Abstract
In Brief
Hyperglycemia in the hospital setting affects 38-46% of noncritically ill hospitalized patients. Evidence from observational studies indicates that inpatient hyperglycemia, in patients with and without diabetes, is associated with increased risks of complications and mortality. Substantial evidence indicates that correction of hyperglycemia through insulin administration reduces hospital complications and mortality in critically ill patients, as well as in general medicine and surgery patients. This article provides a review of the evidence on the different therapies available for hyperglycemia management in noncritically ill hospitalized patients.
Recent studies and meta-analyses have shown that intensive insulin therapy is associated with an increased risk of hypoglycemia,1–3 which has been independently associated with increased morbidity and mortality in hospitalized patients.4 Thus, although insulin therapy is recommended for hyperglycemia management in hospitalized patients,5,6 concerns about hypoglycemia have led to the search for alternative treatment options such as incretin-based therapy.7,8 Incretin agents stimulate insulin secretion in a glucose-dependent manner; thus, the risk of hypoglycemia is minimal when used as monotherapy. In addition, incretin therapy may result in metabolic and cardiovascular benefits, including reduced inflammation and oxidative stress.9,10
Substantial evidence indicates that correction of hyperglycemia through insulin administration reduces hospital complications and mortality in critically ill patients, as well as in general medicine and surgery patients.5,11–15 Animal and human studies have shown multiple beneficial effects of insulin administration during acute stress and illness.16–18 Insulin administration results in a rapid, dose-dependent reduction in endogenous (hepatic) glucose production, improvement of insulin resistance, enhancement of energy delivery to peripheral tissues, and normalization of endothelium-dependent vasodilation.19,20 In addition, insulin has potent anti-inflammatory properties, inhibiting production of tumor necrosis factor-alpha (TNF-α), reactive oxygen species (ROS), intracellular adhesion molecule-1 in macrophages and leukocytes, and suppression of the proinflammatory nuclear factor kappa B (NF- B).16,21
This article provides a review of the evidence on the different therapies available for hyperglycemia management in noncritically ill hospitalized patients.
Insulin Therapy in the Hospital
The positive effects of insulin administration include correction of hyperglycemia, as well as anti-inflammatory, vasodilatory, and antioxidant effects and inhibition of lipolysis and platelet aggregation.16–18,21 Hyperglycemia is associated with impaired leukocyte function, including decreased phagocytosis, impaired bacterial killing, and chemotaxis, which can increase the number of hospital infections.22 Hyperglycemia has also been shown to impair collagen synthesis and to impair wound-healing in patients with poorly controlled diabetes.23 In addition, acute hyperglycemia results in NF-κB activation and production of inflammatory cytokines such as TNF-α; interleukin-6 (IL-6); plasminogen activator inhibitior-1, which causes increased vascular permeability; and leukocyte and platelet activation resulting in an inflammatory and pro-thrombotic state.24 Several studies have reported rapid improvement in high levels of inflammatory and oxidative stress markers after insulin administration and correction of hyperglycemia, although these levels remained higher than those of control subjects without diabetes.25
No single insulin regimen meets the needs of all patients with hyperglycemia. Scheduled subcutaneous insulin therapy with basal or intermediate-acting insulin given once or twice per day in combination with short- or rapid-acting insulin administered before meals is the preferred strategy for glycemic management in noncritically ill patients.5,26 Subcutaneous insulin regimens should address the three components of a patient's total insulin requirement: basal (what is required in the fasting state), nutritional (what is required to dispose of glucose contained in nutrition), and correctional or supplemental (what is required to correct for glucose elevations caused by changes in insulin requirements).26
The practice of discontinuing oral diabetes medications and/or existing insulin therapy and starting sliding-scale insulin (SSI) results in undesirable levels of hypoglycemia and hyperglycemia.27,28 SSI insulin regimens involve the administration of regular or rapid-acting insulin before meals or every 4-6 hours if patients are on NPO (nothing by mouth) status to correct hyperglycemia. Although straightforward and easy to use, SSI regimens are fraught with challenges, including inadequate coverage of glycemic excursions and insulin stacking (accumulation of insulin in subcutaneous tissues).29 We previously reported the results of a prospective, randomized, multicenter trial comparing the efficacy and safety of a basal-bolus insulin regimen to that of SSI in inpatients with type 2 diabetes admitted to general medicine and surgery wards.30 We found that, among 130 insulin-naive patients with an admission blood glucose level between 140 and 400 mg/dl, the use of a basal-bolus insulin regimen led to greater improvement in blood glucose control than SSI alone. A blood glucose target of < 140 mg/dl was achieved in 66% of patients in the glargine-plus-glulisine basal-bolus group and 38% of the SSI group. One-fifth of patients treated with an SSI protocol without a basal component had persistently elevated blood glucose levels > 240 mg/dl during their hospital stay. The incidence of hypoglycemia, defined in this study as a blood glucose level < 60 mg/dl, was low (3%) and was not different between groups.
In general surgery patients, the RABBIT 2 Surgery (Randomized Study of Basal Bolus Insulin Therapy in the Inpatient Management of Patients with Type 2 Diabetes Undergoing General Surgery) trial12 compared the efficacy and safety of a basal-bolus regimen to that of SSI in 211 patients with type 2 diabetes. Study outcomes included differences in daily glucose levels and a composite of postoperative complications, including wound infection, pneumonia, respiratory failure, acute renal failure, and bacteremia. Patients were randomized to receive a basal-bolus regimen with glargine once daily and glulisine before meals at a starting dose of 0.5 units/kg or to receive SSI four times daily for glucose > 140 mg/dl. The basal-bolus regimen resulted in significant improvement in glucose control and a significant reduction in the frequency of the composite of hospital complications. The results of these trials indicate that a basal-bolus regimen is preferred to SSI and results in improved glycemic control and lower rates of hospital complications in general medical and surgical inpatients with type 2 diabetes.
The DEAN (Insulin Detemir Versus NPH Insulin in Hospitalized Patients With Diabetes) trial, an open-label, controlled, multicenter trial, randomly assigned 130 medical patients with type 2 diabetes to receive either detemir once daily and aspart before meals or NPH and regular insulin twice daily.31 Both regimens resulted in significant improvements in inpatient glycemic control, with a glucose target of < 140 mg/dl before meals achieved in 45% in the detemir/aspart group and in 48% of NPH/regular insulin group. Hypoglycemia (< 60 mg/dl) was observed in approximately one-fourth of patients treated with detemir/aspart and NPH/regular insulin during the hospital stay. There was no difference in length of hospital stay or mortality between groups. Thus, a similar improvement in glycemic control can be achieved with basal-bolus therapy with detemir/aspart or with NPH/regular insulin in general medicine patients with type 2 diabetes.
