Abstract
Background
Pulmonary mycobacterial diseases describe both tuberculosis (TB) and nontuberculous mycobacteria (NTM). Few data are available measuring the cost burden of mycobacterial diseases at the national level. The purpose of this study is to evaluate the cost burden and measure emerging trends in hospitalization of pulmonary TB and NTM cases in the United States from 2001 through 2012.
Methods
This study is a retrospective, community-based cost analysis of hospitalized patients with a principal diagnosis of pulmonary mycobacterial diseases from 2001 through 2012. Data for pulmonary TB and NTM were retrieved from the Healthcare Cost and Utilization Project (HCUP), US Department of Health and Human Services. The statistical significance of observed trends of NTM and TB national hospital costs was calculated using Poisson log-linear regression.
Results
20,049 hospital discharges were reported for pulmonary NTM and 69,257 for pulmonary TB in the US from 2001 through 2012. The total associated cost of these discharges was $903,767,292 for pulmonary NTM and $2,078,113,317 for pulmonary TB. During the study period, the national hospital costs of pulmonary NTM increased at a statistically significant rate in the US over each year (P = 0.001). However, no such increase was found for national hospital costs of pulmonary TB.
Conclusions
The national hospital cost of NTM management is increasing. These results emphasize the importance of continued research in pulmonary NTM in order to improve current guidelines in prevention and treatment strategies.
Keywords: Nontuberculous mycobacteria, Tuberculosis, Healthcare costs
Introduction
Pulmonary mycobacterial diseases describe both tuberculosis (TB) and nontuberculous mycobacteria (NTM). Pulmonary mycobacterial disease has been a long-term public health problemin the US and all over the world. TB incidence peaked in the early twentieth century in the US, when it became a major cause of mortality [1].
While efforts in treatment and surveillance of TB have resulted in a decrease in its incidence in recent years [2], the incidence of NTM is increasing and has been classified as an emerging public health problem in the US [3] and the world [4,5]. The incidence of NTM has even surpassed that of TB in several States of the US [6,7].
NTM are organisms that are found ubiquitously in the environment. In the 1950s, NTM was first recognized as human pathogens when 1–2% of various sanitarium’s patients did not respond to routine anti-TB regimens [5,8]. Currently, over 150 NTM species are known, and many new species with clinical relevance have recently been reported [9].
Unlike TB, diseases caused by NTM generally have pro-longed treatment for complete cure. Therefore, the prevalence is far greater than the incidence, and cost of treatment is more dependent on prevalence than incidence.
Healthcare costs have been key factors in national economies, and controlling healthcare costs has become a priority for essentially all countries in the world and is an important area of research. Healthcare costs associated with mycobacterial disease lie more heavily on public healthcare systems because of the communicable nature of TB. The healthcare costs of tuberculosis have been reported several times; the average cost for hospitalization of non-drug-resistant TB was estimated to be $28,000 per patient in 2005–2007 [10]. The hospital costs of managing patients with NTM disease are less clear. A limited amount of data are available measuring the healthcare costs of NTM at the national level. Previously published studies have attempted to measure various aspects of cost, but have done so using small sample sizes or with a limited study period [10–12]. The purpose of this study is to offer a comprehensive evaluation of the in-hospital costs of care for pulmonary TB and NTM using national data during a long study period beginning in 2001 up through 2012.
Methods
Study design and patient data
This is a retrospective, population-based comparative study using data obtained from the National Inpatient Sample (NIS) within the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project (HUCP). NIS is the largest inpatient healthcare dataset in the US providing national estimates of hospital costs stratified by disease State. NIS collects data from every State participating in HCUP, which represents more than 95% of the US population [13]. All patients with a principal diagnosis of pulmonary NTM and TB who were discharged from the hospital during the period 2001 through 2012 were included in this study.
