ABSTRACT
African horse sickness virus (AHSV) is a virus species in the genus Orbivirus of the family Reoviridae. There are nine serotypes of AHSV showing different levels of cross neutralization. AHSV is transmitted by species of Culicoides biting midges and causes African horse sickness (AHS) in equids, with a mortality rate of up to 95% in naive horses. AHS has become a serious threat for countries outside Africa, since endemic Culicoides species in moderate climates appear to be competent vectors for the related bluetongue virus (BTV). To control AHS, live-attenuated vaccines (LAVs) are used in Africa. We used reverse genetics to generate “synthetic” reassortants of AHSV for all nine serotypes by exchange of genome segment 2 (Seg-2). This segment encodes VP2, which is the serotype-determining protein and the dominant target for neutralizing antibodies. Single Seg-2 AHSV reassortants showed similar cytopathogenic effects in mammalian cells but displayed different growth kinetics. Reverse genetics for AHSV was also used to study Seg-10 expressing NS3/NS3a proteins. We demonstrated that NS3/NS3a proteins are not essential for AHSV replication in vitro. NS3/NS3a of AHSV is, however, involved in the cytopathogenic effect in mammalian cells and is very important for virus release from cultured insect cells in particular. Similar to the concept of the bluetongue disabled infectious single animal (BT DISA) vaccine platform, an AHS DISA vaccine platform lacking NS3/NS3a expression was developed. Using exchange of genome segment 2 encoding VP2 protein (Seg-2[VP2]), we will be able to develop AHS DISA vaccine candidates for all current AHSV serotypes.
IMPORTANCE African horse sickness virus is transmitted by species of Culicoides biting midges and causes African horse sickness in equids, with a mortality rate of up to 95% in naive horses. African horse sickness has become a serious threat for countries outside Africa, since endemic Culicoides species in moderate climates are supposed to be competent vectors. By using reverse genetics, viruses of all nine serotypes were constructed by the exchange of Seg-2 expressing the serotype-determining VP2 protein. Furthermore, we demonstrated that the nonstructural protein NS3/NS3a is not essential for virus replication in vitro. However, the potential spread of the virus by biting midges is supposed to be blocked, since the in vitro release of the virus was strongly reduced due to this deletion. VP2 exchange and NS3/NS3a deletion in African horse sickness virus were combined in the concept of a disabled infectious single animal vaccine for all nine serotypes.
INTRODUCTION
African horse sickness virus (AHSV) is the causative agent of African horse sickness (AHS), a disease listed by the World Organisation for Animal Health (OIE). The virus can cause different forms of disease ranging from a mild fever to an acute form (1, 2). The disease can cause mortality in up to 95% of naive horses (3). AHS is endemic to sub-Saharan Africa, where it has a huge economic impact by animal losses and reduction of draft power, transportation, and trade (4). AHSV is transmitted by midges, of which only a few Culicoides species are known competent insect vectors (5–7). In Europe, AHS outbreaks would result in large economic losses to the equestrian industry and would have an enormous emotional impact on owners of pet horses. AHS is associated with the presence of competent insect vectors, and spread could expand by various factors, including climate change (8, 9). Recently, endemic Culicoides species in countries with a moderate climate have appeared to be competent vectors of bluetongue virus serotype 8 (BTV8) (10–12). These findings imply that AHS-free countries with milder climates are at risk of outbreaks of this disease (13). The last AHS outbreak in Europe caused by serotype 4 was reported in Spain and Portugal and also spread to Morocco (14, 15). This outbreak was controlled by the use of a live-attenuated vaccine (LAV) (2). In a later stage, an inactivated AHS vaccine for serotype 4 was also developed (16). LAVs are currently used in Africa but have not been registered for countries outside Africa (3). Several approaches have been explored to develop safe AHS vaccines, but these have not been marketed yet (17–22).
AHSV (genus Orbivirus; family Reoviridae) is closely related to BTV, epizootic hemorrhagic disease virus, and equine encephalosis virus (23). Orbiviruses, of which BTV is the prototype, are nonenveloped viruses containing a genome of 10 double-stranded RNA (dsRNA) segments (segment 1 [Seg-1] to Seg-10) and consist of three protein layers, namely, VP3 (subcore), VP7 (core), and the outer shell proteins VP2 and VP5 (23). VP2 is the serotype-determining protein and the major target for neutralizing antibodies (NAbs), whereas VP7 is the target of serogroup-specific serological tests (24–26). In addition, the orbivirus particle contains VP1, VP4, and VP6, which constitute the replication proteins. Nonstructural orbivirus proteins NS1 to -4 are not incorporated into the virus particle.
Reverse genetics has been developed for AHSV (27) and for BTV, including nonvirulent and virulent BTV strains (28, 29). This technology has been used to generate “synthetic” BTV reassortants by the exchange of genome segments (29–34). Genetic modification of Seg-9 and -10 has shown that the nonstructural proteins NS4 and NS3/NS3a, respectively, are not essential for BTV replication in vitro and in vivo (35–37).
A novel bluetongue disabled infectious single animal (BT DISA) vaccine based on LAV strain BTV6/net08 and NS3/NS3a knockout mutations in Seg-10 abolished virulence and viremia (37). Consequently, the uptake of the BT DISA vaccine virus by vectors can be prevented. Furthermore, release of the BT DISA vaccine virus from Culicoides cells in vitro is strongly reduced, which suggests that onward spread by biting midges is also highly unlikely (36, 38). The prototype of the BT DISA vaccine for serotype 8 induces serotype-specific protection and enables differentiation of infected from vaccinated animals (DIVA) (39, 40). The BT DISA vaccine platform has been explored for more serotypes by VP2 exchange or incorporation of chimeric VP2 (41).
Here, we used reverse genetics for strain AHSV4LP to explore the exchange of serotype-determining Seg-2[VP2] for all nine AHSV serotypes. In addition, the role of the NS3/NS3a proteins of AHSV4LP was studied. Finally, VP2 exchange and NS3/NS3a knockout mutations were combined. These results demonstrate the potential of an AHS DISA vaccine platform for all nine AHSV serotypes.
MATERIALS AND METHODS
Cell lines and viruses.
BSR cells (a clone of baby hamster kidney cells [42]) were cultured in Dulbecco's modified Eagle's medium (DMEM; Invitrogen) containing 5% fetal bovine serum (FBS) and antibiotics (100 IU/ml penicillin, 100 μg/ml streptomycin, and 2.5 μg/ml amphotericin B). Culicoides variipennis Kenyon cells (KC) were grown in modified Schneider's drosophila medium with 15% heat-inactivated FBS, 100 IU/ml penicillin, and 100 μg/ml streptomycin (43).
A LAV for AHSV serotype 4 was generated ∼50 years ago by passage of virulent AHSV HS 32/62 in suckling mice and BHK-21 cells, followed by selection of large plaques on Vero cells (2). The official passage number is HS32/62-10S-10BHK-3LP-7Vero. In this study, we called the virus AHSV4LP. All other viruses described in this study are based on AHSV4LP and were generated by reverse genetics. Virus stocks were obtained by infection of fresh BSR cells at a multiplicity of infection (MOI) of 0.1 and stored at 4°C. Virus titers were determined by endpoint dilution and expressed as log10 50% tissue culture infective doses (TCID50) per milliliter.
cDNAs of AHSV genome segments.