In insulin-naive patients, initial total daily insulin doses have varied widely in different protocols from 0.3 to 1.5 units/kg/day.30,32–34 However, only doses of 0.4 and 0.5 units/kg/day have been studied prospectively.12,30 A case-control analysis of 1,990 patients with diabetes reported that insulin doses > 0.6 units/kg/day were associated with higher odds of hypoglycemia than doses < 0.2 units/kg/day, independent of the types of insulin used.35 In addition, higher rates of hypoglycemia have been seen with increasing age and in patients with impaired renal function. A recent, randomized trial compared the efficacy of basal-bolus regimens at 0.5 and 0.25 units/kg/day in patients with diabetes with moderate renal failure and a glomerular filtration rate (GFR) < 45 ml/min. There were no differences in mean daily glucose concentration, but those in the higher-dose insulin group had twice the rate of hypoglycemia (30 vs. 15.8%) during their hospital stay.36 Thus, lower initial daily doses (0.25-0.3 units/kg/day) should be used in patients with moderate renal failure who are at risk of hypoglycemia.
The recently reported Basal Plus trial37 recruited 375 patients with type 2 diabetes treated with diet, oral antidiabetic agents, or low-dose insulin (≤ 0.4 unit/kg/day) to receive a basal-bolus regimen with glargine once daily and glulisine before meals, a “basal-plus” regimen with glargine once daily and supplemental doses of glulisine for correction of hyperglycemia (> 140 mg/dl) per a sliding scale, and SSI. This trial reported that the basal-plus regimen resulted in improvements in glycemic control and frequency of hypoglycemia that were similar to those of the standard basal-bolus regimen. In addition, treatment with basal-bolus and basal-plus regimens resulted in fewer treatment failures than treatment with SSI. Thus, in insulin-naive patients or in those receiving low-dose insulin on admission (< 0.4 units/kg/day), as well as in patients with reduced oral intake, a basal-plus regimen is an effective alternative to basal-bolus insulin. Patients with persistent hyperglycemia or with regular caloric intake could be moved up from basal-plus to a basal-bolus regimen if needed.
Nonglycemic Effects of Insulin
Hyperglycemia in the hospital setting affects 38-46% of noncritically ill hospitalized patients.38,39 Evidence from observational studies, including our own, indicates that hospital hyperglycemia in patients with and without diabetes is associated with increased risks of complications and mortality, longer hospital stays, higher admission rates to the intensive care unit (ICU), and a greater need for transitional or nursing home care after hospital discharge38,40,41 The mechanisms implicated in the detrimental effects of hyperglycemia during acute illness are not completely understood. Current evidence indicates that hyperglycemia results in impaired neutrophil granulocyte function, overproduction of ROS, circulating free fatty acids, inflammatory mediators that can result in direct cellular damage, and vascular and immune dysfunction.32
Several intervention studies and meta-analyses have reported that intensive insulin therapy, defined as the use of intravenous (IV) insulin infusion protocols to achieve strict glycemic control, improves clinical outcomes in surgical ICU patients but not in medical or mixed ICU settings.2 A recent meta-analysis of seven randomized, controlled studies found that intensive insulin therapy during or after cardiac surgery reduced mortality in the ICU, postsurgical atrial fibrillation, use of epicardial pacing, duration of mechanical ventilation, and length of ICU stay.42 Recent studies of mediators of inflammation have also shown that insulin exerts anti-inflammatory, antithrombotic, and anti-atherogenic effects.43 Insulin counteracts many of the detrimental effects of hyperglycemia, including free radical formation, oxidative stress, apoptotic cell death, and increased levels of proinflammatory cytokines.44 Additionally, insulin has been shown to increase cardiac contractility and coronary vasodilation and to preserve endothelial function.45 The antioxidant and anti-inflammatory effects of insulin are mediated through a number of pathways. Insulin inhibits NF-κB, which is at the center of many proinflammatory pathways, thereby affecting a range of downstream events. Inhibition of mitogen-activated protein kinase suppresses IL-6 signaling, whereas inhibition of c-Jun N-terminal kinase mediates inflammatory processes downstream of TNF-α. TNF-α itself is suppressed via phosphatidyl-inositol 3-kinase-AKT-mediated activation of endothelial nitric oxide synthase.43 Taken together, these findings suggest a cardiac-specific mechanism that may contribute to improved clinical outcomes in insulin-treated patients with hyperglycemia.
Inpatient Hypoglycemia With Insulin Therapy
Although insulin therapy is the standard of care in hospitals, it is a source of medication errors and increased risk of hypoglycemia. An analysis of medication errors between 2006 and 2008 revealed that insulin was the drug with the greatest number of medication errors in hospitals.46 Hypoglycemia in the hospital has been associated with adverse cardiovascular outcomes such as prolonged QT intervals, ischemic electrocardiogram changes/angina, arrhythmias, sudden death, and increased inflammation.47,48 In addition, insulin-induced hypoglycemia is associated with increases in C-reactive protein and pro-inflammatory cytokines (TNF-α, interleukin-1β, IL-6, and interleukin-8), markers of lipid peroxidation, ROS, and leukocytosis.49,50
In non-ICU settings, hypoglycemia has been associated with increased lengths of hospital stay, greater costs of hospitalization, and higher mortality both during hospitalization and after discharge.51,52 Observational studies have demonstrated a J-shaped relationship between inpatient glycemic control and mortality, with increased risk of death at both the high and low extremes of dysglycemia.53 Most of these studies reported that inpatient mortality risk is greater in patients with spontaneous hypoglycemia than in those with insulin-associated hypoglycemia.53–55 This suggests that spontaneous hypoglycemia may be a marker of disease burden instead of a direct cause of mortality.