Study definitions
Pulmonary NTM was defined by any hospital discharge associated with a principal diagnosis of the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9) code 031.0. This code includes pulmonary infection by mycobacterium avium, mycobacterium intracellulare and mycobacterium kansasii. Pulmonary TB was defined by any discharge associated with ICD-9 codes 011.90–011.96. The principal diagnosis was defined as the main reason for discharge. The regions of the US were classified into four zones recognized by the Bureau of the Census as Northeast, Midwest, South and West (Table 1). Length of stay was defined as the number of nights the patient remained in the hospital. Payer was defined by the type of insurance coverage carried by the patient or lack thereof, which included Medicare, Medicaid, private insurance (Blue Cross, commercial carriers, and private HMOs and PPOs), uninsured (which includes an insurance status of “self-pay” and “no charge”), and other (which includes Worker’s Compensation and other government payers). Median income was defined as the median household income of the patient’s zip code of residence and compared with the national median income for the same year. HCUPnet used value ranges of the median household income itemized by year (Table 2) [14].
Table 1.
The regions of the US were classified into four zones recognized by the Bureau of the Census.
| Northeast | Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont |
| Midwest | Illinois, Indiana, Iowa, Kansas, Minnesota, Missouri, Michigan, Nebraska, North Dakota, Ohio, South Dakota and Wisconsin |
| South | Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Maryland, Mississippi, Louisiana, Tennessee, North Carolina, Oklahoma, South Carolina, Texas, Virginia, and West Virginia |
| West | Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming |
Table 2.
Each year value ranges for calculation of median income of patients’ ZIP code.
| Year | Low | Not low |
|---|---|---|
| 2003 | $1–35,999 | $36,000+ |
| 2004 | $1–35,999 | $36,000+ |
| 2005 | $1–36,999 | $37,000+ |
| 2006 | $1–37,999 | $38,000+ |
| 2007 | $1–38,999 | $39,000+ |
| 2008 | $1–38,999 | $39,000+ |
| 2009 | $1–39,999 | $40,000+ |
| 2010 | $1–40,999 | $41,000+ |
| 2011 | $1–38,999 | $39,000+ |
| 2012 | $1–38,999 | $39,000+ |
Adapted form: Ref. [14].
Study variables
Variables included in this study were age group, sex, region, payer, median zip code, hospital length of stay in days, mean hospital charge per discharge, mean aggregated charge, total aggregated charge, and in-hospital deaths.
Statistical analysis
The statistical significance of observed trends of NTM and TB national hospital costs were calculated using Poisson log-linear regression. National hospital costs for NTM and TB were projected in relation to healthcare inflation for each year. Expected mean aggregated charge (EaC) was calculated based on healthcare inflation using the equation: (EaC = HCi × OaC), in which EaC is the expected aggregated hospital charge, Hci is healthcare inflation percent for each year (Hci = total aggregated hospital charge for a specific year divided by the total aggregated hospital charge for the prior year × 100), and OaC is the observed aggregated charge for each medical condition. A regression model was applied to test the correlation between observed and projected aggregated hospital charges, otherwise known as national hospital costs. All statistical analyses were performed using SPSS statistical software (version 21.0, IBM Corporation).
Results
From a total of 36,484,846 discharges, 20,049 hospital discharges were reported with pulmonary NTM and 44,370 with pulmonary TB in the US from 2001 through 2012.
Age distribution varied between the two groups (Table 3). The majority of pulmonary NTM patients were between 65– 84 years old (48.5%), while 70% of TB patients were younger than 65. There was a significant difference between frequencies of subjects more than 65 years old between the two groups (P = 0.0001). There was a significant difference between frequencies of the very elderly (+85) population between the two groups (P < 0.00001, OR = 2.83). Pulmonary NTM was 2.6 times higher in females than pulmonary TB (P < 0.00001).
Table 3.
The demographic characteristics of patients with pulmonary nontuberculous mycobacterial diseases and tuberculosis in the US from 2001 to 2012.
