Abstract
Objective
To investigate contemporary geographic distributions of lung-function impairment and radiographic evidence of coal workers' pneumoconiosis (CWP) and their associations.
Methods
From 2005 to 2009, 6373 underground coal miners completed a health survey, including spirometry testing and chest radiography. Coal workers' pneumoconiosis and progressive massive fibrosis were determined by NIOSH B readers, using the International Labour Office classification. Prevalences of CWP and spirometry less than lower normal limits were mapped by county, and their associ ation assessed.
Results
The prevalences of abnormal spirometry results and CWP were 13.1% and 4.0%, respectively. Counties with elevated prevalences for both the outcomes were located in contiguous areas of southeastern Kentucky, western Virginia, southern West Virginia, and eastern Pennsylvania. Prevalence of abnormal spirometry results increases with increasing category of simple CWP and progressive massive fibrosis.
Conclusions
Abnormal spirometry in coal miners is associated with CWP; these two health outcomes have similar geographic distributions.
The US Coal Mine Health and Safety Act became a law in 1969, establishing an enforceable federal limit on the exposure of underground miners to respirable coal mine dust.1 The goal of the Act was to prevent the severe and lethal forms of pneumoconiosis that were prevalent at that time among coal miners in the United States. It was acknowledged that the exposure limit would not fully protect miners' lung health, so the legislation also provided working-underground coal miners with a program of periodic chest x-ray (CXR) surveillance, known as the Coal Workers' X-ray Surveillance Program (CWXSP), administered by National Institute for Occupational Safety and Health (NIOSH). In the first 30 years of enforcement of the dust limit, an 89% decline was observed in the prevalence of coal workers' pneumoconiosis (CWP) on surveillance CXR examinations of US miners who had worked at least 30 years underground.2 During the same period, a decline of similar magnitude was observed in the premature mortality from CWP. 3 Nevertheless, from about 2000, national data have shown increases in both morbidity and mortality from CWP.2,3 In addition, for some coal miners who participated in surveillance between 1996 and 2002, serial CXR examinations showed that pneumoconiosis had progressed rapidly to advanced and lethal stages. 4
In response to these latter findings, starting in 2005, NIOSH implemented a new Enhanced Coal Workers' Health Surveillance Program (ECWHSP).5 The ECWHSP focused on geographic regions where rapidly progressive CWP had recently been observed,4 as well as areas with lower participation in the ongoing CWXSP. In contrast to the CWXSP, which is limited to CXR examinations done at independent facilities arranged by coal mine operators, all the ECWHSP examinations are done in a mobile unit by NIOSH staff. Because coal miners may also develop lung-function impairment in relation to workplace risk factors,6–10 the ECWHSP included spirometry testing along with the CXR examination.
In light of the geographic clustering of rapidly progressive radiographic changes among underground coal miners,4 we mapped results from the ECWHSP to display the concurrent county-based prevalences of abnormal spirometry results and radiographic pneumoconiosis. We sought to explore evidence for a geographic association between these two health outcomes, as well as to provide additional data in relation to the ongoing controversy concerning the relationship between simple CWP and lung impairment. 9,10
METHODS
Health data collection occurred with the approval of the NIOSH institutional review board in the NIOSH mobile examination unit stationed in coal mining regions. All participants provided informed consent.
Participants
Between September 2005 and October 2009, 6854 underground coal miners participated in the ECWHSP. The current analysis is based on the 6373 miners with valid results from both spirometry and CXR examinations.
CXR Determinations
All CXR examinations were classified independently by two NIOSH B readers (or three, when necessary to resolve nonconcurrence of the first two classifications)* according to the 2000 International Labour Office classification system for pneumoconiosis, using a standardized form for recording dust-related abnormalities.11 A miner's CXR was determined to show simple CWP (small opacity profusion category ≥ 1/0 without large opacities) or progressive massive fibrosis (PMF; CWP with large opacity category≥A), when the finding was reported by at least two of the B readers.
