Abstract
Objective
As the most important risk factors of cardiovascular disease, pre-hypertension and hypertension are important public health challenges. Few studies have focused on the trends of pre-hypertension and hypertension specifically for the aging population in China. Given the anticipated growth of the elderly population in China, there is an urgent need to document the conditions of pre-hypertension and hypertension in this aging population.
Methods
We conducted two cross-sectional surveys of Chinese adults aged ≥60 years in 2001 and 2010. A total of 2,272 (943 males, 1,329 females) and 2,074 (839 males, 1,235 females) participants were included in the two surveys, respectively.
Results
The age- and sex-standardized prevalence of hypertension significantly increased from 60.1% to 65.2% from the 2001 to the 2010 survey. Among the participants with hypertension, the awareness, treatment and control of hypertension all significantly increased from 69.8% to 74.5%, 50.3% to 63.7%, and 15.3% to 30.3%, respectively, from 2001 to 2010. A logistic regression showed that a higher education level, a higher BMI, a family history of hypertension and doctor-diagnosed cardiovascular disease were significantly associated with hypertension awareness and treatment.
Conclusion
Hypertension prevalence increased rapidly between the years surveyed. Although the awareness, treatment and control of hypertension improved significantly, the values of these variables remained low. More attention should be given to the elderly because the population is aging worldwide, and urgent action, optimal treatment approaches and proper public health strategies must be taken to prevent and manage hypertension.
Introduction
According to a WHO report, cardiovascular disease (CVD) is estimated to become the leading cause of morbidity and mortality worldwide by 2020 [1]. As the risk factors of CVD, pre-hypertension and hypertension are important public health challenges worldwide [2, 3]. Therefore, an effective strategy for preventing CVD requires increased prevention of hypertension along with timely diagnosis and appropriate treatment of hypertension [4].
A large number of studies have been conducted to evaluate the prevalence, awareness, treatment and control of hypertension among the Chinese [5–12], but data on recent trends of pre-hypertension and hypertension prevalence are rare in China [13–16]. In developed countries such as the US, studies have reported trends of hypertension prevalence, particularly for older US adults [17, 18]. However, few studies have focused on the trends of pre-hypertension and hypertension specifically for the aging population in urban areas of China. The aging population presents a serious challenge for China; individuals aged ≥60 and ≥80 years will constitute 29.7% and 7.6% of the total Chinese population by 2050, respectively [19]. Given the anticipated growth of the elderly population in China, there is an urgent need to document the conditions of pre-hypertension and hypertension in this population.
As the capital of China, Beijing is highly developed and urbanized. To explore the situation of pre-hypertension and hypertension among the aging population during the past decade of rapid development and change, the current study reported the prevalence of pre-hypertension and the prevalence, awareness, treatment and control of hypertension in participants aged ≥60 years in two cross-sectional surveys that were conducted in 2001 and 2010 in Beijing, China.
Methods
Study design
As described in our previous study [20], a two-stage stratified sampling method was conducted to recruit participants aged 60 years and older in the Wanshoulu Community within the Haidian District, a metropolitan area that was representative of the geographic and economic characteristics of Beijing in 2001. First, we used the randomized cluster sampling method to randomly select 9 of the 94 communities in the Wanshoulu Community. Second, all of the households with elderly residents were selected from the 9 communities, and one elderly resident from each household was selected. A total of 2,680 elderly individuals were selected and invited to participate in our survey. A total of 2,334 participants completed the survey (the response rate was 87.1%). After excluding 62 people with incomplete data, a total of 2,272 participants (943 males and 1,329 females) were included in our survey in 2001.
In 2010, we conducted a second cross-sectional survey in the same district using the same method as with the 2001 survey. In the second survey, 2,162 of 2,510 elderly participants completed the survey (the response rate was 86.1%). After excluding 88 people with incomplete data, a total of 2,074 participants (839 males and 1,235 females) were included in our 2010 survey. After the two surveys were completed, we found that a total of 731 participants (33%) were included in both surveys.
This study was approved by the Independent Ethics Committee of the Chinese People's Liberation Army General Hospital; signed informed consent was obtained from all the participants.
