Abstract
Purpose
To provide guidelines for the selection of an initial contact lens (CL) power based on the preoperative characteristics of the patient in eyes undergoing infantile cataract surgery without primary intraocular lens (IOL) implantation.
Design
Cohort study.
Participants
Eyes were included if cataract surgery was performed without primary IOL implantation before 1 year of age, a SilSoft CL (Bausch & Lomb, Rochester, NY) was placed immediately after surgery, and postoperative refraction data were available within 1 month after surgery.
Methods
The target CL power was calculated by using the postoperative refraction at the corneal plane for each eye. A regression formula was derived using the targeted CL power and the axial length (AL). The CL power also was estimated using various formulas. An A-constant was derived to estimate CL power using IOL power calculation formula.
Main Outcome Measures
Contact lens power.
Results
Fifty eyes of 50 patients were analyzed. Age at the time of cataract surgery was 2.4±1.7 months. Refraction at the corneal plane was 29.6±4.4 diopters (D). Regression analysis revealed that CL power = 84.4 − 3.2 × AL (R2 = 0.82; P<0.001). Contact lens power can be estimated using an A-constant of 112.176 in the IOL power calculation formula. If a CL power of 32 D had been used, 22 (44%) of 50 eyes would have needed a replacement of CL.
Conclusions
We devised guidelines on selecting the initial CL power based on preoperative AL. The IOL power calculator also can help to estimate CL power. Refraction at the conclusion of surgery in infants may be difficult, and preoperative biometry can be used to estimate CL power.
The authors of the 1-year outcome report from the Infant Aphakia Treatment Study (IATS) advised caution when considering intraocular lens (IOL) implantation in infants given the high incidence of adverse events and the absence of an improved short-term visual outcome as compared with contact lens (CL) usage.1 When a primary IOL is not implanted, residual aphakia should be treated using either aphakic glasses or CL. Aphakic glasses can be used for the correction of bilateral aphakia. However, aphakic glasses required for infants generally are very heavy and difficult to wear. In addition, they are not suitable for eyes with unilateral aphakia. To treat infantile aphakia, most physicians prefer to insert either a silicone CL (SilSoft; Bausch & Lomb, Rochester, NY) or a rigid gas permeable CL. Silicone elastomer lenses often are used because of their comfort and handling attributes. Many physicians insert a silicone CL immediately at the end of cataract surgery under general anesthesia, or they insert the lens in the first 1 to 2 weeks after surgery. Early CL insertion also helps with immediate visual rehabilitation, which is imperative for amblyopia management in infantile aphakic eyes.
When faced with the challenges of fitting a CL on the eye of an infant with postsurgical aphakia resulting from the removal of infantile cataract, the problem of power choice arises. As a rule, infants operated for cataracts can be fit with a 7.5-base curve (BC) SilSoft CL. The Super Plus SilSoft series offers a power range from +32 diopters (D) down to +20 D in 3-D steps (32, 29, 26, 23, and 20 D). Adjustments to BC can be made using a fluorescein staining pattern, but rarely is this necessary. As the cornea flattens in the second year of life, most children are transitioned to a 7.7 BC. Compared with the BC, where little variability exists, lens power is more difficult to predict. Because it is difficult to obtain an accurate refraction immediately after surgery, the tendency is to insert a CL of power +32 D (the highest available power in the SilSoft Super Plus series). The IATS study protocol dictates that if an accurate refraction could not be obtained initially, a +32-D CL should be dispensed, and the lens power subsequently should be refined at the earliest opportunity.1 We noted that the CL power frequently needed to be changed (sometime within 1 week after cataract surgery) because of high refraction over the CL. This prompted us to evaluate whether we can more accurately estimate the power of CL based on certain preoperative characteristics. The purpose of this study was to provide pediatric cataract surgeons with suggested powers for the initial CL based on the preoperative characteristics of the patients. We hope that instead of using a CL of power +32 D, these guidelines will provide better aphakic correction and will decrease the need for changing the CL because of high refraction over the initial CL.
