Summary
Background
The prevalence of male obesity is increasing but few men take part in weight loss programmes. We assessed the effect of a weight loss and healthy living programme on weight loss in football (soccer) fans.
Methods
We did a two-group, pragmatic, randomised controlled trial of 747 male football fans aged 35–65 years with a body-mass index (BMI) of 28 kg/m2 or higher from 13 Scottish professional football clubs. Participants were randomly assigned with SAS (version 9·2, block size 2–9) in a 1:1 ratio, stratified by club, to a weight loss programme delivered by community coaching staff in 12 sessions held every week. The intervention group started a weight loss programme within 3 weeks, and the comparison group were put on a 12 month waiting list. All participants received a weight management booklet. Primary outcome was mean difference in weight loss between groups at 12 months, expressed as absolute weight and a percentage of their baseline weight. Primary outcome assessment was masked. Analyses were based on intention to treat. The trial is registered with Current Controlled Trials, number ISRCTN32677491.
Findings
374 men were allocated to the intervention group and 374 to the comparison group. 333 (89%) of the intervention group and 355 (95%) of the comparison group completed 12 month assessments. At 12 months the mean difference in weight loss between groups, adjusted for baseline weight and club, was 4·94 kg (95% CI 3·95–5·94) and percentage weight loss, similarly adjusted, was 4·36% (3·64–5·08), both in favour of the intervention (p<0·0001). Eight serious adverse events were reported, five in the intervention group (lost consciousness due to drugs for pre-existing angina, gallbladder removal, hospital admission with suspected heart attack, ruptured gut, and ruptured Achilles tendon) and three in the comparison group (transient ischaemic attack, and two deaths). Of these, two adverse events were reported as related to participation in the programme (gallbladder removal and ruptured Achilles tendon).
Interpretation
The FFIT programme can help a large proportion of men to lose a clinically important amount of weight; it offers one effective strategy to challenge male obesity.
Introduction
Rising levels of obesity are a major challenge to public health. 11 million adults are expected to be obese in the UK by 2030, accruing to about 668 000 additional cases of diabetes, 461 000 cases of heart disease and stroke, 130 000 cases of cancer, and up to 6·3 million lost quality-adjusted lifeyears (QALYs), with associated medical costs set to increase by £1·9–2 billion per year by 2030.1 In Scotland, more men (69%) than women (60%) are overweight or obese.2
Although 5–10% weight loss can produce substantial health benefits,3 men are under-represented in trials of weight loss interventions (only 27% of participants are men),4 in referrals to commercial weight management programmes (between 11%5 and 13%6 are men), and in the UK’s National Health Service (NHS) weight management services (23%),7 suggesting a need for innovation in weight management for men. Increasing evidence suggests that men will engage with appropriately gender-sensitised weight management interventions and lose weight.8–10 Although findings of recent research have shown the potential of professional sports clubs, especially football (soccer) clubs,11 to engage men in lifestyle change, no controlled studies have been reported.10,12
Football Fans in Training (FFIT) is a weight loss and healthy living programme delivered to fans in Scottish professional football clubs under the auspices of the Scottish Premier League (SPL) trust, which became the Scottish Professional Football League (SPFL) trust in June, 2013. It is gender sensitised in context, content, and style of delivery.13,14 Findings of our feasibility study 9 showed that men could be recruited to a randomised trial in this context and that the programme had potential for ffecting sustained weight loss and positive lifestyle change.9 Here we report the effectiveness and cost-effectiveness of the programme in relation to bodyweight at 12 months.
Methods
Study design and participants
We undertook a two-group, pragmatic, randomised controlled trial to assess delivery of the FFIT programme in 13 Scottish professional football clubs in 2011–12 (12 clubs in the league in 2011–12 and one club that was relegated in 2010–11). Men were randomised with a computer-generated programme to receive intervention or comparator (1:1), stratified by club. We chose randomisation of individuals within clubs (rather than randomisation of clubs) because individual randomisation is more efficient unless contamination is a major risk,15 and the SPL trust were required by programme funders to deliver the programme in all clubs at the same time. Assessment of the primary outcome (mean difference in weight loss between groups at 12 months) was masked. The health economic assessment was undertaken from the NHS and UK Personal Social Service Research Unit (perspective favoured by the National Institute for Health and Care Excellence [NICE]). A summary of the protocol is available.
At the time of the trial, funding from the Scottish Government and The Football Pools (a UK national lottery) was available for three deliveries of the programme (August to December, 2011, February to April, 2012, and August to December, 2012) and we recruited enough men to fill all available places. Formal recruitment started on June 2, 2011, and continued until the week before the baseline measurements in each club, which took place between Aug 11, 2011, and Sept 20, 2011. Participants randomly allocated to the delivery in August to December, 2011, formed the intervention group; those randomly allocated to the August to December, 2012, delivery formed the waiting list comparison group and undertook the programme after the 12 month trial outcomes had been completed; men allocated to the February to April, 2012, delivery did not participate in the trial (their exclusion was pre-planned).
The recruitment strategy consisted of club-based recruitment (eg, club websites, in-stadiums advertising, and FFIT recruitment staff approaching potentially eligible men on match days), media coverage (eg, local and national newspapers, BBC Scotland, and independent radio), and other strategies (eg, staff emails through employers and word-of-mouth). Men were invited to contact the research team by SMS text, email, or telephone to register interest and self-report weight, height, and date of birth; those who expressed interest on match days were telephoned subsequently by the research team. All men whose self-reports suggested they were eligible were invited to participating club grounds for formal eligibility assessment.
Men were eligible if they were aged 35–65 years in 2011–12; had objectively measured body-mass index (BMI) of at least 28 kg/m2; completed the physical activity readiness questionnaire; consented to weight, height, and waist measurements; and had not taken part in FFIT previously. We included only men with BMI at least 28 kg/m2 for three reasons; these men are likely to want to lose weight; are likely to benefit from doing so; and our feasibility study found that men liked being with others with similar weight loss goals.14 Men whose blood pressure contraindicated vigorous exercise (systolic ≥160 mm Hg or diastolic ≥100 mm Hg) were excluded from participation in more intense physical activity during programme sessions until they could provide coaches with evidence of reduction in blood pressure. All men measured at baseline were given a British Heart Foundation booklet on weight management.16 Men were also informed of their weight and BMI, were advised to see their general practitioner if baseline readings of their blood pressure exceeded 140/80 mm Hg, and met club coaches who talked broadly about the programme and gave information about timing.
The University of Glasgow’s College of Social Sciences ethics committee (CSS/2011/029) complies with the UK Economic and Social Research Council’s Framework for Research Ethics and gave ethical approval. All participants provided written informed consent before participation and at each data collection point.
Randomisation and masking
After baseline measurement, the randomisation sequence was generated by the Tayside Clinical Trials Unit (TCTU) statistician (with no day to day role in the study at this point) with SAS (version 9.2), blocked (block size between two and nine dependent on how many participants were recruited at a club), and stratified by club. The allocation sequence was sent in a password-protected file to a database manager (not part of the research team) who assigned individuals to each group. Participants were informed by telephone or letter whether they had been allocated to undertake the programme within 3 weeks of baseline measurements at each club (the intervention group), or whether they had been allocated to the waiting list comparison group that could do the programme 12 months later.
