Abstract
Purpose
Radiation therapy remains an essential to treatment for patients with parameningeal rhabdomyosarcoma (PMRMS), and early radiation therapy may improve local control for patients with intracranial extension (ICE).
Methods and Materials
To address the role of radiation therapy timing in PMRMS in the current era, we reviewed the outcome from two recent clinical trials for intermediate-risk RMS, IRS-IV and Children’s Oncology Group (COG) D9803. PMRMS Patients on IRS-IV with any high risk features (cranial nerve palsy [CNP], cranial base bony erosion [CBBE] or ICE) were treated immediately at day 0 while PMRMS without any of these three features received week 6–9 RT. D9803 PMRMS patients with ICE received day 0 XRT as well; however those with either CNP or CBBE had XRT at week 12.
Results
Compared with the 198 PMRMS patients from IRS-IV, the 192 PMRMS patients from D9803 had no difference (p < 0.05) in 5 year local failure (19% vs. 19%), failure-free-survival (70% vs. 67%), or overall survival (75% vs. 73%) in aggregate. 5 year local failure rates by subset did not differ when classified as no risk features (none, 15% vs 19%, p=0.25), cranial nerve palsy/cranial base of skull erosion (CNP/CBBE, 15% vs 28%, p=0.22), or intracranial extension (ICE, 21% vs 15%, p=0.27). The D9083 patients were more likely to have initial MRI staging (71% vs. 53%).
Conclusions
These data support that a delay in radiation therapy for high risk PMRMS features of CNP/CBBE does not compromise clinical outcomes.
Keywords: IRS-IV, D9803, parameningeal, intracranial extension, radiotherapy
INTRODUCTION
Radiation therapy remains a critical component of multi-modality treatment of patients with parameningeal rhabdomyosarcoma (PMRMS) as demonstrated in the accumulated experience of multi-institutional trials. The presence of high risk of meningeal impingement factors in PMRMS including cranial nerve palsy (CNP), cranial base bony erosion (CBBE), and, most significantly, intracranial extension (ICE) are associated with an increased risk of local progression(1). Treatment strategies to reduce local progression included the use of intrathecal chemotherapy and craniospinal irradiation, evolving recently to involved field irradiation. During this same period, investigators observed an increase in the proportion of PMRMS patients diagnosed with intracranial extension (ICE) from 19% on IRS-II to 41% on IRS IV(2) to 46% on D9803(3). High risk PMRMS patients had improved local control when initiation of radiation therapy occurred within two weeks of diagnosis, although failure-free survival (FFS) and overall survival were similar regardless of the timing of radiotherapy(2). Radiation treatment planning also has evolved from 2 dimensional to 3 dimensional conformal therapy to intensity modulated radiation therapy (IMRT). With these improvements and changes in patient classification, the appropriate timing of radiation therapy for PMRMS patients has become a subject of interest especially with respect for those with high risk of meningeal impingement.
The two most recently completed intermediate-risk PMRMS studies, IRS-IV and Children’s Oncology Group (COG) D9803 differed in the timing of radiation therapy for patients without ICE and help address this issue. We compared the patient characteristics, outcome, and treatment, with an emphasis on the timing of radiation therapy. In IRS-IV, PMRMS patients with high risk features of CNP/CBBE and/or ICE were irradiated immediately (as close to day 0 as possible), while in D9803 high risk PMRMS patients with CNP/CBBE but without ICE were irradiated at week 12. Both IRS-IV and D-9803 required central submission and review of diagnostic imaging studies and radiation treatment plans to optimize the standardization of the technical aspects of radiation therapy delivery in determining PMRMS treatment planning for clinical trial enrollment.
