Abstract
We present a new technique for the combined intra- and extra-articular reconstruction of the anterior cruciate ligament. Intra-articular reconstruction is performed in an outside-in manner according to the precepts of the anatomic femoral tunnel technique. Extra-articular reconstruction is performed with the gracilis tendon while respecting the anatomic parameters of the origin and insertion points and the path described for the knee anterolateral ligament.
Anterior cruciate ligament (ACL) injury is among the most common orthopaedic injuries.1 Despite technological advances in the surgical techniques for ACL reconstruction, the failure rate remains approximately 7%.2,3
Failures can occur because of improper tunnel positioning or problems with patient rehabilitation; however, there are some patients in whom reconstruction fails without any predisposing factors.4 In such cases, failure is believed to be due to non-optimal incorporation of the graft used for reconstruction. A structure located in the anterolateral portion of the knee, adjacent to the joint capsule, called the anterolateral ligament (ALL), has recently been studied in more detail and may be responsible for some cases that do not progress satisfactorily after ACL reconstruction.5-8
Conducting extra-articular lateral reinforcement in association with intra-articular reconstruction of the ACL is not new, and various authors have proposed various nonanatomic techniques for this purpose.9-11 Recent anatomic studies have made it possible to characterize the anatomy of the ALL in this region in detail, thereby making its reconstruction possible. This technique can act as an extra-articular ACL reconstruction that respects the anatomic parameters of the ALL. The aim of this study was to present a combined intra- and extra-articular reconstruction technique for ACL injuries in which the extra-articular reconstruction aimed to anatomically reconstruct the ALL.
Technique
Graft Preparation
The combined technique for ACL and ALL reconstruction was performed using hamstring tendons. Autologous tendons or tendons from a tissue bank can be used, depending on the patient's characteristics and the surgeon's preference (Video 1). The semitendinosus tendon is prepared as a triple graft and the gracilis tendon as a single graft, yielding a quadruple ACL graft; the remaining portion of the gracilis is used for ALL reconstruction (Fig 1).
Fig 1.
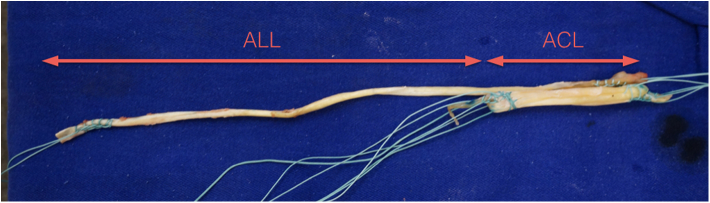
Triple semitendinosus and single gracilis graft prepared for combined anterior cruciate ligament (ACL) and anterolateral ligament (ALL) reconstruction. The part used to reconstruct the ACL is a quadruple graft, and the remaining part of the gracilis is used to reconstruct the ALL.
Lateral Access Route
A lateral access route is established from the lateral epicondyle to an intermediate point between the Gerdy tubercle and the fibular head (Fig 2). After dissection of the skin and subcutaneous tissue, the iliotibial tract is opened toward its fibers. Opening of the tract is performed at the height of the lateral epicondyle, with a length of approximately 3 cm.
Fig 2.
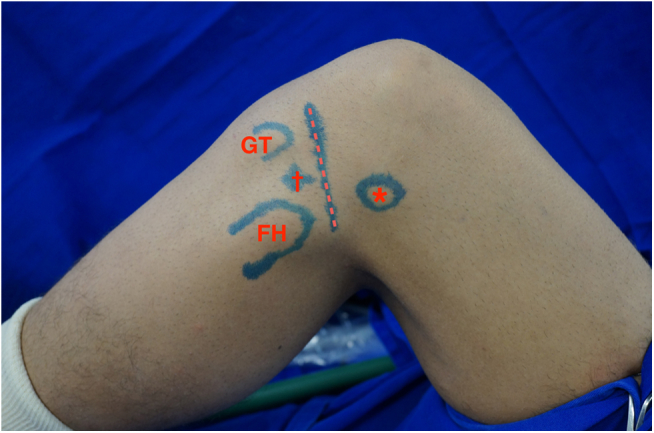
Lateral image of a left knee showing the anterolateral ligament reconstruction landmarks, including the Gerdy tubercle (GT), fibular head (FH), lateral epicondyle (asterisk), and tibial insertion point (dagger) of anterolateral ligament. The joint line is represented by the dotted line.