To mask measurement of the primary outcome, weight was the first measure taken, in a screened-off area to prevent interaction with others, by fieldworkers employed only for 12 month measures who were trained to minimise interaction with men until weight had been recorded. Masking for the other measures was not possible.
Procedures
The development, optimisation, and content of the FFIT programme is described elsewhere.14 Briefly, the programme was designed to work with rather than against prevailing understandings of masculinity.13,14,17 The programme was gender sensitised in relation to context (the traditionally male environment of football clubs and men only groups), content (information about the science of weight loss presented simply, discussion of alcohol and its potential role in weight management, and branding with club insignia), and style of delivery (participative and peer-supported, which is learning that encouraged male banter to help with discussion of sensitive subjects). FFIT was delivered free of charge to participants by community coaching staff employed by clubs, trained over 2 days by the research team, to groups of up to 30 overweight or obese men (participant to coach ratio 15:1) during sessions every week for 12 weeks at the club’s home stadium. Each 90 min session combined advice on healthy diet with physical activity. The balance of classroom and physical activity sessions changed during the 12 weeks; later weeks focused on physical activity as men became fitter, and the shorter classroom sessions focused on revision. Coaches were available at the end of each session if any man wanted to discuss personal issues. Participants were also taught behavioural change techniques known to be effective in physical activity, and dietary interventions (eg, self-monitoring, specific goal setting, implementation intentions, and feedback on behaviour),18 and social support was promoted. The 12 week active phase was followed by a weight maintenance phase with six post-programme email prompts during 9 months and a group reunion at the club 6 months after the end of the sessions.
To assess fidelity, a team of three researchers observed 26 (two per club) of 156 planned delivery sessions. These 26 sessions consisted of 93 key delivery tasks. Observers judged the extent to which coaches delivered each of these tasks as intended with a structured proforma and took notes to explain their judgments. Coach interviews investigated ease of delivery. Coaches were asked to provide an attendance record for each session in the 12 week active phase of the programme.
Data were obtained at baseline, 12 weeks, and 12 months at club stadiums by teams of fieldworkers, who were trained in standard measurement and protocols of questionnaire administration. At baseline and 12 months the intervention and comparison groups were measured in the same sessions; to avoid contamination at 12 weeks, the intervention and comparison group were measured at different sessions. To maximise retention at 12 months men were sent a personalised letter to remind them about upcoming measurements; telephoned to arrange an appointment, which was confirmed by email or post; sent email reminders about a week before their session, and SMS text reminders about a day before their appointment; offered a home visit if attendance to the stadium was difficult; and offered a £40 club voucher to thank them for their time.
Secondary outcomes were: mean difference in weight loss between groups at 12 weeks expressed as absolute weight and percentage of baseline weight; and mean difference at 12 weeks and 12 months in waist circumference, BMI, percentage body fat, systolic and diastolic blood pressure, self-reported physical activity, self-reported diet, and self-reported psychological health and quality of life.
The primary outcome was mean difference in weight loss between groups at 12 months expressed as absolute weight and as a percentage of their baseline weight. Weight (kg) was recorded with electronic scales (Tanita HD 352, Middlesex, UK) with participants wearing light clothing, no shoes, and with empty pockets. Height (cm) was measured without shoes with a portable stadiometer (Seca Leicester, Chino, CA, USA). Waist circumference was measured twice (three times, if the first two measurements differed by 5 mm or more) and the mean of all recorded measurements was calculated. Resting blood pressure was measured with a digital blood pressure monitor (Omron HEM-705CP, Milton Keynes, UK) by a fieldwork nurse. All equipment was calibrated before fieldwork initiation.
For outcomes based on self-report, participants completed self-administered questionnaires. Field staff assisted any participant who seemed to have literacy difficulties and checked questionnaires before the participant left the measurement session to minimise missing data. We assessed self-reported physical activity with the International Physical Activity Questionnaire (IPAQ, Short Form) scored by the IPAQ scoring protocol, and reported total metabolic equivalent task (MET)-min per week from self-reported walking, vigorous, and moderate exercise.
To estimate the extent to which the FFIT programme effected changes in self-reported dietary choice, we queried the frequency of intake of different types of food with an adaptation of the Dietary Instrument for Nutrition Education (DINE).19 We calculated a fatty food score (possible range 8–68), fruit and vegetable score (possible range 0·5–6·0), and sugary food score (possible range 3–16). High scores were indicative of high consumption. The appendix provides further details of what foodstuffs were queried and how the scores were calculated.
We calculated the total number of alcohol units consumed in the previous week with a 7 day recall diary.20 We assessed psychological outcomes with the Rosenberg self-esteem (RSE) scale21, and the Short Form of the positive and negative affect scale (PANAS).22 For both of these measures scores were normalised so that values could be calculated for participants who had missed one or two items contributing to each scale. The PANAS normalised scales range from 1 to 5, with higher scores suggesting high negative affect and positive affect.
Similarly, high scores on RSE (normalised range 0–3) suggest high self-esteem. We assessed quality of life with the Short Form 12, calculating summary scores for mental and physical health.23
The cost calculation for health economic assessment consisted of resources needed to manage and run the programme according to the price paid for them in September, 2011 (appendix). Additionally, at each measurement point we obtained self-reported data relating to the number and type of any NHS resources used in the preceding 12 weeks. Unit costs for visits to a general practitioner, practice nurse, or physiotherapist and attendance at accident and emergency were taken from Personal Social Services Research Unit 2011–12.24 Unit costs for inpatient stays and outpatient visits were taken from Information Services Division Scotland tariffs for 2012 and, as necessary, NHS reference costs for 2011–12. Unit costs for prescriptions for antidepressants, painkillers, asthma, pain gels and creams, anti-inflammatories, and sleeping tablets were taken from a typical prescription of each type from the British National Formulary. The area under the curve method was used to provide an estimate of costs for the within-trial period (ie, 1 year) from the two 12 week periods of data.25
The initial outcome measure for the analysis was the number of men achieving and maintaining the 5% weight reduction in 12 months. Additionally, we converted Short Form 12 values into utility weights with the Short Form 6D algorithm, on the basis of the preference weights of a sample from the general population.26–28 We used the area under the curve method to establish the overall utility for each participant during the trial.25 These values were adjusted to account for differences in the average baseline values between the intervention and comparison groups to provide an estimate of the utility change during the year for each participant. Differences in the average utility change between the intervention and comparison groups provided an estimate of the QALYs gained from the intervention, on the assumption of no differences after the 12 month follow-up. At baseline we recorded participant demographics (age, employment status, educational attainment, deprivation status of postcode of residence [quintiles of Scottish index of multiple deprivation score (SIMD)], marital status, housing status, and ethnic origin), and how participants had heard about the programme.