| Variables | NTM | TB | |
|---|---|---|---|
| All discharges | 20,049 | 44,370 | |
| Age group (%) | <17 | 1.8 | 5.1 |
| 18–44 | 7.6 | 36.3 | |
| 45–64 | 31.3 | 33.8 | |
| 65–84 | 48.5 | 20.7 | |
| >85 | 10.8 | 4.1 | |
| Sex (%) | Male | 44 | 67 |
| Female | 56 | 33 | |
| Region (%) | Northwest | 19 | 21 |
| Midwest | 16 | 13 | |
| South | 43 | 43 | |
| West | 22 | 23 | |
| Payer (%) | Medicare | 61 | 24 |
| Medicaid | 10 | 23 | |
| Private insurance | 22 | 19 | |
| Uninsured | 5 | 25 | |
| Other | 2 | 9 | |
| Median income for zip code (%) | Low | 26 | 41 |
| Not low | 72 | 55 | |
| Missing | 2 | 3 | |
| Length of stay per days (SD) | 9.2 (0.5) | 13.5 (1.5) | |
| Mean hospital charge per discharge ($) | 47,120 | 48,332 | |
| Mean aggregated charge ($) | 80,886,935 | 246,398,995 | |
| Expected mean aggregated charge ($) | 85,005,570 | 282,501,149 | |
| Total aggregated charge ($) | 903,767,292 | 2,078,113,317 | |
| In-hospital deaths (mean/year) | 71 (0.35) | 114 (0.26) |
Note: $: US dollar.
The incidence of pulmonary mycobacterial disease did not vary between TB and NTM by geographical area. The south region recorded the highest numbers of hospital discharges for both in the US.
There was a significant difference in one payer status between the TB and NTM group. Medicare paid 60% of pulmonary NTM inpatient costs, but only 24% of the hospital costs of subjects with pulmonary TB (P < 0.00001). There was no difference in the other payer groups for NTM and TB.
Patients with pulmonary NTM had a higher economic status than patients with TB, based on zip code analysis. Only 26% of pulmonary NTM patients had a household income less than their community, as compared with 41% for patients with pulmonary TB (P = 0.0246, OR = 0.51). TB patients had a longer hospital stay compared with NTM patients–TB averaging 13 days vs. 9 days for NTM.
The total associated costs of a hospital stay for all conditions during the study duration was $1,337,939,745,325, an estimated $903,767,292 of which was directly associated with pulmonary NTM and $2,078,113,317 with pulmonary TB. The national hospital costs of pulmonary NTM increased at a statistically significant rate in the US over each year (P = 0.001) (Fig. 1). A linear regression analysis demonstrated a high degree of correlation between NTM observed and projected national hospital costs (R = 0.938, P < 0.001) (Fig. 2). However, no such correlation between observed and projected national hospital costs was found for pulmonary TB (R = 0.284, P = 0.372).
Fig. 1.
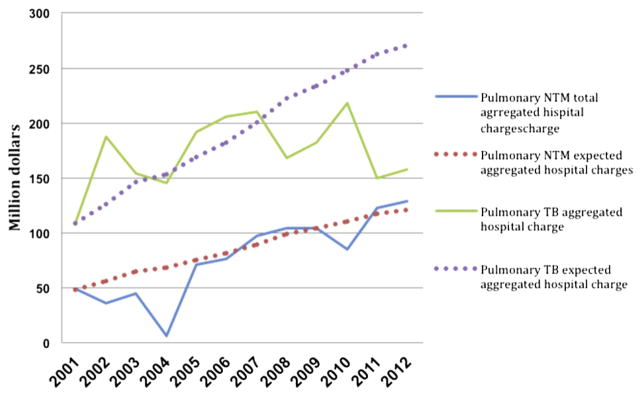
The trends of observed and projected national hospital costs of pulmonary nontuberculous mycobacterial and tuberculosis disease in the US from 2001 to 2012.
Fig. 2.
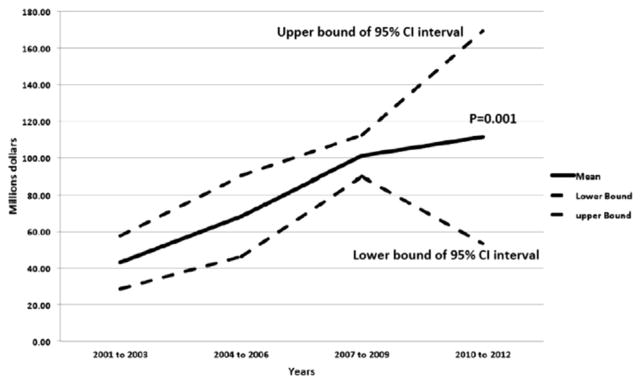
The trends of national hospital costs of pulmonary nontuberculous mycobacterial disease in the US from 2001 to 2012.
