Abstract
BACKGROUND:
The determination of competency of trainees in programs performing bronchoscopy is quite variable. Some programs provide didactic lectures with hands-on supervision, other programs incorporate advanced simulation centers, whereas others have a checklist approach. Although no single method has been proven best, the variability alone suggests that outcomes are variable. Program directors and certifying bodies need guidance to create standards for training programs. Little well-developed literature on the topic exists.
METHODS:
To provide credible and trustworthy guidance, rigorous methodology has been applied to create this bronchoscopy consensus training statement. All panelists were vetted and approved by the CHEST Guidelines Oversight Committee. Each topic group drafted questions in a PICO (population, intervention, comparator, outcome) format. MEDLINE data through PubMed and the Cochrane Library were systematically searched. Manual searches also supplemented the searches. All gathered references were screened for consideration based on inclusion criteria, and all statements were designated as an Ungraded Consensus-Based Statement.
RESULTS:
We suggest that professional societies move from a volume-based certification system to skill acquisition and knowledge-based competency assessment for trainees. Bronchoscopy training programs should incorporate multiple tools, including simulation. We suggest that ongoing quality and process improvement systems be introduced and that certifying agencies move from a volume-based certification system to skill acquisition and knowledge-based competency assessment for trainees. We also suggest that assessment of skill maintenance and improvement in practice be evaluated regularly with ongoing quality and process improvement systems after initial skill acquisition.
CONCLUSIONS:
The current methods used for bronchoscopy competency in training programs are variable. We suggest that professional societies and certifying agencies move from a volume- based certification system to a standardized skill acquisition and knowledge-based competency assessment for pulmonary and thoracic surgery trainees.
Summary of Suggestions
1. We suggest that professional societies and certifying agencies move from a volume-based certification system to skill acquisition and knowledge-based competency assessment for pulmonary trainees (Ungraded Consensus-Based Statement).
2. We suggest that assessment of skill maintenance and improvement in practice be evaluated regularly in similar fashion as recurrent cognitive examinations (Ungraded Consensus-Based Statement).
3. We suggest that ongoing quality and process improvement systems after initial skill acquisition be introduced (Ungraded Consensus-Based Statement).
4. We suggest that bronchoscopy training programs incorporate multiple tools, such as e-learning, lectures, books, case-based reviews, and hands-on training (Ungraded Consensus-Based Statement).
5. We suggest that in countries with comparable levels of medical care, bronchoscopy training program requirements be standardized (Ungraded Consensus-Based Statement).
6. We suggest that professional societies and certifying agencies that oversee training programs for similar procedures in different medical and surgical specialties standardize requirements where applicable (Ungraded Consensus-Based Statement).
7. We suggest that simulation specifically be integrated into a structured bronchoscopy teaching curriculum (Ungraded Consensus-Based Statement).
8. We suggest that high-fidelity simulation due to its cost should be offered in regional simulation centers, which should be accessible to all training programs (Ungraded Consensus-Based Statement).
Procedural training has long been an important component in the specialty of pulmonary and critical care medicine. Airway stabilization, advanced intravascular access procedures, and many other techniques are a mainstay of modern critical care. In addition, bronchoscopy-based procedures have traditionally been a defining skill for the practicing pulmonologist.
Over the last decade, technology has advanced greatly, especially in pulmonary procedural practice. These advances include endobronchial ultrasound (EBUS), pleuroscopy, bronchial thermoplasty, and many others. With this expanse, the question of how proper training in these new areas as well as in established procedures should be conducted so that physicians are taught to the highest standards and patients can rely on the highest competency of their treating health-care provider.
The American College of Chest Physicians (CHEST) convened a diverse group of individuals with content knowledge in procedural medicine, as well as in teaching, and training, who represent different specialty stakeholders and health-care systems. The group was tasked to assess the current state of training and, based on the findings, to issue statements on how new bronchoscopy training content and guidelines should be structured going forward.
Materials and Methods
The determination of competency of trainees in pulmonary and critical care medicine in performing bronchoscopic procedures varies from program to program. Program directors and certifying bodies need guidance to create standards for training programs. Little well-developed literature on the topic exists. To provide credible and trustworthy guidance in this document, rigorous methodology has been applied to the consensus statement development process.
Composition and Selection of Panelists
The chair of the panel was approved by the CHEST Guidelines Oversight Committee (GOC) and disclosed no significant or potential conflicts of interest (COIs). Nine other content experts served on the panel. These panelists were divided among four topic groups as content specialists for their particular area of expertise. A methodologist (J. O.) was also assigned to the panel by the GOC. All panelists were vetted and approved by the GOC after review of their COI disclosures. During the course of this project, all panelists were required to report any new activities that might involve potential COIs for review and approval by the GOC.
Identifying and Reviewing the Evidence
Key Questions and Systematic Search:
Each topic group drafted key questions (KQs) in a PICO (population, intervention, comparator, outcome) format (Table 1). The methodologist performed a systematic search of individual studies for each KQ using the National Library of Medicine’s Medical Subject Headings key word nomenclature and other key words derived from the KQ. Because little evidence was anticipated, a more inclusive, broad-based approach to the search was used that did not limit by population characteristics, study design, or publication date. The two databases systematically searched for individual studies in December 2013 were MEDLINE through PubMed and the Cochrane Library. Manual searches also supplemented the electronic searches. All gathered references were imported into an electronic database (EndNote X6; Thomson Reuters).
TABLE 1 ] .
Structured Clinical Key Questions
| Key Question | Population | Intervention | Comparators | Outcome |
| Key question 1: Among bronchoscopy trainees, is competency-based education more effective than other educational methods for superior bronchoscopy performance? | Trainees, fellows, residents, students | Competency assessment of bronchoscopy training | Other educational methods | Bronchoscopy performance |
| Key question 2: Among bronchoscopy trainees, is training and evaluation outside the USA more effective than inside the USA for superior bronchoscopy performance? | Trainees, fellows, residents, students | Training and evaluation outside the United States | Other educational methods | Bronchoscopy performance |
| Key question 3: Among bronchoscopy trainees, is bronchoscopy training for surgical applications more effective than other training methods for bronchoscopy competency? | Trainees, fellows, residents, students | Surgical applications in bronchoscopy training | Other training methods for surgical applications | Competency assessment |
| Key question 4: Among bronchoscopy trainees, is simulation-based training more effective than other training methods for bronchoscopy competency? | Trainees, fellows, residents, students | Simulation in bronchoscopy training | Other training methods for bronchoscopy | Competency assessment |
USA = United States of America.
