Abstract
Objective. The purpose of this study was to evaluate glycemic control as measured by A1C during a 2-year period after patients received diabetes self-management education (DSME).
Methods. Patients who completed DSME in 2009 and received medical follow-up with A1C measurements for at least 2 years after DSME were included in the evaluation. Primary endpoints were changes in A1C from before to immediately after, 1 year after, and 2 years after DSME. Secondary outcomes included the effects of the following factors on change in A1C: sex, duration of diabetes, uncontrolled diabetes (A1C ≥ 9%), health insurance coverage, and self-reported education level.
Results. Forty-three patients were included in the evaluation. Mean A1C before DSME was 10.2 ± 3.7%. Mean A1C after DSME was 7.8 ± 2.2% (P < 0.0001), a 23.5% reduction. Mean A1C at 1 and 2 years after DSME was 7.8 ± 2.1% for each year and remained unchanged from just after DSME to 1 and 2 years after DSME (P > 0.05). Patients with a duration of diabetes of < 1 year had a significantly greater reduction in mean A1C than those with a duration of diabetes ≥ 1 year (28.7 and 20.2%, respectively, P = 0.001).
Conclusion. DSME improved glycemic control to a substantial degree, and the effect was sustained for up to 2 years. Although the reduction in A1C was significant for all patients receiving DSME, there was a significantly greater reduction for patients who had a duration of diabetes of < 1 year than for those with a duration of diabetes > 1 year.
Diabetes and its complications are a significant health burden in the United States. According to the Centers for Disease Control and Prevention, ∼ 26 million people, or 8.3% of the U.S. population, are affected by diabetes.1 The lifetime risk of type 2 diabetes is now more than one in three in the general U.S. population.2 The American Diabetes Association (ADA) recommends that people with diabetes maintain an A1C of < 7% to prevent the complications associated with diabetes.3 To achieve this, the ADA recognizes diabetes self-management education (DSME) as crucial to the management of diabetes and improvement of patient outcomes.3 DSME, as defined by the National Standards for Diabetes Self-Management Education, is “the ongoing process of facilitating the knowledge, skill, and ability necessary for diabetes self-care.”4 This process, utilizing evidence-based standards and population-based medicine, incorporates the needs and life experiences of people with diabetes.
There are a multitude of methods for delivering diabetes education and teaching self-management skills. The Task Force for the National Standards of DSME does not endorse a particular education program or approach. One of the guiding principles identified by the task force recognizes that there is not a single best method. However, the principle does acknowledge that incorporating behavioral and psychosocial strategies demonstrates improved outcomes, as does incorporating culturally and age-appropriate strategies used in a group setting.4
A large number of studies, including randomized, controlled trials (RCTs), support the efficacy of DSME. Improved outcomes have been reported for educational interventions that occurred over extended periods of time and included follow-up support.3,5,6 A meta-analysis of 18 RCTs published between 1966 and 1999 found a significant decline of 0.43% in mean A1C at a median follow-up time of 6 months.7 By contrast, another meta-analysis of 31 RCTs published between 1980 and 1999 reported a mean A1C reduction of 0.76% immediately after education; however, this significant reduction was not sustained in the following 15 months (0.26% reduction).8 To examine as broadly as possible the efficacy of DSME, both of these meta-analyses included interventions in all settings. Interventions varied by provider type (e.g., physicians, nurses, dietitians, and pharmacists), individual or group-based education, duration, and intensity. A third review of 11 studies from 1988 to 2002 involving 1,532 patients assessed the effects of group-based training in people with type 2 diabetes from 4 to 24 months after the educational intervention. The results were significant A1C reductions of 1.4% at 4-6 months, 0.8% at 12-14 months in 6 trials, and 1% at 2 years in 1 trial.9 Another study demonstrated a 0.5% improvement in A1C at 12 months, which was sustained at 36 months in the more intensive education group.6
Although diabetes education is recognized as being effective, there is limited information about the maintenance of improved glycemic control over time after education. This maintenance of control is essential in preventing devastating long-term complications of diabetes. Some studies have suggested that ongoing educational reinforcement may be needed to sustain control.5,10,11 However, it is unclear whether additional education would be beneficial and, if so, at what time points. Thus, the purpose of this study was to evaluate glycemic control as measured by A1C during a 2-year period after patients received DSME.