Discussion
This study showed that the cost burden for inpatient care of patients with pulmonary mycobacterial diseases in the US was around 3 billion dollars from 2001 through 2012. The aggregated hospital charges for pulmonary NTM had an increasing trend that was in the same trajectory with the health care inflation. However, pulmonary TB inpatient costs were not increasing at the same trend as the trajectory of healthcare cost inflation.
A number of studies attempted to measure outpatient pulmonary NTM-related costs. A small cohort study with 27 pulmonary NTM subjects in a US-based center found an annual antibiotic therapy cost of $5,196 for those infected with MAC and $11,796 for M. abscessus [11]. Also emphasized in this study, the NTM species was a major factor in determining antibiotic cost. For instance M. abscessus was particularly associated with higher treatment cost. Leber and Marras studied 117 individuals with pulmonary NTM to determine outpatient treatment costs in Canada [12]. They found that the annual cost was $5,000 in Canadian currency and antibiotics were responsible for 70% of the cost.
In this study, the hospital costs of pulmonary mycobacterial disease were measured, but the full economic burden of mycobacterial disease is impossible to measure. In addition to the cost of delivering direct medical care in the inpatient and outpatient setting, total cost involves many other financial and human costs, such as lost wages, travel expenses and opportunity costs of the sick, the cost to administer public health programs including surveillance and prevention, and the economic impact on the family and social network of those receiving care for the disease which may also include lost wages, travel expenses and opportunity costs. This study was only able to ascertain the inpatient costs.
Compared to patients with TB, patients with nontuberculous mycobacteria were more often women. They were older and came from areas with higher incomes, which has been found in other studies [3,15,16]. In a population-based study, it was recently shown that females die more frequently from NTM, and the majority (78%) of NTM-related mortality occurs in the patients 55 years of age or older [17]. This is particularly important in the US, considering the aging of the baby boomer population cohort (those born between the years 1945 and 1960), which has impacted population distribution resulting in significantly more elderly people than young and middle-aged in the US.
Adjemian and colleagues showed a relationship between counties in the United States with a higher median household income with the geographical distribution of pulmonary NTM [18]. The data in the present study support their findings in a population-based study.
The major limitation of this study was the use of ICD-9 codes. ICD-9 has limited codes for NTM, which includes only the more common species M. avium complex and M. Kansasii. With more than 150 currently reported species of NTM, this cost assessment only included the most common NTM species associated with pulmonary disease.
Conclusion
Pulmonary mycobacterial diseases are the source of an immeasurable and significant economic burden. This study supports previous data classifying NTM as an emerging disease with increasing incidence and cost. Also, the strong correlation between NTM and the elderly is likewise concerning given the population structure of the US. As the large number of baby boomers enter their final years, the incidence of NTM is likely to demonstrate amplified increases, which could have a profound impact on healthcare costs. More research is needed to understand the total inpatient and out-patient NTM costs and forecasting of future trends based on disease surveillance relative to population distribution.
Acknowledgments
Funding resources
This study was supported by NIH Grant 5 T32 HL 82547-7.
Abbreviations
- TB
tuberculosis
- NTM
nontuberculous mycobacteria
- HCUP
Healthcare Cost and Utilization Project
- NIS
National Inpatient Sample
- US
The United States
- OR
Odds ratio
- ICD-9
International Classification of Diseases, 9th Revision, Clinical Modification
- HMO
Health Maintenance Organization
- PPO
Preferred Provider Organization
Footnotes
Preliminary data generated from this study will be presented in the first Asian-African Mycobacteriology Society meeting, 2015.
Author contributions
Conception, review literature, design and modeling for review writing manuscript: M.M. The review literature, design and modeling for review writing manuscript: M.M., G.E, Writing the article or substantial involvement in its revision before submission: M.M, M.B.A., G.E., D.S.
Conflict of interest statements
All authors have no conflicts of interest to disclose.
Peer review under responsibility of Asian African Society for Mycobacteriology.