A systematic review and meta-analysis by Kennedy et al1 was seriously considered as a possible foundation for developing higher-evidence recommendations instead of consensus statements (where appropriate) for KQ4: Current Practice in Endoscopy Simulation Training. However, the panel decided that the focus of the article was significantly different from what was asked in KQ4 (Table 1). Specifically, the review by Kennedy et al1 focused more on the effectiveness of technology-enhanced simulation approaches, whereas the panel aimed to address simulation as a preferred method to train fellows and residents. Thus, Kennedy et al1 was not used as the foundation for the statements in this document; rather, the referenced individual studies in the review by Kennedy et al1 were added manually for consideration for inclusion during the systematic review.
Study Selection:
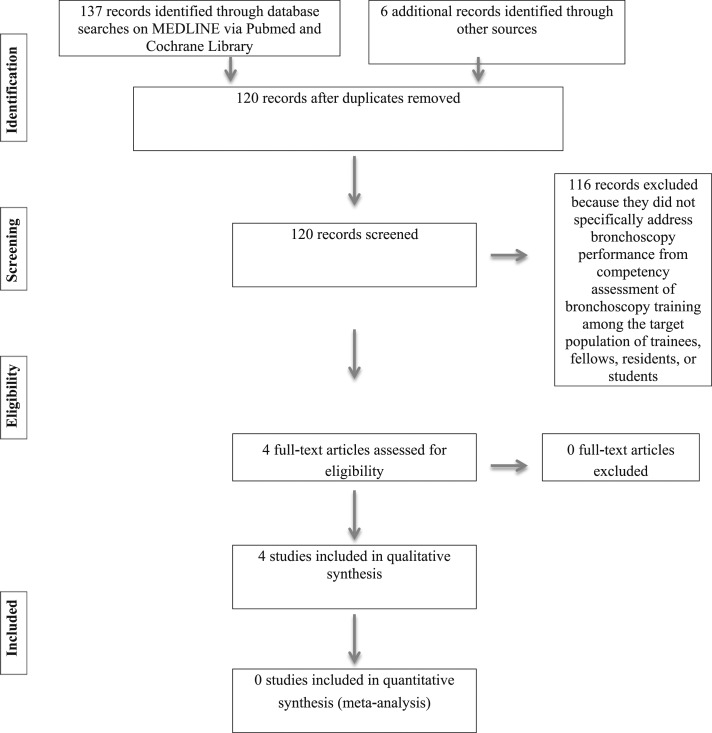
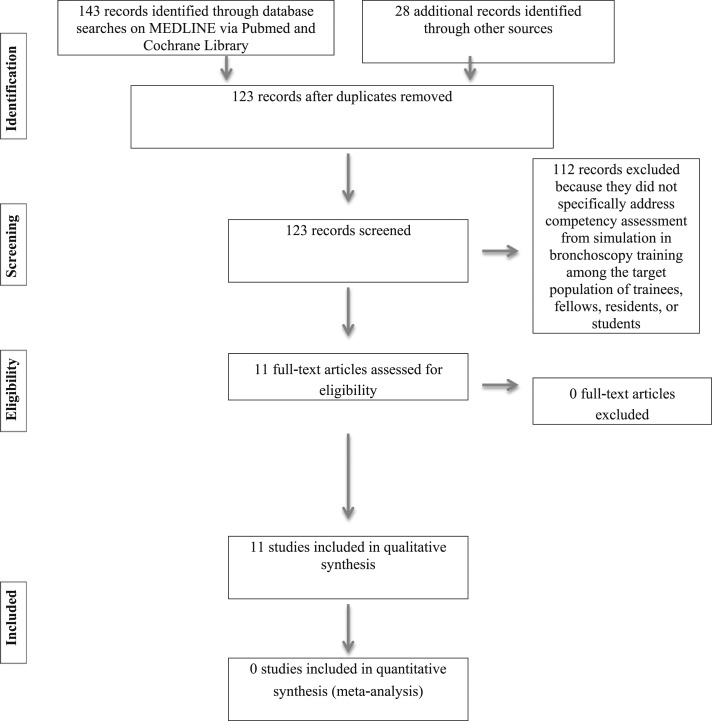
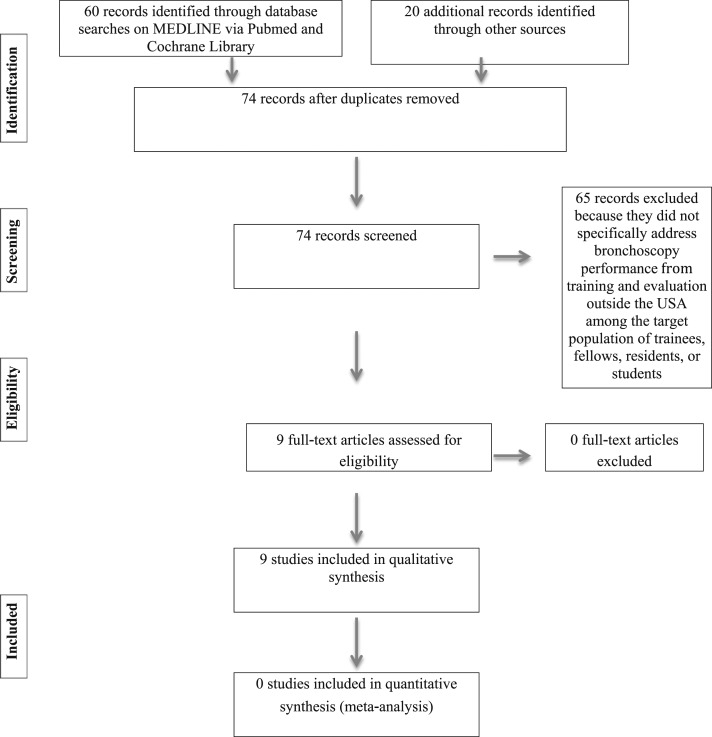
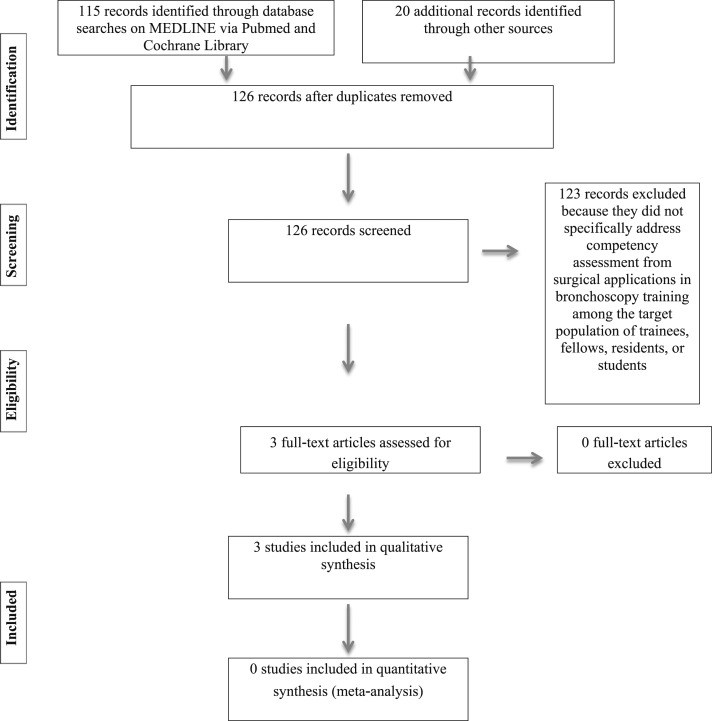
The panelists were assigned to specific topics. From the systematic search performed for each KQ, each topic group screened the identified studies from very specific and particular inclusion criteria based on the PICO components of each KQ (Table 1) and relevance as determined by the panel. Study selection for each KQ occurred in phases as depicted in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagrams (Figs 1-4).2 First, the titles and abstracts of identified records were screened for potential eligibility and relevance. Records deemed eligible by each topic group then underwent full-text screening for final inclusion. After the inclusion phase, the remaining studies had no sufficient data available to serve as a foundation for evidence-based guidelines. Consequently, consensus statements were developed from this limited literature and the clinical knowledge and experience of the panel.
Figure 1 –
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for key question 1: Among bronchoscopy trainees, is competency-based education more effective than other educational methods for superior bronchoscopy performance?
Figure 4 –
PRISMA flow diagram for key question 4: Among bronchoscopy trainees, is simulation-based training more effective than other training methods for bronchoscopy competency? See Figure 1 legend for expansion of abbreviation.
Figure 2 –
PRISMA flow diagram for key question 2: Among bronchoscopy trainees, is training and evaluation outside the USA more effective than inside the USA for superior bronchoscopy performance? USA = United States of America. See Figure 1 legend for expansion of other abbreviation.
Figure 3 –
PRISMA diagram for key question 3: Among bronchoscopy trainees, is bronchoscopy training for surgical applications more effective than other training methods for bronchoscopy competency? See Figure 1 legend for expansion of abbreviation.
Summarizing Evidence and Drafting Suggestions
Drafting Suggestions:
The topic groups each drafted statements based on their clinical expertise and interpretation of the limited evidence with the intent of providing the most appropriate guidance to the end user. The included studies for each KQ were evaluated as an insufficient level of evidence, and all statements were ungraded and consensus based.