Data collection and measurement
Each participant completed a face-to-face interview and a standardized questionnaire on demographic characteristics such as age, gender, marital status, medical history, family history of chronic disease and lifestyle characteristics. Trained observers measured each participant’s height, weight, waist circumference and blood pressure according to the standardized protocol. Height was measured in meters (without shoes), and weight was measured in kilograms (heavy clothing was removed, and one kilogram was deducted for remaining garments). Waist circumference was measured midway between the lower rib margin and iliac crest while participants were in the standing position [21]. Cigarette smoking was defined as having smoked at least one cigarette per day for more than one year [22]. Alcohol consumption was defined as drinking alcohol at least 12 times during the past year [23]. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared [21]. The participants were stratified into the following four age groups: 60 to 64, 65 to 69, 70 to 74 and ≥75 years. Overnight fasting blood specimens were obtained for the measurement of serum lipids and glucose, and the samples were sent to the central certified laboratory of the Chinese PLA General Hospital within 30 minutes.
BP measurement and definitions
The participants were advised to avoid alcohol, cigarette smoking, coffee or tea and exercise prior to blood pressure measurement. Two measurements were obtained from the right arm using standardized mercury sphygmomanometers while participants were in a sitting position [24]. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were defined as the averages from the two readings. If the two measurements differed by over 10 mmHg, the observers measured the blood pressure a third time and calculated the average of the three measurements as the final measurement.
Based on the measured blood pressure, the participants were classified into the following three groups: optimal blood pressure, pre-hypertension, and hypertension. Optimal blood pressure was defined as a mean SBP <120 mmHg and DBP <80 mmHg. Pre-hypertension was defined as SBP ≥120 mmHg and <140 mmHg or DBP ≥80 mmHg and <90 mmHg. Hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg and/or the self-reported use of antihypertensive medication in the previous two weeks [25–27]. Among the participants who were defined as hypertensive in the review, awareness of hypertension was defined as any prior diagnosis of hypertension by a health care professional, treatment of hypertension was defined as use of prescribed antihypertensive medication within the previous two weeks, and control of hypertension was defined as an average SBP <140 mmHg and an average DBP <90 mmHg and was associated with pharmacological treatment of hypertension [28]. The Eighth Joint National Committee (JNC-8) proposed the treatment blood pressure goal of less than 150/90 mmHg among individuals aged 60 years or older [29]. We defined the control of hypertension as SBP <150 mmHg and/or DBP <90 mmHg in a subsequent sensitivity analysis.
Statistical analysis
The data were entered (double entry) using Epidata (3.1) and analyzed using SPSS (Inc., Chicago, IL, USA) for Windows (19.0). A two-sided P-value of <0.05 was considered statistically significant.
The prevalence of pre-hypertension and the prevalence, awareness, treatment and control of hypertension were standardized by age and sex. We weighted the survey data, and age- and sex-standardizations (both treated as the dichotomous variables) were performed based on the urban population distributions in Beijing in 2001 and 2010 [30]. The baseline characteristics were described using descriptive statistics, and t-tests and chi-square tests were used to examine differences in the continuous and categorical variables, respectively. Prevalence in the two surveys from 2001 and 2010 was compared using a chi-square test. A logistic regression was used to calculate the factors associated with the awareness, treatment and control of hypertension in the 2001 and 2010 surveys.
We conducted sensitivity analyses of subject characteristics and the prevalence, awareness, treatment and control of hypertension during 2001–2010 after excluding those individuals who were included in both surveys (n = 731).
Results
As shown in Table 1, a total of 2,272 (943 males and 1329 females) and 2,074 (839 males and 1235 females) participants completed the surveys in 2001 and 2010, respectively. The mean age of the participants was 67.92±5.76 years in 2001 and significantly increased to 71.69±6.56 years in 2010. The proportion of participants aged 75 and older had increased rapidly over the decade, which indicated the aging of the population. SBP and DBP also significantly increased from 137.14±21.27 mmHg to 138.93±19.78 mmHg and 77.03±10.52 mmHg to 77.30±9.93 mmHg, respectively, from 2001 to 2010.
Table 1. Characteristics of the subjects who completed the surveys in 2001 and 2010.