Genome segments of AHSV4LP were sequenced by using next-generation sequencing and conventional sequencing of full-length amplified cDNAs (44). cDNAs of complete genome segments of AHSV4LP (GenBank accession numbers KM820849 to KM820858) were synthesized by GenScript Corporation (Piscataway, NJ, USA) in appropriate plasmids under the control of the T7 promoter. Restriction enzyme sites suitable for full-length runoff RNA transcription were introduced as previously described for BTV (29).
Similarly, plasmids with full-length cDNAs of Seg-2[VP2] of all other serotypes and Seg-6[VP5] of serotypes 3 and 6 were designed (GenBank accession numbers KF859987, KF859997, KM886355, KM886345, KF860007, KF860017, KF860027, and KF860037 and accession numbers KM886359 and KF860011, respectively). Internal SapI sites of cDNAs of Seg-2 of serotypes 2 and 3 (accession numbers KF859997 and KM886355, respectively) were mutated by silent point mutations to allow full-length runoff transcription after SapI digestion. cDNAs of mutated Seg-10 were synthetically derived by GenScript Corporation (Piscataway NJ, USA) or constructed by using standard procedures. Plasmid DNA was linearized to enable runoff transcription, as previously described (29). Synthesized RNAs were purified by using the MEGAclear kit (Ambion), according to the manufacturer's protocol, and stored at −80°C.
Open reading frames (ORFs) encoding VP1, -3, -4, -6, and -7 and NS1 and -2 of AHSV4LP were synthesized (GenScript Corporation) and inserted into expression plasmid HC pSMART or LC pSMART under the control of the immediate early promoter of human cytomegalovirus by using standard procedures (45).
All plasmids were transformed and maintained in Escherichia coli strain DH5α cells (Invitrogen) and isolated by using the High Pure plasmid isolation kit (Roche) or the QIAfilter Plasmid Midi kit (Qiagen).
Rescue of AHSV4LP, reassortants, and mutants.
BSR cell monolayers in wells of M24 plates (2 cm2) at 15 to 20% confluence were transfected with 300 ng DNA of plasmids expressing VP1, -3, -4, -6, and -7 and NS1 and -2 in equimolar amounts by using 0.75 μl Lipofectamine 2000 (1:2.5, 1 mg/ml; Invitrogen) in Opti-MEM I reduced-serum medium, according to the manufacturer's instructions. At 24 h posttransfection, transfected monolayers were transfected again with a total of 600 ng of all 10 capped runoff RNA transcripts in equimolar amounts. At 22 h post-RNA transfection, the transfection mix was replaced with 1 ml DMEM supplemented with 5% FBS, 100 IU/ml penicillin, 100 μg/ml streptomycin, and 2.5 μg/ml amphotericin B.
All transfections were performed in duplicate. At 48 h post-RNA transfection, cell culture medium was harvested, and the transfected monolayers were passed once after trypsinization. Wells of this passage of transfected monolayers were immunostained by using an immunoperoxidase monolayer assay (IPMA). The supernatant was harvested from monolayers showing cytopathogenic effects (CPE) to prepare a virus stock. Stained plaques without CPE suggested virus replication, and duplicate wells of these plaques were passed 1:5. Passage of transfected cells was repeated in anticipation of visible CPE or increased numbers of immunostained plaques as an indicator of virus replication. Cells were passaged until at least 50% of the monolayer either showed CPE or was immunostained. Virus was harvested, and clarified supernatants were stored at 4°C.
When immunostaining was negative after sequential passages, the attempt to rescue the virus was considered unsuccessful. Rescue attempts were repeated at least twice in order to conclude that virus could not be recovered.
Sequencing of Seg-2, Seg-6, and Seg-10.
Viral RNA of the generated mutants and reassortants was isolated from 200 μl of infected-cell culture medium by using the High Pure viral RNA kit (Roche). Seg-10 was entirely amplified, and Seg-2 and Seg-6 were partially amplified by using appropriate primers and the One-Step reverse transcription-PCR (RT-PCR) kit (Qiagen). Amplicons were purified by using the Zymoclean gel DNA recovery kit and sequenced according to standard procedures by using the ABI Prism 3130 genetic analyzer (Applied Biosystems), and sequences were verified by using Lasergene SeqMan Pro software (version 11; DNASTAR).
Immunoperoxidase monolayer assay.
Expression of virus proteins was determined by an IPMA according to standard procedures (46). Monoclonal antibody (MAb) 10AE12 and MAbs 8F9, 1B4, 1E7, and 4D3 are directed to VP5 and NS3 of AHSV4LP, respectively (generous gifts from Ingenasa, Spain). Monospecific polyclonal guinea pig (GP) sera raised against baculovirus-expressed VP2 proteins (anti-VP2 GP serum) of different AHSV serotypes were reported recently (47). Conjugated rabbit anti-mouse serum and conjugated rabbit anti-GP serum were commercially purchased (Dako).
Infected monolayers were fixed with methanol-acetone (1:1) or 4% paraformaldehyde in PBS. To study transient NS3/NS3a expression, BSR cell monolayers were first infected by recombinant fowlpox virus expressing DNA-dependent T7 RNA polymerase (48). After 1.5 h, unbound virus was removed, and monolayers were washed with Opti-MEM I reduced-serum medium and subsequently transfected with a plasmid harboring mutated Seg-10 under the control of the T7 promoter, as described above. Medium was replaced by DMEM after 4 h, and at 24 h posttransfection, monolayers were fixed as described above.
Immunostaining was performed with anti-VP5 MAb, anti-NS3 MAb, or 500×-diluted anti-VP2 GP serum followed by conjugated rabbit anti-mouse serum or conjugated rabbit anti-GP serum. Generally, an IPMA with anti-VP5 MAb was performed to confirm infection or transfection, whereas an IPMA with anti-VP2 GP sera showed serotype-specific immunostaining, and an IPMA with anti-NS3 MAbs was used to study NS3/NS3a expression.
Plaque morphology.
BSR cell monolayers were infected with NS3/NS3a mutants of AHSV4LP at an MOI of 0.1, 0.01, or 0.001 and incubated under overlay medium (1× Eagle's minimal essential medium supplemented with 0.25% sodium bicarbonate, 5% FBS, antibiotics, and 1% methylcellulose). Monolayers were fixed with methanol-acetone (1:1) at the indicated hours postinfection (hpi) and immunostained with anti-VP2 GP serum against serotype 4. CPE of separate plaques were compared and semiquantified as having normal, small, or no CPE.
Virus growth kinetics on BSR cells and KC.
To determine virus growth, BSR cells were infected with AHSV1LP to AHSV9LP in duplicate in wells of M24 plates at an MOI of 0.01. Each experiment was repeated at least once with independently prepared virus stocks. After attachment of virus to cells for 1.5 h, the medium with unbound virus was removed. Monolayers were washed once with culture medium, 1 ml of culture medium was added, and incubation was continued. Cells and medium were harvested at 0, 16, 24, and 48 hpi. Virus was harvested by freeze-thawing at −80°C and centrifugation and stored at −80°C.