Radiographic Femoral Landmarks
After the iliotibial tract has been opened, the radiographic landmark point of the femoral origin of the ALL is found using fluoroscopy.12,13 The Blumensaat line and a line perpendicular to it are used to find the origin of the ALL on an absolute lateral knee radiograph. The ALL femoral point is found at about the halfway point on the Blumensaat line in the anterior to posterior direction, around 3 to 4 mm below it. A 5-mm metal anchor (Fastin, DePuy Mitek, Raynham, MA) is inserted into this bony landmark (Fig 3). Before insertion of the anchor, an ice pick is used to mark the correct point.
Fig 3.
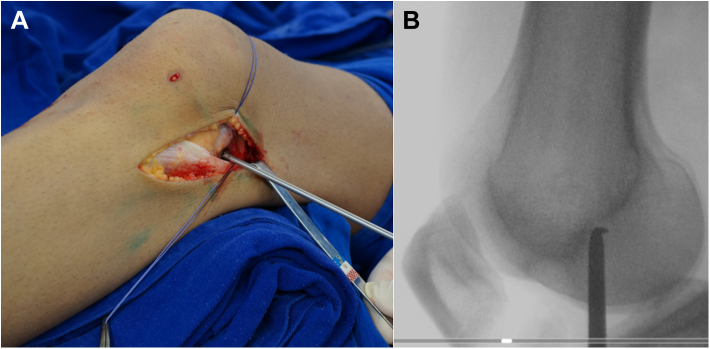
(A) Clinical photograph of the anchor insertion at the femoral point of origin of the anterolateral ligament in a left knee. (B) The radiographic anchor insertion point is obtained using fluoroscopy on a true lateral view.
ACL Reconstruction
After insertion of the femoral anchor, arthroscopy is performed. The knee cavity is inspected, and any meniscal or cartilage injuries identified are treated. The intercondylar area is prepared by shaving the inside wall of the lateral femoral condyle.
The femoral tunnel of the ACL is made using an outside-in technique according to the recommendations of Garofalo et al.14 This tunnel begins outside the lateral femoral condyle, exits into the medial wall of the lateral condyle, and should respect the footprint of the native ACL. When the surgeon is preparing the femoral tunnel for the ACL, care should be taken not to interfere with the anchor already placed on the femur for reconstruction of the ALL. The tibial tunnel is made within the topography of the native ACL tibial footprint.15,16 We first insert a guidewire and then perform the drilling of the tunnels. The surgeon can make both the femoral and tibial tunnels using a standard ACL tibial guide, just adjusting the guide angulation to reach the correct footprints; no special equipment is required to perform this technique. The diameter of the tunnel is equal to the diameter of the previously prepared quadruple ACL graft.
After preparation of the tunnels, the graft is passed from the tibia to the femur. The ACL intra-articular graft is a quadruple graft, and the remaining portion of the gracilis, which will be used for ALL reconstruction, exits through the lateral condyle.
Femoral ACL fixation is initially performed in an outside-in manner using an absorbable interference screw (Biocryl, DePuy Mitek) with a diameter equal to the size of the tunnel; tibial ACL fixation is performed with approximately 30° of knee flexion with an absorbable interference screw one size greater than the tunnel diameter.
ALL Reconstruction
After fixation of the ACL graft, the remaining portion of the gracilis is used for ALL reconstruction. Initially, graft fixation is performed on the anchor that was inserted into the femur before the ACL reconstruction was performed.
