engl J Med 360:1346–1349, 2009 [DOI] [PubMed] [Google Scholar]
- 14.Wiener RS, Wiener DC, Larson RJ: Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA 300:933–944, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Derr R, Sivanandy M, Bronich-Hall, Rodriguez A: Insulin-related knowledge among health care professionals in internal medicine. Diabetes Spectrum 20:177–185, 2007 [Google Scholar]
- 16.Budnitz DS, Shehab N, Kegler SR, Richards CL: Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med 147:755–765, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Wei NJ, Wexler D, Nathan DM, Grant RW: Intensification of diabetes medication and risk for 30-day readmission. Diabet Med 30:e56–e62, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munoz M, Pronovost P, Dintzis J, Kemmerer T, Wang NY, Chang YT, Efird L, Berenholtz SM, Golden SH: Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt Comm J Qual Patient Saf 38:195–206, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parchman ML, Zeber JE, Palmer RF: Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med 8:410–417, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldberg PA, Bozzo JE, Thomas PG, Mesmer MM, Sakharova OV, Radford MJ, Inzucchi SE: “Glucometrics”: assessing the quality of inpatient glucose management. Diabetes Technol Ther 8:560–569, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Schnipper JL, Magee MF, Inzucchi SE, Magee MF, Larsen K, Maynard G: SHM Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts. J Hosp Med 3:66–75, 2008 [DOI] [PubMed] [Google Scholar]
- 22.Yale Center for Medical Informatics : Glucometrics: measuring inpatient glycemic control. Available from http://metrics.med.yale.edu. Accessed 10 December 2012
- 23.Anderson M, Zito D, Kongable G: Benchmarking glucose results through automation: the 2009 Remote Automated Laboratory System report. J Diabetes Sci Technol 4:1507–1513, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Society of Hospital Medicine : SHM glycemic control webinar: introducing the new web-based reporting engine for glucometrics. Available from http://www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement&template=/CustomSource/ondemand/12052012_SHM_Glycemic_Control_Program_Informational_Webinar.cfm. Accessed 20 February 2013
- 25.Johnson TP, Wislar JS: Response rates and non-response errors in surveys. JAMA 307:1805–1806, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Maynard GA, Budnitz TL, Nickel WK, Greenwald JL, Kerr KM, Miller JA, Resnic JN, Rogers KM, Schnipper JL, Stein JM, Whitcomb WF, Williams MV: Mentored implementation: building leaders and achieving results through a collaborative improvement model. 2011 John M. Eisenberg Patient Safety and Quality Award, National Level. Jt Comm J Qual Patient Saf 38:301–310, 2011 [DOI] [PubMed] [Google Scholar]