METHODS
Patient Characteristics
We conducted a subgroup analysis of newly diagnosed, intermediate-risk PMRMS patients with Group III disease (patients with residual disease after resection or biopsy) enrolled on either IRS-IV (198 patients) from 1991–1997 or D9083 (192 patients) from 1999–2005 using the COG central database. The initial outcomes for these trials have been reported (3–5). The eligibility criteria were similar for patients enrolled on either IRS-IV or D9803, and both studies required submission for central review of tumor material to confirm study eligibility. For our analysis, we included eligible for IRS-IV or D9803, Group III patients with PMRMS who had information on type of meningeal involvement. We investigated PMRMS patients with classified high risk features as: None, CNP/CBBE without ICE, and ICE. The median follow-up for this analysis was 8.5 years (range 0 to 12.9 years) for IRS-IV and 5.6 years (range 0 to 9.3 years) for D9803.
Statistical Analysis
A chi-square or Fisher’s exact test when appropriate was used to compare the difference in proportions for baseline characteristics between the two studies. Time to event distributions were estimated using the method of Kaplan and Meier(6) and were compared using the log-rank test(7). Failure-free survival was defined as patients alive without any disease recurrence, local or distal. Estimates of time to local failure were calculated using cumulative incidence curves. A failure was classified as “local” if a local failure was any part of the failure: local only, local and regional, or local and distant. Other failures (distant only, or death as a first event.) were considered as competing risks.
RESULTS
Patient Characteristics
In order to investigate the effect of the timing of radiation on local control, we first determined the underlying differences between the patient cohorts. PMRMS patients on D9803 differed from patients on IRS-IV with respect to several baseline characteristics: a smaller proportion of D9803 patients were classified as CNP/CBBE (13% vs. 27%, p=0.002); a larger proportion of D9803 patients had alveolar histology (37% vs. 18%, p<0.0001) and a smaller proportion of D9803 patients had T2 tumor stage (75% vs. 86%, p=0.007) relative to IRS-IV PM patients (Table 1). The proportion of patients with alveolar histology was not an artifact of the subset analysis as there were 46% of D9803 and 21% IRS-IV PMRMS patients with alveolar histology. Of the 198 patients on IRS-IV, 163 had pretreatment imaging studies submitted for central review with 104 (53%) having MRI, which was less than D9803 where 136 (71%) of the 192 patients had an MRI at baseline. The decrease in the proportion of D9803 patients with CNP/CBBE was not explained by an increase in ICE detection.
Table 1.
Distribution of select patient characteristics by study
| D9803 | IRS-IV | ||||
|---|---|---|---|---|---|
| Variable | Frequency | Percent | Frequency | Percent | p-value |
| Age | |||||
| <1 years | 0 | 1 | 1 | ||
| 1–9 years | 125 | 65 | 140 | 70 | |
| 10+ years | 67 | 35 | 57 | 29 | 0.23 |
| Gender | |||||
| Male | 117 | 61 | 123 | 62 | |
| Female | 75 | 39 | 75 | 38 | 0.83 |
| PM Group | |||||
| Neither ICE nor CNP/CBBE | 80 | 42 | 65 | 33 | |
| CNP/CBBE | 25 | 13 | 54 | 27 | |
| ICE | 87 | 45 | 79 | 40 | 0.002 |
| Histology | |||||
| Alv | 71 | 37 | 36 | 18 | |
| Emb/Spl/Bot | 110 | 57 | 152 | 77 | |
| Other | 11 | 5 | 10 | 5 | <0.0001 |
| Stage | |||||
| 2 | 77 | 40 | 75 | 38 | |
| 3 | 115 | 60 | 123 | 62 | 0.68 |
| Size | |||||
| <= 5 CM | 94 | 49 | 89 | 46 | |
| >5 CM | 98 | 51 | 106 | 54 | 0.54 |
Abbreviations Used: CNP/CBBE: cranial nerve palsy or cranial base boney erosion without intracranial extension; ICE: intracranial extension; PM: Parameningeal; Alv: Alveolar; Emb: Embryonal; Spl: Spindle Cell; Bot: Botryoid.