Adverse events were defined as any injury or newly diagnosed health condition (eg, high blood pressure and diabetes) that arose during the trial; serious adverse events as an adverse event that included the need for hospitalisation or prolonged medical attention, was immediately life threatening (such as cardiac arrest), or was fatal. At each contact, men were given prepaid postcards and details about how to report any adverse events. Serious adverse events were also reported by a coach, by a researcher doing programme observations, and recorded at follow-up sessions. Wherever possible, reporting of serious adverse events was followed up by a telephone call to the participant. The extent to which coaches delivered 93 key tasks in 26 observed delivery sessions is expressed as the percentage of key tasks observers judged coaches to have delivered. Notes about the programme delivery were investigated to explain discrepancies. Interviews were coded thematically in relation to coaches’ experience of delivering various programme elements and the percentage of men who attended at least 50% of sessions was calculated.
Statistical analysis
The study was powered to detect a 5% mean difference in percentage weight loss between the intervention and comparison groups at 12 months, with standard deviation of 19•9%, 80% power, and a two-sided significance level; 250 men were needed in each trial group. On the basis of feasibility work,9 the sample size was increased to 360 men in each group to allow for 30% attrition.
We did all analyses as intention to treat on randomized participants with all available data in mixed models as recommended by White and colleagues.29 We tested distributions for normality and applied logarithmic transformations as appropriate.
We used multiple linear regression for all analyses; baseline measure, group allocation, and club (to allow for stratification by club) were included as fixed effects in adjusted models. We did prespecified subgroup analyses for the primary outcome by adding allocation group by subgroup factor interaction terms in the model; specifically, allocation group by age, marital status, deprivation score, location of measurement (stadium vs home), orientation to masculine norms,30 affiliation to football, whether attended a formal weight management programme in past 3 months, smoking, housing tenure, education, ethnic origin, employment status, joint pain, injuries, and limiting longstanding illness.
Changes are presented as mean (95% CI) unless log transformed, which are presented as median change from baseline and ratio of geometric means (95% CI). Sensitivity analyses for the primary outcome were multiple imputation for missing data assuming data missing at random;29 club as a random variable to account for possible clustering; and repeated measures analysis with results from both 12 weeks and 12 months. All analyses were done with SAS (version 9.3) by the statistician who was masked to group allocation.
The protocol stated that the secondary outcomes of weight loss at 12 weeks and reduction in waist circumference and body fat at 12 weeks and 12 months would be reported as percentages. To be consistent with best statistical practice,31 these are reported as absolute differences. The trial is registered, ISRCTN32677491.
The incremental cost-effectiveness associated with the FFIT programme is presented as incremental cost per additional individual achieving and maintaining the 5% weight reduction over 12 months, and the incremental cost per QALY gained, both compared with no intervention. The 12 month timeframe of the analysis presented here means that costs and outcomes do not need to be discounted. We addressed uncertainty about the estimates of incremental costs, incremental effects, and cost-effectiveness with bootstrapping with 10 000 iterations.
Role of the funding source
The sponsors had no role in the study’s design or conduct; data collection, management, analysis or interpretation; manuscript preparation, review or approval. KH, SW, CMG, CB, PTD, EF, EG, and PR had full access to the data. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
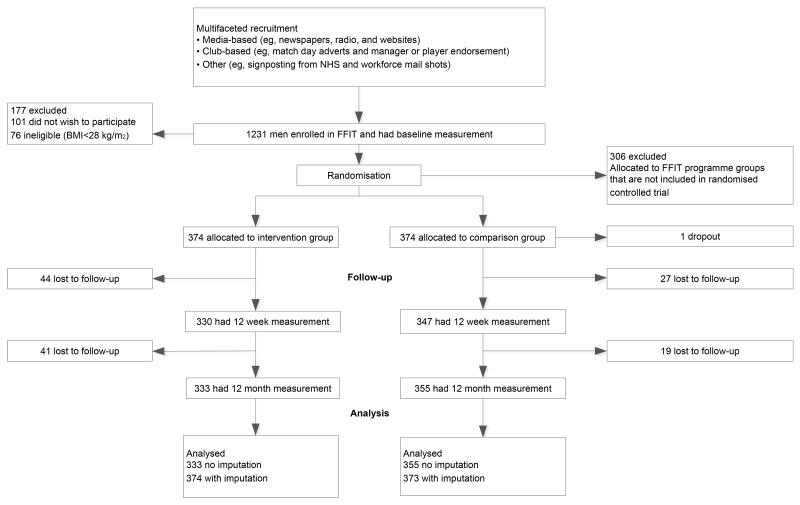
Figure 1 shows participant flow through the trial. The person who dropped out in the comparison group withdrew and requested we destroy his data. Table 1 shows demographic and clinical characteristics of participants (n=747). FFIT attracted men from all socioeconomic groups but few from ethnic minority groups. Retention was high at about 90% at 12 weeks and 12 months (figure 1).
Figure 1. Trial profile.
FFIT=Football Fans in Training. BMI=body-mass index.
Table 1.