Spirometry Testing
Spirometry testing was conducted by trained technicians, using a SensorMedics dry-rolling seal spirometer, model #922 (Occupational Marketing, Inc, Houston, TX), software version 5.05.12, and interpreted in accordance with the 2005 American Thoracic Society and European Respiratory Society guidelines12,13; tests with at least two acceptable curves showing maximum effort were included for analysis. Lower limits of normal (LLN) were calculated for forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and their ratio (FEV1/FVC), using prediction equations on the basis of the data from the Third National Health and Nutrition Examination Survey.14
Patterns of abnormality were defined as follows:
Obstructive : FEV1/FVC < LLN; FVC > LLN; and FEV1 < LLN
Restrictive : FEV1/FVC > LLN; and FVC < LLN
Mixed : FEV1/FVC < LLN; and FVC < LLN
Geographic Distributions of Abnormalities
Geographic distributions of the prevalences of CWP and of abnormal spirometry results were calculated at the county level by using SAS, software version 9.0 (SAS Institute, Cary, NC) and mapped by using MapInfo Professional, version 9.5 (MapInfo Corp, Troy, NY). Of the 92 counties with examinees in 15 states, only 77 counties in 13 states had more than five participants and were included in mapping. The cut points used to display the prevalence categories were derived by using the SAS Univariate procedure: The prevalence values at the first and third quartiles and at the median were used to group the 77 counties into four categories for CWP and abnormal spirometry results, respectively.
Data Analysis
Statistical analysis was performed, using the SAS software version 9.0 (SAS/STAT user's guide, version 9; 2002).
Group Comparisons
Group comparisons for continuous variables were made, using t tests for two groups and analysis of variance for three groups; chi-square tests were used for dichotomous variables between two groups and Cochran-Mantel-Haenszel statistics for more than two groups.
Prevalence Ratio Regression Analysis (SAS Proportional Hazards Regression)
The association between spirometric and radiographic abnormal results was further evaluated, using a modification of the Cox proportional hazards model, controlling for age, body mass index (BMI), tenure (years) in underground mining, and smoking status. The prevalence rate ratio15,16 from the model was considered a measure of the strength and significance of the association. Spirometry results were entered as a categorical variable (normal vs abnormal). The presence of abnormal spirometry results was examined for any influence of covariables, including age, BMI, tenure, smoking status, and CWP status, using partial likelihood estimates of the Cox regression coefficients, prevalence rate ratios, and Pearson correlation coefficients.
RESULTS
Population Characteristics
The 6373 underground coal miners included in the analysis were from 92 counties in a total of 15 states and included 6155 white men (96.6%) and 73 women (1.2%) and 131 black men (2.1%) and 14 women (0.2%). Age ranged from 18 to 74 years (mean, 47 years). There were 22% current smokers, 28% former smokers, and 50% never smokers; 38% were overweight (BMI, 25 to 29 kg/m2) and 51% obese (BMI, 30 kg/m2 or more).
Chest Radiograph Results
A total of 255 miners (4.0%) were determined to have CWP, including 183 cases in small opacity profusion category 1, 61 in category 2, and 11 in category 3. The crude PMF prevalence was 0.71% (45 of 255), including 14 cases in large opacity category A, 27 in category B, and 4 in category C. The prevalences of both CWP and PMF increased with age and tenure; significantly higher prevalences were observed in miners older than 40 years or with 20 years or longer of mining tenure.
Among the 13 states with at least 5 participating miners (see Fig. 1), only two states had no miners with CWP (New Mexico and Maryland, with 28 and 29 participants, respectively). The prevalences of simple CWP and PMF were highest in Kentucky (6.90% and 1.38%, respectively), followed by Virginia (6.61% and 1.31%, respectively), West Virginia (3.66% and 1.15%, respectively), Tennessee (2.56% and 0.00%, respectively), and Pennsylvania (2.42% and 0.28%, respectively). For the remaining 8 states, prevalence of simple CWP ranged from 0 to 1.77%, and PMF ranged from 0 to 0.29%.
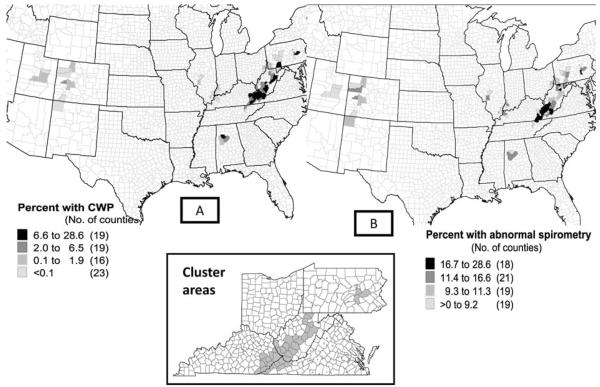
FIGURE 1.