Consensus Development:
All drafted statements were presented to the panel through the formal consensus development process based on the Delphi technique.3 The Delphi technique was applied because it is a systematic way to achieve formal consensus on each drafted statement while accounting for group interaction bias and maintaining anonymity among panel respondents. Using an online survey (www.surveymonkey.com), panelists were requested to indicate their level of agreement on each presented statement using a five-point scale derived from the Grading of Recommendations Assessment, Development and Evaluation grid.4,5 Also, each panelist had the option to provide open-ended feedback on each statement with suggested edits or general remarks supporting his or her vote. Panelists who disclosed a potential COI related to a drafted statement refrained from voting on that item (e-Table 1 (135.1KB, xlsx) ).
Each presented statement required a consensus level of at least 80% of respondents voting in agreement to be included in the final manuscript along with a response rate of at least 75% of eligible panelists. These criteria were not met for one item, so the presented statement was revised by the authoring panelists based on the collated anonymous, open-ended feedback and resubmitted for a second round of voting by the panel. The chair then reviewed each final statement along with the entire manuscript to resolve any areas of confusion or inconsistency before it was submitted to the GOC for peer review.
Peer Review
The peer review process was designed to ensure that the content and methodology were accurate and consistent. Identified reviewers from CHEST NetWorks, the GOC, the CHEST Board of Regents, and the CHEST journal reviewed the entire article. The manuscript was revised according to feedback from peer review, and was subsequently approved by the GOC and CHEST Board of Regents prior to submission to the CHEST Journal.
The Current State of Competency Assessment in Bronchoscopy Training
Summary of Evidence
Currently, the determination of competency of trainees in pulmonary and critical care medicine in performing bronchoscopic procedures is entrusted to the fellowship program director by the American College of Graduate Medical Education (ACGME).6 The determination varies from program to program. Some programs provide fellows with several didactic lectures prior to their performing procedures with hands-on supervision; other programs incorporate advanced simulation centers, whereas others have the supervising attending physician fill out checklists to document completion of various steps. Although no one way has been proven the best, the variability alone suggests that outcomes are variable as well.
Different suggestions or requirements for determining competence are based on volume according to ACGME requirements and guidelines published by CHEST, the British Thoracic Society, and the American Thoracic Society/European Respiratory Society.6-9
The ACGME requires the following:
• Fellows must be able to competently perform all medical, diagnostic, and surgical procedures considered essential for the area of practice.