Baseline characteristics of participants allocated to the Football Fans in Training programme immediately or in 12 months
| Football Fans in Training (n=374) |
Comparison group (n=373) |
Total (n=747) | |
|---|---|---|---|
| Age (years) | 47·0 (8·07) | 47·2 (7·89) | 47·1 (8·0) |
| Ethnic origin | |||
| White (British, Scottish, Irish, or other) | 367 (98·1) | 368 (98·7) | 735 (98·3) |
| Other | 5 (1·4) | 2 (0·5) | 7 (1·0) |
| Missing | 2 (0·5) | 3 (0·8) | 5 (0·7) |
| Scottish index of multiple deprivation (% living in quintiles) | |||
| 1 (most deprived) | 65 (17·4) | 66 (17·6) | 131 (17·5) |
| 2 | 69 (18·4) | 62 (16·6) | 131 (17·5) |
| 3 | 62 (16·6) | 60 (16·0) | 122 (16·3) |
| 4 | 82 (21·9) | 84 (22·5) | 166 (22·2) |
| 5 | 89 (23·8) | 99 (26·5) | 188 (25·1) |
| Missing | 7 (1·9) | 3 (0·8) | 10 (1·3) |
| Employment status | |||
| Paid work | 322 (86·1) | 304 (81·5) | 626 (83·8) |
| Education or training | 3 (0·8) | 5 (1·4) | 8 (1·1) |
| Unemployed | 9 (2·4) | 18 (4·8) | 27 (3·6) |
| Not working* | 8 (2·1) | 8 (2·1) | 16 (2·1) |
| Retired | 14 (3·7) | 18 (4·8) | 32 (4·3) |
| Other | 17 (4·6) | 19 (5·0) | 36 (4·8) |
| Missing | 1 (0·3) | 1 (0·3) | 2 (0·3) |
| Education | |||
| No qualifications | 37 (9·9) | 34 (9·1) | 71 (9·5) |
| Standard grade or highers† | 115 (30·8) | 126 (33·7) | 241 (32·3) |
| Vocational or HNC and HND | 133 (35·6) | 107 (28·7) | 240 (32·1) |
| University education | 75 (20·1) | 81 (21·7) | 156 (20·9) |
| Other | 14 (3·7) | 25 (6·7) | 39 (5·2) |
| Housing tenure | |||
| Owner-occupied | 280 (74·8) | 283 (75·8) | 563 (75·3) |
| Other | 94 (25·2) | 90 (24·2) | 184 (24·7) |
| Marital status | |||
| Married | 249 (66·6) | 269 (72·1) | 518 (69·3) |
| Living with partner | 55 (14·7) | 40 (10·7) | 95 (12·7) |
| Other (single, divorced, or widowed) | 70 (18·7%) | 64 (17·2%) | 134 (17.9) |
| Objectively measured clinical characteristics | |||
| Weight (kg) | 110·3 (17·9) | 108·7 (16·6) | 109·5 (17·3) |
| Waist circumference (cm) | 118·7 (12·3) | 118·0 (11·1) | 118·4 (11·7) |
| BMI (kg/m2) | 35·5 (5·1) | 35·1 (4·8) | 35·3 (4·9) |
| Body fat (% total weight) | 31·8% (5·7) | 31·5% (5·2) | 31·7% (5·5) |
| Missing | 7 | 3 | 10 |
| Blood pressure (mm/Hg) | |||
| Systolic | 139·4 (17·6) | 141·2 (14·9) | 140·3 (16·3) |
| Diastolic | 88·2 (10·3) | 89·5 (10·1) | 88·8 (10·2) |
| Missing | 0 | 2 | 2 |
| Participants with BMI <30 | 35 (9·4) | 40 (10·7) | 75 (10·0) |
| Self–reported physical activity | |||
| Total MET–min per week | 1188 (396, 2559) | 1173 (396,2559) | 1188 (396,2559) |
| Missing | 3 | 2 | 5 |
| Self-reported eating and alcohol intake | |||
| DINE–based measures | |||
| Fatty food score (range 10–58) | 23·3 (7·1) | 23·4 (7·1) | 23·3 (7·1) |
| Fruit and vegetable score (range 1–6) | 2·3 (1·7) | 2·3 (1·7) | 2·3 (1·7) |
| Sugary food score (range 3–16) | 6·0 (2·7) | 6·2 (2·9) | 6·1 (2·8) |
| Total alcohol consumption (units per week) | 16·5 (17·4) | 17·0 (17·4) | 16·7 (17·4) |
| Self-reported psychological health and quality of life Self–esteem‡ | 1·1 (0·5) | 1·1 (0·5) | 1·1 (0·5) |
| Positive affect (PANAS score)§ | 3·2 (0·7) | 3·2 (0·7) | 3·2(0·7) |
| Missing | 1 | 0 | 1 |
| Negative affect (PANAS score)§ | 1·7 (0·6) | 1·7 (0·6) | 1·7 (0·6) |
| Mental health-related quality of life (Short Form 12 score) | 48·9 (10·1) | 48·3 (9·2) | 48·6 (9·7) |
| Missing | 1 | 0 | 1 |
| Physical health-related quality of life (Short Form 12 score) | 47·0 (7·9) | 47·7 (7·5) | 47·4 (7·7) |
| Missing | 1 | 0 | 1 |
Data are number (%), mean (SD), or median (IQR). HNC=Higher National Certificate. HND=Higher National Diploma. BMI=body-mass index. MET=metabolic equivalent task. DINE=dietary instrument for nutritional education. PANAS=positive and negative affect scale.
Due to long-term sickness or disability.
Scottish school-based qualifications taken at ages 15–16 years and 17–18 years.
Normalised Rosenberg self–esteem score, range 0–3.
Normalised PANAS score, range 1–5).
Observers judged coaches to have delivered 81 of 93 (86%) key tasks in 26 delivery sessions. Assessment of observer notes and analysis of coach interviews suggests that only one session was difficult to deliver because it introduced many new ideas. Coaches overcame this problem by missing out less essential elements of the session and introducing them in following weeks. 12 of the 13 clubs provided attendance records for 356 programme participants; 281 of 356 men (78·9%) attended at least six of the 12 sessions in the active phase of the programme. At 12 months, mean weight loss in men in the intervention group was 5·56 kg (95% CI 4·70–6·43) and 0·58 kg (0·04–1·12) in the comparison group; percentage changes were 4·96% (4·20–5·71) and 0·52% (0·03–1·00), respectively. Prespecified subgroup analyses showed no significant predictors of primary outcome. The mean difference in weight loss between groups adjusted for baseline weight and club was 4·94 kg (3·95–5·94, p<0·0001) and percentage weight loss at 12 months, similarly adjusted, was 4·36% (3·64–5·08, p<0.0001), both in favour of the intervention. The respective unadjusted values were 4·11 kg (1·47–6·75, p<0·0023) and 4·36% (3·64–5·09, p<0·0001).
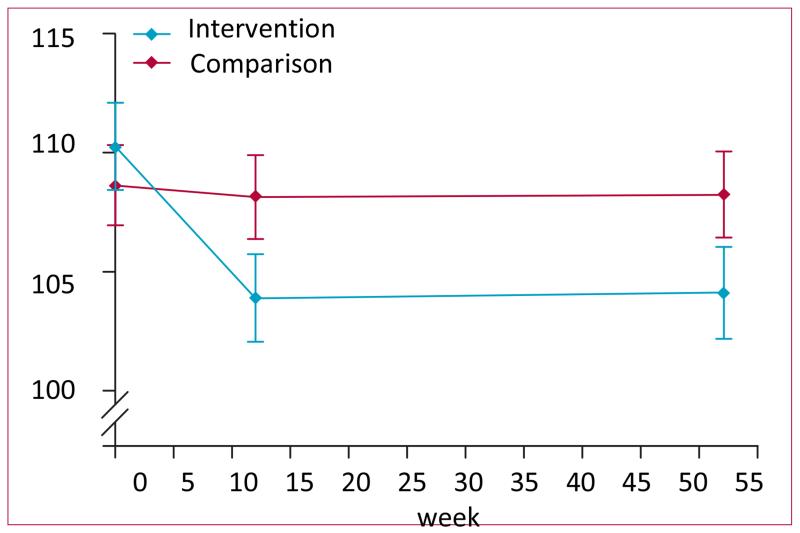
The sensitivity analyses showed similar results: multiple imputation adjusted for weight at baseline and club (4·93 kg [3·92–5·94], p<0·0001); adding club as a random effects adjusted for baseline weight to account for possible clustering (4·94 kg [3·83–6·04], p<0·0001); repeated measures (5·28 kg [4·62–5·94], p<0·0001). Figure 2 shows mean weight (95% CI) at baseline,12 weeks, and 12 months in both groups. More men in the intervention than in the comparison group achieved at least 5% weight loss at 12 months and more had a BMI below 30 kg/m2 (table 2).
Figure 2.