Subsequently, another 5-mm anchor is inserted into the tibial anatomic attachment of the ALL. This point can be found with fluoroscopy or by using anatomic landmarks. Our current preference is to identify this point anatomically between the fibular head and Gerdy tubercle at approximately 5 to 10 mm below the joint line of the lateral tibial plateau (Fig 4). By use of radiographic landmarks, this point is found around 7 mm below the tibial plateau on the frontal view and at around 50% of the plateau length on the lateral view.12 The remaining portion of the gracilis then passes beneath the iliotibial tract until its tibial insertion point and is fixed onto this landmark through the suture anchor inserted (Figs 5 and 6).
Fig 4.
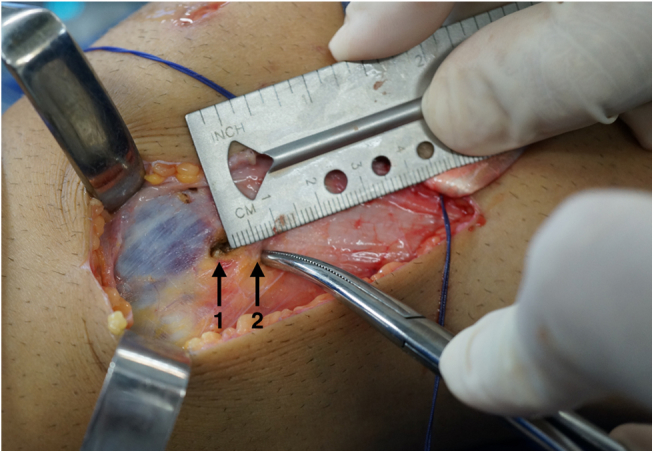
Lateral image of a left knee showing the tibial insertion point of the anterolateral ligament. Arrow 1 indicates the location for placement of the anchor that will be used for tibial fixation at approximately 7 mm below the joint line, which is represented by the tip of the forceps and arrow 2.
Fig 5.
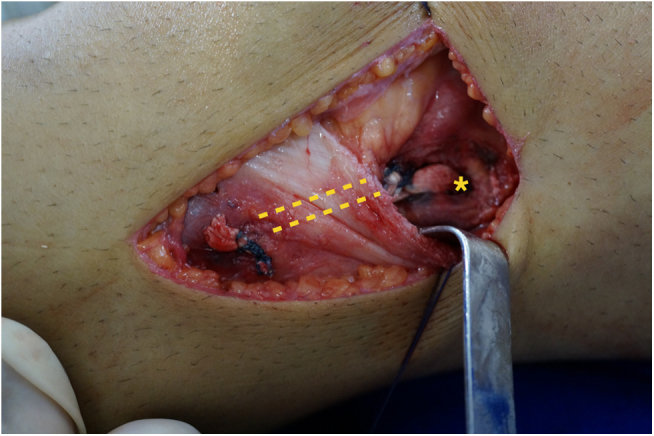
Final view of a left knee showing reconstruction of the anterolateral ligament (ALL). The asterisk indicates the femoral tunnel through which the gracilis portion exits for ALL reconstruction. The ALL passes below the iliotibial tract (with the 2 dotted lines showing its path) and is fixed onto the tibia.
Fig 6.

Three-dimensional computed tomographic reconstruction image showing final placement of femoral tunnel and tibial and femoral anchors for combined reconstruction of anterior cruciate ligament and anterolateral ligament.
Tibial graft fixation is performed with knee flexion between 60° and 90° in accordance with studies that have shown higher tensioning of this structure with knee flexion.17,18 According to the size of the graft, it is possible to render the ALL more calibrous by returning it underneath the iliotibial tract and reattaching it to the femur and to the tibia again, if possible.
After reconstruction, closure is performed. We do not use any type of drain or immobilization after reconstruction.