Use of Oral Agents in the Hospital Setting
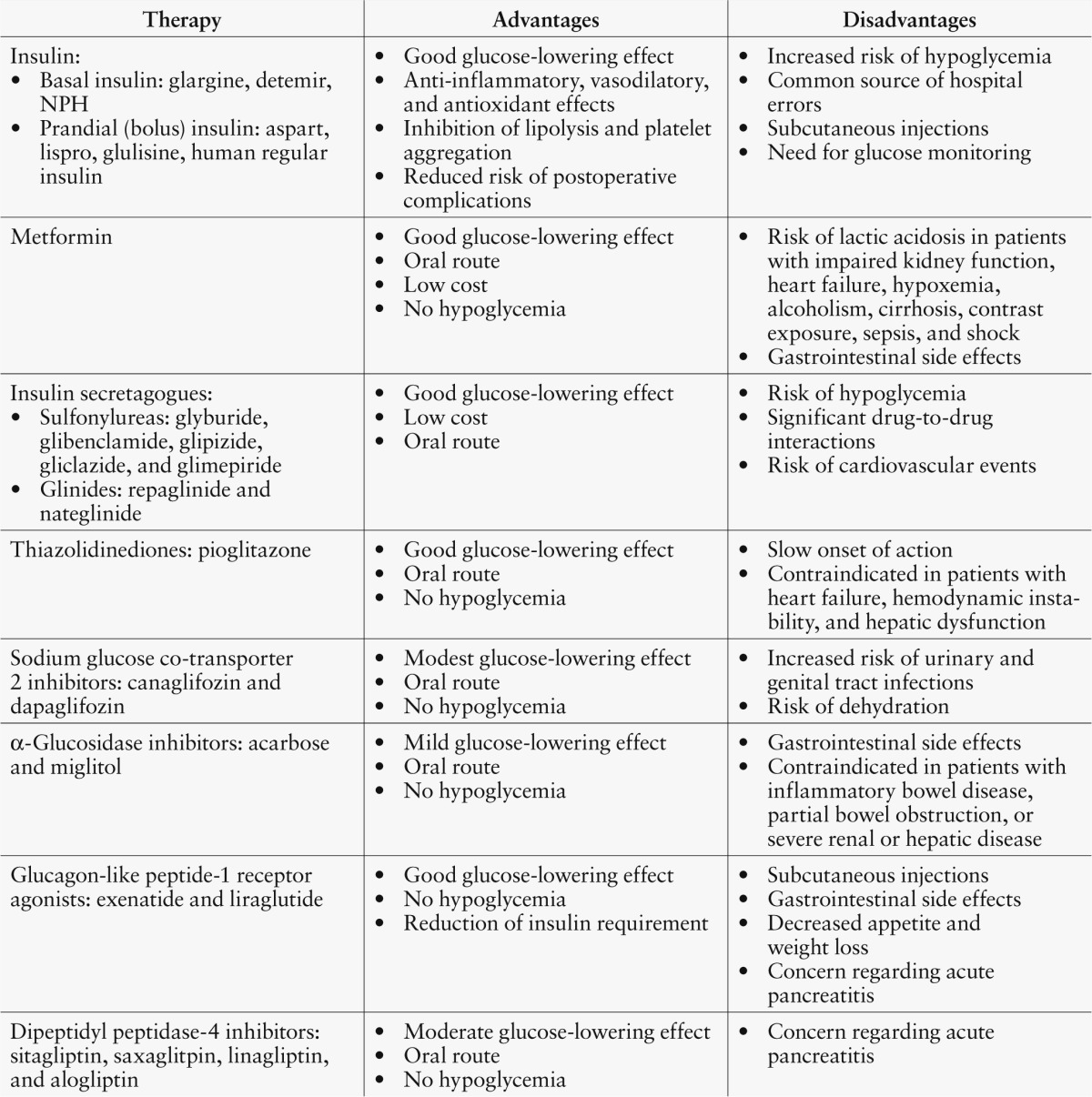
The use of oral antidiabetic agents is not recommended in hospitals because few data are available regarding their safety and efficacy in the inpatient setting. Major limitations to the use of oral agents in the hospital include their side effect profiles and slow onset of action, which does not allow for rapid attainment of glycemic control or dose adjustments to meet the changing needs of acutely ill patients.5,6 Table 1 depicts the advantages and disadvantages of available antidiabetic drugs compared to insulin therapy for the inpatient management of hyperglycemia in noncritical care settings.
Table 1.
Advantages and Disadvantages of Antidiabetic Drugs for the Inpatient Management of Hyperglycemia in Noncritical Care Settings
Metformin therapy
Metformin is the most commonly prescribed glucose-lowering agent for the outpatient treatment of type 2 diabetes.56 Despite a lack of randomized studies on its safety and efficacy in hospitals, metformin is also commonly used in the inpatient setting,57,58 and it is estimated that up to one-fourth of hospitalized patients with type 2 diabetes in the United States are treated with metformin, even in the presence of contraindications.59 Metformin exerts its antidiabetic effect by suppressing excessive hepatic glucose production through a reduction in gluconeogenesis.60 Metformin might also increase glucose utilization in peripheral tissues and possibly reduces food intake and intestinal glucose absorption, resulting in weight loss.61 Because metformin does not stimulate endogenous insulin secretion, it does not cause hypoglycemia when used as monotherapy.62 Gastrointestinal discomfort in the form of abdominal pain, flatulence, and diarrhea occurs in ∼ 25% of patients taking metformin.63
Metformin has been reported to increase the risk of lactic acidosis. The estimated rate of lactic acidosis in patients receiving metformin is of 2-5 cases per 100,000 patient-years, which is similar to that reported for patients with diabetes who do not take metformin.64,65 A 2010 Cochrane systematic review reported no increase in the number of cases of lactic acidosis in ambulatory patients across 347 clinical trials with 70,490 patient-years of metformin use.58 Patients with diabetes, however, are at increased risk of developing lactic acidosis if safety guidelines are ignored and if the drug is continued in the presence of contraindications.66 Impaired kidney function, decompensated heart failure, hypoxemia, alcoholism, cirrhosis, contrast dye exposure, sepsis, and shock are associated with an increased risk of lactic acidosis and are absolute contraindications to the use of metformin therapy.58,67 The importance of adhering to safety recommendations for metformin was illustrated by Pasquel et al.,66 who recently reported a series of cases of metformin-induced lactic acidosis when the drug was prescribed in the hospital despite the presence of contraindications.
Insulin secretagogues (sulfonylureas and glinides)
Sulfonylureas are the second most commonly prescribed antidiabetic agents in patients with type 2 diabetes. Insulin secretagogues exert their antidiabetic effect by stimulating endogenous insulin production.67 The insulinotropic effect of these medications is exerted through binding to a receptor-like structure in the β-cell surface and closing of the ATP-dependent potassium channels in the β-cell membrane.68,69 This results in depolarization of the cell, influx of calcium, and subsequent stimulation of insulin secretion.70 In the outpatient setting, sulfonylureas have proven to be effective in improving glucose control, with an A1C reduction of 1-2 percentage points, and in reducing microvascular complications.71,72 However, sulfonylureas increase the risk of hypoglycemia, especially in elderly patients and in those with impaired renal function or poor oral intake.70 In addition, there is concern that sulfonylureas may worsen cardiac and cerebral ischemia73,74 by inhibiting ATP-sensitive potassium channels, resulting in cell membrane depolarization and increased intracellular calcium concentration.75
Use of sulfonylureas in the inpatient setting is discouraged because of the potential risk of hypoglycemia secondary to long duration of action and variable meal availability in the inpatient setting.5,6 Results of a nested case-control study composed of hospitalized patients who received a sulfonylurea as part of their inpatient regimen reported a prevalence of hypoglycemia in 130 of 692 (19%) of patients.76 Hypoglycemia was highest with the use of glyburide (22%), followed by glimepiride (19%), and glipizide (16%), especially in patients > 65 years of age and with a GFR < 30 ml/min.76
Significant drug-to-drug interactions have also been described with the use of sulfonylureas in hospitalized patients. The use of sulfonylureas in patients receiving fluoroquinolone antibiotics increases the risk of hypoglycemia.77 Additionally, drugs that inhibit hepatic cytochrome CYP2C9, including metronidazole, fluconazole, amiodarone, miconazole, trimethoprim-sulphamethoxazole, valproate, and gemfibrozil, can also exaggerate the effect of sulfonylureas, thereby increasing the risk of hypoglycemia.78
Glinides available in the United States include repaglinide and nateglinide. Repaglinide and nateglinide enhance β-cell insulin production but differ from sulfonylureas in receptor affinity, binding sites, and absorption and elimination rates.79 These differences result in faster onset and shorter duration of action, offering the advantage of better postprandial insulin response.80 A retrospective review of hospitalized patients treated with repaglinide or nateglinide indicated a rate of hypoglycemia of 7%, similar to that reported with insulin therapy in the inpatient setting.81 These agents are not recommended in the inpatient setting because of the potential risk of hypoglycemia and lack of randomized trials evaluating their safety and efficacy in the inpatient management of hyperglycemia.