Patients and Methods
A retrospective evaluation of patients attending DSME in 2009 was approved by the University of Tennessee Health Science Center institutional review board and Regional One Health. The requirement for informed consent was waived. The DSME program is located in the outpatient center of Regional One Health and is recognized by the ADA. Education is provided in two class sessions for a total of 10 hours of instruction. This comprehensive program incorporates the American Association of Diabetes Educators' AADE7 Self-Care Behaviors,3 which include healthy eating, being active, monitoring blood glucose, taking medication, problem-solving, reducing risks, and healthy coping. The diabetes education team is multidisciplinary, consisting of pharmacists, a nurse, and a dietitian.
Patients who attended DSME in 2009 were identified through an electronic diabetes education database. Only patients who completed DSME in 2009 and received medical follow-up and A1C measurements for at least 2 years after DSME were included. Medical management, including medications, during the 2-year period was at the discretion of the treating physician, although care was relatively consistent in this group practice model. Baseline demographic information, self-reported education level, health insurance coverage, duration of diabetes, and A1C values before, immediately after, and 1 and 2 years after DSME were collected. Pre-DSME A1C values were defined as being obtained within 3 months before DSME. Immediately post-DSME A1C values were defined as being obtained within 4-to 6 months after attending the DSME program. The primary endpoints were the changes in A1C from before to immediately after, 1 year after, and 2 years after DSME. The number of patients who achieved an A1C treatment goal of < 7% before DSME and throughout the study period was evaluated. Secondary outcomes included the effects of the following factors on the change in A1C: sex, duration of diabetes, uncontrolled diabetes (A1C ≥ 9%), health insurance coverage, and self-reported education level.
SAS 9.3 (SAS Institute, Cary, N.C.) was used for data and statistical analyses. Repeated-measures analysis of variance was used to evaluate differences in A1C during the study period and a paired t test was used to determine significance between time points. The Bonferroni correction was applied to adjust for multiple comparisons. Participants were stratified into two groups based on duration of diabetes defined as diagnosis < 1 year and ≥ 1 year. The participants were further analyzed for differences in sex, self-reported education level, health insurance coverage, uncontrolled diabetes at baseline, and attainment and maintenance of the A1C treatment goal of < 7%. A χ2 test was used for categorical data in the subgroup analyses. Unless otherwise stated, P < 0.05 was considered statistically significant.
Study Results
A total of 133 patients attended DSME in 2009. Ninety-two (69%) had pre- and post-DSME A1C measurements. Sixty-three of the 92 patients (68%) returned for medical follow-up and had an A1C measured 1 year after DSME. Forty-three of the 63 patients (68%) returned for medical follow-up and had an A1C measured at both 1 and 2 years after DSME. These 43 patients became the final study population evaluated.
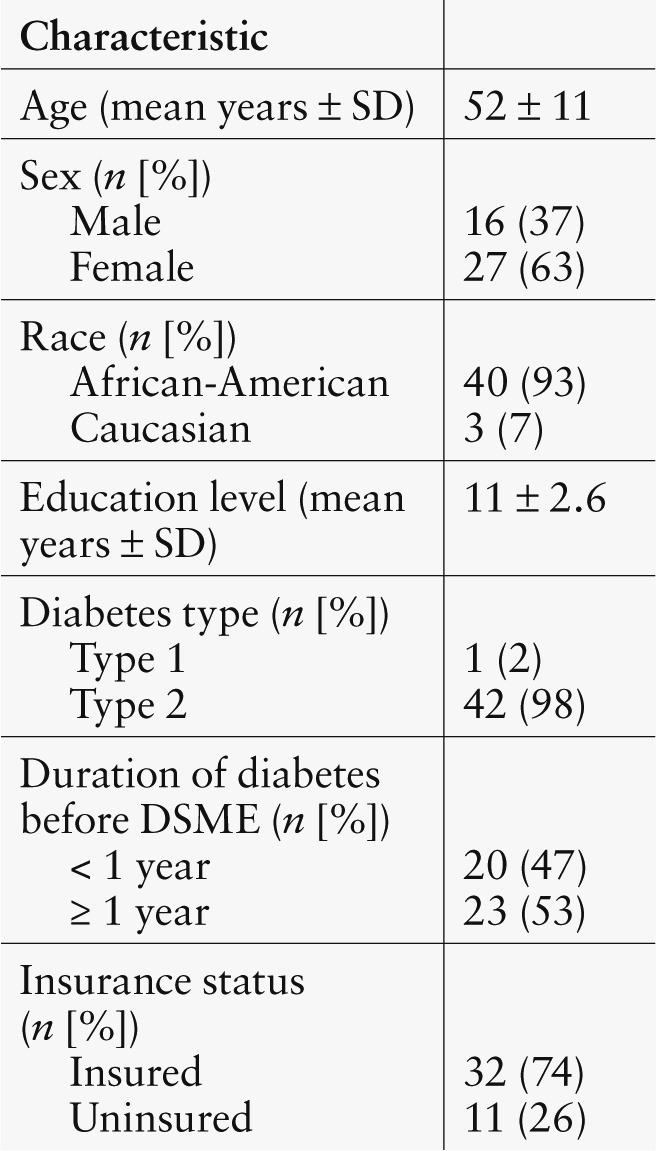
Demographic characteristics are outlined in Table 1. The majority of patients were African-American women with type 2 diabetes. Patients were generally > 50 years of age and had health insurance.