| Characteristics | 2001 (n = 2272) | 2010 (n = 2074) | P-value |
|---|---|---|---|
| Mean±SD | |||
| Age (year) | 67.92±5.76 | 71.69±6.56 | <0.001 |
| Height (m) | 1.61±0.08 | 1.60±0.08 | 0.388 |
| Weight (kg) | 66.70±10.85 | 64.39±10.80 | 0.771 |
| BMI (kg/m2) | 25.62±3.53 | 25.00±3.41 | 0.250 |
| Waist (cm) | 87.70±9.35 | 88.32±9.07 | 0.400 |
| Hip (cm) | 101.20±8.01 | 98.50±7.64 | 0.330 |
| SBP (mmHg) | 137.14±21.27 | 138.93±19.78 | <0.001 |
| DBP (mmHg) | 77.03±10.52 | 77.30±9.93 | 0.035 |
| TC (mmol/l) | 5.33±1.68 | 5.27±1.02 | 0.732 |
| TG (mmol/l) | 1.55±1.05 | 1.67±0.93 | 0.076 |
| HDL-C (mmol/l) | 1.37±0.33 | 1.41±0.37 | <0.001 |
| LDL-C (mmol/l) | 3.26±0.84 | 3.25±0.85 | 0.407 |
| FPG (mmol/l) | 6.12±1.93 | 6.10±1.67 | 0.021 |
| Number (%) | |||
| Age | |||
| 60- | 697 (30.7) | 360 (17.4) | <0.001 |
| 65- | 753 (33.1) | 392 (18.9) | |
| 70- | 525 (23.1) | 589 (28.4) | |
| 75- | 297 (13.1) | 733 (35.3) | |
| Male | 943 (41.5) | 839 (40.5) | 0.481 |
| Married | 1908 (84.0) | 1750 (84.4) | 0.719 |
| Education ≥7 years | 1310 (57.7) | 1496 (72.1) | <0.001 |
| Physical exercise ≥1 (h/d) | 1676 (73.8) | 1780 (85.8) | <0.001 |
| Current drinker | 325 (14.3) | 418 (20.2) | <0.001 |
| Current smoker | 350 (15.4) | 230 (11.1) | <0.001 |
| Family history of hypertension | 780 (34.3) | 806 (38.9) | 0.002 |
| Doctor-diagnosed CVD | 1085 (47.8) | 656 (31.6) | <0.001 |
Prevalence of pre-hypertension and hypertension
Table 2 shows the crude age- and sex-standardized prevalence of optimal blood pressure; pre-hypertension; hypertension; and the awareness, treatment and control of hypertension among females and males in the two surveys from 2001 and 2010.
Table 2. Prevalence of pre-hypertension and the prevalence, awareness, treatment and control of hypertension among females and males who completed the surveys in 2001 and 2010.
| Total | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 (n = 2272) | 2010 (n = 2074) | P-value | 2001 (n = 943) | 2010 (n = 839) | P-value | 2001 (n = 1329) | 2010 (n = 1235) | P-value | P-value* | P-value# | |
| Crude prevalence | |||||||||||
| Current | |||||||||||
| Optimal | 289 (12.7) | 171 (8.2) | <0.001 | 118 (12.5) | 71 (8.5) | 0.006 | 171 (12.9) | 100 (8.1) | <0.001 | 0.803 | 0.767 |
| Pre-hypertension | 625 (27.5) | 494 (23.8) | 0.005 | 263 (27.9) | 228 (27.2) | 0.736 | 362 (27.2) | 266 (21.5) | 0.001 | 0.732 | 0.003 |
| Hypertension | 1358 (59.8) | 1409 (67.9) | <0.001 | 562 (59.6) | 540 (64.4) | 0.039 | 796 (59.9) | 869 (70.4) | <0.001 | 0.887 | 0.004 |
| Awareness | 953 (70.2) | 1058 (75.1) | 0.004 | 387 (68.9) | 388 (71.9) | 0.277 | 566 (71.1) | 670 (77.1) | 0.005 | 0.373 | 0.027 |
| Treatment | 693 (51.0) | 945 (67.1) | <0.001 | 284 (50.5) | 347 (64.3) | <0.001 | 409 (51.4) | 598 (68.8) | <0.001 | 0.758 | 0.077 |