Thiazolidinedione therapy
Pioglitazone is the only thiazolidinedione (TZD) widely available for clinical use in the United States. Pioglitazone is an insulin sensitizer and exerts its glucose-lowering effect through direct activation of the peroxisome proliferator-activated receptor γ.82 TZDs are highly effective in improving glycemic control, with an average A1C reduction of 1-2 percentage points.83 However, the time needed to reach its maximal antihyperglycemic effect can be up to 12 weeks, which makes it a less attractive agent for inpatient management of diabetes and hyperglycemia.5 In addition, TZD therapy is associated with fluid retention leading to edema, especially when used in combination with insulin, and worsening heart failure in some individuals.32,84 TZDs are contraindicated in patients with congestive heart failure, hemodynamic instability, or evidence of hepatic dysfunction.67
Sodium glucose co-transporter 2 inhibitors
Sodium glucose co-transporter 2 (SGLT-2) inhibitors are a new class of oral antidiabetic medications that increase urinary glucose excretion by reducing renal glucose reabsorption in the proximal convoluted tubules.85 Canaglifozin and dapaglifozin are the two available drugs approved by the U.S. Food and Drug Administration for management of type 2 diabetes.86,87 Both agents are effective in reducing A1C by ∼ 0.6-0.8%, with a low risk of hypoglycemia.88 The use of SGLT-2 inhibitors, however, has been associated with an increased risk of urinary and genital tract infections compared to placebo (odds ratio 1.34-3.50, respectively).88 In addition, because of their glycosuric effects, dehydration and hypotension have been reported.89 The potential side effects of SGLT-2 inhibitors make their use less attractive for inpatient management.
α-Glucosidase inhibitors
Acarbose and miglitol, both α-glucosidase inhibitors (AGIs), decrease blood glucose by delaying the breakdown of carbohydrates in the gut and thus slowing the absorption of sugars. Although AGIs can significantly reduce postprandial glucose excursions with a low risk of hypoglycemia, the increased delivery of carbohydrates to the colon commonly results in increased gas production and gastrointestinal symptoms.90 These agents are not recommended for use in the inpatient setting because of their mild antihyperglycemic effect, with most reports showing an A1C reduction of ∼ 0.5% and minimal reduction in fasting plasma glucose.83 AGIs are contraindicated in patients with gastrointestinal diseases such as inflammatory bowel disease, partial bowel obstruction, or severe renal or hepatic disease. In addition, intolerance to these agents is common and affects 25-45% of patients.83
Incretin-based therapies
Two distinct classes of incretin-based therapies are available in the United States: glucagon-like peptide-1 (GLP-1) receptor agonists (i.e., exenatide and liraglutide) and the dipeptidyl peptidase-4 (DPP-4) inhibitors (i.e., sitagliptin, saxagliptin, alogliptin, and linagliptin).67 The benefits and potential risks of incretin-based therapies in hospitalized patients have been reviewed elsewhere.7,8,91,92 Although agents in both classes are well tolerated, the oral administration of DPP-4 inhibitors (as opposed to injectable GLP-1 receptor agonists) might be preferred for patients who are able to take oral medications. The efficacy and safety of incretin-based therapies in hospitalized patients has not been fully determined. However, the potential metabolic and cardiovascular benefits and the low risk of hypoglycemia of these agents make them an attractive possibility for inpatient management of diabetes.
In the hospital setting, the use of native GLP-1 infusion has been shown effective in improving the glycemic response after meals or enteral nutrition similar to insulin administration and also reduces exogenous insulin requirements.93–97 The perioperative administration of exenatide has been shown to improve glucose levels in patients with diabetes undergoing general surgery.98 In addition, exenatide effectively lowered glucose levels when given as an IV infusion for 48 hours to patients with diabetes who were admitted to a cardiac ICU.99 Moreover, the infusion of native GLP-1 has been reported to improve left ventricular function and cardiac functional status in patients with severe heart failure.100 The fact that these beneficial effects occurred in patients with or without diabetes supports a GLP-1 effect on the heart independent of glycemic control. GLP-1 receptor agonist therapy, however, is frequently associated with gastrointestinal side effects and decreased food intake, which could be undesirable in most hospitalized patients. In addition, there is an increased risk of hypoglycemia when these agents are used with insulin.
A recently published, randomized pilot study assessed the safety and efficacy of the DPP-4 inhibitor sitagliptin for the inpatient management of type 2 diabetes.101 In this trial, patients treated with diet, oral antidiabetic agents, or a low daily insulin dose (≤ 0.4 units/kg/day) were randomized to sitagliptin alone or in combination with low-dose insulin glargine or to a basal-bolus insulin regimen plus supplemental doses of insulin lispro. Glycemic control improved similarly in all treatment groups. It should be noted that most patients with an admission glucose < 180 mg/dl who were treated with sitagliptin plus correction doses of rapid-acting insulin responded as well as those treated with a basal-bolus insulin regimen. However, patients with an admission glucose > 180 mg/dl treated with sitagliptin alone had a higher mean daily blood glucose (182.7 ± 30 mg/dl) compared with patients treated with basal-bolus (168.1 ± 31 mg/dl) and sitagliptin plus glargine (161.8 ± 31 mg/dl) (P = 0.08).
Improving glycemic control while decreasing glycemic variability may be another advantage of using incretin-based therapies in the hospital. There is substantial evidence linking high glycemic variability with adverse outcomes in critically ill patients102–104 and with increased lengths of stay and mortality rates in noncritically ill hospitalized patients.105 Incretin therapies are known to reduce glucose fluctuations and glycemic variability measures,99,106 but the potential benefits of these agents on glycemic variability has yet to be determined in the hospital setting.
Increased risk of acute pancreatitis, including fatal and nonfatal hemorrhagic or necrotizing pancreatitis has been reported with incretin therapies.107–111 Although post-marketing reports of these occurrences are exceedingly rare, caution should be used in patients with a history of pancreatitis, abdominal pain, or postsurgical ileus. Additionally, increases of 2-5 bpm in heart rate have been observed in hospitalized patients with cardiovascular disease receiving GLP-1 receptor agonist therapy.100,112 Although clinical trials have found no associations between adverse cardiovascular events and the use of GLP-1 receptor agonists113 or DPP-4 inhibitors,114 long-term studies are needed. Two prospective outpatient cardiovascular outcome trials recently reported that patients treatment with alogliptin or saxagliptin had no increased risk of ischemic events,115,116 although rates of hospitalization for heart failure were increased with saxagliptin therapy.115,116
Hospital Discharge Considerations
To avoid medication errors and hospital readmissions, preparation for transition to the outpatient setting should begin at the time of hospital admission.117 Based on a recent A1C, for patients previously well controlled (A1C < 7%) on oral medications, it is reasonable to resume their previous regimen at the time of discharge. However, patients with higher A1C values will often require intensification of their outpatient regimen or continuation of the inpatient insulin regimen.5
Patients newly started on insulin therapy during hospitalization will require substantial diabetes education before discharge. Although American Diabetes Association guidelines recommend that patients receive “survival skills” education to ensure safe care upon returning home,118 it is unknown whether this actually occurs and whether patients who do receive this training are able to apply it after discharge. There is limited information about follow-up of patients with diabetes after discharge, and there have been virtually no studies on methods to improve the transition of care from the inpatient to the outpatient setting. Nevertheless, current recommendations encourage that patients and their family or caregivers receive both written and oral instructions regarding their diabetes management regimen at the time of hospital discharge.5 In addition, clear communication with outpatient providers is crucial for ensuring a safe and successful transition to outpatient glycemic management.6
Conclusions
Inpatient hyperglycemia is common and associated with increased risks of complications in patients with or without diabetes. Correction of hyperglycemia with insulin administration has been shown to improve clinical outcomes,5,6 and existing clinical evidence favors insulin over other antidiabetic agents in achieving and maintaining glycemic control in hospitalized patients. The basal-bolus approach has been shown to improve glycemic control and reduce perioperative complications in general medicine and surgery patients with diabetes.12,30 Hypoglycemia is the most frequent side effect and the limiting factor for achieving glycemic control in the inpatient setting. Although, recent studies have reported an association between hypoglycemia and increased hospital mortality, it remains unclear whether hypoglycemia is a direct mediator of adverse outcomes and mortality or merely a biomarker of disease burden and severity.