Timing of Radiation Therapy delivery
We determined the actual delivery dates of radiation therapy in both patient cohorts. There was a high compliance rate to protocol guidelines for the timing of XRT as shown in Table 2, with 89–100% of patients starting radiation on time as dictated by both D9803 and IRS-IV. As expected by protocol, IRS-IV patients with no high risk features started radiotherapy at a median of about 10 weeks (69 days) whereas for D9803 treated patients it was about 14 weeks (96 days), reflecting a planned delay in D9803 to assess chemotherapy response For patients with ICE the median start of radiotherapy was week 1 for both groups. Therefore, this analysis cannot estimate the effect of radiation timing on those patients with ICE. For patients with CNP/CBBE only the median start of radiotherapy was: IRS-IV, week 1; D9803, week 13. Therefore, we were able to explore in CNP/CBBE patients whether differences in timing between early (IRS-IV) versus late (D9803) XRT resulted in differences in local failure rates.
Table 2.
Expected Week and Distribution of RT Delivery for PM Groups by Study
| D9803 | IRS-IV | |||
|---|---|---|---|---|
| PM Group | Expected | RT Delivered | Expected | RT Delivered |
| None (Neither ICE nor CNP/CBBE) | Week 12 | 73/80 (91%) | Week 6–9 | 58/65 (89%) |
| CNP/CBBE | Week 12 | 22/25 (88%) | Day 0 | 53/54 (98%) |
| ICE | Day 0 | 81/87 (93%) | Day 0 | 79/79 (100%) |
Clinical Outcomes
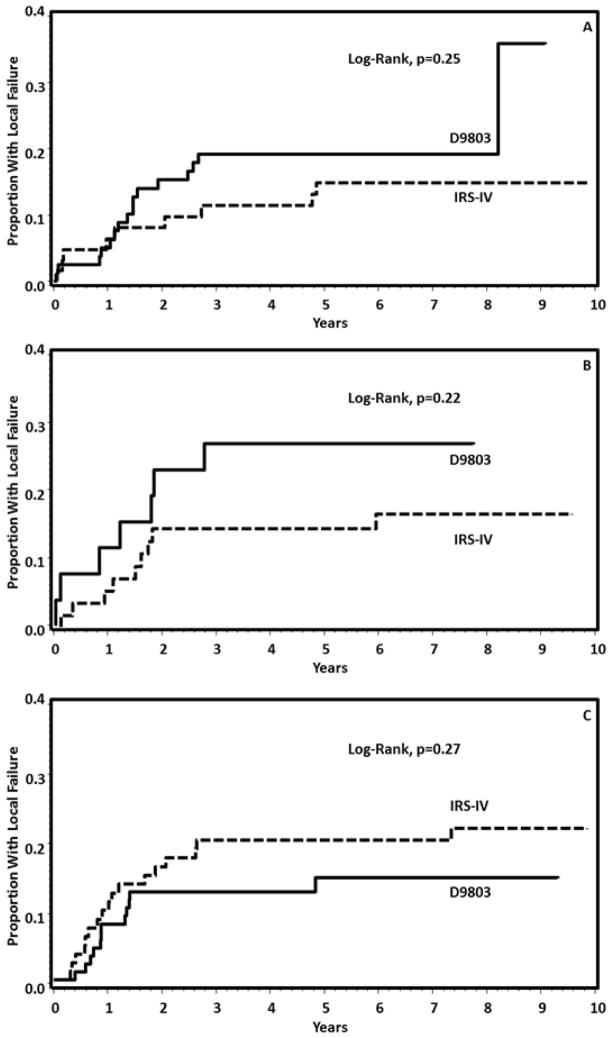
Differences in local failure (LF) among the PMRMS subgroups (No high risk features, [None], CNP/CBBE, or ICE) are shown in Figure 1. The overall failures observed in the 3 subsets were None 45; CNP/CBBE 25; ICE 56. Local failures were the majority of these. For these events, assuming a 5% level of statistical significance (2-sided) and 80% power, the difference that can be detected is a relative risk 0.47:1.00. The D9803 patients with CNP/CBBE were intended to begin RT at Week 12, in contrast to the IRS-IV patients with CNP/CBBE who were intended to begin radiation at Day 0 (Table 2). The estimates of cumulative incidence of local failure by study for each of the PM subsets were reported. For patients classified as none (Figure 1A), IRS-IV had a 15% (95%CI, 7% to 25%) while D9803 demonstrated a 19% (95% CI, 11% to 29%) risk of local failure. Patients with CNP/CBBE (Figure 1B) were observed in IRS IV to have a 15% (95% CI, 7% to 26%) whereas D9803 patients had a 28% (95%CI, 12% to 46%) risk of local failure at five years. Those with ICE (Figure 1C) in IRS IV had a 21% (95%CI, 12% to 30%) five year local failure rate compared with 15% (95% CI, 8% to 24%) in D9803. As local failure can influence distant failure, we looked for differences in failure free survival between the two groups
Figure 1. Local Failure Rates for PMRMS patients by degree of intracranial extension between IRS-IV and D9803.