| Control | 209 (15.4) | 417 (29.6) | <0.001 | 95 (16.9) | 168 (31.1) | <0.001 | 114 (14.3) | 249 (28.7) | <0.001 | 0.194 | 0.326 |
| Age- and sex-adjusted prevalence | |||||||||||
| Current | |||||||||||
| Optimal | 12.7 (11.3–14.1) | 9.3 (8.1–10.6) | <0.001 | 12.6 (10.5–14.7) | 9.9 (7.8–11.9) | 0.075 | 12.8 (11.0–14.6) | 9.0 (7.4–10.6) | 0.002 | 0.893 | 0.468 |
| Pre-hypertension | 27.2 (25.4–29.0) | 25.5 (23.6–27.4) | 0.207 | 28.0 (25.1–30.9) | 29.6 (26.5–32.7) | 0.448 | 26.7 (24.3–29.0) | 22.7 (20.4–25.1) | 0.021 | 0.495 | <0.001 |
| Hypertension | 60.1 (58.1–62.1) | 65.2 (63.1–67.2) | 0.001 | 59.4 (56.3–62.6) | 60.5 (57.2–63.9) | 0.628 | 60.6 (57.9–63.2) | 68.3 (65.7–70.9) | <0.001 | 0.597 | <0.001 |
| Awareness | 69.8 (67.4–72.3) | 74.5 (72.2–76.8) | 0.007 | 68.7 (64.8–72.6) | 72.0 (68.1–75.9) | 0.231 | 70.6 (67.5–73.8) | 76.0 (73.1–78.9) | 0.013 | 0.464 | 0.108 |
| Treatment | 50.6 (47.9–53.2) | 66.4 (63.9–68.9) | <0.001 | 50.3 (46.2–54.5) | 63.7 (59.5–67.9) | <0.001 | 50.7 (47.3–54.2) | 68.0 (64.9–71.2) | <0.001 | 0.863 | 0.100 |
| Control | 15.3 (13.4–17.2) | 30.0 (27.5–32.4) | <0.001 | 16.9 (13.8–20.0) | 31.1 (27.0–35.1) | <0.001 | 14.2 (11.8–16.6) | 29.3 (26.2–32.4) | <0.001 | 0.187 | 0.486 |
* 2001: male vs. female
# 2010: male vs. female
From 2001 to 2010, the proportion of the population with optimal blood pressure decreased significantly, and the age- and sex-standardized prevalence of pre-hypertension decreased from 27.2% to 25.5%, particularly in females (26.7% to 22.7%, P = 0.021). Additionally, the prevalence of hypertension significantly increased from 60.1% to 65.2% (P = 0.001), particularly in females (60.6% to 68.3%, P<0.001). Males had a higher prevalence of pre-hypertension (29.6% for males vs. 22.7% for females in 2010, P<0.001), and females had a higher prevalence of hypertension (60.5% for males vs. 68.3% for females in 2010, P<0.001), particularly in 2010. There were no significant sex differences in pre-hypertension and hypertension prevalence in 2001, but the trend was similar to that in 2010.
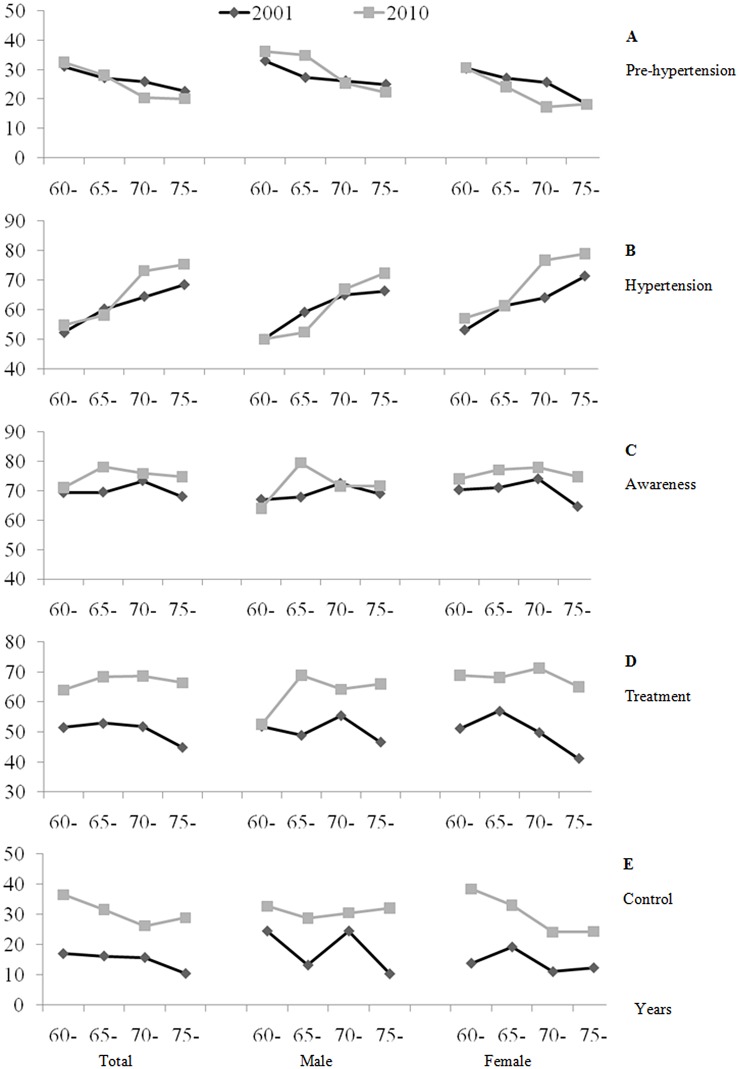
After stratifying the participants into four age groups, the results indicated that the prevalence of pre-hypertension decreased with age and that hypertension markedly increased with age. The greatest decline and increment were in the subgroup of those aged 65–69 years in both sexes (Fig 1A and 1B). As shown in Fig 1B, the age-specific prevalence of hypertension increased in all age groups from the 2001 to the 2010 survey, except for those aged 65–69 years. From 2001 to 2010, the prevalence of hypertension was highest among the subgroup of participants aged ≥70 years in both sexes.