Patients and Methods
Charts were reviewed for all children who had undergone cataract surgery during their first year of life without primary IOL implantation. The submission received institutional review board approval from Medical University of South Carolina. Eyes with associated ocular pathologic features (ectopia lentis, Peters anomaly) were excluded. One eye was selected at random for evaluation in bilateral cases. Eyes were included if a SilSoft CL was placed immediately after cataract surgery and postoperative refraction data were available within 1 month after surgery. For bilateral cataract surgery, occasionally refraction was performed under general anesthesia at the time of cataract surgery in the fellow eye. All initial CL in this study were SilSoft Super Plus silicone with a base curve of 7.5 mm and a diameter of 11.3 mm. For each patient, age at surgery, gender, and ethnicity data were collected. In addition, preoperative axial length (AL), keratometry, corneal diameter, laterality of cataract, right eye or left eye, CL power used, duration between cataract surgery and refraction, and postoperative refraction data were collected. The CL power targeted for each eye was calculated by using postoperative refraction at the corneal plane for each eye. When refraction was performed over the CL, it was converted into a corneal plane adjusting for a vertex distance. Regression analysis was performed using the postoperative refraction at the corneal plane as a dependent variable.
Later, CL power was estimated by using various formulas: (1) regression analysis, (2) focal length formula (F = n/d, where F is total power, n = 1.336, and d is radius of curvature),2 (3) formulas described by McClatchey and Parks,3 (4) estimated aphakic refraction (80.4 − 1.65 × AL − 0.7 × keratometry), (5) Holladay 1, (6) Hoffer Q, and (7) Sanders-Retzlaff-Kraff/T (SRK/T). For the last 3 formulas, we used the Holladay consultant software. First, we inputted all the parameters with IOL power implanted as 0 and using the manufacturer's suggested surgeon factor. This allowed us to calculate a personalized A constant. Then, we re-entered this personalized A-constant in place of the manufacturer's surgeon factor, in the Holladay consultant software, and arrived at an estimated power using each formula. We use this as the estimated CL power for each formula.
Results
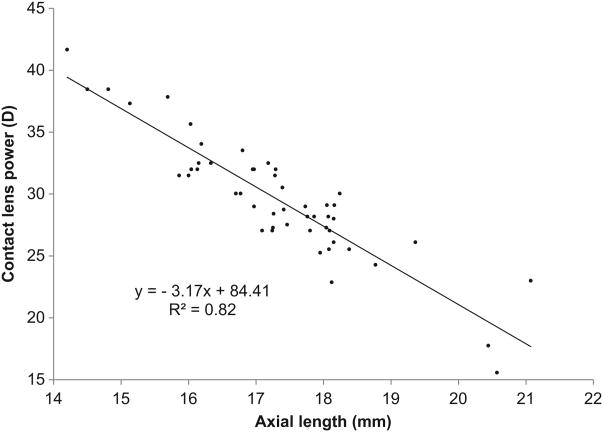
Data from 50 eyes of 50 patients were available for analysis. Thirty-four eyes underwent refraction over CL in a clinic, whereas 16 eyes underwent refraction under general anesthesia. The results are listed in Table 1. Regression analysis showed that CL power = 84.4 − 3 2 × AL (P<0.001; R2 = 0.82; Fig 1). Neither the histogram nor the P-P plot indicates that the normality assumption is violated. The IOL power for emmetropia showed a significant linear relationship (P<0.001; R2 = 0.60). However, it did not contribute to a model already containing AL (P = 0.9). The preoperative keratometry value also demonstrated a significant linear relationship with the required power of CL (P = 0.008; R2 = 0.138). However, it did not contribute significantly to a model already containing AL (P = 0.707). Similarly, age at the time of surgery also demonstrated a significant linear relationship (P<0.001; R2 = 0.231). However, it did not add to a model containing AL (P = −0.97). The follow-up duration did not show a significant linear relationship (P = 0.3; R2 = 0.02).
