ABSTRACT
Viral drug resistance is believed to be less likely to occur if compounds are directed against cellular rather than viral proteins. In this study, we analyzed the feasibility of a crucial viral replication factor, namely, importin-α7, as a cellular drug target to combat pandemic influenza viruses. Surprisingly, only five viral lung-to-lung passages were required to achieve 100% lethality in importin-α7−/− mice that otherwise are resistant. Viral escape from importin-α7 requirement was mediated by five mutations in the viral ribonucleoprotein complex and the surface glycoproteins. Moreover, the importin-α7−/− mouse-adapted strain became even more virulent for wild-type mice than the parental strain. These studies show that targeting host proteins may still result in viral escape by alternative pathways, eventually giving rise to even more virulent virus strains. Thus, therapeutic intervention strategies should consider a multitarget approach to reduce viral drug resistance.
IMPORTANCE Here, we investigated the long-standing hypothesis based on in vitro studies that viral drug resistance occurrence is less likely if compounds are directed against cellular rather than viral proteins. Here, we challenged this hypothesis by analyzing, in an in vivo animal model, the feasibility of targeting the cellular factor importin-α7, which is crucial for human influenza virus replication and pathogenesis, as an efficient antiviral strategy against pandemic influenza viruses. In summary, our studies suggest that resistance against cellular factors is possible in vivo, and the emergence of even more virulent viral escape variants calls for particular caution. Thus, therapeutic intervention strategies should consider a multitarget approach using compounds against viral as well as cellular factors to reduce the risk of viral drug resistance and potentially increased virulence.
INTRODUCTION
Influenza A viruses are responsible for acute respiratory diseases in humans posing a severe burden for health and economy worldwide. Vaccination is considered the best option for disease prophylaxis. However, production of novel vaccines in the case of a pandemic requires at least 6 months. Thus, antiviral drugs are essential to bridge this gap. Two classes of antiviral agents currently are available against influenza virus: neuraminidase inhibitors and adamantanes (1). However, their efficiency is limited, and several influenza virus strains have developed resistance to these virus-directed drugs (2). Hence, development of novel antiviral agents is urgently required.
Inhibitors developed against host cell proteins are considered an attractive strategy compared to drugs that target viral proteins, because they are less prone to mutations than viral proteins. Thus, it is believed that targeting host factors would limit the emergence of drug-resistant virus strains. Several compounds targeting cellular factors to halt influenza virus replication currently are under development (3–5). For example, inhibitors targeting the Raf/MEK/ERK signaling pathway, NF-κB signaling, the phosphatidylinositol 3-kinase/Akt pathway, and the protein kinase C signaling cascade are already in an early phase of preclinical development (6).
For influenza virus, the nuclear import protein importin-α7 is a crucial pathogenicity factor that increases human-type influenza virus replication by an unknown mechanism beyond nuclear import. Mice with a deleted importin-α7 gene (α7−/−) are resistant to an otherwise lethal 2009 pandemic H1N1 influenza virus infection (7–9). Since deletion of the importin-α7 gene did not cause an obvious phenotype in adult α7−/− mice (10), its transient inhibition poses a very attractive target to combat human-type influenza viruses.
In this study, we investigated whether targeting importin-α7 would provide an efficient antiviral strategy against pandemic influenza viruses, reducing the risk of viral resistance. In particular, we employed a method of accelerated viral evolution, thereby challenging viral escape in a resistant host.
MATERIALS AND METHODS
Ethical statement.
All animal experiments were approved by the relevant German authority (Behörde für Gesundheit und Verbraucherschutz, Hamburg, Germany) and performed according to the national guidelines of the animal protection law (Tierschutzgesetz; project number 97/11) in Germany.
Animal experiments.
Importin-α7−/− (α7−/−) mice (8, 10) and wild-type (WT) littermates in the C57BL/6J genetic background were bred and housed under specific-pathogen-free conditions at the animal facility of the Heinrich-Pette-Institute, Leibniz Institute for Experimental Virology, Hamburg, Germany.
Mice were anesthetized with ketamine/xylazine (70 mg/kg of body weight and 7 mg/kg, respectively) and inoculated intranasally with 50 μl of virus diluted in phosphate-buffered saline (PBS). Survival and weight loss were monitored for 14 days. The 50% mouse lethal dose (MLD50) was determined using serial 10-fold virus dilutions (11). Mice were humanely euthanized upon >25% weight loss.
Cells.
Madin-Darby canine kidney (MDCK) cells were grown in minimal essential medium (PAA, Austria) supplemented with fetal calf serum (FCS; PAA, Austria), l-glutamine (PAA, Austria), and penicillin-streptomycin (PAA, Austria). Human embryonic kidney 293T (HEK) and human alveolar adenocarcinoma (A549) cells were grown in DMEM (Dulbecco's modified Eagle's medium; PAA, Austria) supplemented with 10% FCS, l-glutamine, and penicillin-streptomycin. WT and α7−/− murine embryonic fibroblasts (MEF) were grown in DMEM supplemented with 10% FCS, penicillin-streptomycin, l-glutamine, nonessential amino acids (PAA, Austria) and sodium pyruvate (PAA, Austria). MEFs were kindly provided by M. Bader (Max Delbrück Center for Molecular Medicine, Berlin, Germany) (12).
HEK and A549 cells were transduced with lentiviral vectors expressing short hairpin RNA (shRNA) anti-importin-α7 (clone identifier NM_012316.3-223s1c1; Sigma-Aldrich, Germany) to generate importin-α7 knockdown cell lines, named HEK-shα7 and A549-shα7. Transduced cells were selected and maintained in medium containing 2 μg/ml puromycin (Calbiochem, USA). shRNA-mediated knockdown was confirmed by Western blotting using anti-importin-α5/α7 antibody (kindly provided by the E. Hartmann Institute of Biology, Lübeck, Germany) (8). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) expression was detected by an anti-GAPDH antibody (Cell Signaling Technology, Inc., USA).
Adaptation of pH1N1 influenza virus to importin-α7−/− mice.
We used the 2009 pandemic H1N1 A/Hamburg/NY1580/09 virus strain (abbreviated as pH1N1) as a parental strain (8, 13, 14). Three α7−/− mice were intranasally infected with 105 PFU of the pH1N1 strain. Lungs were harvested and homogenized 3 days postinfection (p.i.). Subsequently, 50 μl of the pooled lung homogenate supernatant was used to intranasally infect the next group of three α7−/− mice. Serial passaging was stopped upon 100% lethality. One viral clone was isolated from the lung homogenates of the fifth passage by plaque purification from MDCK cells and named pH1N1-MA7. All experiments were performed at the biosafety level 2 facilities of the Heinrich-Pette-Institute, Leibniz Institute for Experimental Virology.
Plasmids and recombinant pH1N1 viruses.
The gene segments of pH1N1 and pH1N1-MA7 viruses were sequenced as described previously (15). pH1N1 genes were cloned into the pHW2000 vector to generate recombinant influenza viruses by reverse genetics. pH1N1-MA7 specific mutations were introduced using the QuikChange site-directed mutagenesis kit (Stratagene/Agilent Technologies, USA). Virus stocks were grown in MDCK cells and sequenced for verification.
PB1, PB2, PA, and NP genes from pH1N1 or pH1N1-MA7 viruses additionally were cloned from pHW2000 vector into pcDNA3.1 vector to generate pC-HH15-PB1, pC-HH15-PB2, pC-HH15-PA, pC-HH15-NP, pC-HH15-PAMA7, and pC-HH15-NPMA7 expression plasmids.
Polymerase activity.
HEK or HEK-shα7 cells were cotransfected with pC-HH15-PB1, pC-HH15-PB2, pC-HH15-PA, pC-HH15-NP, pC-HH15-PAMA7, or pC-HH15-NPMA7 to generate recombinant RNPs. Reporter constructs pPol-I-NP-Luc-human (encoding firefly luciferase in negative polarity flanked by the nontranslated regions of influenza NP segment) (16) and pRL-TK (encoding Renilla luciferase; Promega, USA) were cotransfected. The transfection solution was prepared by incubating a mixture of DNA, polyethylenimine (PEI; Polysciences), and DMEM in a ratio of 1 μg DNA to 2.4 μg PEI to 600 μl DMEM for 20 min at room temperature. At 20 h posttransfection, luciferase activity was measured with a dual-luciferase reporter assay system (Promega, USA). All experiments were performed in triplicates.
Coimmunoprecipitation assay.
Immunoprecipitations were performed using EZview red anti-FLAG M2 affinity gel (Sigma, USA) and eluted using a 3× FLAG peptide (Sigma, USA) according to the manufacturer's instructions. The quantification of coimmunoprecipitation products was performed by Western blotting using mouse anti-FLAG (Sigma, USA) and rabbit anti-feline panleukemia virus serum (17) antibodies. The β-actin antibody (Abcam, United Kingdom) was used for normalization of the total protein amount used in respective cell lysates. Immunoreactive bands were visualized with the Bioimager Image Quant LAS 4000 at nonsaturated levels and quantified by densitometry with ImageJ software.
Analysis of virus replication.
A549 and A549-shα7 cells were infected at a multiplicity of infection (MOI) of 0.1 with pH1N1 or pH1N1-MA7 virus, respectively, in the presence of 0.25 μg/μl l-1-tosylamide-2-phenylethyl chloromethyl ketone (TPCK)-trypsin. Supernatants were collected at 0, 24, 48, and 72 h p.i., and virus titers were determined as plaque-forming units on MDCK cells.
WT and α7−/− MEFs were infected at an MOI of 2 with pH1N1 recombinant viruses containing pH1N1-MA7 mutations as indicated. Total RNA was isolated at 24 h p.i. by extraction with TRIzol reagent (Invitrogen, USA). Viral RNA accumulation was analyzed by primer extension using specific primers for the viral NP gene (18). Primer PrE-NP− (5′-ATGATGGAAAGTGCAAAGCC-3′) was used to detect vRNA and primer PrE-NP+ (5′-ATTTCTGTGGCATCCTGGC-3′) to detect cRNA and mRNA. A primer detecting cellular 5S rRNA (5′-TCCCAGGCGGTCTCCCATCC-3′) was used for normalization. Transcription products were analyzed on 6% polyacrylamide gels containing 7 M urea in Tris-borate-EDTA (TBE) buffer, detected by autoradiography, and quantified by densitometry of phosphorimages using AIDA software.
Modeling of pH1N1 protein structure domains.
The three-dimensional (3D) conformations of the proteins of interest from the parental pH1N1 strain were modeled to evaluate the effects of the mutations over their structural stability. The templates used to build these structures were their closest homologues with known structures in the Protein Data Bank (PDB) (19, 20), found by sequence similarity through BLAST (21). In all cases, a template containing the region with the mutations was found with an E value of 0, which indicates the probability of a protein-template assignation due to chance. Specifically, PA was modeled over 4AVL-chainD (22), NP over 4DYS-chainC, NA over 4B7R-chainD (23), and HA over 2WR0-chainB (24). Except for PA, the templates covered more than 80% of the protein length. Thirty parental models were created for each protein through MODELLER (25). Global and local energies were analyzed with Prosa (26). Global energy (z score) represents a normalized score of the stability of the protein. Local energy represents the individual stability of each residue in the structural conditions in a given 3D representation. Both values are further divided in surface, pair (structural), and combined (pair plus surface) energy. As a rule, negative values represent stable conformations. A total of 30 variants for each possible mutant of interest were created with Prosa and analyzed for both their global and local energies.
Statistical analysis.
All data shown are presented as means ± standard errors of the means (SEM). Means, SEM, Student's t test (unpaired, 2-tailed), and Mantel-Cox test were calculated with Prism GraphPad software (GraphPad Software, Inc., USA). Statistical significance was defined as P < 0.05 (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
RESULTS
Adaptation of a 2009 pandemic H1N1 influenza virus strain to importin-α7−/− mice.
The importin-α7 gene is crucial for replication and pathogenicity of human-type influenza A viruses in mammals. The lack of the importin-α7 gene leads to 100% survival in mice infected with several 2009 pandemic H1N1 influenza virus strains, whereas 100% of WT mice succumb to infection (8). Here, we addressed whether targeting importin-α7 would pose a promising antiviral strategy to combat human influenza viruses. To analyze whether viral escape would be possible using a cellular target, we challenged this approach by adapting a 2009 pandemic H1N1 strain (A/Hamburg/NY1580/09; pH1N1) to importin-α7−/− (α7−/−) mice by serial lung-to-lung passages. Interestingly, 100% lethality could be achieved after only 5 passages. We isolated one α7−/− mouse-adapted virus clone (pH1N1-MA7) by plaque assay and assessed its pathogenesis in WT and α7−/− mice compared to that of its parental strain (Fig. 1A). Consistent with previous findings, infection of α7−/− mice with the parental pH1N1 strain did not result in significant weight loss or lethality (8). However, the adapted pH1N1-MA7 strain was lethal for WT (MLD50, 102.4 PFU) and α7−/− mice (MLD50, 102.6 PFU). Notably, the pH1N1-MA7 strain was more virulent for WT mice than its nonadapted parental strain, suggesting that its virulence increased during viral escape from importin-α7 requirement (Fig. 1B). Sequencing of both viral genomes revealed two amino acid substitutions in the ribonucleoprotein (RNP) complex (PA D27E and NP G102R) and three substitutions in the viral surface glycoproteins, including two mutations in HA (K171E and D239G) and one mutation in NA (Y170H) (Fig. 1C).
FIG 1.
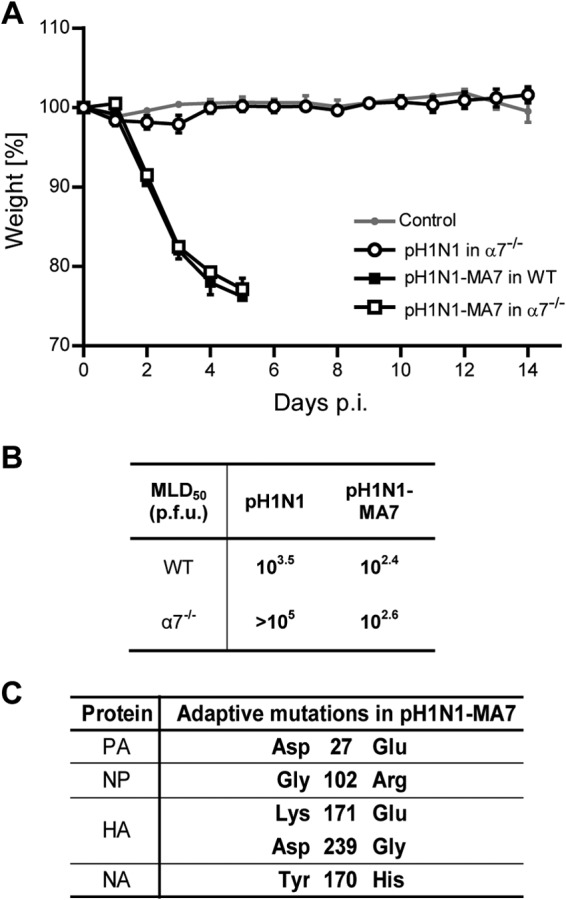
Adaptation of 2009 pH1N1 influenza virus to α7−/− mice. (A) Pathogenicity of pH1N1-MA7 influenza virus. WT (black squares) or α7−/− (open squares) mice were intranasally inoculated with 105 PFU of pH1N1-MA7 virus. As controls, a group of α7−/− mice were infected with the parental strain 2009 pH1N1 (open circles) or received PBS only (gray circle). Weight loss was monitored for 14 days. Data shown represent means ± SEM (n = 5 to 13). (B) MLD50 of pH1N1 and pH1N1-MA7 strains in WT and α7−/− mice. (C) Amino acid sequence differences are shown for parental pH1N1 and adapted pH1N1-MA7 viruses.
Overall, we could show that pH1N1 influenza viruses are able to escape the requirement for importin-α7 by acquiring adaptive mutations in the viral RNP and the surface glycoproteins. This escape rendered the virus even more virulent for WT mice.
Identification of host adaptive sites responsible for overcoming viral restriction in importin-α7−/− mice.
In order to identify the relevant viral genes responsible for the evasion of viral restriction in α7−/− mice, we generated single-gene reassortant (SGR) recombinant influenza viruses containing one exchanged gene segment of the pH1N1-MA7 strain in the parental pH1N1 virus background. In order to study the role of the RNP on viral pathogenesis, we also generated the double gene reassortant pH1N1-PA,NPMA7 virus that contains PA and NP genes of the pH1N1-MA7 strain.
We then assessed the pathogenic potential of these viruses in WT and α7−/− mice (Fig. 2). Infection with the recombinant pH1N1-MA7 (pH1N1-MA7rec) virus containing all five adaptive mutations showed pathogenesis similar to that of the isolated clone. Interestingly, none of the SGR viruses increased lethality in α7−/− mice. However, pH1N1-NPMA7 significantly enhanced weight loss in α7−/− mice, which was further increased when combined with the PAMA7 gene segment. This suggests a synergistic effect of PAMA7 and NPMA7 on viral pathogenesis in α7−/− mice. In contrast, pH1N1-HAMA7 and pH1N1-NAMA7 SGR viruses did not cause any significant weight loss in α7−/− mice. Conversely, in WT mice, adaptive mutations in HA and NA strongly enhanced pathogenicity, in contrast to adaptive mutations in the RNP (Fig. 2B).
FIG 2.
Pathogenicity of pH1N1-MA7 recombinant viruses in WT and α7−/− mice. (A) WT (black square) or α7−/− (open square) mice were intranasally inoculated with recombinant viruses, i.e., 104 PFU of adapted pH1N1-MA7rec, 105 PFU of pH1N1-PAMA7, 105 PFU of pH1N1-NPMA7, 105 PFU of pH1N1-PA,NPMA7, 105 PFU of pH1N1-HAMA7, and 105 PFU of pH1N1-NAMA7. Weight loss and survival was monitored for 14 days. Control mice received PBS only (gray circle). Data shown represent means ± SEM (n = 5 to 15). (B) Weight loss has been summarized as representing the mean area under the curve (AUC). WT (black bars) or α7−/− (white bars) mice were infected with 105 PFU of wild-type viruses (pH1N1 and pH1N1-MA7) and recombinant viruses (pH1N1-PAMA7, pH1N1-NPMA7, pH1N1-PA,NPMA7, pH1N1-HAMA7, and pH1N1-NAMA7). Control mice received PBS (gray bar). Data shown represent means ± SEM (n = 5 to 15; P < 0.05 [*], P < 0.01 [**], and P < 0.001 [***], all by Student's t test compared to the control group).
These data suggest that mutations in the RNP are adaptations to the lack of importin-α7, while mutations in HA and NA seem to represent adaptations to the WT animal. However, a combination of both mutations in the RNP as well as in the glycoproteins is required to completely escape importin-α7-mediated restriction in mice.
Adaptive mutations are localized on the respective protein surface.
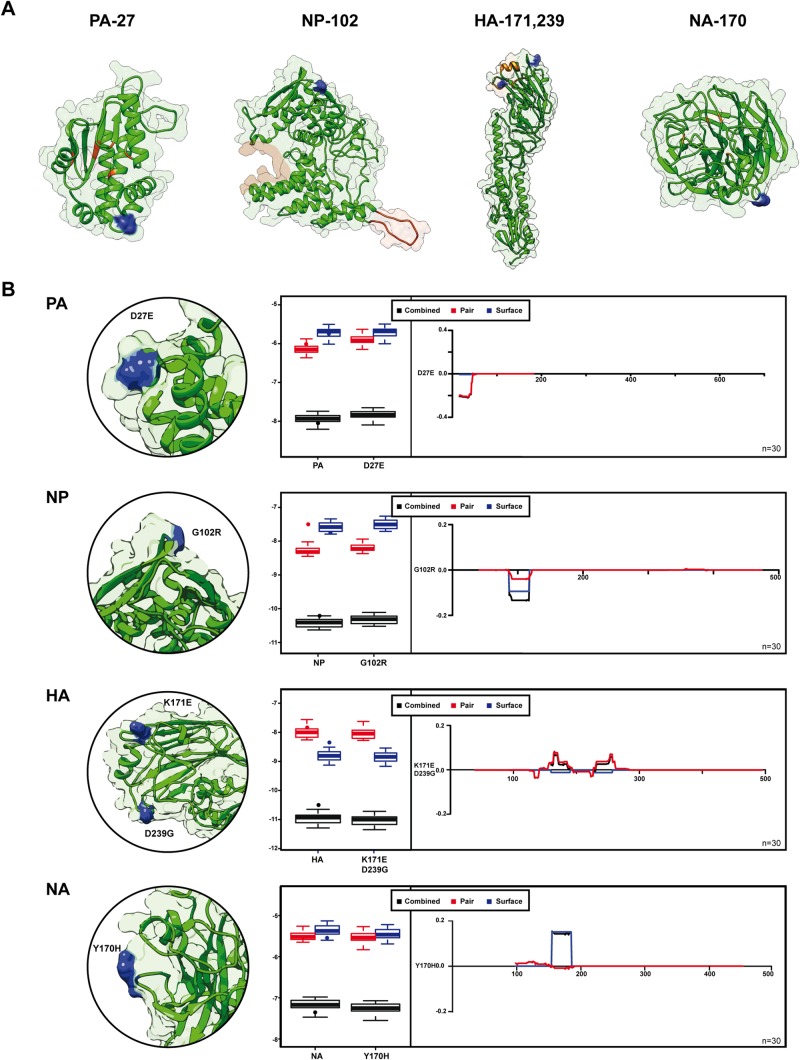
We then generated structural models to investigate the localization of the pH1N1-MA7 adaptive mutations (Fig. 3). All adaptive mutations are located on the surface of the viral proteins. In particular, the PAMA7 D27E mutation is located on the surface of the endonuclease domain. The HAMA7 D239G mutation is included in the 220-loop element of the receptor binding site, and the HAMA7 K171E mutation is near this domain. NPMA7 G102R and NAMA7 Y170H mutations are located in domains without a specific function described at the moment (Fig. 3A).
FIG 3.
Localization of the adaptive mutations in pH1N1 protein structure and their effect on structural stability. (A) Structural models of the regions surrounding the adaptive mutations of pH1N1-MA7 with homologous structures. Adaptive mutations are indicated in blue. Relevant sites in the structures are indicated in orange (PA endonuclease active site, RNA binding site and oligomerization domain of NP, HA receptor binding site, and NA active site). (B) Global z score (as boxplots) and local energy comparison between the mutants of pH1N1-MA7 and their respective wild types (pH1N1). The x axis shows the corresponding amino acid position, and the y axis shows the energy change. Each set is composed of 30 structural models. Pair (red), surface (blue), and combined (black) energy are shown for each analysis. Dots placed above the z score distributions of the pH1N1 models represent the score of the structural template.
To evaluate potential energy changes, we mimicked the adaptive mutations and compared the energies of the different mutants against their parental proteins (Fig. 3B). The comparison showed no significant differences between the parental and the mutant structures in either global (z score) or in local energies. This suggests that these adaptive mutations do not alter the global stability of the protein. Although some local differences are observed, those are extremely small and focused in the surface energy. These results indicate that these mutations in PA, NP, HA, and NA do not directly affect protein conformation, but they might affect interaction with other viral and/or host factors which affect protein functions.
Adaptive mutations increase RNP activity.
To study the effect of the adaptive mutations in PA and NP genes on viral polymerase activity, we reconstituted viral RNPs in wild-type (HEK-WT) as well as in importin-α7 knockdown (HEK-shα7) cell lines (Fig. 4). The pH1N1-MA7 polymerase activity was increased up to 3-fold compared to that of the nonadapted pH1N1 polymerase in HEK-WT cells. Interestingly, PAMA7 was mainly responsible for this increase in viral polymerase activity in HEK-WT cells, while NPMA7 did not show significant effects. However, both pH1N1 and pH1N1-MA7 polymerase activity was restricted in HEK-shα7 compared to that of HEK-WT cells. Similarly, PAMA7 was the main mediator of elevated polymerase activity in HEK-shα7 cells.
FIG 4.
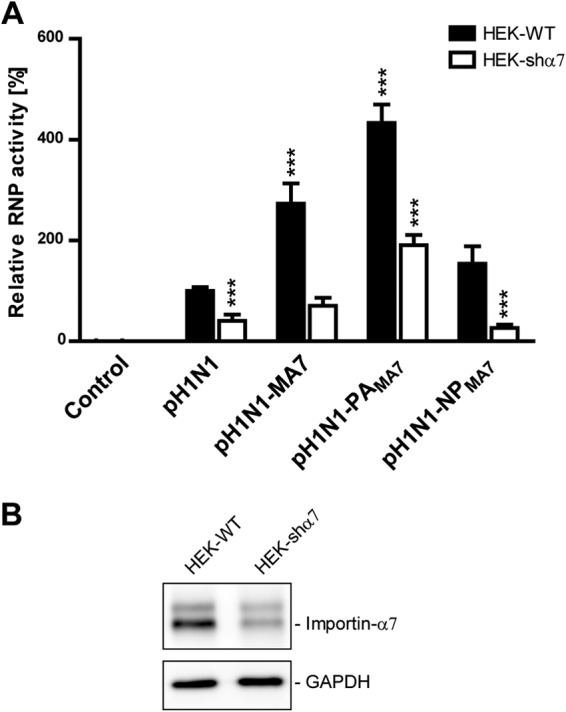
Biological activity of recombinant RNPs with adaptive mutations in epithelial HEK and HEK-shα7 cell lines. (A) Human HEK-WT (black bars) and HEK-shα7 (white bars) cells were cotransfected with plasmids expressing PB1, PA, NP, and PB2, as well as a plasmid encoding Renilla luciferase and a plasmid encoding firefly luciferase in negative polarity, flanked by the nontranslated regions of influenza NP segment. Plasmid expressing PB1 was omitted as a negative control. Plasmids encoding PAMA7 and NPMA7 were used when indicated, and both were used in pH1N1-MA7. At 20 h posttransfection, luciferase accumulation was determined. Values were normalized to Renilla expression, and the activity of the pH1N1 RNP in HEK-WT cells was set to 100% (means ± SEM; n = 9 to 18; ***, P < 0.001 by Student's t test compared to pH1N1 RNP activity in HEK-WT cells). (B) Confirmation of importin-α7 knockdown in human HEK cells by Western blotting. Since importin-α7 antibody cross-reacts with importin-α5, the doublet represents importin-α5 (upper band) and importin-α7 (lower band). GAPDH was used as a loading control.
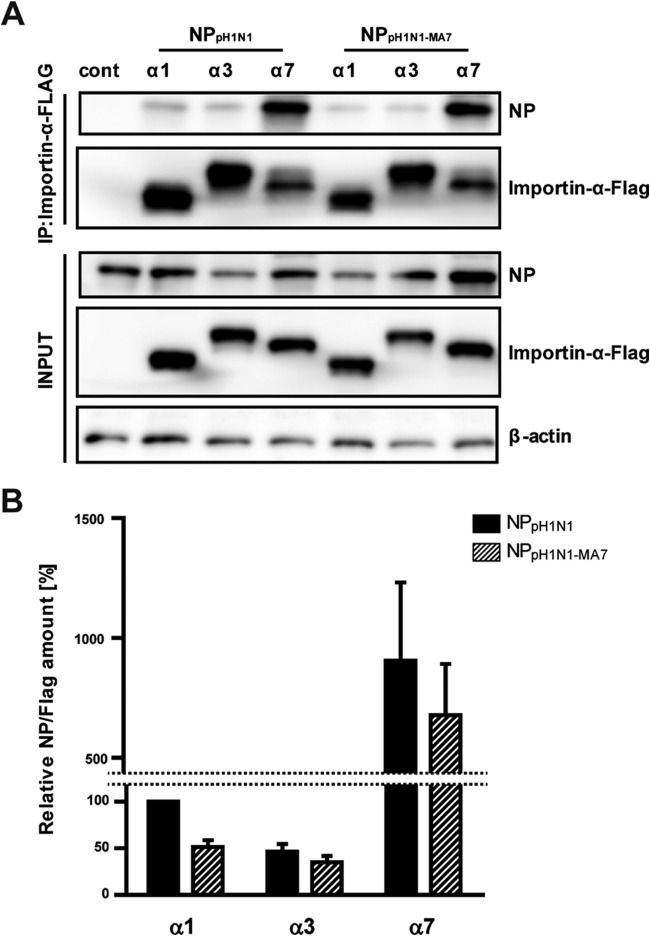
We next addressed whether the adaptive mutation in NPMA7 resulted in altered importin-α binding affecting vRNP activity. NPMA7 shows a generally reduced binding affinity to importin-α1, -α3, and -α7 isoforms, which are relevant for influenza virus replication (8), compared to that to nonadapted NP, albeit at a statistically nonsignificant level (Fig. 5).
FIG 5.
Importin-α binding affinities to NP monomers with adaptive mutation. (A) Human HEK-WT cells were cotransfected with plasmids encoding FLAG-tagged importins (α1, α3, or α7) and NP or NPMA7. NP-only transfected cells served as a control (cont). At 48 h posttransfection, importins were immunoprecipitated using the FLAG tag, and coimmunoprecipitated NP was determined by Western blotting. β-Actin was used as a loading control in the input samples. (B) Quantification of NP (black bars) or NPMA7 (dashed bars) binding to overexpressed importins. Values of NP were normalized against precipitated importin-α levels, and the relative amount of NP bound to importin-α1 was set to 100%. Data shown represent means ± SEM (n = 3).
These findings show that α7−/− adaptive mutations in the RNP mediate partial escape from importin-α7 depletion in mice. However, a complete circumvention of the RNP from importin-α7 requirement could not be achieved. These data suggest that alternative pathways are utilized to circumvent the lack of importin-α7.
Adaptive mutations increase virus replication.
We next analyzed the viral replication kinetics of pH1N1-MA7 compared to those of the parental pH1N1 virus in WT epithelial (A549-WT) and in importin-α7 knockdown (A549-shα7) cell lines (Fig. 6). Consistent with previous reports, parental pH1N1 virus replication was strongly impaired in A549-shα7 cells by approximately 2 logs compared to A549-WT cells. In contrast, pH1N1-MA7 virus replication was only slightly reduced in A549-shα7 compared to that in WT cells.
FIG 6.
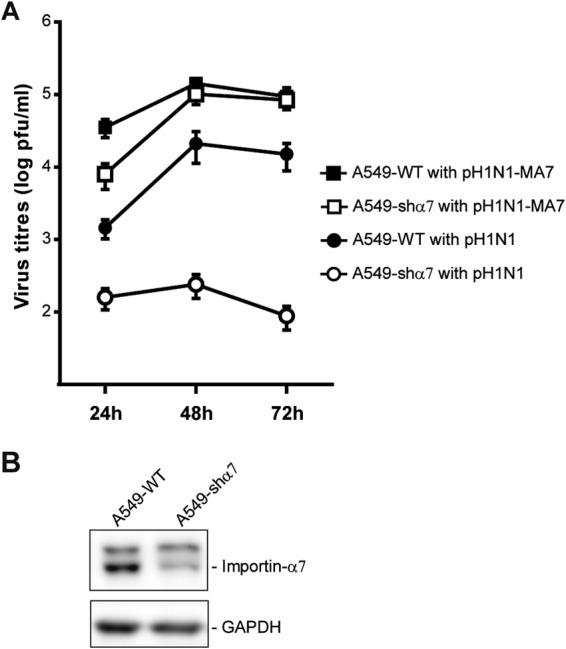
Replication kinetics in epithelial A549 and A549-shα7 cell lines infected with pH1N1-MA7 virus. (A) Human A549-WT and A549-shα7 cells were infected at an MOI of 0.1 with parental (pH1N1) or adapted (pH1N1-MA7) viruses. Virus titers of the supernatants were measured by plaque assay at the indicated hours p.i. Data are expressed as means ± SEM of viral titers (n = 8 to 12). (B) Confirmation of importin-α7 knockdown in human A549 cells by Western blotting. Since importin-α7 antibody cross-reacts with importin-α5, the doublet represents importin-α5 (upper band) and importin-α7 (lower band). GAPDH was used as a loading control.
Compared to the pH1N1 parental strain, pH1N1-MA7 mutations remarkably enhanced virus replication in both cell lines, by about 1 log in parental cells (A549-WT) and 3 logs in importin-α7 knockdown cell lines (A549-shα7). However, both parental pH1N1 and adapted pH1N1-MA7 viruses replicated better when importin-α7 expression was not depleted. This suggests that alternative strategies are exploited to overcome the importin-α7 requirement to restore viral replication efficiency in human cells.
Importin-α7 dependency remains upon adaptation.
We then investigated the effect of these adaptive mutations on virus replication in cells where the entire importin-α7 gene is deleted in order to abolish the possibility that residual importin-α7 still could affect viral replication (Fig. 7). Here, we studied virus RNA accumulation by primer extension analysis in monocycle infections using MEFs isolated from WT or α7−/− mice (12). Adaptive mutations increased vRNA levels in WT and α7−/− cells (Fig. 7A and B). Specifically, vRNA accumulation was increased 220.7% in MEF-α7−/− cells and 2,360.9% in MEF-WT cells. However, importin-α7 dependency persisted with all recombinant viruses analyzed. Accordingly, vRNA accumulation was remarkably reduced during infection of MEF-α7−/− compared to that with MEF-WT cells (Fig. 7C). These data show that importin-α7 dependency remains upon adaptation to α7−/− mice. However, circumvention of the importin-α7 requirement seems to occur by an alternative pathway that results in increased replicative fitness.
FIG 7.
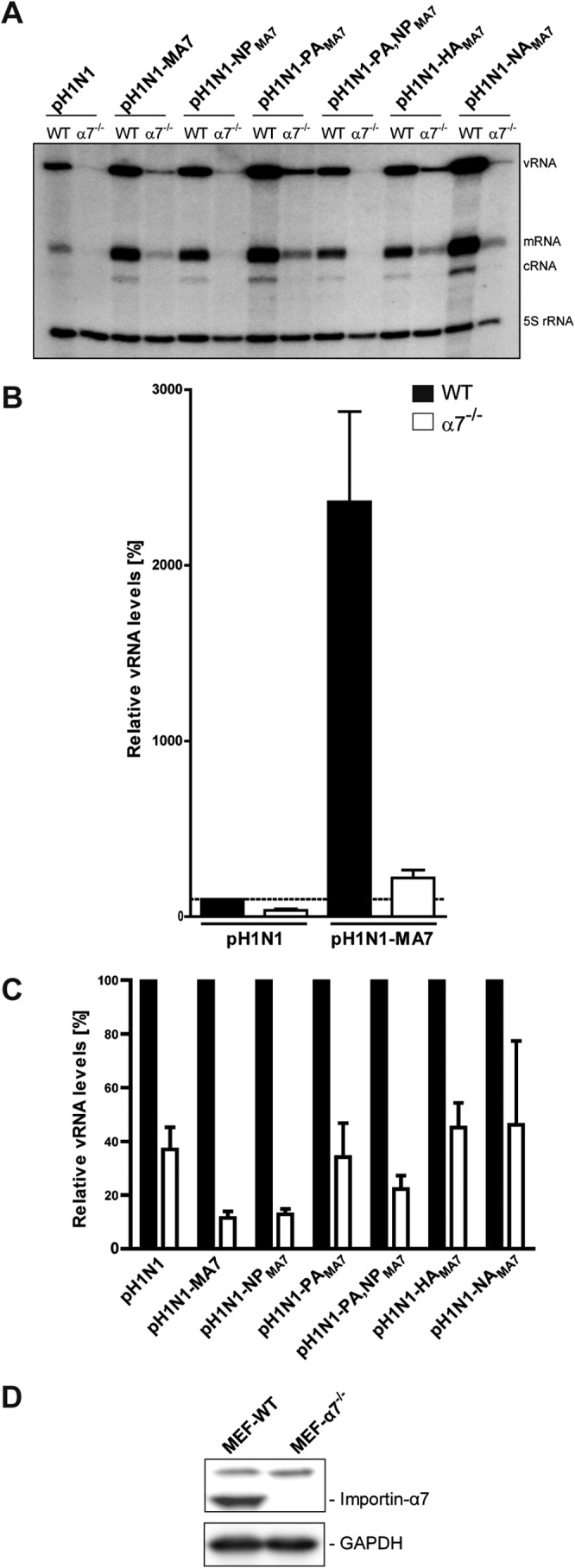
Viral RNA accumulation in WT and α7−/− MEFs infected with pH1N1-MA7 virus. (A) WT and α7−/− MEFs were infected at an MOI of 2 with parental (pH1N1), adapted (pH1N1-MA7), or SGR (pH1N1-PAMA7, pH1N1-NPMA7, pH1N1-PA,NPMA7, pH1N1-HAMA7, and pH1N1-NAMA7) viruses. After 24 h, total RNA was isolated and analyzed by NP gene-specific primer extension. A primer specific for 5S rRNA was used for normalization. (B) vRNA accumulation in MEF-WT (black bars) and MEF-α7−/− (white bars) infected with the parental and adapted viruses. Values were expressed relative to vRNA levels in MEF-WT infected with pH1N1 virus, which was set to 100%. (C) vRNA accumulation was expressed relative to vRNA levels in MEF-WT, which was set to 100% for every virus tested. Data shown represent means ± SEM (n = 9 to 12). (D) Importin-α7 expression in MEF cells was checked by Western blotting. Since importin-α7 antibody cross-reacts with importin-α5, the doublet represents importin-α5 (upper band) and importin-α7 (lower band). GAPDH was used as a loading control.
DISCUSSION
Antiviral drugs play a key role in mitigating influenza disease severity (27), since most of the circulating influenza virus strains are becoming increasingly resistant against currently available drugs that are directed against viral proteins. Thus, the development of novel antiviral strategies is fundamental (28). Targeting cellular proteins required for viral replication is considered a promising strategy, since cellular proteins generally are less prone to mutations than viral proteins (3).
Here, host factors that are essential for viral infection but not for cellular viability are considered excellent targets for therapeutic intervention (3). In this study, we have chosen importin-α7, which is crucial for human-type influenza virus replication as well as severe lung damage and virulence in mice (7, 9, 16). Most importantly, adult mice lacking the importin-α7 gene appear healthy (8, 10). Thus, this is a particularly attractive factor for transient inhibition to combat acute influenza virus infection. Additionally, recent reports highlight that importin-α belongs to the few host proteins that possess sufficient interactive surface area for virtual screening and host-directed drug discovery (3).
Moreover, antiviral compounds targeting importin-α proteins might comprise a novel panviral strategy to combat various viral infections, since different importin-α isoforms were reported to be utilized by many other viruses, such as hepatitis C virus, HIV, severe acute respiratory syndrome coronavirus, Ebola virus, and dengue virus (29–38). However, developing and evaluating novel antiviral candidates often is time and money consuming. Therefore, we sought to study the feasibility of importin-α7 as an attractive cellular target to combat pandemic influenza virus using an in vivo model. Here, we infected α7−/− mice with a 2009 pH1N1 influenza virus and challenged for potential viral escape by serial lung-to-lung passages. Surprisingly, only five passages were required until 100% lethality was reached in α7−/− mice. Importantly, pH1N1-MA7 became approximately 10 times more virulent during viral escape in α7−/− mice than the parental virus strain in WT animals. In contrast, viral variants that escape antiviral drugs, such as oseltamivir, were reported to be as virulent as, but not more virulent than, the parental strain in mice (39). This finding calls for particular caution, since it shows that viral escape can easily occur and leads to the emergence of potentially more virulent strains. This is not in line with previous reports, where viral resistance could not be observed against cellular targets despite serial passaging in cell culture (40). Indeed, no resistance was observed when using the cellular MEK kinase as a target to inhibit influenza B virus replication. However, it should be noted that these studies were performed in cell culture experiments. Since influenza viruses infect several cell types besides epithelial cells, one can speculate that at least the number of cell types to produce potentially more virus variants in vivo would be higher than that in cell culture experiments. Moreover, some influenza virus infections may lead to suppression of innate and adaptive immune responses that might further facilitate the emergence of novel virus variants. As stated above, the different selective pressures in cell culture and the whole organism highlight the need for an adequate animal model to evaluate the risk from newly emerging host-targeting drug-resistant virus strains.
Interestingly, escape from importin-α7 requirement was mediated mainly by mutations in the RNP proteins. Thus, weight loss in α7−/− mice was observed only upon infection with recombinant viruses containing NPMA7 mutation and was further enhanced when combined with PAMA7 mutation. However, combination with adaptive HA and NA mutations was required for an entire circumvention of importin-α7 requirement. However, we did not test the single surface protein mutations combined with vRNP adaptive sites which might have been sufficient for lethality in mice. Thus, several adaptive pathways may have been utilized by the surface glycoproteins and the RNP to overcome the lack of importin-α7.
The PA subunit possesses endonuclease activity that plays a key role in the cap snatching that is required to initiate viral transcription. The PA-D27E mutation is located in the endonuclease domain but outside the active site (22, 41). Hence, this mutation could indirectly influence its endonuclease activity. The NP-G102R mutation is located opposite the oligomerization loop (42, 43). Moreover, the NP-G102R mutant showed a generally reduced binding affinity to other importin-α isoforms relevant for influenza virus replication and pathogenicity (8). This suggests that an alternative nuclear import pathway is preferred, such as the nonclassical nuclear import pathway that is independent of importin-α, like RanBP5, shown to be utilized by PB1 and PA (44). Future studies are required to analyze whether these RNP adaptive mutations represent adaptation to alternative nuclear import pathways or are representative of novel binding sites to viral or cellular proteins increasing virus replication.
Since full circumvention from importin-α7 requirement could be achieved only in combination of adaptive mutations in the RNP with those in HA and NA, drugs targeting crucial host factors might be combined with those preventing cell entry, as shown recently for SALPs (45), or with NA inhibitors, such as oseltamivir, inhibiting viral release to further reduce the risk of antiviral resistance. However, it should be noted that in this case, five mutations in four different gene segments were required to achieve resistance. This could be considered a rather higher resistance barrier compared to that of the single mutation in NA, NA-H274Y, that is sufficient to confer resistance to neuraminidase inhibitors (46). However, the fact that only five passages in vivo were sufficient to overcome importin-α7 requirement seems to be rather low. Clearly, future studies will be required to compare the selective pressures required in vitro and in vivo to overcome drug resistance.
The NA-Y170H mutation that occurred in this study is located in the inner part of the NA tetramer; thus, it is outside the active site of the enzyme (47). This mutation could affect the assembly of NA into tetramers. The receptor binding site (RBS) of HA constitutes three main structural elements: the 190-helix, the 220-loop, and the 130-loop (48). While the HA-K171E mutation is located near the HA RBS, the HA-D239G mutation is included in the 220-loop. Moreover, the D239G substitution corresponds to D222G mutation (H1 numbering) that has been associated with altered receptor specificity, as observed in severe cases of 2009 pandemic H1N1 influenza virus infections in humans (49, 50). As a result, these HA mutations might facilitate receptor binding, thereby increasing virulence in mice.
It should be noted that despite the successful circumvention of the importin-α7 requirement, the pH1N1-MA7 virus still showed dependency, suggesting that the alternative pathway is not entirely able to compensate for the absence of importin-α7. This further highlights that importin-α7 still represents a strong target, but viral escape nevertheless is rapidly possible if only one cellular target is chosen. Thus, future strategies should be directed toward targeting multiple viral and/or cellular factors to reduce the risk of antiviral resistance. This is even more important considering the fact that escape variants from host factors might even be more virulent, posing an increased risk for public health.
ACKNOWLEDGMENTS
This work was supported by grants from the European Union (FLUPHARM) (to G.G.), the Emmy-Noether Programme of the German Research Foundation (to G.G.) (GA 1575/1-1), the Medical Research Council (MRC) (to E.F.) (MR/K000241/1), and the Spanish Ministry of Science and Innovation (MICINN) (to B.O.) (FEDER BIO2011-22568 and EUI2009-04018). P.R.-I. was funded by the Alexander von Humboldt Foundation (3.3SPA/1142463 STP-2) and with a Boehringer Ingelheim Fonds travel grant (BIF TG Infante). D.P. was supported by a Polonsky Foundation Scholarship and Lincoln College, University of Oxford. J.B. was supported by a MICINN fellowship (FEDER BIO2008-0205). The Heinrich-Pette-Institute, Leibniz Institute for Experimental Virology, is supported by the Free and Hanseatic City of Hamburg and the Federal Ministry of Health.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
We thank Gökhan Arman-Kalcek and Ilara Hudjetz for excellent technical assistance.
REFERENCES
- 1.McCullers JA. 2005. Antiviral therapy of influenza. Expert Opin Investig Drugs 14:305–312. doi: 10.1517/13543784.14.3.305. [DOI] [PubMed] [Google Scholar]
- 2.Ison MG. 2011. Antivirals and resistance: influenza virus. Curr Opin Virol 1:563–573. doi: 10.1016/j.coviro.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Muller KH, Kakkola L, Nagaraj AS, Cheltsov AV, Anastasina M, Kainov DE. 2012. Emerging cellular targets for influenza antiviral agents. Trends Pharmacol Sci 33:89–99. doi: 10.1016/j.tips.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Ludwig S, Zell R, Schwemmle M, Herold S. 2014. Influenza, a One Health paradigm–novel therapeutic strategies to fight a zoonotic pathogen with pandemic potential. Int J Med Microbiol 304:894–901. doi: 10.1016/j.ijmm.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 5.Shaw ML. 2011. The host interactome of influenza virus presents new potential targets for antiviral drugs. Rev Med Virol 21:358–369. doi: 10.1002/rmv.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Planz O. 2013. Development of cellular signaling pathway inhibitors as new antivirals against influenza. Antiviral Res 98:457–468. doi: 10.1016/j.antiviral.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Hudjetz B, Gabriel G. 2012. Human-like PB2 627K influenza virus polymerase activity is regulated by importin-alpha1 and -alpha7. PLoS Pathog 8:e1002488. doi: 10.1371/journal.ppat.1002488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabriel G, Klingel K, Otte A, Thiele S, Hudjetz B, Arman-Kalcek G, Sauter M, Shmidt T, Rother F, Baumgarte S, Keiner B, Hartmann E, Bader M, Brownlee GG, Fodor E, Klenk HD. 2011. Differential use of importin-alpha isoforms governs cell tropism and host adaptation of influenza virus. Nat Commun 2:156. doi: 10.1038/ncomms1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Resa-Infante P, Thieme R, Ernst T, Arck PC, Ittrich H, Reimer R, Gabriel G. 2014. Importin-alpha7 is required for enhanced influenza A virus replication in the alveolar epithelium and severe lung damage in mice. J Virol 88:8166–8179. doi: 10.1128/JVI.00270-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rother F, Shmidt T, Popova E, Krivokharchenko A, Hugel S, Vilianovich L, Ridders M, Tenner K, Alenina N, Kohler M, Hartmann E, Bader M. 2011. Importin alpha7 is essential for zygotic genome activation and early mouse development. PLoS One 6:e18310. doi: 10.1371/journal.pone.0018310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am J Epidemiol 27:493–497. [Google Scholar]
- 12.Huegel S, Depping R, Dittmar G, Rother F, Cabot R, Sury MD, Hartmann E, Bader M. 2014. Identification of importin alpha 7 specific transport cargoes using a proteomic screening approach. Mol Cell Proteomics 13:1286–1298. doi: 10.1074/mcp.M112.026856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otte A, Gabriel G. 2011. 2009 Pandemic H1N1 influenza A virus strains display differential pathogenicity in C57BL/6J but not BALB/c mice. Virulence 2:563–566. doi: 10.4161/viru.2.6.18148. [DOI] [PubMed] [Google Scholar]
- 14.Otte A, Sauter M, Alleva L, Baumgarte S, Klingel K, Gabriel G. 2011. Differential host determinants contribute to the pathogenesis of 2009 pandemic H1N1 and human H5N1 influenza A viruses in experimental mouse models. Am J Pathol 179:230–239. doi: 10.1016/j.ajpath.2011.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stech J, Stech O, Herwig A, Altmeppen H, Hundt J, Gohrbandt S, Kreibich A, Weber S, Klenk HD, Mettenleiter TC. 2008. Rapid and reliable universal cloning of influenza A virus genes by target-primed plasmid amplification. Nucleic Acids Res 36:e139. doi: 10.1093/nar/gkn646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gabriel G, Dauber B, Wolff T, Planz O, Klenk HD, Stech J. 2005. The viral polymerase mediates adaptation of an avian influenza virus to a mammalian host. Proc Natl Acad Sci U S A 102:18590–18595. doi: 10.1073/pnas.0507415102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gabriel G, Herwig A, Klenk HD. 2008. Interaction of polymerase subunit PB2 and NP with importin alpha1 is a determinant of host range of influenza A virus. PLoS Pathog 4:e11. doi: 10.1371/journal.ppat.0040011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robb NC, Smith M, Vreede FT, Fodor E. 2009. NS2/NEP protein regulates transcription and replication of the influenza virus RNA genome. J Gen Virol 90:1398–1407. doi: 10.1099/vir.0.009639-0. [DOI] [PubMed] [Google Scholar]
- 19.Berman HM, Westbrook J, Feng Z, Gilliland G, Bhat TN, Weissig H, Shindyalov IN, Bourne PE. 2000. The Protein Data Bank. Nucleic Acids Res 28:235–242. doi: 10.1093/nar/28.1.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oliva B, Planas-Iglesias J, Bonet J, Marín-López MA, Feliu E, Gursoy A. 30 March 2012. Structural bioinformatics of proteins: predicting the tertiary and quaternary structure of proteins from sequence, protein-protein interactions. Comput Exp Tools doi: 10.5772/37856. [DOI] [Google Scholar]
- 21.Altschul SF, Madden TL, Schaffer AA, Zhang J, Zhang Z, Miller W, Lipman DJ. 1997. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res 25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kowalinski E, Zubieta C, Wolkerstorfer A, Szolar OH, Ruigrok RW, Cusack S. 2012. Structural analysis of specific metal chelating inhibitor binding to the endonuclease domain of influenza pH1N1 (2009) polymerase. PLoS Pathog 8:e1002831. doi: 10.1371/journal.ppat.1002831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van der Vries E, Collins PJ, Vachieri SG, Xiong X, Liu J, Walker PA, Haire LF, Hay AJ, Schutten M, Osterhaus AD, Martin SR, Boucher CA, Skehel JJ, Gamblin SJ. 2012. H1N1 2009 pandemic influenza virus: resistance of the I223R neuraminidase mutant explained by kinetic and structural analysis. PLoS Pathog 8:e1002914. doi: 10.1371/journal.ppat.1002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu J, Stevens DJ, Haire LF, Walker PA, Coombs PJ, Russell RJ, Gamblin SJ, Skehel JJ. 2009. Structures of receptor complexes formed by hemagglutinins from the Asian influenza pandemic of 1957. Proc Natl Acad Sci U S A 106:17175–17180. doi: 10.1073/pnas.0906849106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fiser A, Sali A. 2003. Modeller: generation and refinement of homology-based protein structure models. Methods Enzymol 374:461–491. [DOI] [PubMed] [Google Scholar]
- 26.Melo F, Feytmans E. 1998. Assessing protein structures with a non-local atomic interaction energy. J Mol Biol 277:1141–1152. doi: 10.1006/jmbi.1998.1665. [DOI] [PubMed] [Google Scholar]
- 27.Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. 2006. Strategies for mitigating an influenza pandemic. Nature 442:448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Govorkova EA, McCullers JA. 2013. Therapeutics against influenza. Curr Top Microbiol Immunol 370:273–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frieman M, Yount B, Heise M, Kopecky-Bromberg SA, Palese P, Baric RS. 2007. Severe acute respiratory syndrome coronavirus ORF6 antagonizes STAT1 function by sequestering nuclear import factors on the rough endoplasmic reticulum/Golgi membrane. J Virol 81:9812–9824. doi: 10.1128/JVI.01012-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kobiler O, Drayman N, Butin-Israeli V, Oppenheim A. 2012. Virus strategies for passing the nuclear envelope barrier. Nucleus 3:526–539. doi: 10.4161/nucl.21979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Labokha AA, Fassati A. 2013. Viruses challenge selectivity barrier of nuclear pores. Viruses 5:2410–2423. doi: 10.3390/v5102410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neufeldt CJ, Joyce MA, Levin A, Steenbergen RH, Pang D, Shields J, Tyrrell DL, Wozniak RW. 2013. Hepatitis C virus-induced cytoplasmic organelles use the nuclear transport machinery to establish an environment conducive to virus replication. PLoS Pathog 9:e1003744. doi: 10.1371/journal.ppat.1003744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pryor MJ, Rawlinson SM, Butcher RE, Barton CL, Waterhouse TA, Vasudevan SG, Bardin PG, Wright PJ, Jans DA, Davidson AD. 2007. Nuclear localization of dengue virus nonstructural protein 5 through its importin alpha/beta-recognized nuclear localization sequences is integral to viral infection. Traffic 8:795–807. doi: 10.1111/j.1600-0854.2007.00579.x. [DOI] [PubMed] [Google Scholar]
- 34.Ramanan P, Shabman RS, Brown CS, Amarasinghe GK, Basler CF, Leung DW. 2011. Filoviral immune evasion mechanisms. Viruses 3:1634–1649. doi: 10.3390/v3091634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu W, Edwards MR, Borek DM, Feagins AR, Mittal A, Alinger JB, Berry KN, Yen B, Hamilton J, Brett TJ, Pappu RV, Leung DW, Basler CF, Amarasinghe GK. 2014. Ebola virus VP24 targets a unique NLS binding site on karyopherin alpha 5 to selectively compete with nuclear import of phosphorylated STAT1. Cell Host Microbe 16:187–200. doi: 10.1016/j.chom.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Resa-Infante P, Gabriel G. 2013. The nuclear import machinery is a determinant of influenza virus host adaptation. Bioessays 35:23–27. doi: 10.1002/bies.201200138. [DOI] [PubMed] [Google Scholar]
- 37.Caly L, Wagstaff KM, Jans DA. 2012. Nuclear trafficking of proteins from RNA viruses: potential target for antivirals? Antiviral Res 95:202–206. doi: 10.1016/j.antiviral.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 38.Oksayan S, Ito N, Moseley G, Blondel D. 2012. Subcellular trafficking in rhabdovirus infection and immune evasion: a novel target for therapeutics. Infect Disord Drug Targets 12:38–58. doi: 10.2174/187152612798994966. [DOI] [PubMed] [Google Scholar]
- 39.Hamelin ME, Baz M, Abed Y, Couture C, Joubert P, Beaulieu E, Bellerose N, Plante M, Mallett C, Schumer G, Kobinger GP, Boivin G. 2010. Oseltamivir-resistant pandemic A/H1N1 virus is as virulent as its wild-type counterpart in mice and ferrets. PLoS Pathog 6:e1001015. doi: 10.1371/journal.ppat.1001015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ludwig S, Wolff T, Ehrhardt C, Wurzer WJ, Reinhardt J, Planz O, Pleschka S. 2004. MEK inhibition impairs influenza B virus propagation without emergence of resistant variants. FEBS Lett 561:37–43. doi: 10.1016/S0014-5793(04)00108-5. [DOI] [PubMed] [Google Scholar]
- 41.Pflug A, Guilligay D, Reich S, Cusack S. 2014. Structure of influenza A polymerase bound to the viral RNA promoter. Nature 516:355–360. doi: 10.1038/nature14008. [DOI] [PubMed] [Google Scholar]
- 42.Ye Q, Krug RM, Tao YJ. 2006. The mechanism by which influenza A virus nucleoprotein forms oligomers and binds RNA. Nature 444:1078–1082. doi: 10.1038/nature05379. [DOI] [PubMed] [Google Scholar]
- 43.Ng AK, Zhang H, Tan K, Li Z, Liu JH, Chan PK, Li SM, Chan WY, Au SW, Joachimiak A, Walz T, Wang JH, Shaw PC. 2008. Structure of the influenza virus A H5N1 nucleoprotein: implications for RNA binding, oligomerization, and vaccine design. FASEB J 22:3638–3647. doi: 10.1096/fj.08-112110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deng T, Engelhardt OG, Thomas B, Akoulitchev AV, Brownlee GG, Fodor E. 2006. The role of Ran binding protein 5 (RanBP5) in the nuclear import and assembly of the influenza virus RNA polymerase complex. J Virol 80:11911–11919. doi: 10.1128/JVI.01565-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hoffmann J, Schneider C, Heinbockel L, Brandenburg K, Reimer R, Gabriel G. 2014. A new class of synthetic anti-lipopolysaccharide peptides inhibits influenza A virus replication by blocking cellular attachment. Antiviral Res 104:23–33. doi: 10.1016/j.antiviral.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 46.Gubareva LV, Trujillo AA, Okomo-Adhiambo M, Mishin VP, Deyde VM, Sleeman K, Nguyen HT, Sheu TG, Garten RJ, Shaw MW, Fry AM, Klimov AI. 2010. Comprehensive assessment of 2009 pandemic influenza A (H1N1) virus drug susceptibility in vitro. Antivir Ther 15:1151–1159. doi: 10.3851/IMP1678. [DOI] [PubMed] [Google Scholar]
- 47.Varghese JN, Laver WG, Colman PM. 1983. Structure of the influenza virus glycoprotein antigen neuraminidase at 2.9 A resolution. Nature 303:35–40. doi: 10.1038/303035a0. [DOI] [PubMed] [Google Scholar]
- 48.Yang H, Carney P, Stevens J. 2010. Structure and receptor binding properties of a pandemic H1N1 virus hemagglutinin. PLoS Curr 2:RRN1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rykkvin R, Kilander A, Dudman SG, Hungnes O. 2013. Within-patient emergence of the influenza A(H1N1)pdm09 HA1 222G variant and clear association with severe disease, Norway. Euro Surveill 18:20369. [PubMed] [Google Scholar]
- 50.Kilander A, Rykkvin R, Dudman SG, Hungnes O. 2010. Observed association between the HA1 mutation D222G in the 2009 pandemic influenza A(H1N1) virus and severe clinical outcome, Norway 2009-2010. Euro Surveill 15:19498. [DOI] [PubMed] [Google Scholar]