Table 1.
Baseline Patient Characteristics (n = 43)
For the overall group, mean A1C before DSME was 10.2 ± 3.7%, which decreased to 7.8 ± 2.2% immediately after the DSME program (P < 0.0001). This represented a 23.5% A1C reduction (decrease of 2.4 ± 3.3) from the pre-DSME A1C. Mean A1C 1 and 2 years after the DSME program were 7.8 ± 2.1% for each year and remained unchanged from immediately after the DSME program to 1 and 2 years after (P = NS).
Subgroup analysis of the change in mean A1C throughout the study period is shown in Table 2. Patients were stratified by their duration of diabetes. Patients with diabetes for ≥ 1 year had a higher pre-DSME A1C than those with a diabetes duration of < 1 year (10.9 ± 4.0 vs. 9.4 ± 3.2%). However, this was not statistically significant. Mean A1C immediately after the DSME program was 8.7 ± 2.4% for patients with diabetes ≥ 1 year compared to 6.7 ± 1.3% for patients with a diabetes duration of < 1 year.
Table 2.
Mean A1C Before, Immediately After, 1 Year After, and 2 Years After DSME
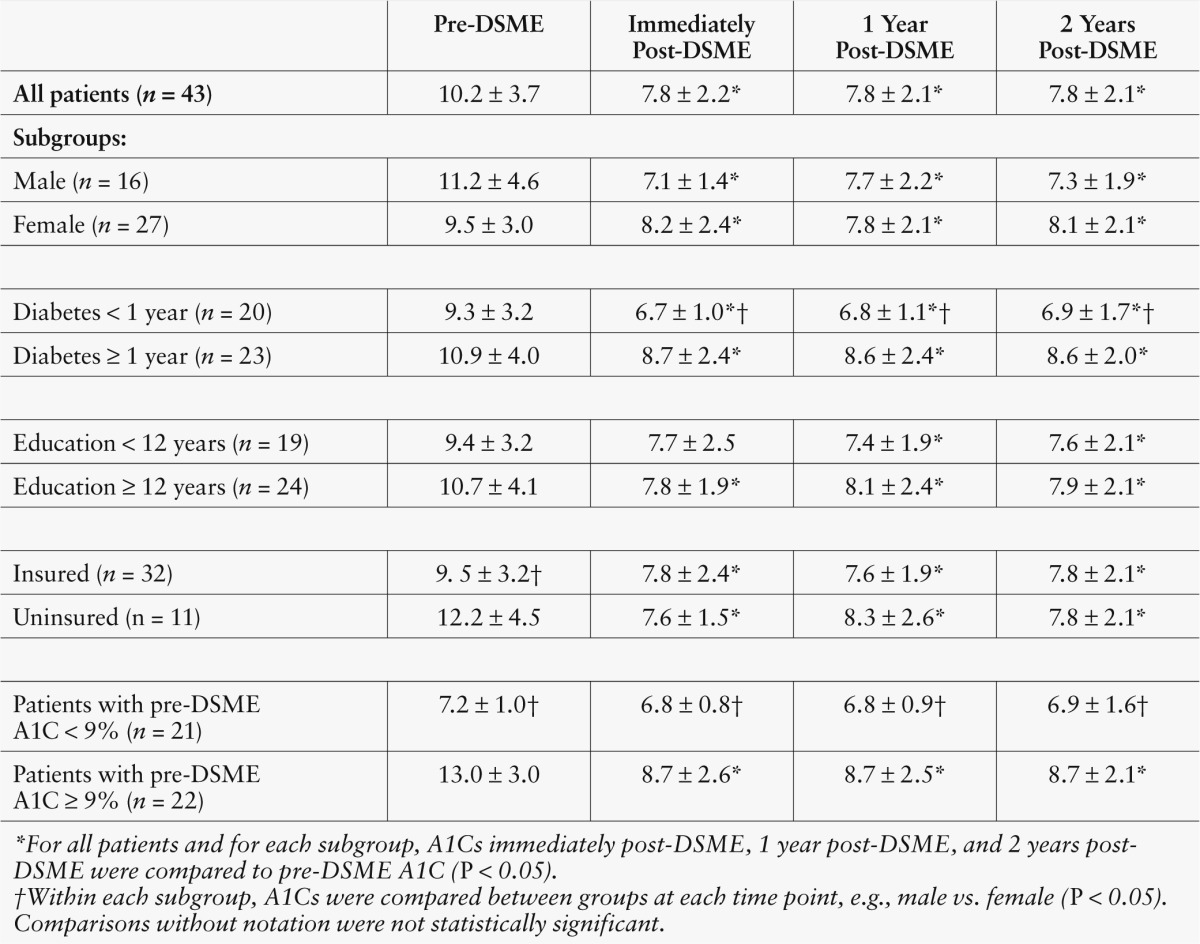
There was a significantly greater reduction in A1C for patients with diabetes < 1 year, with a mean decrease in A1C of 2.7 percentage points (28.7% decrease) compared to 2.2 percentage points (20.2% decrease) with diabetes ≥ 1 year (P = 0.001). These reductions in mean A1C remained constant for the following 2 years but were significantly lower in patients with diabetes < 1 year (P = 0.004).
Patients were stratified by a pre-DSME A1C < 9% or ≥ 9%. Patients with a pre-DSME A1C ≥ 9% had a larger reduction in mean A1C immediately after DSME from 13.0 ± 3.0 to 8.7 ± 2.6% (P < 0.0001). This represents a 33.1% reduction. Patients with a pre-DSME A1C < 9% had a smaller decrease in mean A1C immediately after DSME from 7.2 ± 1.0 to 6.8 ± 0.8% (a reduction of 5.6%, P = NS). Mean A1C at 1 and 2 years after DSME, although similar to A1C levels immediately after DSME in both groups, remained significantly higher in patients whose A1C was ≥ 9% at baseline (P ≤ 0.0001).