To determine virus release, confluent BSR cell or KC monolayers in M24-well plates were infected with Seg-10 mutants of AHSV4LP in duplicate at an MOI of 0.1. Each experiment was repeated at least once with independently prepared virus stocks. After attachment of virus to cells for 1.5 h at 37°C for BSR cells and 28°C for KC, the medium with unbound virus was removed. Monolayers were washed once with culture medium, 1 ml of culture medium was added, and incubation was continued. At the indicated time points (6, 24, 48, and 72 hpi), culture medium was harvested, and the remaining attached cells were collected in 1 ml of fresh medium. Virus in cell fractions was harvested by freeze-thawing at −80°C and centrifugation and stored at −80°C.
Virus titers were determined by endpoint dilution on BSR cells and expressed as log10 TCID50 per milliliter. Therefore, BSR cells were infected with a 10-fold dilution of samples and grown for 72 h. Wells were immunostained with the respective anti-VP2 GP serum or VP5-directed MAb in order to visualize plaques not showing CPE.
RESULTS
Single Seg-2[VP2] synthetic reassortants of AHSV.
Reverse genetics of strain AHSV4LP was developed and will be described in detail elsewhere. Briefly, transfection of expression plasmids for VP1, -3, -4, -6, and -7 and NS1 and -2 of AHSV4LP was followed by transfection of a set of 10 capped runoff RNA transcripts. Initially, reverse genetics was used to exchange the genome segments Seg-2[VP2] and Seg-6[VP5] of serotypes 3 and 6 in AHSV4LP (not shown). Virus rescue was detected by visualization of CPE in freshly infected BSR cell monolayers, Seg-2 and Seg-6 were detected by partial sequencing, and the serotype of these synthetic reassortants was confirmed by IPMAs with serotype-specific anti-VP2 GP sera.
Since the exchange of both segments encoding outer shell proteins appeared flexible, we studied the exchange of the single Seg-2[VP2] reassortant in LAV strain AHSV4LP. Therefore, the set of capped runoff RNA transcripts of AHSV4LP used for transfection was completed with the capped runoff RNA transcript of one Seg-2 of each of the AHSV serotypes. A set of AHSV4LP-related viruses (AHSVxLP, where x indicates the serotype of Seg-2[VP2]) for all nine serotypes, designated AHSV1LP to AHSV9LP, was generated (Table 1). AHSV1LP to AHSV9LP were identified by IPMAs with the respective serotype-specific anti-VP2 GP serum and partial sequencing of Seg-2. These viruses have the same backbone and have only different Seg-2s encoding the serotype-determining VP2 protein.
TABLE 1.
IPMA results for single Seg-2-typed reassortants of AHSV4LPa
| Seg-2-typed AHSVxLP | Staining of GP sera against VP2 of AHSV serotype: |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| AHSV1LP | +++ | ||||||||
| AHSV2LP | +++ | ||||||||
| AHSV3LP | +++ | + | + | + | |||||
| AHSV4LP | +++ | + | + | ||||||
| AHSV5LP | +++ | ||||||||
| AHSV6LP | +++ | ||||||||
| AHSV7LP | + | + | + | +++ | |||||
| AHSV8LP | ± | ± | + | +++ | |||||
| AHSV9LP | + | + | + | ++ | |||||
Immunostaining was semiquantitated as very strong, strong, weak, very weak, and negative (+++, ++, +, ±, and −, respectively).
Serotype specificity and virus growth of AHSV1LP to AHSV9LP.
BSR cell monolayers infected with AHSVxLP viruses were immunostained with monoserotype polyvalent anti-VP2 GP sera of each of the nine AHSV serotypes (Table 1). Immunostaining was very strong for the homologous anti-VP2 GP serum. AHSVxLP viruses of serotypes 1, 2, 5, and 6 were stained only with homologous anti-VP2 GP serum. Furthermore, anti-VP2 GP serum for serotypes 1, 2, 8, and 9 immunostained only BSR cells infected with the homologous AHSVxLP virus and not with other AHSVxLP variants. However, several anti-VP2 GP sera, in particular those raised against VP2 of serotypes 4, 6, and 7, also showed weak immunostaining with several heterologous AHSVxLP viruses (Table 1). Despite this weak immunostaining, AHSV1LP to AHSV9LP are clearly distinguishable by the set of nine anti-VP2 GP sera used at a standardized dilution.
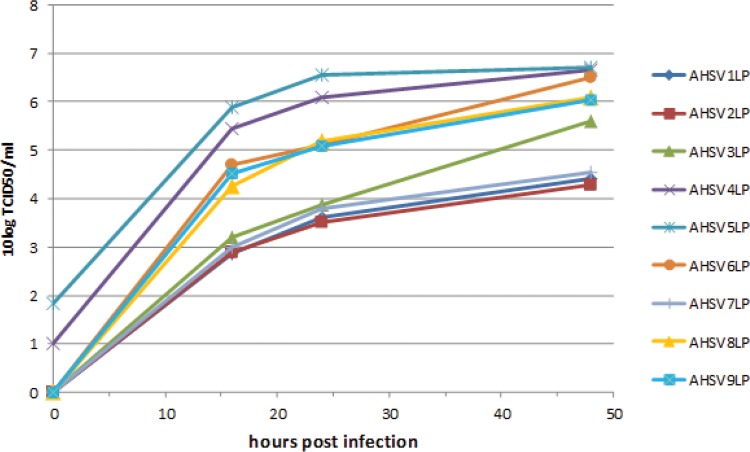
Growth of AHSV1LP to AHSV9LP was studied in more detail by multistep growth curves in BSR cells. Similar growth curves were obtained for independently derived virus stocks. Generally, virus growth differed considerably for several AHSVxLP viruses and could be divided into three groups: serotypes 4 and 5; serotypes 6, 8, and 9; and serotypes 1, 2, 3, and 7 (Fig. 1). Obviously, AHSV4LP and AHSV5LP showed growth characteristics similar to those of AHSVxLP of serotypes 6, 8, and 9 but started at a higher titer at 0 hpi. AHSVxLP viruses of serotypes 1, 2, 3, and 7 showed retarded growth early after infection (16 hpi). Virus growth kinetics from 16 hpi onwards were very similar for all AHSVxLP viruses. These results indicated that VP2 exchange can affect virus growth in vitro, which is most obvious early after infection.
FIG 1.
Virus growth kinetics of single Seg-2 reassortants of AHSV4LP (AHSVxLP) in BSR cells. BSR cell monolayers were infected with AHSVxLP in 2-cm2 wells at an MOI of 0.1. Virus titers were determined at 0, 16, 24, and 48 h postinfection and expressed as log10 TCID50 per milliliter.
NS3/NS3a proteins are not essential for in vitro AHSV replication.