Mean weight (kg, 95% CI) in participants allocated to the Football Fans in Training weight loss programme or waiting list comparison group 12 weeks and 12 months after baseline measurement.
Table 2.
Changes from baseline in objectively measured categorical outcomes at 12 weeks and 12 months and differences between participants allocated to the Football Fans in Training weight loss programme and waiting list comparison group
| Football Fans in Training (n=374) |
Comparison group (n=373) |
Relative risk (95% CI) |
|||
|---|---|---|---|---|---|
| N | N(%) | N | N(%) | ||
| Men who achieved at least 5% weight | |||||
| 12 weeks | 329 | 154 (47%) | 347 | 24 (7%) | 6.77 (4·52–10·13) |
| 12 months | 333 | 130 (39%) | 355 | 40 (11%) | 3·47 (2·51–4·78) |
| Men with BMI <30 kg/m2 | |||||
| 12 weeks | 329 | 85 (26%) | 347 | 44 (13%) | 2·04 (1·46–2·84) |
| 12 months | 333 | 85 (26%) | 355 | 48 (14%) | 1·89 (1·37–2·60) |
The difference between groups in weight loss, waist circumference, and BMI reduction were all significantly in favour of participants on the programme (table 3). Differences in all objectively measured secondary outcomes (weight at 12 weeks, percentage body fat, and systolic and diastolic blood pressure at 12 weeks and 12 months) were also significant and in favour of the intervention (table 3).
Table 3.
Changes in objectively measured continuous outcomes, self-reported outcomes, and self-reported psychological health outcomes
| Football Fans in Training (n=374) |
Comparison group (n=373) |
Mixed models, difference between groups, mean (95% CI) |
Mixed models, difference between groups, mean (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|
| N | Mean (95% CI) or median (IQR) |
N | Mean (95% CI) or median (IQR) |
Unadjusted | p value | Adjusted* | p value | |
| Objectively measure outcomes | ||||||||
| Change in weight (kg) | ||||||||
| 12 weeks | 329 | −5·80 (−6·33 to −5·27) | 347 | −0·42 (−0·76 to −0.09) | −3·93 (−6·47 to −1·38) | 0·0026 | −5·18 (−6·00 to −4·35) | 0·0001 |
| Change in weight (%) | ||||||||
| 12 weeks | 329 | −5·23 (−5·69 to −4·78) | 347 | −0·37 (−0·67 to −0·07) | −4·72 (−5·45 to −3·99) | <0·0001 | −4·71 (−5·44 to −3·98) | <0·0001 |
| Change in waist circumference (cm) | ||||||||
| 12 weeks | 329 | −6·70 (−7·28 to −6·13) | 345 | −1·00 (−1·43 to −0·56) | −4·88 (−6·72 to −3·04) | <0·0001 | −5·57 (−6·41 to −4·72) | <0·0001 |
| 12 months | 318 | −7·34 (−8·18 to −6·49) | 353 | −2·04 (−2·63 to −1·46) | −4·47 (−6·31 to −2·63) | <0·0001 | −5·12 (−5·97 to −4·27) | <0·0001 |
| Change in BMI (kg/m2) | ||||||||
| 12 weeks | 329 | −1·87 (−2·04 to −1·70) | 347 | −0·14 (−0·25 to −0·03) | −1·36 (−2·09 to −0·63) | 0·0003 | −1·66 (−1·93 to −1·40) | <0·0001 |
| 12 months | 333 | −1·79 (−2·07 to −1·51) | 355 | −0·20 (−0·38 to −0·02) | −1·27 (−2·00 to −0·54) | 0·0007 | −1·56 (−1·82 to −1·29) | <0·0001 |
| Change in % body fat | ||||||||
| 12 weeks | 276 | −2·70 (−3·21 to −2·23) | 260 | −0·30 (−0·62 to 0·09) | −1·77 (−2·70 to −0·84) | 0·0002 | −2·16 (−2·81 to −1.51) | <0·0001 |
| 12 months | 271 | −2·20 (−2·88 to −1·60) | 312 | 0·00 (−0·40 to 0·43) | −1·92 (−2·83 to −1·00) | <0·0001 | −2·15 (−2·78 to −1·52) | <0·0001 |
| Change in systolic blood pressure (mm Hg) | ||||||||
| 12 weeks | 295 | −7·50 (−9·14 to −5·89) | 280 | −3·50 (−4·97 to −2·00) | −5·41 (−7·70 to −3·12) | <0·000 | −4·51 (−6·36 to −2·67) | <0·0001 |
| 12 months | 318 | −7·90 (−9·54 to −6·25) | 351 | −6·60 (−7·98 to −5·31) | −3·58 (−5·76 to −1·39) | 0·0025 | −2·27 (−4·01 to −0·54) | 0·0171 |
| Change in diastolic blood pressure (mm Hg) | ||||||||
| 12 weeks | 295 | −3·70 (−4·77 to −2·70) | 280 | −1·5 (−2·53 to −0·54) | −3·10 (−4·56 to −1·64) | <0·000 | −2·51 (−3·71 to −1·32) | <0·0001 |
| 12 months | 318 | −4·60 (−5·63 to −3·60) | 351 | −3·80 (−4·74 to −2·96) | −2·16 (−3·55 to −0·76) | 0·0014 | −1·36 (−2·48 to −0·24) | 0·0102 |
| Self-reported physical activity | ||||||||
| Changes in total MET–min/week (walking, vigorous and moderate exercise) | ||||||||
| 12 weeks | 325 | 1485 (IQR 339 to 3435) | 34 | 0 (IQR −840 to 747) | 2·43 (IQR 1·92 to 3·07) | <0.0001 | 2·38 (IQR 1·90 to 2·98) | p <0.0001 |
| 12 months | 310 | 1219 (IQR 54 to 3111) | 34 | 375 (IQR −414 to 1800) | 1·51 (IQR 1·12 to 2·04) | 0.0.007 | 1·49 (IQR 1·11 to 1·99) | p = 0.008 |
| Self-reported eating and alcohol intake | ||||||||
| Change in DINE-based measures | ||||||||
| Fatty food score | ||||||||
| 12 weeks | 330 | −5·6 (−6·39 to −4·86) | 345 | −1·4 ( −2·03, −0·77) | −4·45 (−5·35 to −3·55) | <0·0001 | −4·39 (−5·16 to −3·61) | <0·0001 |
| 12 months | 318 | −4·5 (−5·32 to −3·74) | 353 | −1·7 (−2·32 to −1·13) | −2·72 (−3·62 to −1.82) | <0·0001 | −2·74 (−3·52 to −1·96) | <0·0001 |
| Fruit and vegetable score | ||||||||
| 12 weeks | 330 | 1·6 (1·39 to 1·81) | 347 | 0·2 (0·03 to 0·41) | 1·26 (1·03 to 1·57) | <0·0001 | 1·32 (1·07 to 1·57) | <0·0001 |
| 12 months | 333 | 0·8 (0·60 to 1·07) | 355 | 0·3 (0·11 to 0·49) | 0·53 (0·26 to 0·80) | 0·0001 | 0·54 (0·29 to 0·79) | <0·0001 |
| Sugary food score | ||||||||
| 12 weeks | 330 | −2·1 (−2·43 to −1·84) | 345 | −0·7 (−0·95 to −0·39) | −1·57 (−1·91 to −1·22) | <0·0001 | −1·52 (−1·83 to 1·21) | <0·0001 |
| 12 months | 318 | −1·3 (−1·62 to −0·97) | 353 | −0·5 (−0·81 to −0·25) | −0·93 (−1·28 to −0·59) | <0·0001 | −0·87 (−1·18 to −0·56) | <0·0001 |
| Change in alcohol consumed (units per week) | ||||||||
| 12 weeks | 329 | −6·2 (−7·58 to −4·79) | 345 | −2·1 (−3·43 to −0·68) | −5·14 (−7·43 to −2·86) | <0·0001 | −4·47 (−6·09 to −2·86) | <0·0001 |
| 12 months | 318 | −4·2 (−5·55 to −2·87) | 353 | −2·2 (−3·39 to −0·96) | −3·40 (−5·69 to −1·11) | 0·0037 | −2·59 (−4·21 to −0·97) | 0·0017 |
