Abstract
Intracranial aspergilloma is extremely rare. The diagnosis and treatment of invasive CNS aspergillosis is very difficult. Early diagnosis is important for a successful treatment. Here, we report a case of intracranial aspergilloma in an 11-year-old boy in 2013. Good outcome was achieved by treatment with a combination of neurosurgical resection and antifungal administration, which we suggest is a good quality management plan.
Keywords: Aspergillus, Immunocompetent patient, Central nervous system
Introduction
Aspergillus is a fungus with a worldwide distribution; the most common types include flavus and fumigatus (1–3). Intracranial fungal infection caused by Aspergillus comes from India, Pakistan, Sudan and Saudi Arabia. In a few cases they are reported to come from turkey and the United States (3–5). The most common primary sites of Aspergillus are paranasal sinuses (6, 7). In these cases the inhalation of Aspergillus spores causes pulmonary infection. It infects the CNS through release into the blood and in cases of involvement of the paranasal sinuses; they invade the CNS due to physical proximity (5, 8). CNS involvement can be seen in immunocompromised patients such as patients with AIDS and patients receiving organ transplants (1, 4, 6, 9–11). However, CNS involvement is rare in immunocompetent people. They are not detected due to similarity of the tumor to the surrounding lesions. It causes death, despite progress made in the diagnosis and treatment of brain abscess (6, 12–14). After lungs, CNS is the second most common site of involvement which leads to death in more than 90% of the cases (2, 6, 13, 15). It rarely involves intraparenchymal, frontal, and temporal lobes. It develops clinical signs consistent with its location of involvement (5). Symptoms include headaches usually neurological defects and seizures (2, 4, 7, 16). CNS aspergillosis usually has a poor prognosis; although, surgery have cured the patient temporarily, especially when it is associated with antifungal treatments (8).
Once approved by the FDA, voriconazole has been the standard treatment of brain aspergillosis. A combination of antifungal therapy and neuro-surgery should be done for the patients (4, 6, 15). This is one of the first cases of CNS Aspergilloma in Iran (17).
Case report
The case was an 11-year-old boy who was admitted to the Department of Neurosurgery, Imam Hossein Hospital, 2013 with the weakness of the left limbs after a generalized seizure. The patient was alert in the initial evaluation. There was no history of illness, hospitalization or special drugs and he was fully conscious (GCS 15/15) with the following vital signs: BP: 110/80, PR: 90, RR: 15, T: 37.2.
In the physical examination the patient had weakness (3/5) of the left limb but other examinations showed normal results. Brain non contrast CT scan showed a hyperdense lesion in the right frontal lobe.
MRI revealed a 30 × 21 mm mass in the right frontal lobe resulting in hyposignal on T1 and iso-signal on T2/Flair, hypersignal and extensive surrounding edema and ring enhancement around the lesion (Fig.1).In the initial evaluation there was a suspected metastatic lesions and infection. Abdominal and pelvic CT was normal. CT scan showed multiple lung nodules with irregular, spiculated margins within the parenchyma of the right lung which was evident for metastatic or infectious lesions. Later the brain mass was removed by surgery. It was a gray circular mass in cortex with a diameter of 3 cm. There was little bleeding during surgery and the mass was stiff with a few arteries which were removed completely. After rehabilitation patient’s force was 5/5. Pathologic assessment showed granulation lesions, giant cells, and areas of necrosis, fragmentation of hyphae within the lesion and cytoplasm of macrophages.