Increasing preliminary data indicate that incretin-based therapies have the potential to improve glycemic control with a low risk of hypoglycemia. However, more prospective studies are needed to determine the safety and efficacy of these agents in the hospital setting. The remaining available antidiabetic drugs have a limited role in the hospital because of their potential for serious adverse side effects, including the risk of lactic acidosis with metformin, hypoglycemia with sulfonylureas and glinides, edema and heart failure with pioglitazone, and dehydration and urinary and genital infections with the SGLT-2 inhibitors.
References
- 1.Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K; German Competence Network Sepsis (SepNet): Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Griesdale DE, de Souza RJ, van Dam RM, Heyland DK, Cook DJ, Malhotra A, Dhaliwal R, Henderson WR, Chittock DR, Finfer S, Talmor D: Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including NICE-SUGAR study data. CMAJ 180:821–827, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chiolero R: A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 35:1738–1748, 2009 [DOI] [PubMed] [Google Scholar]
- 4.Study Investigators NICE-SUGAR, Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ: Intensive versus conventional glucose control in critically ill patients. N Engl J Med 360:1283–1297, 2009 [DOI] [PubMed] [Google Scholar]
- 5.Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, Seley JJ, van den Berghe G, Endocrine Society: Management of hyperglycemia in hospitalized patients in non-critical care setting: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97:16–38, 2012 [DOI] [PubMed] [Google Scholar]
- 6.Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE; American Association of Clinical Endocrinologists, American Diabetes Association: American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care 32:1119–1131, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwartz S, DeFronzo RA: Is incretin-based therapy ready for the care of hospitalized patients with type 2 diabetes? The time has come for GLP-1 receptor agonists! Diabetes Care 36:2107–2111, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Umpierrez GE, Korytkowski M: Is incretin-based therapy ready for the care of hospitalized patients with type 2 diabetes? Insulin therapy has proven itself and is considered the mainstay of treatment. Diabetes Care 36:2112–2117, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rizzo MR, Barbieri M, Marfella R, Paolisso G: Reduction of oxidative stress and inflammation by blunting daily acute glucose fluctuations in patients with type 2 diabetes: role of dipeptidyl peptidase-IV inhibition. Diabetes Care 35:2076–2082, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makdissi A, Chaudhuri A, Kuhadiya N, Batra M, Dandona P: Comment on: Rizzo et al. Reduction of oxidative stress and inflammation by blunting daily acute glucose fluctuations in patients with type 2 diabetes: role of dipeptidyl peptidase-IV inhibition. Diabetes Care 2012;35:2076–2082. Diabetes Care 36:e80, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Furnary AP, Gao G, Grunkemeier GL, Wu Y, Zerr KJ, Bookin SO, Floten HS, Starr A: Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 125:1007–1021, 2003 [DOI] [PubMed] [Google Scholar]
- 12.Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, Umpierrez D, Newton C, Olson D, Rizzo M: Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 Surgery). Diabetes Care 34:256–261, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R: Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367, 2001 [DOI] [PubMed] [Google Scholar]
- 14.van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R: Intensive insulin therapy in the medical ICU. N Engl J Med 354:449–461, 2006 [DOI] [PubMed] [Google Scholar]
- 15.McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ: The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care 28:810–815, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Dandona P, Aljada A, Mohanty P, Ghanim H, Hamouda W, Assian E, Ahmad S: Insulin inhibits intranuclear nuclear factor kappaB and stimulates IkappaB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? J Clin Endocrinol Metab 86:3257–3265, 2001 [DOI] [PubMed] [Google Scholar]
- 17.Chaudhuri A, Janicke D, Wilson MF, Tripathy D, Garg R, Bandyopadhyay A, Calieri J, Hoffmeyer D, Syed T, Ghanim H, Aljada A, Dandona P: Anti-inflammatory and profibrinolytic effect of insulin in acute ST-segment-elevation myocardial infarction. Circulation 109:849–854, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Cheung NW, Wong VW, McLean M: The Hyperglycemia: Intensive Insulin Infusion in Infarction (HI-5) study: a randomized controlled trial of insulin infusion therapy for myocardial infarction. Diabetes Care 29:765–770, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Corssmit EP, Romijn JA, Sauerwein HP: Regulation of glucose production with special attention to nonclassical regulatory mechanisms: a review. Metabolism 50:742–755, 2001 [DOI] [PubMed] [Google Scholar]
- 20.Rizza RA, Mandarino LJ, Gerich JE: Dose-response characteristics for effects of insulin on production and utilization of glucose in man. Am J Physiol 240:E630–E639, 1981 [DOI] [PubMed] [Google Scholar]
- 21.Langouche L, Vanhorebeek I, Vlasselaers D, Vander Perre S, Wouters PJ, Skogstrand K, Hansen TK, van den Berghe G: Intensive insulin therapy protects the endothelium of critically ill patients. J Clin Invest 115:2277–2286, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagdade JD, Root RK, Bulger RJ: Impaired leukocyte function in patients with poorly controlled diabetes. Diabetes 23:9–15, 1974 [DOI] [PubMed] [Google Scholar]
- 23.Edwards FH, Grover FL, Shroyer AL, Schwartz M, Bero J: The Society of Thoracic Surgeons National Cardiac Surgery Database: current risk assessment. Ann Thorac Surg 63:903–908, 1997 [DOI] [PubMed] [Google Scholar]
- 24.Garg R, Chaudhuri A, Munschauer F, Dandona P: Hyperglycemia, insulin, and acute ischemic stroke: a mechanistic justification for a trial of insulin infusion therapy. Stroke 37:267–273, 2006 [DOI] [PubMed] [Google Scholar]
- 25.Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE: Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Diabetes 53:2079–2086, 2004 [DOI] [PubMed] [Google Scholar]
- 26.King AB, Armstrong DU: Basal bolus dosing: a clinical experience. Curr Diabetes Rev 1:215–220, 2005 [DOI] [PubMed] [Google Scholar]
- 27.Umpierrez G, Maynard G: Glycemic chaos (not glycemic control) still the rule for inpatient care: how do we stop the insanity? J Hosp Med 1:141–144, 2006 [DOI] [PubMed] [Google Scholar]