A. The local failure rates for patients with no intracranial extension (A), CNP/CBBE (B) and ICE (C) for patients enrolled on IRS-IV (dashed line) or D9803 (solid line).
We determined the observed failure free survival (FFS) rates between the three PMRMS subsets. There were no statistically significant differences in FFS observed between the IRS-IV and D9803 patients within the None (p=0.35), CNP/CBB (p=0.09), or ICE (p=0.61) subsets. These results along with figure 1 are consistent with no detectable difference of either LR or FFS based on the presence of PM risk factors.
We examined differences in aggregate outcome between PMRMS patients from IRS-IV and D9803. There was no difference in the cumulative LF, with a 5-year estimate nearly 19% for both studies (p=0.67), Figure 2. The 5-year FFS of IRS-IV (70%) versus that in D9803 (67%, p=0.32) were also similar. The 5-year overall survival rates (OS) were also similar, 75% in IRS-IV versus 73% in D9803 (p=0.45).
Figure 2. Local Failure Rates for all PMRMS patients regardless of intracranial extension between IRS-IV and D9803.
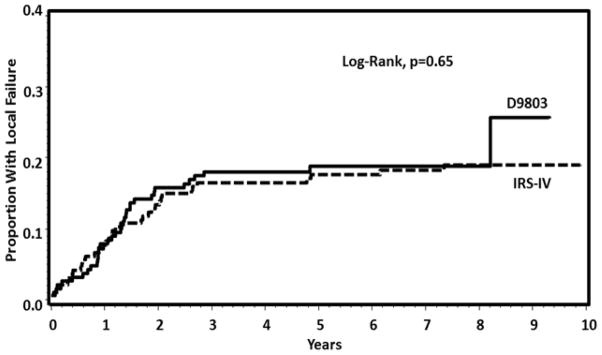
The local failure rate for patients enrolled on IRS-IV (dashed line) or D9803 (solid line).
DISCUSSION
We conducted this study in order to investigate whether timing of radiation therapy influenced LF, FFS, or OS in PMRMS patients with high risk features, in aggregate or divided into PM risk factor groups. We compared two previously reported sequential cooperative group trials, D9803 and IRS-IV which differed in their timing of radiation therapy for patients with CNP or CBBE. Importantly, the rates of protocol compliance regarding RT timing were 89% or better for all PMRMS subtypes, minimizing the likelihood of an intent-to-treat analysis error. We found overall no difference in LF, FFS, or OS for PMRMS patients between these two trials overall or analyzed separately by high risk features, CNP/CBBE, or ICE. These observations, however, deserve further explanation.