Table 1. Baseline Characteristics.
| Age at surgery (mos) | |
| Mean ± SD | 2.4±1.7 |
| Range | 0.2–7.7 |
| Gender (female/male) | 30/20 |
| Ethnicity | |
| Black | 10 |
| White | 38 |
| Asian | 1 |
| Hispanic | 1 |
| Preoperative axial length (mm) | |
| Mean ± SD | 17.3±1.4 |
| Range | 14.2–21.1 |
| Preoperative keratometry (D) | |
| Mean ± SD | 47.8±3.6 |
| Range | 42.5–63.5 |
| Preoperative corneal diameter (mm) | |
| Mean ± SD | 10.1±0.7 |
| Range | 8.5–11.5 |
| Laterality | |
| Unilateral | 20 |
| Bilateral | 30 |
| Right eye/left eye | 27/23 |
| CL power used (D) | |
| 32 | 30 |
| 29 | 16 |
| 26 | 2 |
| 23 | 1 |
| 18 | 1 |
| Follow-up (days) | |
| Mean ± SD | 11.9±10.2 |
| Range | 1–30 |
| Refraction over CL (D as SE) | |
| Mean ± SD | −0.1±4.0 |
| Range | −13 to +11 |
| CL refraction (D) | |
| Mean ± SD | 29.6±4.8 |
| Range | 15.6–41.7 |
| CL required (including +2 D near focus) | |
| Mean ± SD | 31.6±4.8 |
| Range | 17.6–43.7 |
CL = contact lens; D = diopter; SD = standard deviation; SE = spherical equivalent.
Figure 1.
Scatterplot illustrating preoperative axial length on the x-axis and contact lens power on the y-axis. D = diopter.
By inputting the parameters in the Holladay consultant software, we arrived at an A-constant of 112.176. Refraction at the corneal plane or estimated CL power was 29.6±4.4 D. The required CL power (including +2 for a near focus) was less than 30.5 D in 22 eyes. Table 2 shows the correlation between targeted CL power and estimated CL power using various formulas. Table 3 shows the prediction error and the absolute prediction error for the same.
Table 2. Estimation of Contact Lens Power.
| Formula* | Power | Correlation | P Value |
|---|---|---|---|
| Regression | 30.0±4.4 | 0.90 | <0.001 |
| Hug | 29.8±5.8 | 0.75 | <0.001 |
| Aphakic glasses | 23.7± 4.4 | 0.42 | 0.002 |
| McClatchey | 30.9±5.9 | 0.76 | <0.001 |
| Holladay 1 | 29.5±5.0 | 0.71 | <0.001 |
| Hoffer Q | 30.1±5.9 | 0.86 | <0.001 |
| SRK/T | 29.0±4.6 | 0.79 | <0.001 |
SRK/T = Sanders-Retzlaff-Kraff/T.
Note that refraction at corneal plane was 29.6±4.4 diopters.
Table 3. Prediction Error and Absolute Prediction Error.
| Formula | Prediction Error | Absolute Prediction Error |
|---|---|---|
| Regression | −0.4±2.0 | 1.7±1.1 |
| Hug | −0.3±3.9 | 3.0±2.4 |
| Aphakic glasses | 5.8±4.9 | 6.2±4.5 |
| McClatchey | −1.3±3.9 | 3.3±2.4 |
| Holladay 1 | 0.1±3.7 | 2.7±2.6 |
| Hoffer Q | −0.5±3.1 | 2.5±1.8 |
| SRK/T | 0.5±3.1 | 2.3±2.1 |
SRK/T = Sanders-Retzlaff-Kraff/T.