• Fellows must demonstrate competence in procedural and technical skills, including flexible bronchoscopy procedures where endobronchial and transbronchial biopsies and transbronchial needle aspirations are performed (each fellow must perform a minimum of 100 such procedures).
• Fellows must demonstrate knowledge of indications, contraindications, limitations, complications, techniques, and interpretation of results of those diagnostic and therapeutic procedures integral to the discipline. Fellows are expected to develop skills and habits to be able to meet the following goal: obtain procedure-specific informed consent by competently educating patients about rationale, technique, and complications of procedures.
• Direct supervision of procedures performed by each fellow must occur until proficiency has been acquired and documented by the program director.
The American Thoracic Society/European Respiratory Society and CHEST guidelines are summarized in Table 2.10
TABLE 2 ] .
CHEST and ATS/ERS Training Requirements
| Procedure | CHEST Threshold | ATS/ERS Threshold | ATS/ERS Ongoing/Year |
| Advanced bronchoscopy (diagnostic and therapeutic) | ... | ... | ... |
| Rigid bronchoscopy | 20 | 20 | 15 |
| Autofluorescence bronchoscopy | 20 | 10 | ... |
| EBUS guided | 50 | 40 | ... |
| TBNA (radial and convex probe) | ... | 25 | ... |
| EBUS-TBNA | ... | 40 | ... |
| Endoluminal therapies | ... | ... | ... |
| Laser | 15 | 20 | 10-15 |
| Electrocautery/argon plasma coagulation | 15 | 10 | 5-10 |
| Cryotherapy | 10 | 10 | 5-10 |
| Brachytherapy | 5 | 5 | 5-10 |
| Photodynamic therapy | 10 | 10 | 5-10 |
| Airway stents silicone (silastic, metallic, dynamic Y, hybrid) | 20 | 10 | 5-10 |
| Balloon tracheobronchoplasty | 5 | ... | ... |
| TTNA | ... | 10 | 5-10 |
ATS = American Thoracic Society; CHEST = American College of Chest Physicians; EBUS = endobronchial ultrasound; EBUS-TBNA = endobronchial ultrasound-guided transthoracic needle aspiration; ERS = European Respiratory Society; TBNA = transbronchial needle aspiration; TTNA = transthoracic needle aspiration. (Reprinted with permission from Lamb et al.10)
Guidelines based on number of procedures have not been proven adequate to determine competence. Ideally, bronchoscopy educators would link their fellows’ performances to meaningful clinical outcomes rather than to surrogate markers of competence. Such ideal outcomes might include diagnostic yield, complication rates, and patient tolerance. A low-stake multichoice questionnaire of 11 ideal questions on the Essential Bronchoscopist website11 has been used to assess knowledge-based competence, but much more is needed to evaluate the technical and cognitive components of bronchoscopy. The Canadian Anesthesiologists’ Society has demonstrated the use of a bedside observational tool (EBUS-STAT) able to distinguish the bronchoscopist’s level of competence, but this tool has yet to be tested in the training of pulmonary fellows.12 Some training programs have been moving toward incorporating simulation training and web-based virtual bronchoscopy training (see next section). In summary, no validated methods of determining competency exist at this time.
Suggestions:
1. We suggest that professional societies and certifying agencies move from a volume-based certification system to skill acquisition and knowledge-based competency assessment for pulmonary trainees (Ungraded Consensus-Based Statement).
2. We suggest that assessment of skill maintenance and improvement in practice be evaluated regularly in similar fashion as recurrent cognitive examinations (Ungraded Consensus-Based Statement).
3. We suggest that ongoing quality and process improvement systems after initial skill acquisition be introduced (Ungraded Consensus-Based Statement).
Training and Evaluation Outside the United States
Summary of Evidence
An appropriate training program should include some didactic teaching in the form of lectures and be complemented with appropriate books.13,14 Web-based learning using a digital resource such as videos of clinical examples of procedures enhances training.15 Training on inanimate models as part of a multimodality training program helps in the acquisition of specific skills.13
Several articles have suggested that the use of simulators for bronchoscopy and EBUS enhances and speeds up the learning process.16,17 One article suggested that initial demonstration of a few clinical cases by an experienced operator followed by the use of a simulator is more effective than only using the simulator.18 Apprenticeship-style learning alone on patients is associated with more-prolonged procedures, greater doses of sedation, and higher complication rates.19
The evidence suggests a training program that includes all the available tools, such as lectures, books, digital media, interactive computer programs, inanimate models, static bronchoscopy models, simulators, and formal demonstration of both virtual and real clinical cases, will provide the best opportunity for learning. Learners acquire skills differently; hence, a comprehensive program should address the range of educational needs that will resonate with most trainees. Simulators can also be used to evaluate whether individual students have acquired the minimum skills and knowledge required for performing bronchoscopic procedures.
Procedural Numbers Required
In the United Kingdom and Canada, no absolute minimum number of individual procedures is required for a trainee to be deemed competent. Competence is judged by supervisors who directly observe the trainee’s performance of bronchoscopic procedures and sign a document when the trainee is deemed competent for performing unsupervised bronchoscopies. More objective-based outcome assessments are gradually being introduced. For novel procedures, each hospital has an internal governance mechanism to check that the individual performing the procedure has the appropriate skills and training.
Although the European guidelines state minimum numbers of supervised procedures required for bronchoscopy (Table 2), there is no uniform mandatory requirement.8 For example, in Germany, a minimum number of 200 bronchoscopies is required for the trainee to be deemed competent in bronchoscopy. There are no minimum requirements in Australia or New Zealand.20
Clinical Assessment
Competence can be evaluated in the clinical setting. Kemp et al21 evaluated the success rates of consecutive procedures with EBUS by new operators. A learning curve was calculated using cumulative sum analysis. This article highlighted variations in learning curves between individuals and was able to show how outcome-based assessment can be used to determine when an individual has acquired the necessary skills and is competent.
Suggestions:
4. We suggest that bronchoscopy training programs incorporate multiple tools, such as e-learning, lectures, books, case-based reviews, and hands-on training (Ungraded Consensus-Based Statement).