There were no differences with regard to sex or self-reported educational level in the change in mean A1C during the study period. Mean pre-DSME A1C was significantly higher in patients without health insurance coverage (12.2 ± 4.5%) than in those with health insurance (9.5 ± 3.2%, P = 0.0323), but both groups experienced significant reductions in A1C immediately after DSME (7.6 ± 1.5 and 7.3 ± 2.4%, respectively, P ≤ 0.0001).
Only nine patients (21%) had achieved the ADA-recommended A1C goal of < 7% before DSME. This increased to 21 patients (49%) immediately after DSME and remained constant at 20 patients (47%) and 19 patients (44%) over the next 2 years (P = 0.03).
Discussion
Although other studies have confirmed the benefit of DSME on initial diabetes control, this study was conducted because previous publications had not definitively established the sustainability of DSME in improving glycemic control during an extended period. In two small studies, A1C reductions of 0.5–1% at 2–3 years were demonstrated, but benefit at 3 years was only attained in the intensive intervention group.6,9
Our findings indicate that a comprehensive, multidisciplinary DSME program significantly improved glycemic control by achieving a 23.5% reduction in A1C from 10.2% before DSME to 7.8% through the remainder of the study period. At the study conclusion, nearly one-half of patients were at the goal A1C of < 7%. Importantly, the majority of patients maintained A1C improvement for 2 years after DSME. Patient groups with a diabetes duration of < 1 year and ≥ 1 year both had significant improvements in A1C after DSME. Although patients with diabetes for ≥ 1 year maintained their post-DSME A1C improvements, their post-intervention A1C was not at goal (< 7%). By contrast, the group with diabetes for < 1 year maintained improved glycemic control and consistently met the goal A1C of < 7% after education. These results suggest that, despite attainment of similar A1C reductions in patients with a baseline A1C ≥ 9%, this group may need ongoing interventions to ensure that their self-management strategies will continue and result in an ongoing A1C decline to meet a goal A1C of < 7%. Our results also suggest that earlier education interventions have a long-term impact in helping patients control their diabetes and attain a goal A1C of < 7%.