Fig. 1:
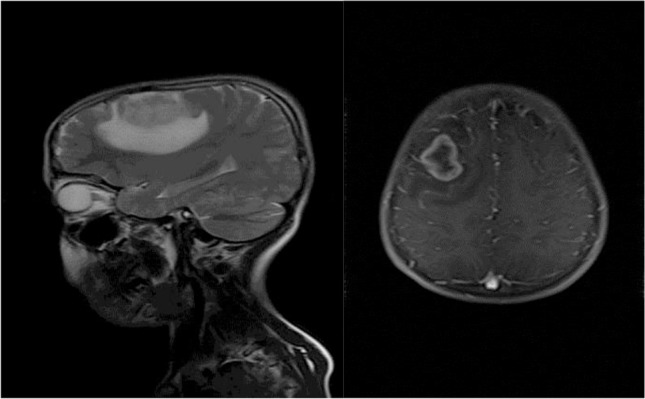
Brain T2 and T1 with contrast MRI showing a lesion in the right frontal lobe
There was no trace of cancer. Aspergillus antigen test (galactomannan and IgG) was negative and culture of the Brain lesion and pulmonary secretions confirmed the presence of A. flavus. There was no trace of immunocompromised condition as well: WBC 12000 /μl, CH50: 97, C3–C4: NL. HIV 1and 2 negative, HBCAb negative, HBS Ag negative, IgE, IgA, IgG, IgM normal, Hb.14.
The patient was treated with voriconazole (6 mg per kg intravenously twice a day on day 1, followed by 4 mg per kilogram intravenously twice daily), prednisolone, and beta interferon for 3 months. Then lesions were resolved with continued treatment. After one year, patient had weakness (3/5) of the left limb. A 3cm lesion was observed in the previous location. The patient went under repeated surgery and the lesion was removed. Histological tests and culture of the Brain lesion confirmed the presence of A. flavus. The hyphae appearance with branches of 45 degrees is a typical and specific finding for Aspergillus infection. After another rehabilitation session patients force was 5/5 and there were no signs of recurrence in a follow-up study one year later (Fig. 2). According to the Ethical issues, a written informed consent was obtained from patient's parents for publishing current paper.
Fig. 2:
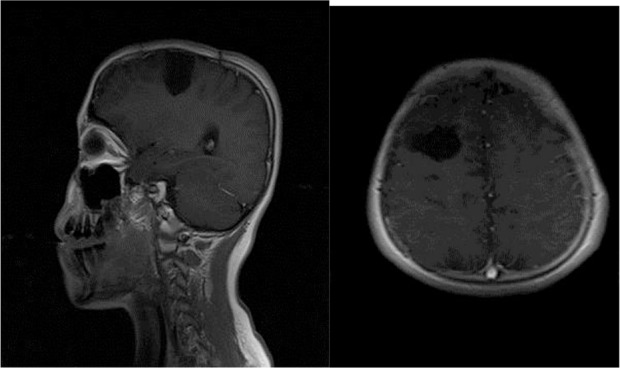
One year postoperative Brain T1 with contrast MRI showing a lesion location in the right frontal lobe
Discussion
In immunocompetent patients, cerebral aspergillosis is rare but has a high mortality rate (18). Voriconazole advantages outweigh its disadvantages. It has a better penetration rate into CSF compared to Amphotericin (1). The most common site of aspergilloma is the frontal area which is consistent with our study and after that the most common locations is parasellar region. In immunocompetent patients aspergiloma form as granuloma formation secondary to immune response which matches the result of our study. In our case the lesion was like tuberculoma. The diagnosis of the presence of aspergiloma in the lungs was confirmed too. This could be the source of a CNS infection and the most frequent place of colonization of aspergillosis (12). In our case, Galactomannan antigen was negative but this negative result does not reject the presence of aspergilloma (16).
Our case is an example of the rare presentation of fungal infection. Hence, we conclude that pre-operative diagnosis of cerebral fungal lesion is difficult and is frequently missed. Proper clinical, radiological and hematological evaluation with direct histopathological examination and culture are the ultimate requirement for final diagnosis of the aspergilloma. In these patients high index of suspicion, aggressive approach of diagnosis with timely and vigorous neurosurgical treatment and antifungal treatment is indicated for proper removal of the infection.
Our case suggests that aspergilloma should be included in the differential diagnosis of patients with CNS lesions. Therefore, rapid diagnosis and efficient medical and surgical intervention are required to preserve neurologic function.
Acknowledgments
The authors have declared that no conflict of interest exists.