5. We suggest that in countries with comparable levels of medical care, bronchoscopy training program requirements be standardized (Ungraded Consensus-Based Statement).
Bronchoscopy in Thoracic Surgery Training Programs
Summary of Evidence
Although bronchoscopy is a procedure that helps to define the pulmonologist, thoracic surgery training programs require residents to adequately perform a myriad of procedures, some of which are technically much more complicated than bronchoscopy. The available literature in the surgical field includes a limited number of studies, mostly dealing with junior-level general surgery residents (interns); ear, nose, and throat residents; and anesthesia residents.
The American Board of Thoracic Surgery (ABTS) requires resident-trainees in the general thoracic surgery track to perform 40 bronchoscopic procedures. Of those, 30 can be simple diagnostic procedures, including airway inspection, BAL, and endobronchial or transbronchial biopsy. An additional 10 must be therapeutic procedures, including “core out” of tumor, laser, dilatation of strictures, stent placement, and photodynamic therapy, or other interventions such as cryotherapy, electrocautery, or argon plasma coagulation. Investigation of mediastinal adenopathy requires performing 30 procedures, 10 of which must include EBUS with fine needle aspiration.22
A thorough understanding of the role of bronchoscopy is necessary in the diagnostic evaluation and management of patients with benign and malignant disorders of the chest. This understanding is of paramount importance in selecting the ideal bronchoscopic technique and its role in selecting the best surgical treatment of a particular airway or pulmonary problem. This point is where a significant difference emerges between pulmonary and thoracic surgery trainees. Whereas pulmonary fellows may be more focused on the diagnostic and palliative management of a particular chest disorder, thoracic surgery trainees focus on bronchoscopy with an eye toward definitive surgical correction. For example, a patient who presents with an airway tumor occluding the right upper lobe undergoes a diagnostic bronchoscopy. The pulmonologist must obtain tissue for diagnosis and may perform EBUS for staging purposes. The thoracic surgery resident, in addition to obtaining tissue for diagnosis, has to make a decision regarding surgical treatment based on the endoscopic findings. Is the patient a candidate for lobectomy, sleeve lobectomy, or pneumonectomy? A thorough understanding of the airway anatomy and familiarity with surgical techniques and postoperative management are necessary to select the most appropriate treatment option. There is, however, a paucity of good-quality data evaluating basic and advanced diagnostic and therapeutic bronchoscopy (flexible and rigid) training in surgery residents, particularly, in thoracic surgery trainees.
Surgery residents are exposed to bronchoscopy during both general and thoracic surgery residency. In the past, these two groups were clearly separate, and all thoracic surgery trainees had some exposure to bronchoscopy during their general surgery residency before beginning cardiothoracic surgery training. In 2011, however, the Thoracic Surgery Directors Association in conjunction with ABTS established an integrated 6-year program (the I-6 Program).23 These residents begin their cardiothoracic surgery training after completing medical school and have no prior exposure to bronchoscopy. Therefore, they are required to learn the essential skills of bronchoscopy before moving into more-complex endoscopic procedures. An established practice in most thoracic surgery programs is to perform intraoperative bronchoscopy in almost all patients undergoing thoracic surgical procedures. The large majority of these bronchoscopies constitute simple airway inspection because no abnormality is expected and the procedure does not add risk or significant time to the operation. In some circumstances, however, bronchoscopy is an essential part of the procedure, and the information obtained will influence the choice of operation. For example, a tumor in the lobar bronchus or more proximal will determine what type of operation is required, as detailed previously.
Although surgical trainees may be exposed to a reasonable number of diagnostic bronchoscopies during which technical skills can be acquired to become proficient in basic bronchoscopy, this is not true for therapeutic bronchoscopic procedures, such as rigid bronchoscopy, stent placement, dilatation, and endoluminal tumor ablation—procedures that typically require a higher level of practice and skill. There are no reports in the literature evaluating the level of proficiency of recently graduated thoracic surgery trainees, but it is highly unlikely that most are fully competent in advanced therapeutic bronchoscopy at the completion of their residency.
Review of the literature revealed no reports addressing formal training in bronchoscopy among thoracic surgery trainees. Although ABTS and the Thoracic Surgery Directors Association recommend a minimum number of procedures, a belief remains that a structured format incorporating simulation may result in significant benefits, as has been shown in the literature for laparoscopy, GI endoscopy, and bronchoscopy. The existing literature in the surgical field is very limited, and although it demonstrates the value of simulation in training surgery residents for bronchoscopy, it does not apply directly to thoracic surgery trainees because the reports include general surgery; pulmonary medicine; ear, nose, and throat; and anesthesia residents. Blum et al24 conducted a randomized trial to evaluate the effectiveness of a flexible bronchoscopy simulator in teaching clinical bronchoscopy. Three groups of general surgery residents were evaluated while performing an intraoperative flexible bronchoscopy prior to a thoracic surgery procedure. Postgraduate year (PGY) 1 residents were randomly assigned to perform bronchoscopy either with (n = 5) or without (n = 5) preprocedural bronchoscopic simulator training (preoperative AccuTouch Flexible Bronchoscopy Simulator; Immersion Medical). PGY2 and 3 (n = 3) residents with prior bronchoscopic experience (≥ 10 bronchoscopies) underwent evaluation without simulator training. The authors concluded that the skill level of PGY1 residents who had preprocedural training on the simulator was similar to that of PGY2 and 3 residents experienced in bronchoscopy. Limitations of this study include a small sample size and the fact that no cardiothoracic residents were included in this study.