Discussion
The silicone elastomer CL is currently the first choice of many practitioners for pediatric aphakia. It is easy to fit and can be used as an extended-wear CL. This study attempted to provide a guide to CL correction in pediatric aphakia within the parameters currently available for the Bausch & Lomb SilSoft Silicone Elastomer Lens. SilSoft Super Plus pediatric lenses are available from 20 to 32 D in 3-D steps (for lower power, the aphakic series is available as 11.5 to 20 D in 0.5-D steps). The data from our study showed that CL power = 84.4 − 3.2 × AL (P<0.001; R2 = 0.82). The significance of the F statistic is less than 0.001, which means that the variation explained by the model is not the result of chance. The coefficient of determination, R2, is the squared value of the multiple correlation coefficient. It shows that this model explains approximately 82% of the variation in CL power. This model suggests change of 3.2 D per 1 mm of AL. The preoperative AL helps in planning the CL power to be used. Using linear regression, we made use of the relationship between AL and CL power for future patients undergoing cataract surgery. Martin et al4 provided regression analysis based on age (CL = 30.28−0.3554 age in months; R = 0.96). Within the CL parameters available, the authors indicated the following silicone elastomer lens powers for the corresponding ages: 0 to 6 months, +29 D; 7 to 17 months, +26 D; 18 to 28 months, +23 D; and 29 to 34 months, +18 D.5 Moore noted that the mean spherical equivalent refractive error for these patients was +28.5 D at 6 months, +26.5 D at 12 months, +23 D at 24 months, and +21.5 D at 36 months.6
The estimated CL power based on the regression formula was 30±4.4 D (correlation, 0.90). However, use of this regression formula can be criticized unless we validate the regression formula in future studies using a different dataset. Further prospective studies are planned using the regression formula derived in this study and applying it to data from the IATS. Using the Holladay 1, Hoffer Q, and SRK/T formulas, the correlation was 0.71, 0.86, and 0.79, respectively. We hope to continue our data collection with a larger sample size and to provide better predictability using the IOL power calculator for the estimation of CL power. A new CL generally is prescribed when the residual refractive error is more than 3 D. The CL power required (including +2 for near focus) was less than 30.5 D in 22 eyes. This suggests that if we had used +32 D as the initial CL power, 44% of eyes would have required a change in CL. Refraction over CL was ranging from −13 D to +11 D, and based on this wide range, the CL needed replacement within 1 day to 1 week after initial insertion. Inappropriate aphakic correction could be amblyogenic. In addition, the average cost of a silicone elastomer CL is $150/unit. Replacement costs resulting from an incorrect estimation of CL power can be decreased by using the results provided in this study.
Aphakic infants are unable to accommodate. They are, akin to other infants, more likely to be interested in objects that are close to them such as faces and toys.7 Consequently, they should be overcorrected to focus vision on a near viewing point and to account for their so-called near world.8,9 Various studies have used an addition of +4 to +2 D. Addition is usually decreased gradually with increasing age. The IATS design reads that within 1 week after surgery, patients in the CL group were fitted with a silicone, SilSoft CL, or rigid gas permeable CL with a +2-D overcorrection to provide a near-point correction. If an accurate refraction could not be obtained initially, a +32-D CL was dispensed, and the lens power subsequently was refined at the earliest opportunity. At 2 years of age, the eye was corrected for emmetropia, and bifocal glasses were added for near viewing.1 Considering an approximate overcorrection of +2 D and the availability of SilSoft CL powers, we recommend a 32-D CL when the preoperative AL was less than 17 mm, a 29-D Cl when the preoperative AL was between 17 and 18.5 mm, a 26-D CL when the preoperative AL was 18.5 to 19.5 D, a 23-D CL when the preoperative AL was between 19.5 and 20 mm (21 mm), and a 20-D CL for an AL of 20 to 21 mm (20 D for >21 mm). These power suggestions are a starting point before the necessary retinoscopic overrefraction. When the CL power falls between available powers (SilSoft Super Plus lenses are available in 3-D steps), customized decision should be made by the physician. For example, what if an eye requires 30.5 D? A +32-D CL can be chosen because the infant's visual needs are mostly at near. However, a +29-D CL can be chosen if the CL will be replaced in the near future because it is likely that the eye will grow very fast in this age group and soon this eye will require a +29-D CL.