Prevalences of CWP (A) and abnormal spirometry results (B) by county among 6373 underground coal miners in the Enhanced Coal Workers' Health Surveillance Program, 2005 to 2009, including 77 counties with at least five participating miners. Inset shows counties included in the cluster area.
Spirometry Measurements
Abnormal spirometry results were detected in 13.1% (836 of 6373) of miners—6.4% with restrictive, 5.4% with obstructive, and 1.3% with mixed impairment. Average percentage predicted values of spirometry indices differed significantly among miners with either PMF or simple CWP (Table 1) compared to those without. Table 2 displays group comparisons of demographics and spirometry measurements by simple CWP small opacity profusion categories; all spirometry values decrease as the x-ray small opacity profusion category increases, even excluding the 45 miners with PMF. Among all 6373 participants, the prevalences of abnormal spirometry results were 12.5% for miners with a CXR in category 0, 24.9% for category 1, 28.9% for categories 2 and 3 (P < 0.0001; Cochran-Mantel-Haenszel statistics), and 40% for those with PMF. Table 3 shows the differences of demographics and CWP prevalence between groups of lung-function impaired and not impaired miners. Among 836 miners with abnormal spirometry results, only 9% (72 of 836) had CWP.
TABLE 1.
Mean Age, BMI, and Spirometry Results by CWP Status (N = 6373)*
| No CWP (n = 6118) | Simple CWP (n = 210 | PMF (n = 45) | |
|---|---|---|---|
| Age, y | 46.7B | 52.4A | 51.4A |
| BMI, kg/m2 | 30.2A | 29.0A | 27.5B |
| PP FEV1, % | 96.6A | 90.2B | 81.9C |
| PP FVC, % | 99.1A | 96.2A | 91 9B |
| PP FEF25–75, % | 93.9A | 79.8B | 68.7C |
| PP PEF, % | 100.7A | 93.9B | 83.6C |
| FEV1/FVC, % | 76.5A | 72.5B | 69.9C |
One-way analysis of variance, using Duncan statistics for testing; means with the same letter are not significantly different, ie, p > 0.05.
BMI, body mass index; CWP, coal workers' pneumoconiosis; FEF, forced midexpiratory flow rate; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; PEF, peak expiratory flow; PMF, progressive massive fibrosis; PP, percentage predicted; y, years.
TABLE 2.
Mean Age, BMI, and Spirometry Results by X-Ray Small Opacity Category (n = 6328)*
| X-Ray Small Opacity Profusion Category |
|||
|---|---|---|---|
| Category 0 (n = 6118) | Category 1 (n = 165) | Categories 2 and 3 (n = 45) | |
| Age, y | 46.7B | 52.5A | 52.0A |
| BMI, kg/m2 | 30.2A | 29.0A | 28.9A |
| PP FEV1, % | 96.6A | 90.6B | 88.7B |
| PP FVC, % | 99.1A | 97.0A | 93.0B |
| PP FEF25–75, % | 93.9A | 79.5B | 81.0B |
| PP PEF, % | 100.7A | 94.4B | 92.0B |
| FEV1/FVC, % | 76.5A | 72.2B | 73.9B |
A total of 45 cases of progressive massive fibrosis were excluded from this analysis.
One-way analysis of variance using Duncan statistics for testing; means with the same letter are not significantly different, ie, p > 0.05.
BMI, body mass index; FEV, forced midexpiratory flow rate; FEF, forced midexpiratory flow rate; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; PEF, peak expiratory flow; PP, percentage predicted; y, years.
TABLE 3.
Demographics and CWP Prevalence by Lung Function Status (N = 6373)*
| Impaired (n = 836) | Not Impaired (n = 5537) | P | |
|---|---|---|---|
| Age, mean (SD; range), y | 48.6 (9.3; 21–74) | 46.6 (10.6; 18–74) | <0.0001 |
| Weight, mean (SD; range), kg | 96.9 (20.2; 49.5–202.7) | 92.8 (16.6; 47.7–183.2) | <0.0001 |
| Tenure underground, mean (SD; range), y | 19.3 (12.8; 0–58) | 18.1 (12.9; 0–60) | <0.05 |
| Current smoker, n (%) | 303 (36.2) | 1105 (20.0) | <0.0001 |
| BMI ≥ 30 kg/m2, n (%) | 476 (56.9) | 2776 (50.1) | <0.001 |
| Simple CWP, n (%) | 54 (6.60) | 156 (2.83) | <0.0001 |
| PMF, n (%) | 18 (2.15) | 27 (0.49) | <0.0001 |
Sex, race, and height not significantly different between the two groups.