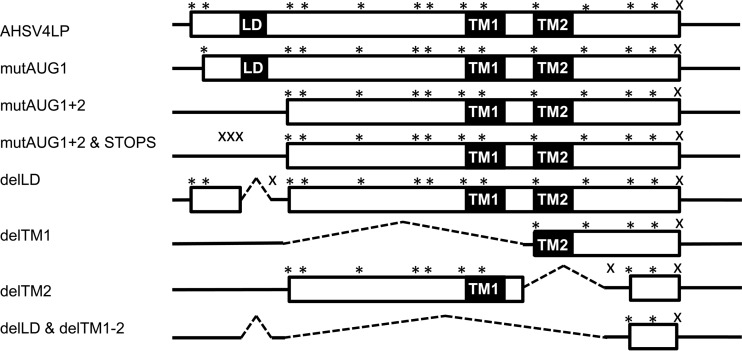
NS3/NS3a of AHSV was studied by the introduction of several mutations into Seg-10. First, the start codon of NS3 (mutAUG1), the start codons of NS3 and NS3a (mutAUG1+2), and three additional in-frame stop codons downstream of these mutated start codons (mutAUG1+2&STOPS) were studied (Fig. 2). All mutations were successfully incorporated into Seg-10 of AHSV4LP. Immunostaining of infected monolayers with NS3-directed MAbs was still positive for mutAUG1, indicating expression of the NS3a protein. Immunostaining was negative for mutAUG1+2 and mutAUG1+2&STOPS (Table 2). Transient translation from DNA-dependent T7 RNA polymerase-driven transcription (see Materials and Methods) is more sensitive, and transient expression of mutAUG1+2 and mutAUG1+2&STOPS showed immunostaining with NS3 MAbs, which suggested weak NS3-related expression by viruses with the respective mutated Seg-10. To ensure the knockout of any NS3-related translation, mutAUG1+2 was combined with an out-of-frame deletion of 32 bp (positions 92 to 123) (delLD) encompassing the putative late domain (LD) of NS3 (49), with an in-frame deletion of 315 bp (positions 139 to 453) encompassing the putative transmembrane region 1 (delTM1), or with an out-of-frame deletion of transmembrane region 2 of 145 bp (positions 454 to 598) (delTM2) (Fig. 2). All deletion variants of AHSV4LP were successfully rescued. Cells infected with these mutants tested negative by IPMAs with NS3 MAbs (Table 2). However, transient NS3-related expression for delLD was positive, and a derivative of delTM2 with wild-type start codons of NS3 and NS3a showed weak immunostaining with NS3 MAbs. Finally, mutAUG1+2 was combined with delLD, delTM1, and delTM2 (Fig. 2). This deletion in Seg-10 of 266 bp (delLD&delTM1+2) was also stably incorporated into AHSV4LP, and immunostaining with NS3 MAbs was negative for both infected monolayers and NS3-related transient expression (Table 2). We conclude that NS3/NS3a of AHSV is not essential for virus replication in vitro, but Seg-10 RNA is essential, as virus rescue without this RNA failed. Apparently, Seg-10 of delLD&delTM1+2 contains RNA sequences sufficient but essential for in vitro replication of AHSV.
FIG 2.
Overview of mutations in Seg-10 of AHSV4LP. AUG and stop codons in the ORF of NS3 are indicated by * and ×, respectively. Seg-10 RNA sequences are indicated by lines, and putatively translated NS3-related ORFs are represented by boxes. Locations of the late domain (LD) and transmembrane regions 1 and 2 (TM1 and TM2, respectively) are indicated. Deletions are indicated by dashed lines.
TABLE 2.
AHSV4LP with mutated Seg-10a
| Virus | CPE detected | IPMA result |
||
|---|---|---|---|---|
| VP2 | NS3 | NS3* | ||
| AHSV4LP | + | + | + | + |
| AHSV4LP without Seg-10 | None | ND | ND | ND |
| mutAUG1 | + | + | + | + |
| mutAUG1+2 | + | + | − | + |
| mutAUG1+2&STOPS | Small | + | − | + |
| delLD | Small | + | − | + |
| delTM1 | − | + | − | − |
| delTM2 | − | + | − | ± |
| delLD&delTM1-2 | − | + | − | − |
Rescue of virus without Seg-10 RNA was not successful (none). CPE was normal (+), reduced (small), or absent (−). NS3/NS3a expression was determined by IPMAs of infected monolayers (NS3) and of transient expression (NS3*) as positive (+), very weak (±), or negative (−). ND, not determined.
NS3/NS3a of AHSV is essential for cytopathogenic effect in mammalian cells.
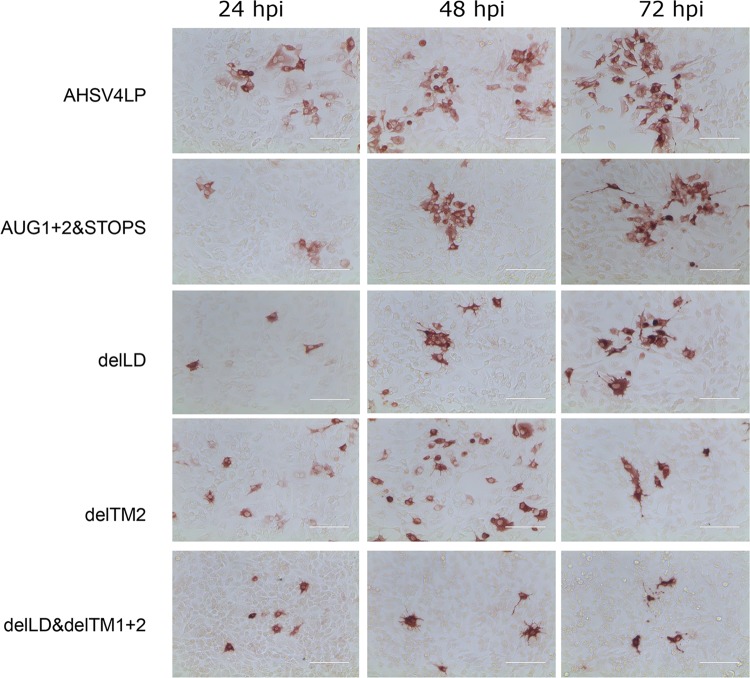
CPE of Seg-10 mutants of AHSV4LP were studied (Table 2). The mutAUG1+2 mutant formed plaques showing normal CPE, whereas mutAUG1+2&STOPS and delLD formed plaques with reduced CPE (small CPE). The delTM1, delTM2, and delLD&delTM1+2 mutants formed plaques without obvious CPE (no CPE). To semiquantitate CPE in more detail, BSR cell monolayers were infected with AHSV4LP, AUG1+2&STOPS, delLD, delTM2, and delLD&delTM1+2 at an appropriate MOI to generate foci of infected cells that were investigated by IPMAs (Fig. 3). The mutAUG1+2&STOPS and delLD mutants induced small CPE. This smaller CPE seems to be associated with a delay of CPE induction of ∼1 day. CPE of AHSV4LP at 24 hpi and 48 hpi were comparable to those of AUG1+2&STOPS and delLD at 48 hpi and 72 hpi, respectively (Fig. 3). The delTM2 and delLD&delTM1+2 mutants induced no CPE up to 72 hpi. Apparently, CPE is associated with NS3 expression and in particular with the expression of one or two transmembrane regions.
FIG 3.
Plaque morphology of Seg-10 mutants of AHSV4LP. BSR cell monolayers were infected with Seg-10 mutants of AHSV4LP and grown under overlay medium. At 24, 48, and 72 h postinfection, cells were fixed and immunostained. Separate plaques were semiquantitated as having normal CPE (AHSV4LP), small CPE, and no CPE, corresponding to +, small, and −, respectively, in Table 2.
NS3/NS3a is essential for AHSV release from Culicoides cells.