The most readily identifiable difference among the cohorts which might be expected to influence clinical outcome was fewer D9803 patients fewer had CBP/CBBE, altering the distribution of PM risk factors between the studies. Patients treated on D9803 were less likely to be diagnosed with CNP/CBBE with higher rates of both None and ICE seen than PM patients treated on IRS-IV. This is not consistent with merely increased sensitivity of imaging studies, as this would result in a higher rate of both CBBE and ICE. Alternatively, more sensitive imaging might result the following two scenarios. First, some patients previously classified as CNP/CBBE could be classified as ICE due to subtle meningeal enhancement seen better on MRI than CT. Second, ambiguous abnormalities on imaging which previously were consistent with CBBE might actually be seen more clearly and classified as None. MRI has been shown to complement the inherent disadvantages of CT imaging in other tumor sites such as nasopharyngeal carcinoma to delineate base of skull erosion and intracranial extension to alter staging(8) or in detecting perineural spread of adenoid cystic carcinoma(9). In reality, the D9803 cohort has a bimodal distribution compared to the more uniform distribution of IRS-IV, and this may indicate patients classified as having CNP/CBBE are clearly not comparable between the two studies.
After determining the baseline differences and similarities between the two cohorts, we examined LF, FFS, and OS. The FFS for the None and ICE subsets do not differ between IRS-IV and D9803, which is not surprising since these groups were treated with delayed (None) or early (ICE) XRT on both studies. Patients with CNP/CBBE however, received early XRT on IRS-IV in contrast to delayed XRT on D9803. We did not find a statistically significant difference seen for the CNP/CBBE subset in LF or FFS. It is unclear whether the patients being compared are indeed similar because of the substantial difference in the distribution of patients across the PM risk factor subsets between the two studies. However, additional attempts to reclassify the distribution would also be fraught with recall bias as well as differences in potentially available imaging modalities. Delaying XRT could increase the rate of progression for chemotherapy-resistant tumors. However, the actual rate of progression during chemotherapy for both of these studies as a whole was only 2%, and was only 2.5% for the parameningeal RMS subets none and CNP/CBBE (10). Despite these limitations to our methodology, there is no clear evidence that delaying radiation until week 12 for patients with CNP and CBBE compromises LF, FFS, or OS Even though no significant difference could be appreciated for LF as function of RT timing, the power calculations suggest that this high p value may be due to a deficiency in statistical power, and in fact a difference may exist between these two cohorts that was not detected. We are unable to make a statement regarding the timing of radiation for patients with ICE as both studies required these patients to have immediate irradiation.
Additional investigators have reported satisfactory results for group III PMRMS patients with high risk features detected by imaging. In a pilot trial designed to determine the feasibility of a response-based approach, 26 patients with ICE, CBBE, or CNP were treated with neoadjuvant chemotherapy and XRT delivered at week 12 unless there was progressive disease after 4 cycles of intensified chemotherapy (11). Twenty five of the 26 patients had a complete or partial response, and the remaining patient had no response, consistent with a small risk of progression with chemotherapy. This approach led to a 5 year event-free survival of 81+/−15% and local control of 92 +/− 11%. These data compare favorably to the D9803 PMRMS patients with reported four year FFS of 68% and OS of 73% and the IRS-IV FFS of 61% and OS of 65%.
There are implications from our study for current and future treatment of patients with PMRMS. First, patients with CNP/CBBE who are treated using modern radiation techniques may not have as poor a prognosis as identified on IRS-II and III. If so, management of PMRMS patients could be included on general studies with stratification based on absence or presence of being a PM site with or without ICE. The previously reported analysis of IRSII, III, and IV observed that earlier XRT does lower local failure rates for all PMRMS patients with high-risk factors without improving FFS. However, our data suggest that in the era of modern imaging, delaying XRT for those with high risk features of CNP/CBBE may not negatively impact local failure. We cannot determine whether those with imaging evidence of frank ICE may also delay radiation therapy. Future studies must ensure modern and appropriate imaging, along with a dedicated central review.
SUMMARY.
Early irradiation of high-risk Parameningeal Rhabdomyosarcoma (PMRMS) patients on IRS II-IV reduced local failure rates. D9803 allowed some high-risk patients to received delayed radiation therapy. Patients with cranial nerve palsy (CNP) or cranial base boney erosion (CBBE) treated on IRS IV (immediate radiation) versus D9803 (delayed radiation) had similar rates of local failure. These results suggest in the modern era PMRMS patients with CNP/CBBE may receive delayed radiation without compromising local failure risk.