Discussion
The presented technique offers the main advantage of reliable reproduction of the anatomy of both the ACL and the ALL. We believe that just as the techniques for ACL reconstruction have evolved from nonanatomic procedures to procedures attempting to maximally reproduce the anatomy of the injured ACL, in the near future, extra-articular reconstructions will also tend to reproduce the anatomy of the ALL.19
Regardless of the fact that, so far, there is no research to suggest that ALL reconstruction improves the results of ACL reconstruction and the benefit of reconstructing this “new” structure is purely theoretical at this point, the addition of an extra-articular procedure for arthroscopic ACL reconstruction has yielded good results in several studies.20-23 Vadalà et al.20 studied female athletes with ACL injuries and concluded that those who underwent extra-articular reinforcement had a lower rate of residual rotatory instability. Dejour et al.21 investigated the addition of the Lemaire procedure to ACL reconstruction with a patellar tendon and showed less anterior translation of the lateral plateau relative to intra-articular reconstruction alone. Monaco et al.22 showed reduced internal rotation at 30° with the addition of a lateral plasty to single-band reconstruction when compared with double-band reconstruction alone. Trojani et al.23 studied revisions of ACL reconstructions in more than 160 patients and concluded that the addition of a lateral extra-articular procedure increased knee stability.
Even though several recent studies have shown the possible benefits of the addition of extra-articular reconstruction, its indication is still far from receiving a unanimous vote in the literature.9 One alternative that might be useful for the characterization of patients with lateral lesions would be an accurate viewing of the ALL capsule through imaging; however, existing studies continue to have difficulties in the characterization of this structure using magnetic resonance imaging, even in knees without ACL injury.24,25 Therefore we suggest the association of extra-articular reconstruction in cases with higher grades on the pivot-shift test and in cases requiring revision ACL reconstruction, especially those without an apparent cause of failure (Table 1).
Table 1.
Advantages, Indications, Contraindications, Tips and Pearls, and Pitfalls and Risks of Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction
| Advantage |
| Provides anatomic reconstruction of ACL and ALL |
| Indication |
| Cases with higher grades on the preoperative pivot-shift test and reconstruction revision cases, especially those without an apparent cause of failure |
| Contraindications |
| Autologous grafts of insufficient size (unless one can use tissue bank grafts) |
| Performance of our technique without treatment of known causes of ACL failure in revision cases |
| Tips and pearls |
| Measure the lengths of grafts right after harvesting them. |
| Open the iliotibial tract toward its fibers on the lateral access route. |
| Find the correct radiographic landmark to insert the femoral anchor. |
| Note that anatomically locating the tibial landmark for ALL reconstruction is easier between the Gerdy tubercle and fibular head. |
| Avoid leaving the anchor protruding both on the femur and on the tibia. |
| Pass the ALL graft under the iliotibial band to fix it on the tibia. |
| Pitfalls and risks |
| Protruded anchors can irritate the iliotibial band. |
| An absolute lateral view must be obtained to find the correct femoral radiographic landmarks; small inaccuracies can lead to totally incorrect points. |
| When preparing the femoral tunnel for the ACL, care should be taken not to interfere with the anchor already placed on the femur for the ALL reconstruction. |
| Patients can have lateral discomfort because of the iliotibial tract incision for up to 6 weeks. |
ACL, anterior cruciate ligament; ALL, anterolateral ligament.
Several techniques have already been used with the aim of enhancing isolated intra-articular reconstruction. Among these, the technique of Colombet10 perhaps has the most similar concepts to our presented technique. In his technique, Colombet prepares the femoral tunnel from the outside in using flexor tendons. He uses the same tendons used for ACL reconstruction to rebuild the ALL, thus minimizing the number of grafts. An important difference with our technique is the nonanatomic reconstruction of the ALL with origin and insertion points that do not correspond to the anatomic landmarks of the ALL described in the literature, which originates anteriorly and distally to the lateral collateral ligament (LCL) and is inserted between the Gerdy tubercle and fibular head.
Another difference that we consider important with respect to the Colombet technique is the fact that our technique has a quadruple reconstructed ACL, whereas in some situations, Colombet10 reconstructs the ACL with a double graft, although this is not his preference. This situation could render the ACL less biomechanically resistant. The decision to use a triple semitendinosus graft in association with a single gracilis graft aims to obtain a graft with a diameter equal to or greater than 8 mm, which is difficult to achieve with the isolated use of a double hamstring tendon graft. The MOON (Multicenter Orthopaedic Outcomes Network) cohort found that patients with graft diameters less than or equal to 7 mm had a higher rate of neoligament rupture.26 Despite this theoretical situation, Marcacci et al.11 studied 54 patients treated with combined intra- and extra-articular reconstruction of the ACL using a double hamstring graft for intra-articular reconstruction for a mean follow-up period of 11 years and observed good or excellent results in more than 90% of cases, as well as a low failure rate. Perhaps the association with extra-articular reconstruction reduces the risk of failure in grafts with a lower intra-articular diameter, but because we have no such evidence, we choose to perform intra-articular reconstruction with a triple semitendinosus graft in association with a single gracilis graft while always seeking to reconstruct the ACL with the largest possible diameter.