- 28.Hirsch IB: Sliding scale insulin: time to stop sliding. JAMA 301:213–214, 2009 [DOI] [PubMed] [Google Scholar]
- 29.Umpierrez GE, Palacio A, Smiley D: Sliding scale insulin use: myth or insanity? Am J Med 120:563–567, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Umpierrez GE, Smiley D, Zisman A, Prieto LM, Palacio A, Ceron M, Puig A, Mejia R: Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial). Diabetes Care 30:2181–2186, 2007 [DOI] [PubMed] [Google Scholar]
- 31.Umpierrez GE, Hor T, Smiley D, Temponi A, Umpierrez D, Ceron M, Munoz C, Newton C, Peng L, Baldwin D: Comparison of inpatient insulin regimens with detemir plus aspart versus neutral protamine hagedorn plus regular in medical patients with type 2 diabetes. J Clin Endocrinol Metab 94:564–569, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB; American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals. Diabetes Care 27:553–591, 2004 [DOI] [PubMed] [Google Scholar]
- 33.Maynard G, Lee J, Phillips G, Fink E, Renvall M: Improved inpatient use of basal insulin, reduced hypoglycemia, and improved glycemic control: effect of structured subcutaneous insulin orders and an insulin management algorithm. J Hosp Med 4:3–15, 2009 [DOI] [PubMed] [Google Scholar]
- 34.Pietras SM, Hanrahan P, Arnold LM, Sternthal E, McDonnell ME: State-of-the-art inpatient diabetes care: the evolution of an academic hospital. Endocr Pract 16:512–521, 2010 [DOI] [PubMed] [Google Scholar]
- 35.Rubin DJ, Rybin D, Doros G, McDonnell ME: Weight-based, insulin dose-related hypoglycemia in hospitalized patients with diabetes. Diabetes Care 34:1723–1728, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baldwin D, Zander J, Munoz C, Raghu P, DeLange-Hudec S, Lee H, Emanuele MA, Glossop V, Smallwood K, Molitch M: A randomized trial of two weight-based doses of insulin glargine and glulisine in hospitalized subjects with type 2 diabetes and renal insufficiency. Diabetes Care 35:1970–1974, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Umpierrez GE, Smiley D, Hermayer K, Khan A, Olson DE, Newton C, Jacobs S, Rizzo M, Peng L, Reyes D, Pinzon I, Fereira ME, Hunt V, Gore A, Toyoshima MT, Fonseca VA: Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: Basal Plus trial. Diabetes Care 36:2169–2174, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE: Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87:978–982, 2002 [DOI] [PubMed] [Google Scholar]
- 39.Cook CB, Kongable GL, Potter DJ, Abad VJ, Leija DE, Anderson M: Inpatient glucose control: a glycemic survey of 126 U.S. hospitals. J Hosp Med 4:E7–E14, 2009 [DOI] [PubMed] [Google Scholar]
- 40.Falciglia M, Freyberg RW, Almenoff PL, D'Alessio DA, Render ML: Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med 37:3001–3009, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kitabchi AE, Freire AX, Umpierrez GE: Evidence for strict inpatient blood glucose control: time to revise glycemic goals in hospitalized patients. Metabolism 57:116–120, 2008 [DOI] [PubMed] [Google Scholar]
- 42.Haga KK, McClymont KL, Clarke S, Grounds RS, Ng KY, Glyde DW, Loveless RJ, Carter GH, Alston RP: The effect of tight glycaemic control, during and after cardiac surgery, on patient mortality and morbidity: a systematic review and meta-analysis. J Cardiothorac Surg 6:3, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dandona P, Mohanty P, Chaudhuri A, Garg R, Aljada A: Insulin infusion in acute illness. J Clin Invest 115:2069–2072, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aljada A, Ghanim H, Saadeh R, Dandona P: Insulin inhibits NFkappaB and MCP-1 expression in human aortic endothelial cells. J Clin Endocrinol Metab 86:450–453, 2001 [DOI] [PubMed] [Google Scholar]
- 45.Ng KW, Allen ML, Desai A, Macrae D, Pathan N: Cardioprotective effects of insulin: how intensive insulin therapy may benefit cardiac surgery patients. Circulation 125:721–728, 2012 [DOI] [PubMed] [Google Scholar]
- 46.Rashidee A, Hart J, Chen J, Kumar S: High-alert medications: error prevalence and severity. Patient Safety & Quality Healthcare July-August 2009 [Google Scholar]
- 47.Gill GV, Woodward A, Casson IF, Weston PJ: Cardiac arrhythmia and nocturnal hypoglycaemia in type 1 diabetes: the 'dead in bed' syndrome revisited. Diabetologia 52:42–45, 2009 [DOI] [PubMed] [Google Scholar]
- 48.Desouza C, Salazar H, Cheong B, Murgo J, Fonseca V: Association of hypoglycemia and cardiac ischemia: a study based on continuous monitoring. Diabetes Care 26:1485–1489, 2003 [DOI] [PubMed] [Google Scholar]
- 49.Desouza CV, Bolli GB, Fonseca V: Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care 33:1389–1394, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Razavi Nematollahi L, Kitabchi AE, Stentz FB, Wan JY, Larijani BA, Tehrani MM, Gozashti MH, Omidfar K, Taheri E: Proinflammatory cytokines in response to insulin-induced hypoglycemic stress in healthy subjects. Metabolism 58:443–448, 2009 [DOI] [PubMed] [Google Scholar]
- 51.Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML: Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care 32:1153–1157, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Curkendall SM, Natoli JL, Alexander CM, Nathanson BH, Haidar T, Dubois RW: Economic and clinical impact of inpatient diabetic hypoglycemia. Endocr Pract 15:302–312, 2009 [DOI] [PubMed] [Google Scholar]
- 53.Boucai L, Southern WN, Zonszein J: Hypoglycemia-associated mortality is not drug-associated but linked to comorbidities. Am J Med 124:1028–1035, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kosiborod M, Inzucchi SE, Krumholz HM, Masoudi FA, Goyal A, Xiao L, Jones PG, Fiske S, Spertus JA: Glucose normalization and outcomes in patients with acute myocardial infarction. Arch Intern Med 169:438–446, 2009 [DOI] [PubMed] [Google Scholar]
- 55.Garg R, Hurwitz S, Turchin A, Trivedi A: Hypoglycemia, with or without insulin therapy, is associated with increased mortality among hospitalized patients. Diabetes Care 36:1107–1110, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Diamant M: Choosing a blood-glucose-lowering agent after metformin. Lancet 379:2220–2221, 2012 [DOI] [PubMed] [Google Scholar]
- 57.Lipska KJ, Bailey CJ, Inzucchi SE: Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care 34:1431–1437, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Salpeter SR, Greyber E, Pasternak GA, Salpeter Posthumous EE: Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev 1:CD002967, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kosmalski M, Drozdowska A, Sliwinska A, Drzewoski J: Inappropriate metformin prescribing in elderly type 2 diabetes mellitus (T2DM) patients. Adv Med Sci 57:65–70, 2012 [DOI] [PubMed] [Google Scholar]