BMI, body mass index; CWP, coal workers' pneumoconiosis; PMF, progressive massive fibrosis; y, years.
Geographic Distributions of CWP and Abnormal Spirometry Results
Figure 1 illustrates the prevalences of CWP and abnormal spirometry results by county. Only 77 counties with more than five participating miners were included in the mapping. The ranking of the 77 counties is similar whether ordered by the prevalence of abnormal spirometry results or by the prevalence of CWP (Wilcoxon signed rank test; P = 0.74). There were 26 individual counties in which the prevalence of both CWP and abnormal spirometry results were more than the median. Nearly all of these counties were located either in the region covered by southeastern Kentucky, western Virginia, and southern West Virginia or were in Pennsylvania. The 37 contiguous counties located in these areas were defined as the cluster areas (see Fig. 1 inset). When compared with miners from all other areas combined, miners located in the cluster areas showed five times more simple CWP, sixteen times more PMF, and 60% more spirometry abnormal results; they were slightly younger (46.5 vs 47.2 years) and had slightly longer underground mining tenure (21.7 vs 18.8 years). The estimates of prevalence ratios (95% confidence interval) for simple CWP, PMF, and abnormal spirometry results were 5.3 (3.7 to 7.5), 16.5 (5.1 to 53.3), and 1.6 (1.4 to 1.9), respectively, all highly significant (Table 4).
TABLE 4.
Group Comparisons by Geographic Location (N = 6373)
| Cluster Areas (n = 2945) | Other Location (n = 3428) | P | |
|---|---|---|---|
| Age, mean (SD; range), y | 46.5 (10.0; 18–74) | 47.2 (10.8; 18–74) | <0.05 |
| Height, mean (SD; range), cm | 175.6 (6.6; 138.4–200.7) | 176.1 (6.9; 142.2–198.1) | <0.01 |
| Weight, mean (SD; range), kg | 93.4 (17.1; 47.7–202.7) | 93.3 (17.2; 50.0–178.2) | 0.7408 |
| Tenure underground, mean (SD; range), y | 21.7 (11.2; 1–45) | 18.8 (12.1; 0–50) | <0.0001 |
| men, n (%) | 2933 (99.6) | 3353 (97.8) | <0.0001 |
| Race-White, n (%) | 2919 (99.1) | 3309 (96.5) | <0.0001 |
| Current Smoker, n (%) | 728 (24.7) | 680 (19.9) | <0.0001 |
| BMI ≥ 30 kg/m2, n (%) | 1541 (52.3) | 1711 (49.9) | <0.05 |
| Simple CWP, n (%) | 170 (5.86) | 40 (1.17) | <0.0001 |
| PMF, n (%) | 42 (1.43) | 3 (0.09) | <0.0001 |
| Spi-abn, n (%) | 475 (16.1) | 361 (10.5) | <0.0001 |
BMI, body mass index; CWP, coal workers' pneumoconiosis; PMF, progressive massive fibrosis; Spi-abn, abnormal spirometry results; y, years.
Association of Pneumoconiosis and Abnormal Spirometry Results—Cox Proportional Hazards Models
Table 5 shows results from the Cox proportional hazards analysis of the association of lung-function impairment with CWP and PMF. After adjustment for age, BMI, underground tenure, and cigarette smoking, the estimated prevalence rate ratios imply that a coal miner with simple CWP would have 1.8-fold greater risk of suffering abnormal lung function than a miner without CWP (model 3) and that a miner with PMF would have a 3.7-fold greater risk of lung-function impairment than a miner without PMF (model 2).
TABLE 5.