Few studies evaluating simulation training and bronchoscopy among thoracic surgery residents have been performed. Salud et al25 developed a method to measure resident performance during a video-guided rigid bronchoscopy using a mannequin-based simulation. They inserted pressure sensors in a commercially available bronchoscopy task trainer. Participants were divided into two groups based on self-reported levels of expertise: novice (none to minimal experience in rigid bronchoscopy) and expert (moderate to extensive experience). All were either thoracic surgery residents or thoracic surgeons. The time taken to complete the rigid bronchoscopy was of no significant difference between experts and novices; however, novices touched a greater number of areas in the upper airway than experts, showing that novices induce a higher number of unnecessary soft tissue contact than experts. Cohen and colleagues (Alberto de Hoyos, MD; Elaine Cohen, MD; Kyra Wood, BS; Lawrence Salud, MS; Richard Feins, MD; and Carla Pugh, MD, PhD, unpublished data, 2015) took these findings a step farther by using computer analysis to assess soft tissue damage by fellows during rigid bronchoscopy. Thirty-two first-year cardiothoracic surgery residents participated in the study using a rigid bronchoscopy simulator. This modified task trainer was instrumented internally with electronic sensors that monitored and reported forces on contact structures, including the tongue, hypopharynx, vocal cords, upper trachea-esophageal junction, anterior trachea, esophagus, and epiglottis. Electronic data were collected from the sensor-enabled simulator as the participants performed two complete rigid bronchoscopies (video guided and non-video guided), including advancing the rigid bronchoscope through the airway, inspecting the carina, and withdrawing the scope. Analysis of the computer-generated sensor data revealed significant differences between the video-guided and non-video-guided approaches. The video-guided approach required less time and a lower number of tissue contact occasions (frequency). This analysis reconfirmed that the video-guided approach took less time (22.44 s less [P < .01]) and resulted in a lower frequency of tissue contact in a number of anatomic locations, including the hypopharynx and vocal cords. This study is the only one available in thoracic surgery residents using a sensor-monitored simulator of rigid bronchoscopy. It is limited by a small number of participants during a one-time session.
Although none of these studies has been formally validated, there is no inherent reason to believe that the robust work published in simulation and training among pulmonary trainees is not translatable to thoracic surgery residents. Further research is needed to assess the efficacy of simulation in thoracic surgery training for basic and advanced bronchoscopy, to establish benchmarks for competency, and to ensure patient safety.
Suggestion:
6. We suggest that professional societies and certifying agencies that oversee training programs for similar procedures in different medical and surgical specialties standardize requirements where applicable (Ungraded Consensus-Based Statement).
Current Practice in Endoscopy Simulation Training
Summary of Evidence
Simulation technology in bronchoscopy is available in two forms: low-fidelity inanimate mechanical airway models and high-fidelity computer-based electronic simulation.26 Low-fidelity simulation models consist of molded tracheobronchial trees that offer realistic tubular-shaped airway-like structures with accurate anatomy to the first subsegmental bronchial level.27,28 They assist novice learners in memorizing airway anatomy, building muscle memory, and enhancing hand-eye coordination. Their main advantage is their relative low cost; their main disadvantage is the lack of interactive capability, which limits situational learning.
High-fidelity simulation models present computer-generated three-dimensional images of the airways and offer bronchoscopy skill training through a proxy bronchoscope with various scenarios and iterations of anatomy and cases.29 High-fidelity simulators can track performance metrics and generate a performance score. Their main advantages include repeated training in a safe, stress-free environment; exposure to rare or difficult scenarios; and receipt of immediate feedback on performance. The main disadvantage is the high cost.
Some data exist on use of simulation in bronchoscopy training. High-fidelity simulators have been validated as a performance measurement tool with an ability to discriminate among bronchoscopists with varying levels of bronchoscopy skills.15,30-32 High-fidelity simulators have been shown to speed the acquisition of bronchoscopy skills among novice bronchoscopists.15,33-36 This is supported by a well-conducted meta-analysis.1 Both low- and high-fidelity simulators have been compared as teaching tools, with findings suggesting that animal or plastic models may be superior to more costly virtual reality simulators.1
Suggestions:
7. We suggest that simulation specifically be integrated into a structured bronchoscopy teaching curriculum (Ungraded Consensus-Based Statement).
8. We suggest that high-fidelity simulation due to its cost should be offered in regional simulation centers, which should be accessible to all training programs (Ungraded Consensus-Based Statement).
Conclusions
In this in-depth review of the state of the art of teaching bronchoscopy in pulmonary medicine, the findings were not surprising. Few specific guidelines that govern training are available. They are quite divergent when covering the same procedure, depending on which specialty issues them and in what country the health-care provider practices. Little guidance is given on modern teaching tools that should be used, and many documents still suggest volume-based criteria for assessing competency. This does not serve patients well and leaves well-meaning training programs to their own devices on how to best ensure training and competency assessment of their residents and fellows.
Our findings suggest that it may be time to change the conventional approach and consider a redesign of bronchoscopy training curricula, incorporating the formulated suggestions. Standardization, where appropriate, has been shown to decrease variation in outcomes and would foster easier collaboration between training programs in pooling resources, even between specialties. Clearly, it will be equally important to start judging successful skill acquisition with other means than just counting the number of interventions performed. More work is needed in this area over the next few years.
It should also be realized that training and learning should not stop once skill acquisition has been completed. Rather, one should consider this part of practice as ongoing learning with opportunity for continuous improvement and, potentially, for periodic reassessment of skill levels, such as is the case of advanced cardiac life support or cognitive knowledge in most medical specialties.
It can be argued that the process used for this review and consensus building is flawed and based on simple consensus by a limited number of individuals and that the science underlying some of the suggestions is soft. We would agree that a higher degree of research grade in the science of bronchoscopy training would be desirable, but it simply does not exist. We are encouraged to see that new studies adding to the body of knowledge in this area have been published since the time of our literature review. What cannot be argued with is the disparity of training guidelines that clearly makes no sense when looking at the same procedure and the very high degree of agreement among the panel members through the modified Delphi process on the suggestions.
We recognize that this review and its potential implications are focused on bronchoscopy training in the developed world. This is partially driven by the fact that little published evidence is available outside and that many resources reviewed here may plainly not be available. It is certainly our hope that a focus on training content and standardization will show positive effects all around the world.