The limitations of the presented technique include the size of the flexor grafts used and fixation of the graft onto the tibia with the use of anchors. A minimum gracilis size of 18 cm is needed to make at least a double ALL. If the prepared gracilis tendon is shorter than this length, reconstruction should be performed with a single-bundle gracilis or a different technique or, if available, tissue bank grafts should be considered. Given the macroscopic anatomic characteristics of the ALL,6 a single gracilis graft may meet the biomechanical needs of this ligament, but biomechanical studies are needed to analyze these characteristics. Regarding fixation with anchors, the femoral anchor functions only to perform the graft tenodesis at its anatomic point so that the femoral fixation is doubled consequent to the interference screw used for ACL reconstruction. Tibial fixation is performed with only 1 anchor, but we believe that this type of fixation is adequate, given the biomechanical demands presented by the ALL. We also suggest that fixation be performed with a metal anchor associated with a high resistance and slow absorption or a nonabsorbable thread. The advantage of using an anchor in this situation is that it eliminates the need to make a second tibial tunnel. Marcacci et al.11 used only staples in their reconstructions and achieved excellent results.
Because of the proximity of the ALL to the LCL on the femur, the use of an anchor in this region protects the LCL against iatrogenic damage that could be caused by a femoral tunnel. Femoral tunnels, even if small, have a high probability of damaging the LCL origin in this region. We have ascertained in our anatomic studies that 8-mm tunnels can cause lesions involving half the insertion of the LCL in approximately 50% of patients (unpublished data, C.P.H, June 2014).
The limitations of this study include the non-performance of biomechanical tests to prove the effectiveness of the described technique relative to techniques already existing in the literature and the fact that ALL reconstruction has not yet been shown to yield short- or long-term clinical improvements; however, we believe that we could combine similar techniques in an attempt to apply the already used concepts to perform an extra-articular anatomic reconstruction. Moreover, the aim of this article is to describe our technique without presenting clinical or radiologic results. Clinical and radiologic studies are being conducted to show the effectiveness of this technique, and an initial series should be presented as soon as we have sufficient cases with an adequate minimum follow-up period.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Combined anterior cruciate ligament and anterolateral ligament reconstruction in a left knee.
References
- 1.Frank R.M., Verma N.N. Graft selection in revision ACL reconstruction. In: Bach B.R. Jr., Provencher M.T., editors. ACL surgery: How to get it right the first time and what to do if it fails. SLACK; Thorofare, NJ: 2010. pp. 217–229. [Google Scholar]
- 2.Hussein M., van Eck C.F., Cretnik A., Dinevski D., Fu F.H. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40:512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 3.Piefer J.W., Pflugner T.R., Hwang M.D., Lubowitz J.H. Anterior cruciate ligament femoral footprint anatomy: Systematic review of the 21st century literature. Arthroscopy. 2012;28:872–881. doi: 10.1016/j.arthro.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 4.Denti M., Lo Vetere D., Bait C., Schönhuber H., Melegati G., Volpi P. Revision anterior cruciate ligament reconstruction: Causes of failure, surgical technique, and clinical results. Am J Sports Med. 2008;10:1896–1902. doi: 10.1177/0363546508318189. [DOI] [PubMed] [Google Scholar]