The most recent estimates from the National Health and Nutrition Examination Survey indicate that ∼ 53% of adults achieve an A1C of < 7%.12 The patient population that maintained follow-up through the study period nearly met the national average after DSME. Before diabetes education, only 21% of patients in the study had an A1C at the goal of < 7%; this number increased to 49% after education.
The significant improvement in mean A1C of 2.4 ± 3.3% seen throughout the study is a much greater improvement than the results found in earlier meta-analyses and reviews.7-9 This reduction reaches a noteworthy threshold for diabetes care, but the results may have limited external validity. The high attrition rate may have produced biased results. Patient demographics changed from baseline to the end of the 2-year study period as the sample size decreased by 53%. Although these changes were not statistically significant, a greater number of female patients with health insurance maintained follow-up throughout the study period. The 43 patients who maintained follow-up might represent patients who are more likely to meet disease goals from the outset. The high attrition rate could be the result of multiple factors, including moving from the geographical area, changes in health care providers, nonadherence, or changes in health insurance coverage.
The benefits of A1C reduction have been well established in people with type 2 diabetes, who are at elevated risk for a number of serious health problems. The U.K. Prospective Diabetes Study demonstrated that a 1% reduction in A1C was associated with a 21% decrease in diabetes-related endpoints, an 18% decrease in combined fatal and nonfatal myocardial infarction, a 12% decrease in stroke, a 37% decrease in microvascular endpoints, a 25% reduction in diabetes-related deaths, and a 7% reduction in all-cause mortality.13 The magnitude of the A1C reduction in this study suggests the possibility of similar benefits over time. Our individualized, focused DSME program attained remarkable results demonstrating sustained efficacy.
Conclusion
DSME improved glycemic control to a substantial degree, and the effect was sustained for up to 2 years. Before undertaking this study, there was a question as to whether patients reach a time point beyond diabetes education at which they begin to lose the maximal benefits of DSME and would gain from additional education or a refresher course. It appears that patients who were diagnosed with diabetes for ≥ 1 year before DSME do not have as significant a reduction in A1C as patients with diabetes for < 1 year, and their A1C remained higher for 2 years. These patients may benefit from additional education.
References
- 1.Centers for Disease Control and Prevention : National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, Ga, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 2.Gregg EW: Are children in the future of type 2 diabetes prevention? N Engl J Med 362:548–550, 2010 [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association : Standards of medical care in diabetes-2013. Diabetes Care 36 (Suppl. 1):S11–S66, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, Siminerio LM, Weinger K, Weiss MA: National standards for diabetes self-management education. Diabetes Care 35 (Suppl. 1):S101–S108, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polonsky WH, Earles J, Smith S, Pease DJ, Macmillan M, Christensen R, Taylor T, Dickert J, Jackson RA: Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care 26:3048–3053, 2003 [DOI] [PubMed] [Google Scholar]
- 6.Piatt GA, Anderson RM, Brooks MM, Songer T, Siminerio LM, Korytkowski MM, Zgibor JC: 3-year follow-up of clinical and behavioral improvements following a multifaceted diabetes care intervention: results of a randomized controlled trial. Diabetes Educ 36:301–309, 2010 [DOI] [PubMed] [Google Scholar]
- 7.Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL: Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ 29:488–501, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM: Self-management education for adults with type 2 diabetes. Diabetes Care 25:1159–1171, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Deakin TA, McShane CE, Cade JE, Williams R: Group based training for self-management strategies in people with type 2 diabetes mellitus [Review]. Cochrane Database Syst Rev 2005:CD003417. [DOI] [PubMed] [Google Scholar]
- 10.Sperl-Hillen J, Beaton S, Fernandes O, Von Worley A, Vazquez-Benitez G, Hanson A, Lavin-Tompkins J, Parsons W, Adams K, Spain CV: Are benefits from diabetes self-management education sustained? Am J Manag Care 19:104–112, 2013 [PubMed] [Google Scholar]
- 11.Tang TS, Funnell MM, Brown MB, Kurlander JE: Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ Couns 79:178–184, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics, Division of Health Interview Statistics : Crude and Age-Adjusted Percentage of Civilian, Noninstitutionalized Adults with Diagnosed Diabetes, United States, 1980-2010. Atlanta, Ga, Centers for Disease Control and Prevention, Division of Diabetes Translation, 2012 [Google Scholar]
- 13.U.K. Prospective Diabetes Study Group : Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321:405–412, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]