Taking into account the advances in technology in the past decade with their quick adaptation in practice and their ability to supplant more-invasive procedures often performed surgically, this review of bronchoscopy training requirements across specialties and delivery systems is timely. We hope that our findings and suggestions prove useful for ongoing research in bronchoscopy training and potentially to other procedural training.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: A. E. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. A. E., M. M. W., C. A. R., J. D. B., D. J. A.-H., P. L. S., F. J. F. H., A. d. H. P., J. O., L. Y., and G. A. S. participated in the literature review, condensing of the information, and drafting of the final suggestions. Specific assignments were as follows: The Current State of Competency Assessment in Training Bronchoscopy, C. A. R., J. D. B., and D. J. A.-H.; Training and Evaluation Outside the United States summary of evidence, P. L. S. and F. J. F. H.; Bronchoscopy in Thoracic Surgery Training Programs literature review, A. d. H. P. and G. A. S.; and Current Practice in Endoscopy Simulation Training, A. E., M. M. W., and L. Y. J. O. performed the systematic searches for each topic and supervised the methodology design for the project.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Ernst received compensation for consulting services to Boston Scientific Corporation, Pulmonx, Uptake Medical, and Aeris. In the past 3 years Drs Wahidi, Buckley, and Addrizzo-Harris received compensation for legal assistance to malpractice and personal injury cases. Dr Wahidi received compensation for consulting services to Olympus Corporation; Terumo Medical Corporation; Gerson Lehrman Group, Inc; Holaira, Inc; Johnson & Johnson Services, Inc; Pinnacle Systems; Boston Scientific Corporation; Uptake Medical; and PneumRx. Dr Wahidi also serves on the board of the American Association of Bronchology and Interventional Pulmonology and serves on several committees with the American Thoracic Society. Dr Wahidi taught numerous courses at CHEST, all of which included simulation. Dr Buckley received salary support from a grant on open disclosures of medical errors from the Agency for Healthcare Research and Quality and served as the program chair of the 2013 CHEST Annual Meeting but received no honoraria. Dr Addrizzo-Harris serves on the board of the Association of Pulmonary and Critical Care Medicine Program Directors. Dr Shah received compensation from Olympus Corporation, Pulmonx, and PneumRx for consulting services. Dr Herth received compensation for speaking engagements sponsored by Pulmonx and Novartis AG. Dr Yarmus received compensation for speaking engagements sponsored by Boston Scientific Corporation and received salary support from a grant for lung cancer research from the National Institutes of Health. Dr Yarmus also serves on a committee with the American Thoracic Society and has participated in a CHEST course related to bronchoscopy and EBUS. Dr Silvestri has received research support and served on the scientific advisory board for Allegro Diagnostics Inc; Veran Medical Technologies, Inc; and Olympus Corporation. Dr Silvestri also has received research support from Bronchus and has been a consultant to Boston Scientific Corporation. Drs Read, de Hoyos Parra, and Ornelas have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Endorsements: This guideline has been endorsed by the Canadian Thoracic Society and the European Respiratory Society.
Role of sponsors: CHEST was the sole supporter of these guidelines, this article, and the innovations addressed within.
Other contributions: The panel thanks Rex Yung, MD, for his support in his role as liaison from the GOC.
Additional information: The e-Table can be found in the Supplemental Materials section of the online article.
ABBREVIATIONS
- ABTS
American Board of Thoracic Surgery
- ACGME
Accreditation Council for Graduate Medical Education
- CHEST
American College of Chest Physicians
- COI
conflict of interest
- EBUS
endobronchial ultrasound
- GOC
Guidelines Oversight Committee
- KQ
key question
- PYG
postgraduate year
Footnotes
FOR EDITORIAL COMMENT SEE PAGE 301
FUNDING/SUPPORT: This consensus statement was supported solely by internal funds from CHEST.
DISCLAIMER: CHEST Expert Panel Reports are intended for general information only, are not medical advice, and do not replace professional medical care and physician advice, which always should be sought for any medical condition. The complete disclaimer for this guideline can be accessed at http://www.chestnet.org/Guidelines-and-Resources/Guidelines-and-Consensus-Statements/CHEST-Guidelines.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Kennedy CC, Maldonado F, Cook DA. Simulation-based bronchoscopy training: systematic review and meta-analysis. Chest. 2013;144(1):183-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.PRISMA. The PRISMA statement. PRISMA website. http://www.prisma-statement.org/statement.htm. Accessed October 25, 2014.
- 3.Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: characteristics and guidelines for use. Am J Public Health. 1984;74(9):979-983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaeschke R, Guyatt GH, Dellinger P, et al. ; GRADE Working Group. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008;337:a744. [DOI] [PubMed] [Google Scholar]
- 5.Lewis SZ, Diekemper R, Ornelas J, Casey KR. Methodologies for the development of CHEST guidelines and expert panel reports. Chest. 2014;146(1):182-192. [DOI] [PubMed] [Google Scholar]
- 6.Program and Institutional Accreditation. Accreditation Council for Graduate Medical Education website. http://www.acgme.org/acgmeweb/tabid/83/ProgramandInstitutionalAccrediation.aspx. Accessed May 2, 2014.
- 7.Ernst A, Silvestri GA, Johnstone D; American College of Chest Physicians. Interventional pulmonary procedures: guidelines from the American College of Chest Physicians. Chest. 2003;123(5):1693-1717. [DOI] [PubMed] [Google Scholar]
- 8.Bolliger CT, Mathur PN, Beamis JF, et al. ; European Respiratory Society/American Thoracic Society. ERS/ATS statement on interventional pulmonology. Eur Respir J. 2002;19(2):356-373. [DOI] [PubMed] [Google Scholar]
- 9.British Thoracic Society Bronchoscopy Guidelines Committee, a Subcommittee of Standards of Care Committee of British Thoracic Society. British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001;56(suppl 1):i1-i21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lamb CR, Feller-Kopman D, Ernst A, et al. An approach to interventional pulmonology fellowship training. Chest. 2010;137(1):195-199. [DOI] [PubMed] [Google Scholar]
- 11.The Essential Bronchoscopist website. http://www.essential-bronchoscopy.org/. Accessed May 2, 2014.