Some physicians may not prefer to insert a CL immediately at the end of surgery and may consider prescribing a CL after a clinical evaluation. de Brabander et al10 reported that the CL was inserted at an average of 2.4 weeks after surgery. When fitting infant eyes with CLs, it may not always be possible to obtain accurate measurements of refraction. The results of our study can guide those physicians to select an appropriate CL power.
The results of our study may not be applied to other types of CLs or other age groups. We did not have many eyes with a higher AL. We measured overrefraction under general anesthesia for some eyes. General anesthesia will bring about a reduction in intraocular pressure, which can affect the corneal topography. Therefore, the corneal curvature and refractive error determined under anesthesia can be different from those obtained when the infant is awake.6 Despite these limitations, our study has important implications. Based on the results of this study, we do not advocate the practice of inserting a standard +32-D CL. We recommend either using the regression analysis model provided in this study for an estimation of CL power or the use of the formula for IOL power calculation with an A-constant of 112.176, which provides a good correlation of CL estimation.
Acknowledgments
Supported in part by the Grady Lyman Fund, MUSC Health Science foundation; the National Institutes of Health, Bethesda, Maryland (grant no.: EY-14793); and an unrestricted grant to the Storm Eye Institute, Medical University of South Carolina, from Research to Prevent Blindness, Inc, New York, New York.
Footnotes
Financial Disclosure(s): The author(s) have no proprietary or commercial interest in any materials discussed in this article.
References
- 1.Infant Aphakia Treatment Study Group. The Infant Aphakia Treatment Study: design and clinical measures at enrollment. Arch Ophthalmol. 2010;128:21–7. doi: 10.1001/archophthalmol.2009.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hug T. Use of the aphakic refraction in intraocular lens (IOL) power calculations for secondary IOLs in pediatric patients. J Pediatr Ophthalmol Strabismus. 2004;41:209–11. doi: 10.3928/0191-3913-20040701-07. [DOI] [PubMed] [Google Scholar]
- 3.McClatchey SK, Parks MM. Myopic shift after cataract removal in childhood. J Pediatr Ophthalmol Strabismus. 1997;34:88–95. doi: 10.3928/0191-3913-19970301-07. [DOI] [PubMed] [Google Scholar]
- 4.Martin NF, Kracher GP, Stark WJ, Maumenee AE. Extended-wear soft contact lenses for aphakic correction. Arch Ophthalmol. 1983;101:39–41. doi: 10.1001/archopht.1983.01040010041003. [DOI] [PubMed] [Google Scholar]
- 5.Lightman JM, Marshall D., Jr Clinical evaluation of back optic radius and power determination by age in pediatric aphakia due to congenital cataract fitted with a Silicone Elaster contact lens. Optom Vis Sci. 1996;73:22–7. doi: 10.1097/00006324-199601000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Moore BD. Contact lens problems and management in infants, toddlers, and preschool children. Probl Optom. 1990;2:365–93. [Google Scholar]
- 7.Lindsay RG, Chi JT. Contact lens management of infantile aphakia. Clin Exp Optom. 2010;93:3–14. doi: 10.1111/j.1444-0938.2009.00447.x. [DOI] [PubMed] [Google Scholar]
- 8.Aasuri MK, Venkata N, Preetam P, Rao NT. Management of pediatric aphakia with SilSoft contact lenses. CLAO J. 1999;25:209–12. [PubMed] [Google Scholar]
- 9.Friendly DS, Oldt NW. Contact lenses for aphakic children. Int Ophthalmol Clin. 1977;17:205–19. [PubMed] [Google Scholar]
- 10.de Brabander J, Kok JH, Nuijts RM, Wenniger-Prick LJ. A practical approach to and long-term results of fitting silicone contact lenses in aphakic children after congenital cataract. CLAO J. 2002;28:31–5. [PubMed] [Google Scholar]