Results From Cox Proportional Hazards Models of Abnormal Spirometry Resultsa
| Model 1 (All Variables, Including Both CWP, PMF; n = 6372b) |
Model 2 (210 Simple CWP Excluded; n = 6162b) |
Model 3 (45 Miners With PMF Excluded; n = 6327b) |
||||
|---|---|---|---|---|---|---|
| Variable | Coefficient (SE) | Prevalence Ratio | Coefficient (SE) | Prevalence Ratio | Coefficient (SE) | Prevalence Ratio |
| Age, y | 0.018 (0.004) | 1.02*** | 0.018 (0.004) | 1.02*** | 0.018 (0.004) | 1.02*** |
| BMI, kg/m2 | 0.046 (0.006) | 1.05*** | 0.047 (0.006) | 1.05*** | 0.046 (0.006) | 1.05*** |
| Tenure underground, y | −0.0002 (0.003) | 1.00 | −0.0001 (0.003) | 1.00 | −0.0005 (0.003) | 1.00 |
| Current smoker (1, 0) | 0.808 (0.074) | 2.24*** | 0.809 (0.076) | 2.25*** | 0.821 (0.074) | 2.27*** |
| PMF (1, 0) | 0.724 (0.273) | 2.06* | 1.309 (0.240) | 3.70*** | NA | NA |
| CWP (1, 0) | 0.583 (0.143) | 1.79*** | NA | NA | 0.582 (0.143) | 1.79*** |
P < 0.01;
P < 0.0001.
Model 1—full model, independent variables for both CWP and PMF. Model 2—210 simple CWP not included in the model. Model 3—excluding 45 cases of PMF.
One subject missing underground tenure.
BMI, body mass index; CWP, coal workers' pneumoconiosis; NA, not applicable; PMF, progressive massive fibrosis; y, years.
DISCUSSION AND CONCLUSIONS
To reduce miners' risk of occupational pneumoconiosis, legislation was passed in 1969 that mandated controls for respirable dust in underground coal mines.1 Between 1970 and 1995, morbidity and mortality from CWP among United States miners improved greatly.2,3 Nevertheless, in 2005, Antao and colleagues4 described geographic clustering of rapidly progressive pneumoconiosis; and following that publication, an increase has been reported in the overall prevalence and severity of pneumoconiosis in US coal miners.2,17
Recent studies have generally not reported lung function among US miners. To address this issue, we assessed contemporary geographic patterns of abnormal spirometry results and associations with radiographic pneumoconiosis by using data collected by the ECWHSP from 2005 to 2009.5 Although only a small minority of the miners with abnormal spirometry results had CWP, the results demonstrated a clear relationship between increasing radiographic profusion of small pneumoconiotic opacities and lung-function impairment, after accounting for other relevant factors, including age, BMI, underground mining tenure, and tobacco smoking. Among miners with PMF, an even greater proportion showed impairment. The development of PMF has long been recognized as a cause of abnormal spirometry results. In contrast, an association of simple CWP and reduced lung function has recently been reported, after adjusting for age, smoking, and exposures;18 but this effect was not observed in several earlier studies.19,20 It has been suggested that the impact of simple pneumoconiosis on lung function became identifiable only after investigators used a more recent revision of the International Labour Office classification system, which provided recognition not just of rounded small opacities but also of small opacities of irregular shape.21 Small irregular radiographic opacities are known to increase with cumulative coal mine dust exposure and have been associated with reduced lung function21; they are often the predominant type of opacity recorded in US coal miners.22
Mapping of these surveillance data also suggests a similarity in the geographic distribution (by county) of abnormal spirometry results and radiographic evidence of CWP. Elevated proportions of both of these abnormalities generally seemed to cluster in coal mining areas in which rapidly progressive CWP was previously reported.4
One limitation of our analysis is that the participation in health surveillance programs is voluntary. The ECWHSP staff encouraged involvement among miners working in regions with prior low participation in the CWXSP as well as in the recognized “hot spot” areas, and over half the results reported here were from miners outside of the defined cluster areas. Nevertheless, unidentified participation biases may still have affected the results. In addition, exposures were not measured. Many studies have firmly associated the level of exposure to respirable mine dust with both radiographic pneumoconiosis and lung-function deficits.9 The inclusion of underground tenure in the model (Table 5) may not have fully accounted for impairment related to dust exposures. In addition to dusts, in some mines, other respiratory hazards may be present, such as blasting gases, diisocyanates, and bioaerosols. For the miners included in the current analysis, the specific cause(s) of the lung impairments observed cannot be determined with certainty. Nevertheless, the similarity in geographic clustering of two respiratory disorders suggests that the working environments responsible for the increasing prevalence and radiographic severity of pneumoconiosis among US coal miners may also be a risk for important abnormalities in ventilatory lung function.
In 1995, NIOSH recommended that the permissible limit for respirable coal mine dust be further reduced from 2 to 1 mg/m3, on the basis of an extensive review of the literature regarding coal miners' risks for pneumoconiosis and lung-function impairments.9 A 2011 review of the science reaffirmed that recommendation.10 A growing body of recent literature indicates that serious and fatal occupational lung diseases are continuing to occur among both underground and surface coal miners in the United States.23–26 These current surveillance results document radiographic changes of pneumoconiosis among working US coal miners in nearly all coal mining states and associate the presence of radiographic abnormal results with a significant likelihood of lung impairment.
SUMMARY
Results from surveillance examinations of 6373 working US coal miners undertaken from 2005 to 2009 demonstrate geographic clustering of both lung-function abnormalities and radiographic pneumoconiosis. The findings support the recommendation that underground coal miners should be offered spirometry monitoring to facilitate prompt detection of important functional abnormalities and reinforce the need to better protect US coal miners from both pneumoconiosis and significant reductions in lung function.9,10,27,28
Acknowledgments
Funded by National Institute for Occupational Safety and Health.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of National Institute for Occupational Safety and Health. Mention of a specific product or company does not constitute endorsement by the Centers for Disease Control and Prevention.
No conflicts of interest declared.
NIOSH operates a system for assessing proficiency in classification of pneumoconiosis. Physicians seeking to become NIOSH B Readers (http://www.cdc.gov/niosh/topics/chestradiography/breader.html) must pass a certification examination, and recertify every 4 years.
REFERENCES
- 1.Federal Coal Mine Health and Safety Act. 1969 Public Law no. 91–173.
- 2.Centers for Disease Control and Prevention . Work-Related Lung Disease Surveillance Report 2007. US Department of Health and Human Services, Centers for Disease Control and Prevention; Cincinnati, OH: [Accessed July 19, 2012]. 2008. DHHS (NIOSH) publication no. 2008-143a. Available at: http://www.cdc.gov/niosh/docs/2008-143. [Google Scholar]
- 3.Centers for Disease Control and Prevention Coal workers' pneumoconiosis-related years of potential life lost before age 65 years—United States, 1968–2006. MMWR Morb Mortal Wkly Rep. 2009;58:1412–1416. [PubMed] [Google Scholar]
- 4.Antao VC, Petsonk EL, Sokolow LZ, et al. Rapidly progressive coal workers' pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med. 2005;62:670–674. doi: 10.1136/oem.2004.019679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Occupational Safety and Health [Accessed May 22, 2012];Enhanced Coal Workers' Health Surveillance Program (ECWHSP) Available at: http://www.cdc.gov/niosh/topics/surveillance/ords/ecwhsp.html. Published March 9, 2011.
- 6.Wang ML, Petsonk EL, Beeckman LF, Wagner GR. Clinically important FEV1 declines among coal miners: an exploration of previously unrecognized determinants. Occup Environ Med. 1999;56:837–844. doi: 10.1136/oem.56.12.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beeckman LF, Wang ML, Wagner GR, Petsonk EL. Accelerated declines in FEV1 and subsequent increased respiratory symptoms, illnesses, and mortality in coal miners. Am J Respir Crit Care Med. 2001;163:633–639. doi: 10.1164/ajrccm.163.3.2008084. [DOI] [PubMed] [Google Scholar]
- 8.Wang ML, Wu ZE, Du QG, et al. Rapid decline in forced expiratory volume in 1 second (FEV1) and the development of bronchitic symptoms among new Chinese coal miners. J Occup Environ Med. 2007;49:1143–1148. doi: 10.1097/JOM.0b013e31814b8d51. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Occupational Safety and Health . Criteria for a Recommended Standard: Occupational Exposure to Coal Mine Dust. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; Washington, DC: 1995. p. 336. DHHS (NIOSH) publication no. 95–106. [Google Scholar]
- 10.Attfield M, Hale J, Suarthana E, Wang ML, Castranova V, Clough-Thomas K. Current Intelligence Bulletin 64: Coal Mine Dust Exposures and Associated Health Outcomes—a Review of Information Published Since 1995. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; Cincinnati, OH: 2011. p. 38. DHHS (NIOSH) publication no. 2011-172. [Google Scholar]