The same set of selected Seg-10 mutants of AHSV4LP (mutAUG1+2&STOPS, delLD, delTM2, and delLD&delTM1+2) was studied for virus release from mammalian (BSR) and insect (KC) cells (Fig. 4). The virus titers of AHSV mutants in culture medium (released virus) of BSR cells were ∼1.5- to 2.0-log10 TCID50/ml lower than that of AHSV4LP (Fig. 4B). This difference was observed at 24 hpi and remained similar at 48 and 72 hpi. These results suggest that virus release is delayed in the first round of infection due to the lack of NS3/NS3a expression. The virus titer of cell-associated virus was 6 to 7 log10 TCID50/ml for both AHSV4LP and mutants of AHSV4LP, which indicated that virus replication in BSR cells is not affected by Seg-10 mutations (Fig. 4A).
FIG 4.
Virus release form mammalian and insect cells. Monolayers were infected at an MOI of 0.1. Virus titers (log10 TCID50 per milliliter) in cell medium and cell fractions were determined at the indicated hours postinfection. (A) BSR cell-associated virus; (B) virus released from BSR cells; (C) KC-associated virus; (D) virus released from KC.
AHSV mutants and AHSV4LP also replicated to titers of 5 to 7 log10 TCID50/ml in KC. The titer of cell-associated AHSV4LP was slightly higher and that of delTM2 was slightly lower than those of the other tested Seg-10 mutants of AHSV4LP (Fig. 4C). In contrast to BSR cells, however, virus release from KC was hardly detected for Seg-10 mutants, whereas AHSV4LP was quickly released into the culture medium to a virus titer of 5 to 6 log10 TCID50/ml at 24 hpi (Fig. 4D). No virus release was observed for Seg-10 mutants at 48 and 72 hpi, which clearly demonstrates that NS3/NS3a expression is essential for virus release from KC.
DISA vaccine candidates for AHS.
As an example, AHSV4LP mutants with the NS3/NS3a knockout mutation AUG1+2&STOPS and Seg-2 of serotype 1 or 8 were successfully generated, resulting in AHSV1LP-(NS3/NS3amut) and AHSV8LP-(NS3/NS3amut) (Table 3). Similarly to previous experiments, Seg-2 and Seg-10 of these mutant viruses were confirmed by sequencing and IPMAs. Despite the fact that AHSV1LP grew to lower virus titers, VP2 exchange for serotype 1 in combination with an NS3/NS3a mutation was efficiently rescued. This shows the flexibility to combine VP2 exchange with NS3/N3a mutations. We conclude that the constellation of the AHSV genome can be freely composed by using reverse genetics. We suggest that the results presented here are the first steps toward the development of an AHS DISA vaccine for all serotypes.
TABLE 3.
AHSV4LP with exchanged Seg-2 and mutated Seg-10 (AHS DISA vaccine candidates)a
| Virus | Seg-2 serotype | Segment of AHSV4LP | CPE | VP2 serotype determined by IPMA | NS3 expression determined by IPMA |
|---|---|---|---|---|---|
| AHSV4LP | 4 | 1–10 | + | 4 | + |
| mutAUG1+2 | 4 | 1–9 | + | 4 | + |
| mutAUG1+2&STOPS | 4 | 1–9 | Small | 4 | − |
| AHSV1LP-(NS3/NS3a)mut | 1 | 1, 3–9 | Small | 1 | − |
| AHSV8LP-(NS3/NS3a)mut | 8 | 1, 3–9 | Small | 8 | − |
Data for the mutation mutAUG1+2&STOPS (NS3/NS3amut) in combination with Seg-2 exchange in AHSV1LP-(NS3/NS3a)mut and AHSV8LP-(NS3/NS3a)mut are shown. CPE was normal (+) or reduced (small). Expression was determined by IPMA as positive for the indicated serotype for VP2 and as positive (+) or negative (−) for NS3.
DISCUSSION
Reverse genetics for strain AHSV4LP was used to study the exchange of Seg-2 and genetic modification of Seg-10. The exchange of both outer shell proteins of several serotypes was shown for BTV6/net08 and for AHSV (31, 47). However, this was limited to certain BTV serotypes (28, 34, 50). Recently, single Seg-2[VP2] exchange was also limited for BTV (34, 41). Here we succeeded in single Seg-2 exchange for all AHSV serotypes (AHSV1LP to AHSV9LP) (Table 1). Apparently, single Seg-2 exchange for AHSV is more flexible than that for BTV.
AHSV1LP to AHSV9LP differ only in Seg-2, encoding the serotype-determining VP2 protein and the major target for NAbs (17–22, 25). Immunostaining of AHSVxLP viruses was highly specific with monospecific polyclonal anti-VP2 GP sera, which detect neutralizing as well as nonneutralizing epitopes (Table 1). In general, semiquantitative immunostaining largely but not necessarily reflects NAb titers, likely due to nonneutralizing antibodies (Abs) (47). Taken together, we assume that the single Seg-2 variants AHSV1LP to AHSV9LP will induce serotype-specific immune responses in equids.
AHSV1LP to AHSV9LP showed similar CPE, but virus titers of serotypes 1, 2, 3, and 7 were lower than those of the ancestor virus AHSV4LP and the other single Seg-2 variants at 16 hpi, which suggested that virus entry was delayed. However, reduced virus production after the first round of virus replication could be caused by many processes, e.g., infection; uncoating; transcription; translation; mRNA recruitment; and the replication, assembly, release, and stability of the virus. Thus, VP2 exchange can affect interactions with host proteins as well as interactions with viral proteins. For BTV, VP2 of serotype 2 on the BTV1 backbone also showed delayed virus growth, and a virus with single Seg-2s of several other serotypes was not viable (34, 41). Chimeric BTV VP2 was used to change the serotype of the BTV backbone of previously nonviable single VP2 reassortants of BTV (41). Possibly, chimeric AHSV VP2 could also be used to increase the virus growth of AHSVxLP variants, like those of serotypes 1 to 3 and 7.
Transcription, translation, and replication of heterologous RNA could be different from those of homologous RNA, and even the assembly or stability of the virus could be affected by the incorporation of heterologous RNA sequences. Indeed, deletions of RNA sequences and the incorporation of foreign RNA sequences appeared to be unstable in BTV, and a mutated Seg-10 with additional mutations arose rapidly in virus passages (38, 51). These studies demonstrate that RNA sequences in the remaining and interrupted open reading frame affect virus growth. Thus, heterologous Seg-2 in AHSV may also affect virus growth, irrespective of the translated VP2 protein.
Mutations of start codons and introduced stop codons did not completely abolish NS3-related translation, as shown by transient expression. It is likely that immunogenic regions of NS3/NS3a mutants are weakly expressed by artificial translation, which suggests that this expression is associated with plaque morphology. Interestingly, deletion of regions encoding putative transmembrane regions resulted in the absence of CPE (delTM1, delTM2, and delLD&delTM1+2), and NS3-related expression for these mutants was negative or extremely low (Table 2). This suggests that any NS3-related expression, in particular that of transmembrane regions, is associated with CPE.
Deletions in AHSV Seg-10 were stably incorporated into AHSV (Table 2). AHSV Seg-10 of delLD&delTM1-2 is only 266 bp long but is genetically stable. In contrast, many small deletions scattered over Seg-10 of BTV were not stable and changed during passages by additional insertions or deletions (38). It would be interesting to further enlarge deletions in NS3 of AHSV delLD&delTM1-2 to determine essential RNA sequences in Seg-10 of AHSV.