Fig 1. Age-specific prevalence of pre-hypertension and the prevalence, awareness, treatment and control of hypertension.
Fig 1 shows the age-specific prevalence of (A). prehypertension (B). prevalence (C). awareness (D). treatment and (E). control of hypertension.
Awareness, treatment and control of hypertension
Among the participants who had hypertension, 69.8% were aware of their condition in 2001, and this rate significantly increased to 74.5% in 2010 (P = 0.007), particularly in females (from 70.6% to 76.0%, P = 0.013).
From 2001 to 2010, there was a significant increase in hypertensive patients receiving treatment both in males (50.3% to 63.7%, P<0.001) and females (50.7% to 68.0%, P<0.001).
In 2001, only 15.3% of patients with hypertension had controlled their blood pressure to reach the optimal range, but in 2010, this proportion approximately doubled to 30.3% (31.1% for males and 29.3% for females, both P<0.001).
The age-specific subgroups in both sexes indicated that the participants aged 60–64 years and ≥75 years had both the lowest hypertension awareness and treatment rates in both surveys (Fig 1C and 1D). In 2010, the participants aged 60–64 years had the highest hypertension control rate (Fig 1E).
Factors associated with awareness, treatment and control of hypertension
The logistic regression model analysis results of factors associated with hypertension awareness, treatment and control in 2001 and 2010 are shown in Table 3. A higher education level, a higher BMI, a family history of hypertension and doctor-diagnosed CVD were all significantly associated with hypertension awareness and treatment in both 2001 and 2010. A lower age, a higher education level and doctor-diagnosed CVD were significantly associated with hypertension control in 2001. We also found that a lower BMI and a family history of hypertension were significantly associated with hypertension control in 2010.
Table 3. Factors associated with the awareness, treatment and control of hypertension in two surveys, 2001 and 2010.
| Awareness | Treatment | Control | ||||
|---|---|---|---|---|---|---|
| 2001 (n = 1358) OR (95% CI) | 2010 (n = 1409) OR (95% CI) | 2001 (n = 1358) OR (95% CI) | 2010 (n = 1409) OR (95% CI) | 2001 (n = 1358) OR (95% CI) | 2010 (n = 1409) OR (95% CI) | |
| Age | ||||||
| 60- | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 65- | 1.04 (0.75–1.45) | 1.57 (0.99–2.49) | 1.15 (0.85–1.55) | 1.36 (0.89–2.08) | 0.88 (0.60–1.30) | 0.83 (0.55–1.25) |
| 70- | 1.28 (0.90–1.84) | 1.38 (0.91–2.08) | 1.09 (0.79–1.51) | 1.45 (0.98–2.13) | 0.89 (0.58–1.35) | 0.64 (0.44–0.94)* |
| 75- | 1.10 (0.72–1.69) | 1.29 (0.85–1.94) | 0.90 (0.61–1.34) | 1.30 (0.89–1.91) | 0.54 (0.31–0.96)* | 0.72 (0.49–1.04) |
| P for trend | 0.53 | 0.27 | 0.46 | 0.30 | 0.21 | 0.13 |
| Female | 1.06 (0.79–1.42) | 1.22 (0.90–1.65) | 1.10 (0.84–1.42) | 1.25 (0.95–1.66) | 0.87 (0.61–1.23) | 0.92 (0.70–1.22) |
| Married | 0.92 (0.65–1.30) | 0.80 (0.55–1.16) | 0.90 (0.66–1.24) | 0.87 (0.63–1.22) | 1.24 (0.78–1.97) | 0.80 (0.57–1.12) |
| Education ≥7 years | 1.36 (1.04–1.79)* | 1.32 (0.98–1.77) | 1.93 (1.51–2.47)*** | 1.73 (1.32–2.26)*** | 1.43 (1.02–1.99)* | 1.75 (1.31–2.33)*** |
| Physical exercise ≥1 (h/d) | 1.11 (0.84–1.46) | 0.82 (0.56–1.20) | 1.04 (0.81–1.34) | 0.82 (0.58–1.16) | 1.02 (0.73–1.44) | 0.93 (0.66–1.30) |
| BMI (kg/m2) | 1.10 (1.06–1.14)*** | 1.05 (1.01–1.09)* | 1.08 (1.05–1.12)*** | 1.02 (0.99–1.06) | 1.01 (0.97–1.06) | 0.95 (0.92–0.99)** |
| Current smokers | 0.82 (0.57–1.17) | 1.07 (0.70–1.64) | 0.81 (0.58–1.14) | 0.82 (0.56–1.21) | 1.30 (0.85–1.99) | 0.74 (0.48–1.14) |