References
- 1.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. JAMA, J Am Med Assoc. 1999;281(1):61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 2.Lobato MN, Wang YC, Becerra JE, Simone PM, Castro KG. Improved program activities are associated with decreasing tuberculosis incidence in the United States. Public Health Rep. 2006;121(2):108–115. doi: 10.1177/003335490612100202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirsaeidi M, Farshidpour M, Ebrahimi G, Aliberti S, Falkinham JO., 3rd Management of nontuberculous mycobacterial infection in the elderly. Eur J Int Med. 2014;25(4):356–363. doi: 10.1016/j.ejim.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marras TK, Daley CL. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. 2002;23(3):553–567. doi: 10.1016/s0272-5231(02)00019-9. [DOI] [PubMed] [Google Scholar]
- 5.Velayati AA, Farnia P, Mozafari M, Malekshahian D, Seif S, et al. Molecular epidemiology of nontuberculous mycobacteria isolates from clinical and environmental sources of ametropolitan city. PLoS ONE. 2014;9(12):e114428. doi: 10.1371/journal.pone.0114428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan K, Wang J, Marras TK. Nontuberculous mycobacterial sensitization in the United States: national trends over three decades. Am J Respir Crit Care Med. 2007;176(3):306–313. doi: 10.1164/rccm.200702-201OC. [DOI] [PubMed] [Google Scholar]
- 7.Kendall BA, Varley CD, Choi D, Cassidy PM, Hedberg K, et al. Distinguishing tuberculosis from nontuberculous mycobacteria lung disease, Oregon, USA. Emerg Infect Dis. 2011;17(3):506–509. doi: 10.3201/eid1703.101164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masson AM, Prissick FH. Cervical lymphadenitis in children caused by chromogenic Mycobacteria. Can Med Assoc J. 1956;75(10):798–803. [PMC free article] [PubMed] [Google Scholar]
- 9.Tortoli E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev. 2014;27(4):727–752. doi: 10.1128/CMR.00035-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marks SM, Flood J, Seaworth B, Hirsch-Moverman Y, Armstrong L, Mase S, et al. Treatment practices, outcomes, and costs of multidrug-resistant and extensively drug-resistant tuberculosis, United States, 2005–2007. Emerg Infect Dis. 2014;20(5):812–821. doi: 10.3201/eid2005.131037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ballarino GJ, Olivier KN, Claypool RJ, Holland SM, Prevots DR. Pulmonary nontuberculous mycobacterial infections: antibiotic treatment and associated costs. Respir Med. 2009;103(10):1448–1455. doi: 10.1016/j.rmed.2009.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leber A, Marras TK. The cost of medical management of pulmonary nontuberculous mycobacterial disease in Ontario. Canada, Eur Respir J. 2011;37(5):1158–1165. doi: 10.1183/09031936.00055010. [DOI] [PubMed] [Google Scholar]
- 13. [Accessed on Jan 2, 2015]; < http://www.hcup-us.ahrq.gov/nisoverview.jsp>.
- 14. [Accessed on Jan 2, 2015]; < http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=C73A51CC022179F8&Form=SelPAT&GoTo=ZIPinc&JS=Y&DefId=>.
- 15.Mirsaeidi M, Farshidpour M, Allen MB, Ebrahimi G, Falkinham JO. Highlight on advances in nontuberculous mycobacterial disease in North America. BioMed Res Int. 2014 doi: 10.1155/2014/919474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomson RM. NTM working group at Queensland TB Control Centre, Queensland Mycobacterial Reference Laboratory. Changing epidemiology of pulmonary nontuberculous mycobacteria infections. Emerg Infect Dis. 2010;16(10):1576–1583. doi: 10.3201/eid1610.091201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mirsaeidi M, Machado RF, Garcia JG, Schraufnagel DE. Nontuberculous mycobacterial disease mortality in the United States, 1999–2010: a population-based comparative study. PLoS ONE. 2014;9(3):e91879. doi: 10.1371/journal.pone.0091879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adjemian J, Olivier KN, Seitz AE, Falkinham JO, 3rd, Holland SM, Prevots DR. Spatial clusters of nontuberculous mycobacterial lung disease in the United States. Am J Respir Crit Care Med. 2012;186(6):553–558. doi: 10.1164/rccm.201205-0913OC. [DOI] [PMC free article] [PubMed] [Google Scholar]