References
- 1. Bokhari R, Baeesa S, Al-Maghrabi J, Madani T. (2014). Isolated Cerebral Aspergillosis in Immunocompetent Patients. World Neurosurgery, 82( 1): e325–e33. [DOI] [PubMed] [Google Scholar]
- 2. Alapatt JP, Kutty RK, Gopi PP, Challissery J. (2006). Middle and posterior fossa aspergilloma. Surgical Neurology, 66( 1): 75–8. [DOI] [PubMed] [Google Scholar]
- 3. Koshy R, Malhotra P. (2011). Treatment of primary aspergilloma of the central nervous system in a diabetic immunocompetent patient with surgical resection and voriconazole: a case report and review of the literature. Turkish Neurosurgery, 21 ( 4): 641–4. [PubMed] [Google Scholar]
- 4. Hoenigl M, Krause R. (2013). Antifungal therapy of aspergillosis of the central nervous system and Aspergillus endophthalmitis. Current Pharmaceutical Design, 19( 20): 3648–68. [DOI] [PubMed] [Google Scholar]
- 5. Sundaram C, Murthy JM. (2011). Intracranial Aspergillus granuloma. Patholog Res Int, 2011: 157320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kourkoumpetis TK, Desalermos A, Muhammed M, Mylonakis E. (2012). Central nervous system aspergillosis: a series of 14 cases from a general hospital and review of 123 cases from the literature. Medicine, 91( 6): 328–36. [DOI] [PubMed] [Google Scholar]
- 7. Bai J, Cheng J-l, Zhang Y, Xue K-k. (2015). Neuroimaging features of cerebral aspergillus abscess: Case report. Radiol Infect Dis, In Press. [Google Scholar]
- 8. Partridge BM, Chin AT. (1981). Cerebral aspergilloma. Postgraduate Med J, 57( 669): 439–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Muzumdar D. (2011). Central nervous system infections and the neurosurgeon: A perspective. Int J Surger, 9( 2): 113–6. [DOI] [PubMed] [Google Scholar]
- 10. Shamim MS, Enam SA, Ali RP, Ali SF, Wasay M. (2009). Overview of surgical management of infectious non-suppurative brain lesions. Pak J Neurol Sci, 4(2): 77. [Google Scholar]
- 11. Mardari R, Della Puppa A, Rotilio A, Sgarabotto D, Baracchini C, Carollo C, Manara R. (2011). Pontocerebellar angle aspergillosis: clinical and radiological findings. The Neurologist, 17( 2): 75–8. [DOI] [PubMed] [Google Scholar]
- 12. Nadkarni T, Goel A. (2005). Aspergilloma of the brain: an overview. J Postgraduate Med, 51( 5): 37. [PubMed] [Google Scholar]
- 13. Lee J-C, Lim D-J, Ha S-K, Kim S-D, Kim S-H. (2012). Fatal case of cerebral aspergillosis: a case report and literature review. J Korean Neurosur Soc, 52( 4): 420–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Srinivasan U. (2008). Intracranial aspergilloma in immunocompetent patients successfully treated with radical surgical intervention and antifungal therapy: case series. Annals of the Academy of Medicine, Singapore, 37( 9): 783–7. [PubMed] [Google Scholar]
- 15. Chen S, Pu J-L, Yu J, Zhang J-M. (2011). Multiple Aspergillus cerebellar abscesses in a middle-aged female: case report and literature review. Int J Med Sci, 8( 7): 635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Spapen H, Spapen J, Taccone FS, Meersseman W, Rello J, Dimopoulos G, Charles P-E, Rao R, Pérez M, Martin C. (2014). Cerebral aspergillosis in adult critically ill patients: a descriptive report of 10 patients from the AspICU cohort. Int J Antimicrob Agents. 43( 2): 165–9. [DOI] [PubMed] [Google Scholar]
- 17. Azarpira N, Esfandiari M, Bagheri MH, Rakei S, Salari S. (2008). Cerebral aspergillosis presenting as a mass lesion. Brazilian J Infect Dis, 12( 4): 349–51. [DOI] [PubMed] [Google Scholar]
- 18. Garcia RJ, Troya P, Edwards C. (2006). Invasive aspergillosis with central nervous system dissemination in a presumably immunocompetent, non-neutropenic patient: case report and review. Southern Med J, 99( 6): 607–10. [DOI] [PubMed] [Google Scholar]