- 12.Davoudi M, Colt HG, Osann KE, Lamb CR, Mullon JJ. Endobronchial ultrasound skills and tasks assessment tool: assessing the validity evidence for a test of endobronchial ultrasound-guided transbronchial needle aspiration operator skill. Am J Respir Crit Care Med. 2012;186(8):773-779. [DOI] [PubMed] [Google Scholar]
- 13.Deutsch ES, Christenson T, Curry J, Hossain J, Zur K, Jacobs I. Multimodality education for airway endoscopy skill development. Ann Otol Rhinol Laryngol. 2009;118(2):81-86. [DOI] [PubMed] [Google Scholar]
- 14.Kupeli E, Memis L, Ozdemirel TS, Ulubay G, Akcay S, Eyuboglu FO. Transbronchial needle aspiration “by the books.” Ann Thorac Med. 2011;6(2):85-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duplaga M, Juszkiewicz K, Leszczuk M. Telelearning standards and their application in medical education. Stud Health Technol Inform. 2004;105:308-316. [PubMed] [Google Scholar]
- 16.Ost D, DeRosiers A, Britt EJ, Fein AM, Lesser ML, Mehta AC. Assessment of a bronchoscopy simulator. Am J Respir Crit Care Med. 2001;164(12):2248-2255. [DOI] [PubMed] [Google Scholar]
- 17.Stather DR, Maceachern P, Rimmer K, Hergott CA, Tremblay A. Assessment and learning curve evaluation of endobronchial ultrasound skills following simulation and clinical training. Respirology. 2011;16(4):698-704. [DOI] [PubMed] [Google Scholar]
- 18.Bjerrum AS, Hilberg O, van Gog T, Charles P, Eika B. Effects of modelling examples in complex procedural skills training: a randomised study. Med Educ. 2013;47(9):888-898. [DOI] [PubMed] [Google Scholar]
- 19.Stather DR, MacEachern P, Chee A, Dumoulin E, Tremblay A. Trainee impact on procedural complications: an analysis of 967 consecutive flexible bronchoscopy procedures in an interventional pulmonology practice. Respiration. 2013;85(5):422-428. [DOI] [PubMed] [Google Scholar]
- 20.Fielding D, Phillips M, Robinson P, Irving L, Garske L, Hopkins P; Thoracic Society of Australia and New Zealand. Advanced interventional pulmonology procedures: training guidelines from the Thoracic Society of Australia and New Zealand. Respirology. 2012;17(8):1176-1189. [DOI] [PubMed] [Google Scholar]
- 21.Kemp SV, El Batrawy SH, Harrison RN, et al. Learning curves for endobronchial ultrasound using cusum analysis [published correction appears in Thorax. 2010;65(9):844]. Thorax. 2010;65(6):534-538. [DOI] [PubMed] [Google Scholar]
- 22.Operative requirements. American Board of Thoracic Surgery website. https://www.abts.org/root/home/certification/operative-requirements.aspx. Accessed May 2, 2014.
- 23.Booklet of information. American Board of Thoracic Surgery website. https://www.abts.org/documents/PDF/2013_Booklet_of_Information.pdf. Accessed May 2, 2014.
- 24.Blum MG, Powers TW, Sundaresan S. Bronchoscopy simulator effectively prepares junior residents to competently perform basic clinical bronchoscopy. Ann Thorac Surg. 2004;78(1):287-291. [DOI] [PubMed] [Google Scholar]
- 25.Salud LH, Peniche AR, Salud JC, de Hoyos AL, Pugh CM. Toward a simulation and assessment method for the practice of camera-guided rigid bronchoscopy. Stud Health Technol Inform. 2011;163:535-541. [PubMed] [Google Scholar]
- 26.Davoudi M, Colt HG. Bronchoscopy simulation: a brief review. Adv Health Sci Educ Theory Pract. 2009;14(2):287-296. [DOI] [PubMed] [Google Scholar]
- 27.Di Domenico S, Simonassi C, Chessa L. Inexpensive anatomical trainer for bronchoscopy. Interact Cardiovasc Thorac Surg. 2007;6(4):567-569. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg R, Colt HG, Davoudi M, Cherrison L. Realistic and affordable lo-fidelity model for learning bronchoscopic transbronchial needle aspiration. Surg Endosc. 2009;23(9):2047-2052. [DOI] [PubMed] [Google Scholar]
- 29.Bro-Nielsen M, Tasto JL, Cunningham R, Merril GL. PreOp endoscopic simulator: a PC-based immersive training system for bronchoscopy. Stud Health Technol Inform. 1999;62:76-82. [PubMed] [Google Scholar]
- 30.Moorthy K, Smith S, Brown T, Bann S, Darzi A. Evaluation of virtual reality bronchoscopy as a learning and assessment tool. Respiration. 2003;70(2):195-199. [DOI] [PubMed] [Google Scholar]
- 31.Crawford SW, Colt HG. Virtual reality and written assessments are of potential value to determine knowledge and skill in flexible bronchoscopy. Respiration. 2004;71(3):269-275. [DOI] [PubMed] [Google Scholar]
- 32.Chen JS, Hsu HH, Lai IR, et al. ; National Taiwan University Endoscopic Simulation Collaborative Study Group (NTUSEC). Validation of a computer-based bronchoscopy simulator developed in Taiwan. J Formos Med Assoc. 2006;105(7):569-576. [DOI] [PubMed] [Google Scholar]
- 33.Jabbour N, Reihsen T, Sweet RM, Sidman JD. Psychomotor skills training in pediatric airway endoscopy simulation. Otolaryngol Head Neck Surg. 2011;145(1):43-50. [DOI] [PubMed] [Google Scholar]
- 34.Colt HG, Crawford SW, Galbraith O., III Virtual reality bronchoscopy simulation: a revolution in procedural training. Chest. 2001;120(4):1333-1339. [DOI] [PubMed] [Google Scholar]
- 35.Wahidi MM, Silvestri GA, Coakley RD, et al. A prospective multicenter study of competency metrics and educational interventions in the learning of bronchoscopy among new pulmonary fellows. Chest. 2010;137(5):1040-1049. [DOI] [PubMed] [Google Scholar]
- 36.Davoudi M, Wahidi MM, Zamanian Rohani N, Colt HG. Comparative effectiveness of low- and high-fidelity bronchoscopy simulation for training in conventional transbronchial needle aspiration and user preferences. Respiration. 2010;80(4):327-334. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement