Abstract
Several surgical techniques have been described for the treatment of talar chondral lesions. Among them, microfracture is well established. Autologous matrix-induced chondrogenesis (AMIC), using microfracture and biomaterials, has shown promising results for the treatment of knee osteochondral lesions and has been proposed for the ankle as an open technique. We describe an all-arthroscopic AMIC technique. The benefits of an all-arthroscopic procedure include smaller incisions with less soft-tissue dissection, better visualization of the joint, and a quicker recovery compared with open surgery. The use of matrix to support cartilage regeneration promotes good-quality cartilage tissue with satisfactory long-term outcomes. Our all-arthroscopic AMIC technique uses a type I–type III porcine collagen matrix (Chondro-Gide; Geistlich Pharma, Wolhusen, Switzerland) and is characterized by 2 different arthroscopic surgical phases. First, adequate exposure is achieved through use of a Hintermann spreader (Integra LifeSciences, Plainsboro, NJ) with sufficient joint distraction and wet lesion preparation. The second surgical step is performed dry, involving matrix placement and fixation. The all-arthroscopic AMIC technique for the treatment of osteochondral lesions of the talus allows a very precise reconstruction in the case of cartilage defects and avoids the need for a more invasive operation associated with higher morbidity and a longer surgical time.
Ankle pain is often encountered in young persons who actively participate in sports. One of the main sources of ankle pain is sprains that can cause instability and talar chondral lesions. Chronic instability resulting from recurrent sprains is suspected as the major cause of chronic talar osteochondral lesions.1
The most described treatment in the literature is microfracture therapy,2 but long-term follow-up and ineffectiveness in regenerating hyaline cartilage are the main issues.3,4 Autologous matrix-induced chondrogenesis (AMIC) is a matrix-assisted microfracture technique that allows stabilization and protection of the blood clot derived from the subchondral bone, thus providing the bone marrow–derived mesenchymal stem cells with a regeneration chamber because the collagen matrix is able to retain them. This treatment has been designed to be performed by an open technique that often involves a medial malleolar osteotomy, which is associated with known morbidity.5 In an attempt to minimize morbidity, we have developed an all-arthroscopic AMIC technique using a type I–type III porcine collagen matrix (Chondro-Gide; Geistlich Pharma, Wolhusen, Switzerland) with smaller incisions, less soft-tissue dissection, better visualization of the joint, and a quicker patient recovery compared with the open technique (Table 1). The aim of this work is to describe our technique for the treatment of osteochondral lesions of the talus.
Table 1.
Indications and Contraindications for Arthroscopic Autologous Matrix-Induced Chondrogenesis Technique
| Indications |
| Osteochondral lesion |
| Lesion >1.0 cm2 |
| Age 18-55 yr |
| Primary or revision procedure |
| Contraindications |
| Metabolic arthropathy |
| Kissing lesions |
| Major defects (i.e., defects that cannot be reconstructed) |
| Non-correctable hindfoot malalignment |
| Systemic disorders |
| Obesity |
Surgical Technique
Preoperative planning involves clinical examination of both ankles with assessment of range of motion, point tenderness, and alignment of the hindfoot. Preoperative imaging includes a weight-bearing radiograph of the foot and ankle6 to assess any alignment issues and a magnetic resonance imaging (MRI) scan to study the cartilage defect (Fig 1).
Fig 1.

Preoperative radiographs. (A) Anteroposterior view and (B) lateral view of the ankle of a patient with an osteochondral lesion of the talus. (C) A preoperative magnetic resonance imaging scan (sagittal view) shows an osteochondral lesion of the talus, confirming the indication to perform the autologous matrix-induced chondrogenesis technique.
The procedure can be performed with the patient under either spinal or general anesthesia in the supine position, and the entire procedure is performed arthroscopically using anteromedial and anterolateral portal approaches for the ankle, with application of a thigh tourniquet at a pressure of 250 mm Hg in all patients (Video 1). Before the surgical procedure, we have found it useful to draw on the skin, with a dermographic pen, the tendons and bone surfaces that are easily palpable. During surgery, it is not uncommon for the soft tissues to become edematous, making them difficult to identify (Fig 2).
Fig 2.

Outside views of ankle during surgical planning: (A) frontal view and (B) lateral view. With the patient in the supine position, it is useful to identify all the landmarks on the joint needed for the surgical procedure and to mark the anteromedial and anterolateral arthroscopic portals.
The anteromedial portal is the first portal to be placed: It is located immediately medial to the anterior tibialis tendon, between the medial malleolus and the medial convexity of the talus just distal to the joint line. Care must be taken to avoid the saphenous vein because it is close to the described surgical area. For the anterolateral portal, the joint line is checked, and the portal is then positioned medial to the lateral malleolus and lateral to the extensor digitorum tendon. Attention must be taken to avoid superficial peroneal nerve damage; therefore it is necessary to cut only the skin and reach the capsule by blunt dissection.
The next step is to confirm the presence of the defect, as well as its size and shape. At this point, a Hintermann spreader (Integra LifeSciences, Plainsboro, NJ) is percutaneously placed to distract the joint and allow exposure of the lesion. The Hintermann spreader has an opening lever arm applied on two 2.5-mm K-wires previously positioned in the tibia and talar bone medially or laterally, according to the lesion side (Fig 3). In the case of a lateral lesion, care must be taken to insert the proximal K-wire in the tibial bone, avoiding the fibula, to achieve better distraction of the joint (Table 2). After identification and isolation of the lesion, the damaged cartilage, as well as the typically necrotic and sclerotic bone, is removed to create a regular-shaped site with shouldered borders. For this procedure, we typically use a standard arthroscopic curette. At this point, a 5.5-mm cannula is inserted through the closest portal to the lesion. To measure the lesion, an aluminum template (Geistlich Pharma), provided with the matrix kit, is introduced by the aforementioned cannula and adjusted on the lesion surface. It is important to bend the lateral edges of the template to be able to pass it through the cannula without damaging it.
Fig 3.
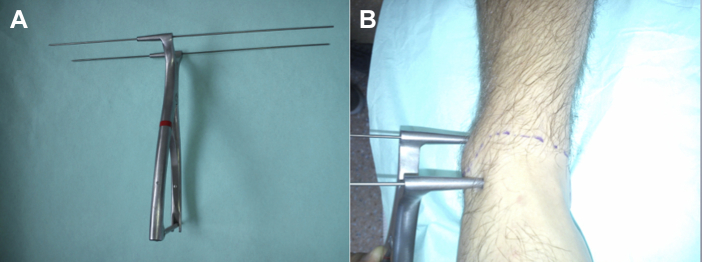
(A) Hintermann spreader with 2 pins measuring 2.5 mm. (B) Outside view. The spreader has been positioned on the medial side of the ankle, with the pin inserted at the level of the tibia and talus. This device allows better and safe distraction of the joint with good exposure.
Table 2.
Technical Pearls for Algorithm of Joint Distraction With Hintermann Spreader
| K-Wire Positioning |
|||
|---|---|---|---|
| Tibia | Talus | Fibula | |
| Medial lesion | Medial border | Medial surface | None |
| Lateral lesion | Lateral border | Lateral surface | None |
Microfractures are induced by a Chondro Pick (Arthrex, Naples, FL) on the healthy subchondral bone underneath the defect (Fig 4). This procedure is performed for the entire size of the lesion. At this time, the intra-articular water is removed by appropriate suction and the remaining liquid is dried using a cotton sponge. When needed, cancellous bone is harvested from the homolateral calcaneus with an accessory lateral approach on the calcaneus wall. The cancellous bone is introduced using the same cannula and impacted into the bony defect to fill it entirely. In the case of a shouldered lesion, it is important to completely fill the gap with cancellous harvested bone to restore the real anatomy. This procedure is technically more demanding when the lesion is on either the medial or lateral corner.
Fig 4.
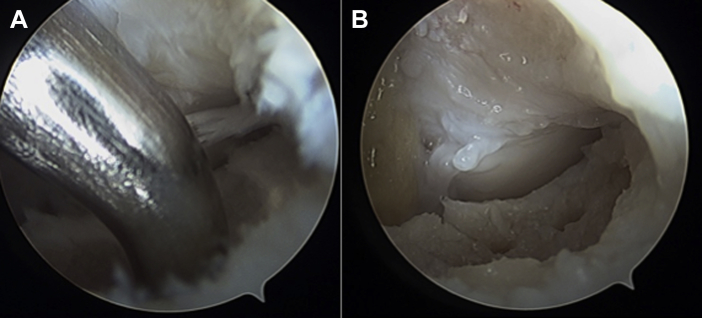
Arthroscopic views from anteromedial portal. (A) To stimulate bleeding, microfractures are made at the level of the osteochondral lesion covering the entire surface with the Chondro Pick inserted by the anterolateral portal. (B) Creation of microfractures at level of osteochondral lesion.
Next, the Chondro-Gide matrix is prepared according to the template, inserted through the cannula, and positioned at the lesion site (Fig 5A). When the correct matrix size is in doubt, downsizing the membrane is an advisable principle because it has the trend to be slightly oversized when it is introduced in such a wet environment as the ankle joint. Furthermore, to avoid upside-down positioning, it is useful to sign the top of the membrane with a dermographic pen before the implantation. Once the matrix fits the lesion perfectly, it is glued by synthetic fibrin glue (Tisseel; Baxter, Deerfield, IL) along the lesion edges (Fig 5B). At this moment, the Hintermann spreader is removed, and the stability of the matrix within a normal ankle range of motion is then arthroscopically checked (Table 3).
Fig 5.
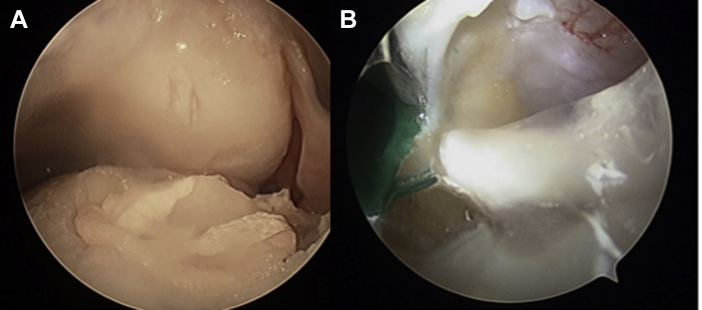
Arthroscopic views from anteromedial portal. (A) Correct positioning of the collagen membrane—inserted by the anterolateral portal and previously cut according to the template—at the level of the osteochondral lesion. (B) The collagen matrix is fixed with synthetic fibrin glue injected by a syringe through the 5.5-mm cannula.
Table 3.
Main Surgical Steps (Key Points) of Arthroscopic Autologous Matrix-Induced Chondrogenesis Technique for Treatment of Talar Osteochondral Lesions
| Placement of patient in supine position |
| Portal placement: anteromedial and anterolateral |
| Identification of lesion |
| Positioning of Hintermann spreader |
| Debridement and shaving of lesion |
| Microfracture |
| Measurement of lesion using template |
| Removal of water and drying of joint space |
| Harvesting of cancellous bone from homolateral calcaneus |
| Impaction of cancellous bone into bony defect |
| Preparation of Chondro-Gide matrix according to template |
| Matrix insertion through cannula |
| Matrix fixation by fibrin glue |
| Checking of stability of matrix within normal ankle range of motion |
Postoperative management requires movement restriction for 15 days to avoid membrane mobilization and no weight bearing for 40 days. The healing process is routinely monitored with an MRI scan at 6 months' follow-up (Fig 6).
Fig 6.
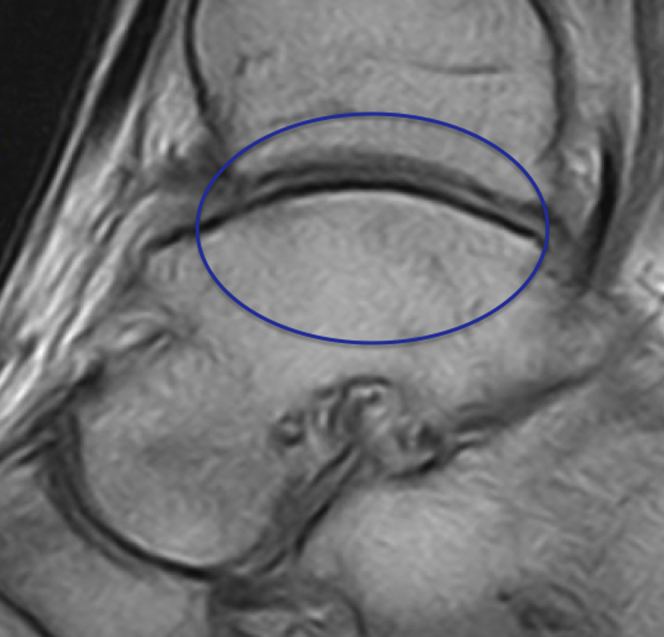
A postoperative magnetic resonance imaging scan (sagittal view) at 1 year of follow-up in a patient who underwent the autologous matrix-induced chondrogenesis technique for the treatment of an osteochondral lesion of the talus. The blue oval shows the healed ostechondral lesion after treatment with AMIC. The image shows satisfactory osteochondral healing.
Discussion
AMIC for the repair of cartilage defects has been used successfully for other joints for some years.7-9 This procedure for talar dome osteochondral lesions was first described by Wiewiorski et al.10; in this field, they reported excellent results in a case series of 42 patients with a minimum follow-up time of 12 months. Recently, AMIC has been defined as a safe and reliable procedure for the treatment of osteochondral lesions in the ankle with overall good clinical and MRI results.11
Up to now, the AMIC technique for osteochondral lesions of the talus has been performed with an arthrotomy approach, including a malleolar osteotomy, to achieve good talar dome exposure to successfully restore the dome anatomy. However, this approach is associated with a longer surgical time and described morbidity.5 The proposed advantages of this all-arthroscopic technique include smaller incisions with less soft-tissue dissection, thus resulting in patient benefits and cost-saving advantages in terms of a shorter hospital stay and faster return to work. Furthermore, the first arthroscopic step allows the status of the cartilage to be detected and accurately assessed, reducing the risk of overestimating the lesion size according to only MRI findings.
Notably, this arthroscopic procedure is a challenging operation, with a long learning curve, but the advantages related to this technique are significant compared to open techniques. We began using this technique more than 24 months ago and have seen no intraoperative or postoperative complications in 27 patients, although the technique can be associated with some possible complications (Table 4). Our results have shown sustained excellent outcomes. In conclusion, the all-arthroscopic AMIC technique for the treatment of osteochondral lesions of the talus allows a very precise reconstruction in the case of cartilage defects and avoids the need for a more invasive operation.
Table 4.
Possible Complications Related to Arthroscopic Autologous Matrix-Induced Chondrogenesis Technique for Treatment of Talar Osteochondral Lesions
| Matrix detachment |
| Unknown collagen allergy |
| Early membrane mobilization |
| Hyperproliferative healing reaction with subsequent joint impingement |
| Common ankle arthroscopy complications12 |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
From the standard anterior portal, it is possible to identify the lesion and begin preparation of the site. The microperforation procedure is shown. At the end of this step, the joint is dried and cleaned, and the autologous matrix-induced chondrogenesis membrane is positioned. Stability of the membrane is achieved with fibrin glue.
References
- 1.Savage-Elliott I., Ross K.A., Smyth N.A., Murawski C.D., Kennedy J.G. Osteochondral lesions of the talus: A current concepts review and evidence-based treatment paradigm. Foot Ankle Spec. 2014;7:414–422. doi: 10.1177/1938640014543362. [DOI] [PubMed] [Google Scholar]
- 2.Adams S.B., Jr., Demetracopoulos C.A., Parekh S.G., Easley M.E., Robbins J. Arthroscopic particulated juvenile cartilage allograft transplantation for the treatment of osteochondral lesions of the talus. Arthrosc Tech. 2014;3:e533–e537. doi: 10.1016/j.eats.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donnenwerth M.P., Roukis T.S. Outcome of arthroscopic debridement and microfracture as the primary treatment for osteochondral lesions of the talar dome. Arthroscopy. 2012;28:1902–1907. doi: 10.1016/j.arthro.2012.04.055. [DOI] [PubMed] [Google Scholar]
- 4.Ross K.A., Hannon C.P., Deyer T.W. Functional and MRI outcomes after arthroscopic microfracture for treatment of osteochondral lesions of the distal tibial plafond. J Bone Joint Surg Am. 2014;96:1708–1715. doi: 10.2106/JBJS.M.01370. [DOI] [PubMed] [Google Scholar]
- 5.Siegel S.J., Mount A.C. Step-cut medial malleolar osteotomy: Literature review and case reports. J Foot Ankle Surg. 2012;51:226–233. doi: 10.1053/j.jfas.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Saltzman C.L., el-Khoury G.Y. The hindfoot alignment view. Foot Ankle Int. 1995;16:572–576. doi: 10.1177/107110079501600911. [DOI] [PubMed] [Google Scholar]
- 7.Kusano T., Jakob R.P., Gautier E., Magnussen R.A., Hoogewoud H., Jacobi M. Treatment of isolated chondral and osteochondral defects in the knee by autologous matrix-induced chondrogenesis (AMIC) Knee Surg Sports Traumatol Arthrosc. 2012;20:2109–2115. doi: 10.1007/s00167-011-1840-2. [DOI] [PubMed] [Google Scholar]
- 8.Anders S., Volz M., Frick H., Gellissen J. A randomized, controlled trial comparing autologous matrix-induced chondrogenesis (AMIC) to microfracture: Analysis of 1- and 2-year follow-up data of 2 centers. Open Orthop J. 2013;7:133–143. doi: 10.2174/1874325001307010133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gille J., Behrens P., Volpi P. Outcome of autologous matrix induced chondrogenesis (AMIC) in cartilage knee surgery: Data of the AMIC Registry. Arch Orthop Trauma Surg. 2013;133:87–93. doi: 10.1007/s00402-012-1621-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiewiorski M., Leumann A., Buettner O., Pagenstert G., Horisberger M., Valderrabano V. Autologous matrix-induced chondrogenesis aided reconstruction of a large focal osteochondral lesion of the talus. Arch Orthop Trauma Surg. 2011;131:293–296. doi: 10.1007/s00402-010-1048-9. [DOI] [PubMed] [Google Scholar]
- 11.Valderrabano V., Miska M., Leumann A., Wiewiorski M. Reconstruction of osteochondral lesions of the talus with autologous spongiosa grafts and autologous matrix-induced chondrogenesis. Am J Sports Med. 2013;41:519–527. doi: 10.1177/0363546513476671. [DOI] [PubMed] [Google Scholar]
- 12.Carlson M.J., Ferkel R.D. Complications in ankle and foot arthroscopy. Sports Med Arthrosc. 2013;21:135–139. doi: 10.1097/JSA.0b013e31828e5c6c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
From the standard anterior portal, it is possible to identify the lesion and begin preparation of the site. The microperforation procedure is shown. At the end of this step, the joint is dried and cleaned, and the autologous matrix-induced chondrogenesis membrane is positioned. Stability of the membrane is achieved with fibrin glue.