Viral RNA genomes are very compact, and their encoded proteins have been considered essential for the virus life cycle; for arthropod-borne viruses, this includes efficient virus transmission to susceptible hosts by competent insect vectors. We showed here that NS3/NS3a expression is not essential for in vitro replication of AHSV, which is in agreement with previously reported findings for the prototype midge-borne orbivirus BTV (36, 38). In further agreement with the data for BTV, CPE caused by AHSV in mammalian cells and virus release from cultured insect cells are dependent on NS3/NS3a expression (Fig. 3) (36). NS3/NS3a of AHSV has been associated with virulence and viremia (52, 53), and virulent BTV8 without NS3/NS3a is not virulent and strongly reduced in viremia (37). Based on these in vitro similarities, we hypothesize that virulent AHSV lacking NS3/NS3a is not virulent in equids.
The virulent isolate AHSV HS 32/62 has been attenuated by passages and selected by large-plaque morphology, resulting in LAV strain AHSV4LP (2). The safety of replicating vaccines such as these traditional LAVs is controversial, particularly when used as multivalent vaccine—cocktails of different LAVs—due to the risk of reversion to virulence by reassortment. However, monovalent AHSV4LP was successfully and safely used to control AHS on the Iberian Peninsula in the late 1980s, without reports of adverse effects or “reversion to virulence.” It is likely that synthetic AHSV4LP is indistinguishable from this ancestor virus in horses, as has been shown for synthetic viruses derived from many virus families by reverse genetics, including virulent BTV8 and avirulent BTV6 (29).
The flexibility to change the serotype of AHSV4LP by the exchange of Seg-2[VP2] was demonstrated (AHSV1LP to AHSV9LP). Live-attenuated BTV6/net08 with VP2 and VP5 of virulent BTV8/net06 is not virulent (31), although VP2 of BTV is involved in virulence (54). Similarly, AHSVxLPs will be attenuated like AHSV4LP, although virulence markers on Seg-2 have also been suggested (44, 55). Furthermore, AHSV without NS3/NS3a expression shows in vitro characteristics (Fig. 3 and 4) similar to those of BTV without NS3/NS3a proteins (36). Previously, we demonstrated that virulent BTV8/net06 without NS3/NS3a is not virulent (37). Finally, live-attenuated BTV6/net08 without NS3/NS3a, named bluetongue disabled infectious single animal (BT DISA) vaccine, harboring heterologous VP2 protects sheep against the respective virulent BTV serotypes, and NAbs are highly serotype specific (37, 40, 41).
Thus, live-attenuated AHSV4LP without NS3/NS3a might be a suitable AHS DISA platform to develop vaccine candidates for different serotypes. As an example, Seg-2 of serotype 1 or 8 was incorporated into AHSV4LP with the mutAUG1+2&STOPS mutation (Table 3). AHS DISA vaccines will also enable serological DIVA (differentiating infected from vaccinated animals) by accompanying tests detecting AHSV NS3-directed antibodies (56). Development of AHS DISA vaccine candidates with DIVA potential, preferably by deletion of Seg-10 sequences associated with stability, for all nine serotypes is in progress. These AHS DISA vaccine candidates will share nine segments and differ only in Seg-2. Consequently, virulent variants of AHS DISA vaccines cannot arise by reassortment, and cocktails of proposed AHS DISA vaccines are as safe as monovalent AHS DISA vaccines.
In summary, we demonstrated the exchange of single Seg-2[VP2] of all AHSV serotypes. Furthermore, we showed that NS3/NS3a proteins are not essential for AHSV replication in vitro. NS3/NS3a knockout mutants of AHSV exhibit in vitro characteristics similar to those of NS3/NS3a knockout mutants of BTV. We therefore propose that the NS3/NS3a knockout mutant of live-attenuated AHSV will harbor properties in horses similar to those of the BT DISA vaccine in ruminants. By using this AHS DISA platform, vaccines for all AHSV serotypes will be feasible by single Seg-2[VP2] exchange. Promising vaccine candidates will be extensively investigated in vitro before vaccination/challenge experiments in horses are planned.
ACKNOWLEDGMENTS
We thank Carmen Vela and Paloma Rueda (Ingenasa, Spain) for MAbs directed against VP2, VP5, and NS3 of AHSV4. Guinea pig sera against baculovirus-expressed VP2 proteins of different AHSV serotypes were generated in collaboration with the European Union-funded project OrbiVac KBBE-245266 (CVI project 1630017000), coordinated by Polly Roy (London School of Hygienic and Tropical Medicine, United Kingdom). This research was funded by the Dutch Ministry of Economic Affairs (CVI project 1630022900).
We greatly appreciate the stimulating discussions with Baltus Erasmus and the technical assistance of Mieke Maris-Veldhuis and Femke Feenstra.
REFERENCES
- 1.Theiler A. 1921. African horse sickness. Science bulletin 19, p 1–32. Department of Agriculture, Union of South Africa. [Google Scholar]
- 2.Erasmus BJ. 1972. The pathogenesis of African horse sickness, p 1–11. In Proceedings of the 3rd International Conference on Equine Infectious Diseases Karger, Basel, Switzerland. [Google Scholar]
- 3.Mellor PS, Hamblin C. 2004. African horse sickness. Vet Res 35:445–466. doi: 10.1051/vetres:2004021. [DOI] [PubMed] [Google Scholar]
- 4.Diouf ND, Etter E, Lo MM, Lo M, Akakpo AJ. 2013. Outbreaks of African horse sickness in Senegal, and methods of control of the 2007 epidemic. Vet Rec 172:152. doi: 10.1136/vr.101083. [DOI] [PubMed] [Google Scholar]
- 5.Du Toit RA. 1944. The transmission of blue-tongue and horse sickness by Culicoides. Onderstepoort J Vet Sci Anim Ind 19:7–16. [Google Scholar]
- 6.Venter GJ, Graham SD, Hamblin C. 2000. African horse sickness epidemiology: vector competence of South African Culicoides species for virus serotypes 3, 5 and 8. Med Vet Entomol 14:245–250. doi: 10.1046/j.1365-2915.2000.00245.x. [DOI] [PubMed] [Google Scholar]
- 7.Venter GJ, Paweska JT. 2007. Virus recovery rates for wild-type and live-attenuated vaccine strains of African horse sickness virus serotype 7 in orally infected South African Culicoides species. Med Vet Entomol 21:377–383. doi: 10.1111/j.1365-2915.2007.00706.x. [DOI] [PubMed] [Google Scholar]
- 8.Purse BV, Mellor PS, Rogers DJ, Samuel AR, Mertens PP, Baylis M. 2005. Climate change and the recent emergence of bluetongue in Europe. Nat Rev Microbiol 3:171–181. doi: 10.1038/nrmicro1090. [DOI] [PubMed] [Google Scholar]
- 9.Gale P, Brouwer A, Ramnial V, Kelly L, Kosmider R, Fooks AR, Snary EL. 2010. Assessing the impact of climate change on vector-borne viruses in the EU through the elicitation of expert opinion. Epidemiol Infect 138:214–225. doi: 10.1017/S0950268809990367. [DOI] [PubMed] [Google Scholar]