| Self-reported psychological health and quality of life outcomes | ||||||||
| Change in self–esteem (Rosenberg score) | ||||||||
| 12 weeks | 330 | 0·3 (0·24 to 0·32) | 344 | 0·1 (0·05 to 0·12) | 0·17 (0·10 to 0·25) | <0·000 | 0·19 (0·14 to −0·24) | <0·0001 |
| 12 months | 317 | 0·3 (0·22 to 0·30) | 350 | 0·1 (0·10 to 0·17) | 0·11 (0·03 to 0·18) | 0·005 | 0·12 (0·07 to 0·17) | <0·0001 |
| Change in positive affect (PANAS score) | ||||||||
| 12 weeks | 328 | 0·5 (0·45 to 0·59) | 344 | 0·1 (0·01 to 0·14) | 0·45 (0·34 to 0·55) | <0·000 | 0·44 (0·36 to 0·53) | <0·0001 |
| 12 months | 317 | 0·3 (0·27 to 0·41) | 350 | 0·1 (0·01 to 0·14) | 0·29 (0·18 to 0·39) | <0·0001 | 0·28 (0·19 to 0·36) | <0·0001 |
| Change in negative affect (PANAS score) | ||||||||
| 12 weeks | 329 | −0·2 (−0·21 to −0·11) | 344 | −0·1 (−0·11 to −0·01) | −0·08 (−0·16 to 0·00) | 0·0591 | −0·09 (−0·15 to −0·03) | 0·0039 |
| 12 months | 317 | −0·2 (−0·24 to −0·13) | 350 | −0·1 (−0·14 to −0·05) | −0·07 −(0·15 to −0·01) | 0·0998 | −0·08 (−0·15 to −0·02) | 0·0079 |
| Change in mental health-related quality of life (short form 12 score) | ||||||||
| 12 weeks | 328 | 3·2 (2·33 to 4·12) | 345 | 1·5 (0·66 to 2·39) | 2·56 (1·12 to 4·00) | 0·000 | 2·01 (0·89 to 3·12) | 0·0004 |
| 12 months | 316 | 1·9 (0·93 to 2·83) | 351 | 1·6 (0·82 to 2·42) | 0·97 (0·47 to 2·42) | 0·186 | 0·50 (−0·62 to 1·62) | 0·3822 |
| Change in physical health-related quality of life (short form 12 score) | ||||||||
| 12 weeks | 328 | 3·3 (2·53 to 4·00) | 345 | 0·4 (−0·33 to 1·12) | 2·00 (0·77 to 3·24) | 0·001 | 2·60 (1·60 to 3·60) | <0·0001 |
| 12 months | 316 | 2·3 (1·48 to 3·21) | 351 | 0·2 (−0·62 to 0·93) | 1·30 (0·06 to 2·54) | 0·040 | 1·89 (0·89 to 2·90) | 0·0002 |
PANAS=positive and negative affect scale.
Adjusted for baseline, stratified by club.
We also recorded significant differences between groups in self-reported physical activity, and consumption of fatty and sugary food, fruit and vegetables, and units of alcohol (table 3). In adjusted analyses, psychological and quality of life outcomes were also positive (table 3) with the exception of changes in mental aspects of health-related quality of life at 12 months. The total costs associated with the intervention group were estimated as £254 579 (US$417 120) (£680 per participant), compared with total costs for the no intervention group of £177 025 (US$290 050) (£475 per participant), which is an incremental cost of £77 554 or £205 per individual (95% CI 27–386). This cost is driven mostly by the additional cost of the intervention.
The cost-effectiveness of FFIT was estimated as £862 per additional man achieving and maintaining a 5% weight reduction at 12 months. The programme was also associated with a gain in QALYs of 0•015 (0•003–0•027) and an incremental cost-effectiveness of £13 847 per QALY gained. The cost-effectiveness acceptability curve (appendix) shows the probability that the intervention is cost-effective for any given value of the cost-effectiveness threshold. For a cost-effectiveness threshold of £20 000 per QALY, the probability that FFIT is cost-effective, compared with no intervention, is 0•72. This probability rises to 0•89 for a cost-effectiveness threshold of £30 000 per QALY.
Eight serious adverse events were reported, five in the intervention group (lost consciousness due to drugs for pre-existing angina, gallbladder removal, hospitalised with suspected heart attack, ruptured gut, and ruptured Achilles tendon), and three in the comparison group (transient ischaemic attack and two deaths, but we did not ask families for further details). Only two were reported as related to participation in the programme: the participant who ruptured an Achilles tendon did so while playing football during the FFIT programme; the participant who had his gallbladder removed was told by his doctor that his intermittent abdominal pains from gallstones could have been aggravated or caused by weight or dietary changes.
Discussion
The findings of this trial show that a 12 session, gender-sensitised programme for weight management and healthy living and subsequent light-touch weight loss support can help men to achieve significant changes in weight, waist circumference, body fat, BMI, blood pressure, self-reported physical activity, dietary intake, alcohol consumption, and measures of psychological and physical wellbeing 12 months after baseline measurement. Mean weight loss in the intervention group fell 4•96% and is likely to be of clinical benefit.
Although outcomes were significantly improved in the intervention group, we recorded small improvements in the comparison group. This finding might be because all men attending the baseline measures were already motivated to lose weight. Second, the information provided at baseline (an advice booklet, their weight and BMI, personalised advice on consulting about high blood pressure, and some information about the programme from club coaches) might have been sufficient to help men on the waiting list comparison group to lose weight independently. Third, some men allocated to the comparison group might have known men in the intervention group and gleaned some details about theapproach taken to weight loss in the programme. Finally, our recruitment activities within clubs could have changed men’s views about the acceptability of weight loss in men or among their peers. Taken together, these factors suggest that the difference in weight loss between the groups is a conservative estimate of what the FFIT programme can deliver.