- 5.Vincent J.P., Magnussen R.A., Gezmez F. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 6.Helito C.P., Demange M.K., Bonadio M.B. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1: doi: 10.1177/2325967113513546. 2325967113513546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pomajzl R., Maerz T., Shams C., Guettler J., Bicos J. A review of the anterolateral ligament of the knee: Current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy. 2015;31:585–591. doi: 10.1016/j.arthro.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Duthon V.B., Magnussen R.A., Servien E., Neyret P. ACL reconstruction and extra-articular tenodesis. Clin Sports Med. 2013;32:141–153. doi: 10.1016/j.csm.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Colombet P.D. Navigated intra-articular ACL reconstruction with additional extra-articular tenodesis using the same hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2011;19:384–389. doi: 10.1007/s00167-010-1223-0. [DOI] [PubMed] [Google Scholar]
- 11.Marcacci M., Zaffagnini S., Giordano G., Iacono F., Presti M.L. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009;37:707–714. doi: 10.1177/0363546508328114. [DOI] [PubMed] [Google Scholar]
- 12.Helito C.P., Demange M.K., Bonadio M.B. Radiographic landmarks for locating the femoral origin and tibial insertion of the knee anterolateral ligament. Am J Sports Med. 2014;42:2356–2362. doi: 10.1177/0363546514543770. [DOI] [PubMed] [Google Scholar]
- 13.Rezansoff AJ, Caterine S, Spencer L, Tran MN, Litchfield RB, Getgood AM. Radiographic landmarks for surgical reconstruction of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc in press, available online 17 June, 2014. doi:10.1007/s00167-014-3126-y. [DOI] [PubMed]
- 14.Garofalo R., Mouhsine E., Chambat P., Siegrist O. Anatomic anterior cruciate ligament reconstruction: The two-incision technique. Knee Surg Sports Traumatol Arthrosc. 2006;33:510–516. doi: 10.1007/s00167-005-0029-y. [DOI] [PubMed] [Google Scholar]
- 15.Siebold R, Schuhmacher P, Fernandez F, et al. Flat midsubstance of the anterior cruciate ligament with tibial “C”-shaped insertion site. Knee Surg Sports Traumatol Arthrosc in press, available online 20 May, 2014. doi:10.1007/s00167-014-3058-6. [DOI] [PMC free article] [PubMed]
- 16.Han Y., Kurzencwyg D., Hart A., Powell T., Martineau P.A. Measuring the anterior cruciate ligament’s footprints by three-dimensional magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20:986–995. doi: 10.1007/s00167-011-1690-y. [DOI] [PubMed] [Google Scholar]
- 17.Helito C.P., Helito P.V., Bonadio M.B. Evaluation of the anterolateral ligament length and isometric pattern with serial computer tomography. Orthop J Sports Med. 2014;2 doi: 10.1177/2325967114562205. 2325967114562205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parsons E.M., Gee A.O., Spiekerman C., Cavanagh P.R. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:669–674. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chambat P., Guier C., Sonnery-Cottet B., Fayard J.M., Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37:181–186. doi: 10.1007/s00264-012-1759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vadalà A.P., Iorio R., De Carli A. An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop. 2013;37:187–192. doi: 10.1007/s00264-012-1571-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dejour D., Vanconcelos W., Bonin N., Saggin P.R. Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop. 2013;37:193–199. doi: 10.1007/s00264-012-1718-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monaco E., Labianca L., Conteduca F., De Carli A., Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15:1168–1174. doi: 10.1007/s00167-007-0368-y. [DOI] [PubMed] [Google Scholar]
- 23.Trojani C., Beaufils P., Burdin G. Revision ACL reconstruction: Influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc. 2012;20:1565–1570. doi: 10.1007/s00167-011-1765-9. [DOI] [PubMed] [Google Scholar]
- 24.Helito C.P., Helito P.V.P., Costa H.P. MRI evaluation of the anterolateral ligament of the knee: Assessment in routine 1.5-T scans. Skeletal Radiol. 2014;43:1421–1427. doi: 10.1007/s00256-014-1966-7. [DOI] [PubMed] [Google Scholar]
- 25.Claes S., Bartholomeeusen S., Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg. 2014;80:45–49. [PubMed] [Google Scholar]
- 26.Mariscalco M.W., Flanigan D.C., Mitchell J. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29:1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Combined anterior cruciate ligament and anterolateral ligament reconstruction in a left knee.