Acknowledgments
ACS would like to thank the members of the COG STS committee for mentorship and guidance necessary for the completion of this study. Supported by Grants No. U10 CA98543, U10 CA98413, and U10 CA29511 from the National Cancer Institute/National Institutes of Health. Presented at the SIOP/PROS meeting, London, UK, October 5th, 2012.
Footnotes
Conflicts of Interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Raney RB, Jr, Tefft M, Newton WA, et al. Improved prognosis with intensive treatment of children with cranial soft tissue sarcomas arising in nonorbital parameningeal sites. A report from the Intergroup Rhabdomyosarcoma Study. Cancer. 1987;59:147–155. doi: 10.1002/1097-0142(19870101)59:1<147::aid-cncr2820590129>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 2.Michalski JM, Meza J, Breneman JC, et al. Influence of radiation therapy parameters on outcome in children treated with radiation therapy for localized parameningeal rhabdomyosarcoma in Intergroup Rhabdomyosarcoma Study Group trials II through IV. Int J Radiat Oncol Biol Phys. 2004;59:1027–1038. doi: 10.1016/j.ijrobp.2004.02.064. [DOI] [PubMed] [Google Scholar]
- 3.Arndt CA, Stoner JA, Hawkins DS, et al. Vincristine, actinomycin, and cyclophosphamide compared with vincristine, actinomycin, and cyclophosphamide alternating with vincristine, topotecan, and cyclophosphamide for intermediate-risk rhabdomyosarcoma: children’s oncology group study D9803. J Clin Oncol. 2009;27:5182–5188. doi: 10.1200/JCO.2009.22.3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crist WM, Anderson JR, Meza JL, et al. Intergroup rhabdomyosarcoma study-IV: results for patients with nonmetastatic disease. J Clin Oncol. 2001;19:3091–3102. doi: 10.1200/JCO.2001.19.12.3091. [DOI] [PubMed] [Google Scholar]
- 5.Donaldson SS, Meza J, Breneman JC, et al. Results from the IRS-IV randomized trial of hyperfractionated radiotherapy in children with rhabdomyosarcoma--a report from the IRSG. Int J Radiat Oncol Biol Phys. 2001;51:718–728. doi: 10.1016/s0360-3016(01)01709-6. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan ELMP. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 7.Peto R, Pike MC, Armitage P, et al. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer. 1977;35:1–39. doi: 10.1038/bjc.1977.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liao XB, Mao YP, Liu LZ, et al. How does magnetic resonance imaging influence staging according to AJCC staging system for nasopharyngeal carcinoma compared with computed tomography? Int J Radiat Oncol Biol Phys. 2008;72:1368–1377. doi: 10.1016/j.ijrobp.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Hanna E, Vural E, Prokopakis E, et al. The sensitivity and specificity of high-resolution imaging in evaluating perineural spread of adenoid cystic carcinoma to the skull base. Arch Otolaryngol Head Neck Surg. 2007;133:541–545. doi: 10.1001/archotol.133.6.541. [DOI] [PubMed] [Google Scholar]
- 10.Minn AY, Lyden ER, Anderson JR, et al. Early treatment failure in intermediate-risk rhabdomyosarcoma: results from IRS-IV and D9803--a report from the Children’s Oncology Group. J Clin Oncol. 2010;28:4228–4232. doi: 10.1200/JCO.2010.29.0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douglas JG, Arndt CA, Hawkins DS. Delayed radiotherapy following dose intensive chemotherapy for parameningeal rhabdomyosarcoma (PM-RMS) of childhood. Eur J Cancer. 2007;43:1045–1050. doi: 10.1016/j.ejca.2007.01.033. [DOI] [PubMed] [Google Scholar]