The programme was inexpensive to deliver and was cost-effective, with the incremental cost of £13 847 per QALY gained falling below the threshold range of £20 000–£30 000 per QALY used by NICE. The cost-effectiveness results are similar to those shown for community-based physical activity interventions that ranged from US$14 000 to $69 000 per QALY (about £8640–£42 600 with present conversions). The within-trial cost-effectiveness analysis assumes there are no differences in QALYs between the groups beyond the 12 month trial follow-up. An additional analysis, to be published separately, will estimate the longer-term effect of the intervention on costs, health outcomes, QALYs, and cost-effectiveness.
A recent systematic review reported only 11 other randomised controlled trials investigating interventions to reduce obesity in men (panel),10 of which only three were of interventions combining dietary and physical activity advice with support for behavioural change (the most effective approach10). Only two of these three trials reported outcomes for both intervention and comparison groups to 12 months.32,33 Both studies were of internet-based programmes with some one-to-one support; findings showed mean differences in weight loss of 2•2 kg (95% CI 1•25–5•65)33 and 0•6 kg (0•14–1•52)32 at 12 months. FFIT is an intense, although inexpensive, programme and is gender sensitised in content, but also context (the football club) and style of delivery (participative, peer-supported learning). These differences might explain why weight loss was greater in FFIT than in earlier trials. The weight loss that the intervention group achieved at 12 weeks was similar to that reported in a UK study5 of primary care referral to a 12 week commercial weight management programme. Stubbs and colleagues5 reported increased weight loss and percentage weight loss in men (mean weight loss at roughly 12 weeks [SD]): 5•8 kg (4•9) in men, 3•8 kg (3•5) in women; percentage weight loss at around 12 weeks was −4•9% (4•0) in men and −3•9% (3•5) in women. However, only 11% of the 34 271 participants were men and outcome data were available only up to the last session attended (with outcome measures obtained as part of routine data collection within the referral programme) so no comparable data are available at 12 months.
Panel: Research in context.
Systematic review
We searched the 2013 systematic review by Robertson and colleagues10 (about the identification of evidence-based management strategies to treat obesity and engage men in weight management services), but did not identify any adequately powered controlled studies of weight management programmes for men delivered in professional sports club settings. Robertson and colleagues’10 review did identify two randomised controlled trials that targeted their content at men, combined dietary and physical activity advice with support for behavioural change, and reported outcomes for both intervention and comparison groups at 12 months.32,33 These trials were of internet-based programmes with some one-to-one support and recorded mean between-group differences in weight loss of 2·2 kg (95% CI 1·25–5·65)33 and 0·6 kg (0·14–1·52)32 in favour of the interventions at 12 months. We used evidence from guidelines and from a systematic review of behavioural change techniques known to be effective in eating and physical activity interventions to design a group-based, gender-sensitised, 12 week, weight management and physical activity programme, with subsequent minimum contact support.14 The programme was delivered by club community coaches in 13 Scottish professional football clubs in 2011–12. We did a randomised controlled trial to assess the programme’s effectiveness at 12 months.
Interpretation
Rising levels of obesity and low participation in weight management programmes in men demand high quality assessment of innovative programmes in community settings to extend the evidence base for cost-effective strategies to support weight loss in men. After feasibility research, we did a robust and appropriately powered pragmatic, randomized controlled trial in a professional sports club setting. The improvements in weight were greater than those seen in other trials32,33 of weight management interventions that were specifically designed for men but were delivered via the internet. These differences might be because Football Fans in Training is a group-based programme and is gender-sensitised not only in content, but also in context (the football club) and style of delivery (participative, peer-supported, and learning).
The FFIT programme has many strengths. It was specifically designed with few exclusion criteria to increase generalisability. Moreover, the people delivering the programme do not need much training; after only 2 days training, coaches found FFIT easy to deliver and were able to deliver the programme’s content largely as intended, although we acknowledge that because we observed only 26 of 156 planned sessions, our data for fidelity are partial. FFIT reached men from all socioeconomic groups showing the reach of football across social groups.34 We report elsewhere that the programme succeeded in attracting men at high risk of future disease; in the 3 months before starting the programme, only 27 of 747 (3•6%) of men had attended a commercial weight management programme and only 13 of 747 (1•7%) a primary-care based programme.17 Thus, FFIT succeeded in reaching high-risk men who were not attracted to other weight management programmes. However, unlike health-related initiatives within the English Premier League,12 it attracted few men from ethnic minority groups. The assessment also had key strengths. We were pragmatic and were able to mask measurement of the primary outcome through careful fieldwork procedures. We exceeded our recruitment and retention targets and participating men fully represented the socioeconomic mix of football supporters. We believe that our results have excellent generalisability to other football-based settings. Further, the results have relevance for lifestyle improvement programmes delivered through other types of sports club—eg, rugby or cricket.
We have shown that a rigorous, pragmatic, randomised controlled trial can be done in a professional sports club setting, and have delivered a programme that helped a significant proportion of men to achieve clinically important weight loss sustained to 12 months. Rising levels of obesity and decreased participation in existing weight management programmes in men demand high-quality assessment of innovative programmes in community settings to extend the evidence base for cost-effective strategies to support weight loss in men. FFIT, an evidence-based programme, gender-sensitised in context, content, and style of delivery, offers one such strategy.
Supplementary Material
Acknowledgments
We thank: the FFIT participants who took part in the research; the club coaches in the Scottish Premiere League (SPL) clubs (Aberdeen FC, Celtic FC, Dundee United FC, Dunfermline Athletic FC, Hamilton Academical FC, Heart of Midlothian FC, Hibernian FC, Inverness Caledonian Thistle FC, Kilmarnock FC, Motherwell FC, Rangers FC, St Johnstone FC, and St Mirren FC) who delivered the FFIT programme; and members of the survey office, fieldwork team leaders, and fieldworkers at Medical Research Council/Chief Scientist Office Social and Public Health Sciences Unit, Glasgow University, in particular Catherine Ferrell, Elaine Hindle, Alice Maclean, Alan Pollock, Mark Robinson, Susan Smillie, David Walker, and Karen Wood. We would particularly like to acknowledge present and former colleagues at the SPL Trust, now the SFPL Trust (Billy Singh, Mark Dunlop, and Stuart MacPhee) for their support in the development, delivery, and assessment of Football Fans in Training (FFIT); the UKCRN registered Tayside Clinical Trials Unit for support for data management; the Scottish Executive Health Department Chief Scientist Office for funding the feasibility pilot that preceded this randomised controlled trial (CZG/2/504); the Medical Research Council who funded KH and additional developmental research through the MRC/CSO SPHSU Gender and Health programme (5TK50/25605200-68094), and Sally Macintyre and Laurence Moore for comments on an earlier draft of the paper. Views and opinions expressed are those of the authors and do not necessarily reflect those of the NIHR PHR Programme, the Department of Health, nor any of the other funders named above.
Funding
Scottish Government and The UK Football Pools funded delivery of the programme through a grant to the Scottish Premier League Trust. The National Institute for Health Research Public Health Research Programme funded the assessment (09/3010/06).