- 10.Meiswinkel R, van Rijn P, Leijs P, Goffredo M. 2007. Potential new Culicoides vector of bluetongue virus in northern Europe. Vet Rec 161:564–565. doi: 10.1136/vr.161.16.564. [DOI] [PubMed] [Google Scholar]
- 11.Mehlhorn H, Walldorf V, Klimpel S, Jahn B, Jaeger F, Eschweiler J, Hoffmann B, Beer M. 2007. First occurrence of Culicoides obsoletus-transmitted bluetongue virus epidemic in Central Europe. Parasitol Res 101:219–228. doi: 10.1007/s00436-007-0519-6. [DOI] [PubMed] [Google Scholar]
- 12.Dijkstra E, van der Ven IJ, Meiswinkel R, Holzel DR, Van Rijn PA, Meiswinkel R. 2008. Culicoides chiopterus as a potential vector of bluetongue virus in Europe. Vet Rec 162:422. doi: 10.1136/vr.162.13.422-a. [DOI] [PubMed] [Google Scholar]
- 13.Backer JA, Nodelijk G. 2011. Transmission and control of African horse sickness in The Netherlands: a model analysis. PLoS One 6:e23066. doi: 10.1371/journal.pone.0023066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodriguez M, Hooghuis H, Castano M. 1992. African horse sickness in Spain. Vet Microbiol 33:129–142. doi: 10.1016/0378-1135(92)90041-Q. [DOI] [PubMed] [Google Scholar]
- 15.Capela R, Purse BV, Pena I, Wittman EJ, Margarita Y, Capela M, Romao L, Mellor PS, Baylis M. 2003. Spatial distribution of Culicoides species in Portugal in relation to the transmission of African horse sickness and bluetongue viruses. Med Vet Entomol 17:165–177. doi: 10.1046/j.1365-2915.2003.00419.x. [DOI] [PubMed] [Google Scholar]
- 16.House JA, Lombard M, Dubourget P, House C, Mebus CA. 1994. Further studies on the efficacy of an inactivated African horse sickness serotype 4 vaccine. Vaccine 12:142–144. doi: 10.1016/0264-410X(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 17.Roy P, Bishop DH, Howard S, Aitchison H, Erasmus B. 1996. Recombinant baculovirus-synthesized African horsesickness virus (AHSV) outer-capsid protein VP2 provides protection against virulent AHSV challenge. J Gen Virol 77(Part 9):2053–2057. [DOI] [PubMed] [Google Scholar]
- 18.Scanlen M, Paweska JT, Verschoor JA, van Dijk AA. 2002. The protective efficacy of a recombinant VP2-based African horsesickness subunit vaccine candidate is determined by adjuvant. Vaccine 20:1079–1088. doi: 10.1016/S0264-410X(01)00445-5. [DOI] [PubMed] [Google Scholar]
- 19.Castillo-Olivares J, Calvo-Pinilla E, Casanova I, Bachanek-Bankowska K, Chiam R, Maan S, Nieto JM, Ortego J, Mertens PP. 2011. A modified vaccinia Ankara virus (MVA) vaccine expressing African horse sickness virus (AHSV) VP2 protects against AHSV challenge in an IFNAR-/- mouse model. PLoS One 6:e16503. doi: 10.1371/journal.pone.0016503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El Garch H, Crafford JE, Amouyal P, Durand PY, Edlund Toulemonde C, Lemaitre L, Cozette V, Guthrie A, Minke JM. 2012. An African horse sickness virus serotype 4 recombinant canarypox virus vaccine elicits specific cell-mediated immune responses in horses. Vet Immunol Immunopathol 149:76–85. doi: 10.1016/j.vetimm.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 21.Calvo-Pinilla E, de la Poza F, Gubbins S, Mertens PP, Ortego J, Castillo-Olivares J. 2014. Vaccination of mice with a modified vaccinia Ankara (MVA) virus expressing the African horse sickness virus (AHSV) capsid protein VP2 induces virus neutralising antibodies that confer protection against AHSV upon passive immunisation. Virus Res 180:23–30. doi: 10.1016/j.virusres.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Alberca B, Bachanek-Bankowska K, Cabana M, Calvo-Pinilla E, Viaplana E, Frost L, Gubbins S, Urniza A, Mertens P, Castillo-Olivares J. 2014. Vaccination of horses with a recombinant modified vaccinia Ankara virus (MVA) expressing African horse sickness (AHS) virus major capsid protein VP2 provides complete clinical protection against challenge. Vaccine 32:3670–3674. doi: 10.1016/j.vaccine.2014.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mertens PPC, Maan S, Samuel A, Attoui H. 2005. Orbiviruses, Reoviridae, p 466–483. In Fauquet CM, Mayo MA, Maniloff J, Desselberger U, Ball LA (ed), Virus taxonomy. Eighth report of the International Committee on Taxonomy of Viruses. Elsevier Academic Press, San Diego, CA. [Google Scholar]
- 24.Huismans H, Erasmus BJ. 1981. Identification of the serotype-specific and group-specific antigens of bluetongue virus. Onderstepoort J Vet Res 48:51–58. [PubMed] [Google Scholar]
- 25.Huismans H, van der Walt NT, Erasmus BJ. 1985. Immune response against the purified serotype specific antigen of bluetongue virus and initial attempts to clone the gene that codes for the synthesis of this protein. Prog Clin Biol Res 178:347–353. [PubMed] [Google Scholar]
- 26.Huismans H, van der Walt NT, Cloete M, Erasmus BJ. 1987. Isolation of a capsid protein of bluetongue virus that induces a protective immune response in sheep. Virology 157:172–179. doi: 10.1016/0042-6822(87)90326-6. [DOI] [PubMed] [Google Scholar]
- 27.Kaname Y, Celma CC, Kanai Y, Roy P. 2013. Recovery of African horse sickness virus from synthetic RNA. J Gen Virol 94:2259–2265. doi: 10.1099/vir.0.055905-0. [DOI] [PubMed] [Google Scholar]
- 28.Boyce M, Celma CC, Roy P. 2008. Development of reverse genetics systems for bluetongue virus: recovery of infectious virus from synthetic RNA transcripts. J Virol 82:8339–8348. doi: 10.1128/JVI.00808-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Gennip RG, van de Water SG, Potgieter CA, Wright IM, Veldman D, van Rijn PA. 2012. Rescue of recent virulent and avirulent field strains of bluetongue virus by reverse genetics. PLoS One 7:e30540. doi: 10.1371/journal.pone.0030540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Celma CC, Roy P. 2009. A viral nonstructural protein regulates bluetongue virus trafficking and release. J Virol 83:6806–6816. doi: 10.1128/JVI.00263-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Gennip RG, van de Water SG, Maris-Veldhuis M, van Rijn PA. 2012. Bluetongue viruses based on modified-live vaccine serotype 6 with exchanged outer shell proteins confer full protection in sheep against virulent BTV8. PLoS One 7:e44619. doi: 10.1371/journal.pone.0044619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shaw AE, Ratinier M, Nunes SF, Nomikou K, Caporale M, Golder M, Allan K, Hamers C, Hudelet P, Zientara S, Breard E, Mertens P, Palmarini M. 2013. Reassortment between two serologically unrelated bluetongue virus strains is flexible and can involve any genome segment. J Virol 87:543–557. doi: 10.1128/JVI.02266-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coetzee P, Van Vuuren M, Stokstad M, Myrmel M, van Gennip RG, van Rijn PA, Venter EH. 2014. Viral replication kinetics and in vitro cytopathogenicity of parental and reassortant strains of bluetongue virus serotype 1, 6 and 8. Vet Microbiol 171:53–65. doi: 10.1016/j.vetmic.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Nunes SF, Hamers C, Ratinier M, Shaw A, Brunet S, Hudelet P, Palmarini M. 2014. A synthetic biology approach for a vaccine platform against known and newly emerging serotypes of bluetongue virus. J Virol 88:12222–12232. doi: 10.1128/JVI.02183-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ratinier M, Caporale M, Golder M, Franzoni G, Allan K, Nunes SF, Armezzani A, Bayoumy A, Rixon F, Shaw A, Palmarini M. 2011. Identification and characterization of a novel non-structural protein of bluetongue virus. PLoS Pathog 7:e1002477. doi: 10.1371/journal.ppat.1002477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Gennip RG, van de Water SG, van Rijn PA. 2014. Bluetongue virus nonstructural protein NS3/NS3a is not essential for virus replication. PLoS One 9:e85788. doi: 10.1371/journal.pone.0085788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feenstra F, van Gennip RG, Maris-Veldhuis M, Verheij E, van Rijn PA. 2014. Bluetongue virus without NS3/NS3a expression is not virulent and protects against virulent bluetongue virus challenge. J Gen Virol 95:2019–2029. doi: 10.1099/vir.0.065615-0. [DOI] [PubMed] [Google Scholar]
- 38.Feenstra F, van Gennip RG, van de Water SG, van Rijn PA. 2014. RNA elements in open reading frames of the bluetongue virus genome are essential for virus replication. PLoS One 9:e92377. doi: 10.1371/journal.pone.0092377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Rijn PA, van de Water SG, van Gennip HG. 2013. Bluetongue virus with mutated genome segment 10 to differentiate infected from vaccinated animals: a genetic DIVA approach. Vaccine 31:5005–5008. doi: 10.1016/j.vaccine.2013.08.089. [DOI] [PubMed] [Google Scholar]
- 40.Feenstra F, Maris-Veldhuis M, Daus FJ, Tacken MG, Moormann RJ, van Gennip RG, van Rijn PA. 2014. VP2-serotyped live-attenuated bluetongue virus without NS3/NS3a expression provides serotype-specific protection and enables DIVA. Vaccine 32:7108–7114. doi: 10.1016/j.vaccine.2014.10.033. [DOI] [PubMed] [Google Scholar]
- 41.Feenstra F, Pap JS, van Rijn PA. 2015. Application of bluetongue disabled infectious single animal (DISA) vaccine for different serotypes by VP2 exchange or incorporation of chimeric VP2. Vaccine 33:812–818. doi: 10.1016/j.vaccine.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 42.Sato M, Tanaka H, Yamada T, Yamamoto N. 1977. Persistent infection of BHK21/WI-2 cells with rubella virus and characterization of rubella variants. Arch Virol 54:333–343. doi: 10.1007/BF01314778. [DOI] [PubMed] [Google Scholar]
- 43.Wechsler SJ, McHolland LE, Tabachnick WJ. 1989. Cell lines from Culicoides variipennis (Diptera: Ceratopogonidae) support replication of bluetongue virus. J Invertebr Pathol 54:385–393. doi: 10.1016/0022-2011(89)90123-7. [DOI] [PubMed] [Google Scholar]
- 44.Potgieter AC, Page NA, Liebenberg J, Wright IM, Landt O, van Dijk AA. 2009. Improved strategies for sequence-independent amplification and sequencing of viral double-stranded RNA genomes. J Gen Virol 90:1423–1432. doi: 10.1099/vir.0.009381-0. [DOI] [PubMed] [Google Scholar]
- 45.van Rijn PA, Miedema GK, Wensvoort G, van Gennip HG, Moormann RJ. 1994. Antigenic structure of envelope glycoprotein E1 of hog cholera virus. J Virol 68:3934–3942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wensvoort G, Terpstra C, Bloemraad M. 1988. Detection of antibodies against African swine fever virus using infected monolayers and monoclonal antibodies. Vet Rec 122:536–539. doi: 10.1136/vr.122.22.536. [DOI] [PubMed] [Google Scholar]
- 47.Kanai Y, van Rijn PA, Maris-Veldhuis M, Kaname Y, Athmaram TN, Roy P. 2014. Immunogenicity of recombinant VP2 proteins of all nine serotypes of African horse sickness virus. Vaccine 32:4932–4937. doi: 10.1016/j.vaccine.2014.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Britton P, Green P, Kottier S, Mawditt KL, Penzes Z, Cavanagh D, Skinner MA. 1996. Expression of bacteriophage T7 RNA polymerase in avian and mammalian cells by a recombinant fowlpox virus. J Gen Virol 77(Part 5):963–967. [DOI] [PubMed] [Google Scholar]
- 49.Wirblich C, Bhattacharya B, Roy P. 2006. Nonstructural protein 3 of bluetongue virus assists virus release by recruiting ESCRT-I protein Tsg101. J Virol 80:460–473. doi: 10.1128/JVI.80.1.460-473.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Celma CC, Boyce M, van Rijn PA, Eschbaumer M, Wernike K, Hoffmann B, Beer M, Haegeman A, De Clercq K, Roy P. 2013. Rapid generation of replication-deficient monovalent and multivalent vaccines for bluetongue virus: protection against virulent virus challenge in cattle and sheep. J Virol 87:9856–9864. doi: 10.1128/JVI.01514-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shaw AE, Veronesi E, Maurin G, Ftaich N, Guiguen F, Rixon F, Ratinier M, Mertens P, Carpenter S, Palmarini M, Terzian C, Arnaud F. 2012. Drosophila melanogaster as a model organism for bluetongue virus replication and tropism. J Virol 86:9015–9024. doi: 10.1128/JVI.00131-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.van Niekerk M, Smit CC, Fick WC, van Staden V, Huismans H. 2001. Membrane association of African horsesickness virus nonstructural protein NS3 determines its cytotoxicity. Virology 279:499–508. doi: 10.1006/viro.2000.0709. [DOI] [PubMed] [Google Scholar]
- 53.van Niekerk M, van Staden V, van Dijk AA, Huismans H. 2001. Variation of African horsesickness virus nonstructural protein NS3 in southern Africa. J Gen Virol 82:149–158. [DOI] [PubMed] [Google Scholar]
- 54.Janowicz A, Caporale M, Shaw A, Gulletta S, Di Gialleonardo L, Ratinier M, Palmarini M. 2015. Multiple genome segments determine virulence of bluetongue virus serotype 8. J Virol 89:5238–5249. doi: 10.1128/JVI.00395-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Manole V, Laurinmaki P, Van Wyngaardt W, Potgieter CA, Wright IM, Venter GJ, van Dijk AA, Sewell BT, Butcher SJ. 2012. Structural insight into African horsesickness virus infection. J Virol 86:7858–7866. doi: 10.1128/JVI.00517-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Laviada MD, Roy P, Sanchez-Vizcaino JM, Casal JI. 1995. The use of African horse sickness virus NS3 protein, expressed in bacteria, as a marker to differentiate infected from vaccinated horses. Virus Res 38:205–218. doi: 10.1016/0168-1702(95)00061-T. [DOI] [PubMed] [Google Scholar]