- 60.Hundal RS, Krssak M, Dufour S, Laurent D, Lebon V, Chandramouli V, Inzucchi SE, Schumann WC, Petersen KF, Landau BR, Shulman GI: Mechanism by which metformin reduces glucose production in type 2 diabetes. Diabetes 49:2063–2069, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aronne LJ: Therapeutic options for modifying cardiometabolic risk factors. Am J Med 120 (3 Suppl. 1):S26–S34, 2007 [DOI] [PubMed] [Google Scholar]
- 62.Kirpichnikov D, McFarlane SI, Sowers JR: Metformin: an update. Ann Intern Med 137:25–33, 2002 [DOI] [PubMed] [Google Scholar]
- 63.Rojas LB, Gomes MB: Metformin: an old but still the best treatment for type 2 diabetes. Diabetol Metab Syndr 5:6, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brown JB, Pedula K, Barzilay J, Herson MK, Latare P: Lactic acidosis rates in type 2 diabetes. Diabetes Care 21:1659–1663, 1998 [DOI] [PubMed] [Google Scholar]
- 65.Cryer DR, Nicholas SP, Henry DH, Mills DJ, Stadel BV: Comparative outcomes study of metformin intervention versus conventional approach the COSMIC approach study. Diabetes Care 28:539–543, 2005 [DOI] [PubMed] [Google Scholar]
- 66.Pasquel FJ, Klein R, Adigweme A, Hinedi Z, Coralli R, Pimentel JL, Umpierrez GE: Metformin-associated lactic acidosis. Am J Med Sci. 2013. Epub ahead of print (doi: 10.1097/MAJ.0b013e3182a562b7) [DOI] [PubMed] [Google Scholar]
- 67.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR, American Diabetes Association (ADA), European Association for the Study of Diabetes (EASD): Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 35:1364–1379, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sturgess NC, Ashford ML, Cook DL, Hales CN: The sulphonylurea receptor may be an ATP-sensitive potassium channel. Lancet 2:474–475, 1985 [DOI] [PubMed] [Google Scholar]
- 69.Boyd AE. 3rd: Sulfonylurea receptors, ion channels, and fruit flies. Diabetes 37:847–850, 1988 [DOI] [PubMed] [Google Scholar]
- 70.Groop LC: Sulfonylureas in NIDDM. Diabetes Care 15:737–754, 1992 [DOI] [PubMed] [Google Scholar]
- 71.Bolen S, Feldman L, Vassy J, Wilson L, Yeh HC, Marinopoulos S, Wiley C, Selvin E, Wilson R, Bass EB, Brancati FL: Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus. Ann Intern Med 147:386–399, 2007 [DOI] [PubMed] [Google Scholar]
- 72.U.K. Prospective Study Group : Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853, 1998 [PubMed] [Google Scholar]
- 73.Meinert CL, Knatterud GL, Prout TE, Klimt CR: A study of the effects of hypoglycemic agents on vascular complications in patients with adult-onset diabetes. II. Mortality results. Diabetes 19 (Suppl):789–830, 1970 [PubMed] [Google Scholar]
- 74.Brady PA, Terzic A: The sulfonylurea controversy: more questions from the heart. J Am Coll Cardiol 31:950–956, 1998 [DOI] [PubMed] [Google Scholar]
- 75.Ashcroft FM, Rorsman P: K(ATP) channels and islet hormone secretion: new insights and controversies. Nat Rev Endocrinol 9:660–669, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Deusenberry CM, Coley KC, Korytkowski MT, Donihi AC: Hypoglycemia in hospitalized patients treated with sulfonylureas. Pharmacotherapy 32:613–617, 2012 [DOI] [PubMed] [Google Scholar]
- 77.Mohr JF, McKinnon PS, Peymann PJ, Kenton I, Septimus E, Okhuysen PC: A retrospective, comparative evaluation of dysglycemias in hospitalized patients receiving gatifloxacin, levofloxacin, ciprofloxacin, or ceftriaxone. Pharmacotherapy 25:1303–1309, 2005 [DOI] [PubMed] [Google Scholar]
- 78.Tirkkonen T, Heikkila P, Huupponen R, Laine K: Potential CYP2C9-mediated drug-drug interactions in hospitalized type 2 diabetes mellitus patients treated with the sulphonylureas glibenclamide, glimepiride or glipizide. J Intern Med 268:359–366, 2010 [DOI] [PubMed] [Google Scholar]
- 79.Melander A: Kinetics-effect relations of insulin-releasing drugs in patients with type 2 diabetes: brief overview. Diabetes 53 (Suppl. 3):S151–S155, 2004 [DOI] [PubMed] [Google Scholar]
- 80.Dornhorst A: Insulinotropic meglitinide analogues. Lancet 358:1709–1716, 2001 [DOI] [PubMed] [Google Scholar]
- 81.Varghese P, Gleason V, Sorokin R, Senholzi C, Jabbour S, Gottlieb JE: Hypoglycemia in hospitalized patients treated with antihyperglycemic agents. J Hosp Med 2:234–240, 2007 [DOI] [PubMed] [Google Scholar]
- 82.Ahmadian M, Suh JM, Hah N, Liddle C, Atkins AR, Downes M, Evans RM: PPARgamma signaling and metabolism: the good, the bad and the future. Nat Med 19:557–566, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B; American Diabetes Association, European Association for Study of Diabetes: Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 32:193–203, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mudaliar S, Chang AR, Henry RR: Thiazolidinediones, peripheral edema, and type 2 diabetes: incidence, pathophysiology, and clinical implications. Endocr Pract 9:406–416, 2003 [DOI] [PubMed] [Google Scholar]
- 85.Ferrannini E, Solini A: SGLT2 inhibition in diabetes mellitus: rationale and clinical prospects. Nat Rev Endocrinol 8:495–502, 2012 [DOI] [PubMed] [Google Scholar]
- 86.U.S. Food and Drug Administration : FDA approves Invokana to treat type 2 diabetes. Available from http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm345848.htm. Accessed 10 February 2014
- 87.U.S. Food and Drug Administration : FDA approves Farxiga to treat type 2 diabetes. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm380829.htm. Accessed 10 February 2014
- 88.Vasilakou D, Karagiannis T, Athanasiadou E, Mainou M, Liakos A, Bekiari E, Sarigianni M, Matthews DR, Tsapas A: Sodium-glucose cotransporter 2 inhibitors for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 159:262–274, 2013 [DOI] [PubMed] [Google Scholar]
- 89.Komoroski B, Vachharajani N, Boulton D, Kornhauser D, Geraldes M, Li L, Pfister M: Dapagliflozin, a novel SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharmacol Ther 85:520–526, 2009 [DOI] [PubMed] [Google Scholar]
- 90.Derosa G, Maffioli P: Efficacy and safety profile evaluation of acarbose alone and in association with other antidiabetic drugs: a systematic review. Clin Ther 34:1221–1236, 2012 [DOI] [PubMed] [Google Scholar]
- 91.Butler PC, Elashoff M, Elashoff R, Gale EA: A critical analysis of the clinical use of incretin-based therapies: are the GLP-1 therapies safe? Diabetes Care 36:2118–2125, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nauck MA: A critical analysis of the clinical use of incretin-based therapies: the benefits by far outweigh the potential risks. Diabetes Care 36:2126–2132, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Deane AM, Chapman MJ, Fraser RJ, Burgstad CM, Besanko LK, Horowitz M: The effect of exogenous glucagon-like peptide-1 on the glycaemic response to small intestinal nutrient in the critically ill: a randomised double-blind placebo-controlled cross over study. Crit Care 13:R67, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Meier JJ, Weyhe D, Michaely M, Senkal M, Zumtobel V, Nauck MA, Holst JJ, Schmidt WE, Gallwitz B: Intravenous glucagon-like peptide 1 normalizes blood glucose after major surgery in patients with type 2 diabetes. Crit Care Med 32:848–851, 2004 [DOI] [PubMed] [Google Scholar]
- 95.Mussig K, Oncu A, Lindauer P, Heininger A, Aebert H, Unertl K, Ziemer G, Haring HU, Holst JJ, Gallwitz B: Effects of intravenous glucagon-like peptide-1 on glucose control and hemodynamics after coronary artery bypass surgery in patients with type 2 diabetes. Am J Cardiol 102:646–647, 2008 [DOI] [PubMed] [Google Scholar]
- 96.Sourij H, Schmolzer I, Kettler-Schmut E, Eder M, Pressl H, Decampo A, Wascher TC: Efficacy of a continuous GLP-1 infusion compared with a structured insulin infusion protocol to reach normoglycemia in nonfasted type 2 diabetic patients: a clinical pilot trial. Diabetes Care 32:1669–1671, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ritzel RA, Kleine N, Holst JJ, Willms B, Schmiegel W, Nauck MA: Preserved GLP-1 effects in a diabetic patient with Cushing's disease. Exp Clin Endocrinol Diabetes 115:146–150, 2007 [DOI] [PubMed] [Google Scholar]
- 98.Kohl BA, Hammond MS, Cucchiara AJ, Ochroch EA: Intravenous GLP-1 (7-36) amide for prevention of hyperglycemia during cardiac surgery: a randomized, double-blind, placebo-controlled study. J Cardiothorac Vasc Anesth 2013. Epub ahead of print (doi: 10.1053/j.jvca.2013.06.021) [DOI] [PubMed] [Google Scholar]
- 99.Abuannadi M, Kosiborod M, Riggs L, House JA, Hamburg MS, Kennedy KF, Marso SP: Management of hyperglycemia with the administration of intravenous exenatide to patients in the cardiac intensive care unit. Endocr Pract 19:81–90, 2013 [DOI] [PubMed] [Google Scholar]
- 100.Sokos GG, Nikolaidis LA, Mankad S, Elahi D, Shannon RP: Glucagon-like peptide-1 infusion improves left ventricular ejection fraction and functional status in patients with chronic heart failure. J Card Fail 12:694–699, 2006 [DOI] [PubMed] [Google Scholar]
- 101.Umpierrez GE, Gianchandani R, Smiley D, Jacobs S, Wesorick DH, Newton C, Farrokhi F, Peng L, Reyes D, Lathkar-Pradhan S, Pasquel F: Safety and efficacy of sitagliptin therapy for the inpatient management of general medicine and surgery patients with type 2 diabetes: a pilot, randomized, controlled study. Diabetes Care 36:3430–3435, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Krinsley JS: Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med 36:3008–3013, 2008 [DOI] [PubMed] [Google Scholar]
- 103.Su G, Mi SH, Tao H, Li Z, Yang HX, Zheng H, Zhou Y, Tian L: Impact of admission glycemic variability, glucose, and glycosylated hemoglobin on major adverse cardiac events after acute myocardial infarction. Diabetes Care 36:1026–1032, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Farrokhi F, Chandra P, Smiley D, Pasquel FJ, Peng L, Newton CA, Umpierrez GE: Glucose variability is an independent predictor of mortality in hospitalized patients treated with total parenteral nutrition. Endocr Pract 20:41–45, 2014 [DOI] [PubMed] [Google Scholar]
- 105.Mendez CE, Mok KT, Ata A, Tanenberg RJ, Calles-Escandon J, Umpierrez GE: Increased glycemic variability is independently associated with length of stay and mortality in noncritically ill hospitalized patients. Diabetes Care 36:4091–4097, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Galiatsatos P, Gibson BR, Rabiee A, Carlson O, Egan JM, Shannon RP, Andersen DK, Elahi D: The glucoregulatory benefits of glucagon-like peptide-1 (7-36) amide infusion during intensive insulin therapy in critically ill surgical patients: a pilot study. Crit Care Med 42:638–645, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Merck : Januvia (sitagliptin) tablets prescribing information. Available from http://www.merck.com/product/usa/pi_circulars/j/januvia/januvia_pi.pdf. Accessed 13 February 2014
- 108.Novartis Pharmaceuticals : GALVUS (vildagliptin). Available from http://www.novartis.com.au/PI_PDF/gal.pdf. Accessed 13 February 2014
- 109.Amylin Pharmaceuticals : Byetta (exenatide) prescribing information. Available from http://packageinserts.bms.com/pi/pi_byetta.pdf. Accessed 13 February 2014
- 110.Novo Nordisk : Victoza (liraglutide) rDNA injection prescribing information. Available from http://www.novo-pi.com/victoza.pdf. Accessed 13 February 2014
- 111.Bristol-Myers Squibb : Onglyza (saxagliptin) prescribing information. Available from http://packageinserts.bms.com/pi/pi_onglyza.pdf. Accessed 13 February 2014
- 112.Halbirk M, Norrelund H, Moller N, Holst JJ, Schmitz O, Nielsen R, Nielsen-Kudsk JE, Nielsen SS, Nielsen TT, Eiskjaer H, Botker HE, Wiggers H: Cardiovascular and metabolic effects of 48-h glucagon-like peptide-1 infusion in compensated chronic patients with heart failure. Am J Physiol Heart Circ Physiol 298:H1096–H1102, 2010 [DOI] [PubMed] [Google Scholar]
- 113.Monami M, Cremasco F, Lamanna C, Colombi C, Desideri CM, Iacomelli I, Marchionni N, Mannucci E: Glucagon-like peptide-1 receptor agonists and cardiovascular events: a meta-analysis of randomized clinical trials. Exp Diabetes Res 2011:215764 (doi: 10.1155/2011/215764) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Monami M, Dicembrini I, Martelli D, Mannucci E: Safety of dipeptidyl peptidase-4 inhibitors: a meta-analysis of randomized clinical trials. Curr Med Res Opin 27 (Suppl. 3):57–64, 2011 [DOI] [PubMed] [Google Scholar]
- 115.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mosenzon O, McGuire DK, Ray KK, Leiter LA, Raz I, SAVOR-TIMI 53 Steering Committee and Investigators: Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 369:1317–1326, 2013 [DOI] [PubMed] [Google Scholar]
- 116.White WB, Pratley R, Fleck P, Munsaka M, Hisada M, Wilson C, Menon V: Cardiovascular safety of the dipetidyl peptidase-4 inhibitor alogliptin in type 2 diabetes mellitus. Diabetes Obes Metab 15:668–673, 2013 [DOI] [PubMed] [Google Scholar]
- 117.Schnipper JL, Magee M, Larsen K, Inzucchi SE, Maynard G; Society of Hospital Medicine Glycemic Control Task Force: Society of hospital medicine glycemic control task force summary: practical recommendations for assessing the impact of glycemic control efforts. J Hosp Med 3 (Suppl. 5):66–75, 2008 [DOI] [PubMed] [Google Scholar]
- 118.American Diabetes Association : Standards of medical care in diabetes-2013. Diabetes Care 36 (Suppl. 1):S11–S66, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]