Footnotes
Conflicts of interest
AB has received research grants from Merck, AstraZeneca, and Roche. He has received consultancy and honoraria from Bayer, Merck, AstraZeneca, Servier, and Boehringer Ingelheim. PD has received research grants in the past from GlaxoSmithKline, Pfizer, Otsuka, and Amgen.
References
- 1.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USAand the UK. Lancet. 2011;378:815–25. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 2.Bradshaw P, Bromley C, Corbett J, et al. The Scottish health survey. Volume 1: adults. The Scottish Government; Edinburgh: 2012. [Google Scholar]
- 3.National Institute for Health and Care Excellence [accessed Jan 9, 2014];Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children. 07 Jun 7; 2006. http://guidance.nice.org.uk/CG43/guidance.
- 4.Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2012;20:1234–39. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- 5.Stubbs RJ, Pallister C, Whybrow S, Avery A, Lavin J. Weight outcomes audit for 34,271 adults referred to a primary care/ commercial weight management partnership scheme. Obesity Facts. 2011;4:113–20. doi: 10.1159/000327249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jebb SA, Ahern AL, Olson AD, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet. 2011;378:1485–92. doi: 10.1016/S0140-6736(11)61344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ross HM, Laws R, Reckless J, Lean M, Counterweight Project T Evaluation of the Counterweight Programme for obesity management in primary care: a starting point for continuous improvement. Br J Gen Pract. 2008;58:548–54. doi: 10.3399/bjgp08X319710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young MD, Morgan PJ, Plotnikoff RC, Callister R, Collins CE. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes Rev. 2012;13:393–408. doi: 10.1111/j.1467-789X.2011.00967.x. [DOI] [PubMed] [Google Scholar]
- 9.Gray C, Hunt K, Mutrie N, Anderson A, Treweek S, Wyke S. Weight management for overweight and obese men delivered through professional football clubs: a pilot randomized trial. Int J Behav Nutr Phys Act. 2013;10:121. doi: 10.1186/1479-5868-10-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robertson C, Archibald D, Avenell A, et al. Systematic reviews and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men: report commissioned by the NIHR HTA Programme as project number 09/127/01. Health Technol Assess. doi: 10.3310/hta18350. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brady AJB, Perry C, Murdoch DL, McKay G. Sustained benefits of a health project for middle-aged football supporters, at Glasgow Celtic and Glasgow Rangers Football Clubs. Eur Heart J. 2010;31:2966–68. [PubMed] [Google Scholar]
- 12.Pringle A, Zwolinsky S, McKenna J, Daly-Smith A, Robertson S, White A. Effect of a national programme of men’s health delivered in English Premier League football clubs. Public Health. 2013;127:18–26. doi: 10.1016/j.puhe.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Hunt K, McCann C, Gray CM, Mutrie N, Wyke S. “You’ve got to walk before you run”: positive evaluations of a walking program as part of a gender-sensitized, weight-management program delivered to men through professional football clubs. Health Psychol. 2013;32:57–65. doi: 10.1037/a0029537. [DOI] [PubMed] [Google Scholar]
- 14.Gray C, Hunt K, Mutrie N, et al. Football Fans in Training: the development and optimization of an intervention delivered through professional sports clubs to help men lose weight, become more active and adopt healthier eating habits. BMC Public Health. 2013;13:232. doi: 10.1186/1471-2458-13-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torgerson DJ. Contamination in trials: is cluster randomisation the answer? BMJ. 2001;322:355–57. doi: 10.1136/bmj.322.7282.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.British Heart Foundation [accessed Jan 9, 2014];So you want to lose weight…for good. 2009 Mar 5; http://www.bhf.org.uk/publications/view_publication.aspx?ps=1000807.
- 17.Hunt K, Gray C, Maclean A, Smillie S, Bunn C, Wyke S. Do weight management programmes delivered at professional football clubs attract and engage high risk men? BMC Public Health. 2014;14:50. doi: 10.1186/1471-2458-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions:a meta-regression. Health Psychol. 2009;28:690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 19.Roe L, Strong C, Whiteside C, Neil A, Mant D. Dietary intervention in primary care: validity of the DINE method for diet assessment. Fam Pract. 1994;11:375–81. doi: 10.1093/fampra/11.4.375. [DOI] [PubMed] [Google Scholar]
- 20.Emslie C, Lewars H, Batty GD, Hunt K. Are there gender differences in levels of heavy, binge and problem drinking? Evidence from three generations in the west of Scotland. Public Health. 2009;123:12–14. doi: 10.1016/j.puhe.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenberg M. Society and the adolescent self-image. Princeton University Press; Princeton, NJ: 1965. [Google Scholar]
- 22.Thompson ER. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS) J Cross Cult Psychol. 2007;38:227–42. [Google Scholar]
- 23.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. J Clin Epidemiol. 1998;51:1171–78. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 24.Personal Social Services Research Unit [accessed Nov 9, 2013];Unit cost of health and social care. 2011 http://www.pssru.ac.uk/project-pages/unit-costs/2011/index.php.
- 25.Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs intrial-based cost-effectiveness analysis: the importance of controllingfor baseline utility. Health Econ. 2005;14:487–96. doi: 10.1002/hec.944. [DOI] [PubMed] [Google Scholar]
- 26.Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42:851–59. doi: 10.1097/01.mlr.0000135827.18610.0d. [DOI] [PubMed] [Google Scholar]
- 27.McCabe C, Brazier J, Gilks P, et al. Using rank data to estimate health state utility models. J Health Econ. 2006;25:418–31. doi: 10.1016/j.jhealeco.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Kharroubi SA, Brazier JE, Roberts J, O’Hagan A. Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Health Econ. 2007;26:597–612. doi: 10.1016/j.jhealeco.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 29.White IR, Carpenter J, Horton NJ. Including all individuals is not enough: lessons for intention-to-treat analysis. Clin Trials. 2012;9:396–407. doi: 10.1177/1740774512450098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahalik JR, Locke BD, Ludlow LH, et al. Development of the conformity to masculine norms inventory. Psychol Men Masculin. 2003;4:3–25. [Google Scholar]
- 31.Vickers A. The use of percentage change from baseline as an outcome in a controlled trial is statistically inefficient: a simulation study. BMC Med Res Methodol. 2001;1:6. doi: 10.1186/1471-2288-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patrick K, Calfas K, Norman G, et al. Outcomes of a 12-month web-based intervention for overweight and obese men. Ann Behav Med. 2011;42:391–401. doi: 10.1007/s12160-011-9296-7. [DOI] [PubMed] [Google Scholar]
- 33.Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. 12-month outcomes and process evaluation of the SHED-IT RCT:an internet-based weight loss program targeting men. Obesity. 2011;19:142–51. doi: 10.1038/oby.2010.119. [DOI] [PubMed] [Google Scholar]
- 34.Barclays Premier League [accessed Nov 12, 2013];Research and insight, season 2011-2012. http://fansurvey.premierleague.com/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.