- 11.International Labour Office . Guidelines for the Use of the ILO International Classification of Radiographs of Pneumoconioses. International Labour Office; Geneva, Switzerland: 2002. [Google Scholar]
- 12.American Thoracic Society/European Respiratory Society Standardization of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 13.American Thoracic Society/European Respiratory Society Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 14.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 15.Lee J, Chia KS. Estimation of prevalence rate ratios for cross-sectional data: an example in occupational epidemiology. Br J Ind Med. 1993;50:861–862. doi: 10.1136/oem.50.9.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zocchetti C, Consonni D, Bertazzi PA. Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol. 1995;24:1064–1065. doi: 10.1093/ije/24.5.1064. [DOI] [PubMed] [Google Scholar]
- 17.Laney AS, Attfield MD. Coal workers' pneumoconiosis and progressive massive fibrosis are increasingly more prevalent among workers in small underground coal mines in the United States. Occup Environ Med. 2010;67:428–431. doi: 10.1136/oem.2009.050757. [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Yu IT, Wong TW, Yano E. Respiratory symptoms and pulmonary function in coal miners: looking into the effects of simple pneumoconiosis. Am J Ind Med. 1999;35:124–131. doi: 10.1002/(sici)1097-0274(199902)35:2<124::aid-ajim3>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 19.Cochrane AL, Higgins IT. Pulmonary ventilatory functions of coalminers in various areas in relation to the x-ray category of pneumoconiosis. Br J Prev Soc Med. 1961;15:1–11. doi: 10.1136/jech.15.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogan JM, Attfield MD, Jacobsen M, Rae S, Walker DD, Walton WH. Role of dust in the working environment in the development of chronic bronchitis in British coal miners. Br J Ind Med. 1973;30:217–226. doi: 10.1136/oem.30.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collins HP, Dick JA, Bennett JG, et al. Irregularly shaped small shadows on chest radiographs, dust exposure, and lung function in coalworkers' pneumoconiosis. Br J Ind Med. 1988;45:43–55. doi: 10.1136/oem.45.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laney AS, Petsonk EL. Small pneumoconiotic opacities on U.S. coal worker surveillance chest radiographs are not predominantly in the upper lung zones. Am J Ind Med. 2012;55:793–798. doi: 10.1002/ajim.22049. [DOI] [PubMed] [Google Scholar]
- 23.Petsonk EL, Parker JE. Coal workers' lung diseases and silicosis. In: Fishman AP, Fishman JA, Grippi MA, Kaiser LB, Senior RM, editors. Fishman's Pulmonary Diseases and Disorders. 4th McGraw-Hill; New York, NY: 2008. pp. 967–980. [Google Scholar]
- 24.Wade WA, Petsonk EL, Young B, Mogri I. Severe occupational pneumoconiosis among West Virginian coal miners: one hundred thirty-eight cases of progressive massive fibrosis compensated between 2000 and 2009. Chest. 2011;139:1458–1462. doi: 10.1378/chest.10-1326. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Laney AS, Wolfe AL, Petsonk EL, Halldin CN. Pneumoconiosis and advanced occupational lung disease among surface coal miners—16 states, 2010–2011. MMWR Morb Mortal Wkly Rep. 2012;61:431–434. [PubMed] [Google Scholar]
- 26.Suarthana E, Laney AS, Storey E, Hale JM, Attfield MD. Coal workers' pneumoconiosis in the United States: regional differences 40 years after implementation of the 1969 Federal Coal Mine Health and Safety Act. Occup Environ Med. 2011;68:908–913. doi: 10.1136/oem.2010.063594. [DOI] [PubMed] [Google Scholar]
- 27.National Institute for Occupational Safety and Health . OSHA–NIOSH Info Sheet: Maximize Your Spirometry Screening and Surveillance Resources. Division of Respiratory Disease Studies, National Institute for Occupational Safety and Health; Morgantown, WV: 2011. DHHS (NIOSH) publication no. 2011–133. [Google Scholar]
- 28.National Institute for Occupational Safety and Health . OSHA–NIOSH Worker Info: Protect Yourself—Spirometry Breathing Test. Division of Respiratory Disease Studies, National Institute for Occupational Safety and Health; Morgantown, WV: 2011. DHHS (NIOSH) publication no. 2011–132. [Google Scholar]