| Current drinker | 0.91 (0.63–1.31) | 0.79 (0.56–1.11) | 0.86 (0.61–1.20) | 0.99 (0.72–1.36) | 0.73 (0.46–1.16) | 1.17 (0.85–1.62) |
| Family history of hypertension | 2.07 (1.59–2.70)*** | 2.37 (1.80–3.12)*** | 1.58 (1.25–1.99)*** | 2.22 (1.74–2.84)*** | 1.05 (0.77–1.42) | 1.36 (1.07–1.72)* |
| Doctor diagnosed CVD | 2.43 (1.90–3.12)*** | 2.55 (1.90–3.43)*** | 1.79 (1.43–2.25)*** | 2.26 (1.75–2.93)*** | 1.75 (1.28–2.40)*** | 1.52 (1.19–1.94)** |
*** P<0.001;
** P<0.01;
* P<0.05
Sensitivity analysis
After excluding the data of the 731 participants who were included in both surveys, we assessed the subject characteristics and the prevalence, awareness, treatment and control of hypertension in 2001 and 2010 (S1 and S2 Tables), and the results were similar to those reported above. According to the new treatment blood pressure goal (JNC-8) of the elderly participants [29], the control rate of hypertension significantly increased from 25.3% in 2001 to 36.9% in 2010 (S3 Table).
Discussion
To our knowledge, the present study is the first to report the trends of pre-hypertension prevalence and hypertension prevalence, awareness, treatment and control in the past decade in an elderly population in Beijing, China. Two cross-sectional surveys were conducted with participants aged ≥60 years in the same district and using the same methods in both 2001 and 2010. The results showed that the age- and sex-standardized prevalence of pre-hypertension decreased and that the prevalence, awareness, treatment and control of hypertension all increased significantly from 2001 to 2010.
The upward trends in age- and sex-standardized prevalence of hypertension (from 60.1% in 2001 to 65.2% in 2010) found in the current study are consistent with the results of previous studies in China. Among participants aged ≥60 years, Xi et al. reported that the prevalence of hypertension increased from 48.4% in 1991 to 53% in 2009 in nine provinces in China [16]. Zhao et al. reported that the prevalence of hypertension increased from 42.2% in 1999 to 70.8% in 2007 in Shandong Province [13], and the prevalence of hypertension in a northern Chinese population increased from 68.6% in 1991 to 71.2% in 2011 [14]. However, the prevalence of hypertension in US elderly individuals has been relatively stable over the past decade [31, 32], and the prevalences of hypertension in the present study of participants aged ≥75 years (75.4%) and ≥60 years (65.2%) in 2010 are similar to those reported in the US. Bromfield et al. reported that 76.5% of US adults ≥80 years had hypertension in 2005–2010 [17], and Guo et al. reported that the prevalence of hypertension was 66.7% among US adults ≥60 years in 2009 and 2010 [31].
From 2001 to 2010, the prevalence of pre-hypertension decreased, whereas the prevalence of hypertension increased with increasing age, which is consistent with other studies [13, 15 33, 34]. Males had a higher prevalence of pre-hypertension but a lower prevalence of hypertension, particularly in 2010, demonstrating a trend similar to that reported for the subgroup aged 65–74 by Gu et al. [28]. These results indicate that females in the aging population might have an increased chance of developing hypertension if they are pre-hypertensive. Whether gender influences the progression of pre-hypertension to hypertension among elderly people might be an interesting topic to explore with a larger sample size in the future.
Among the participants with hypertension, the awareness, treatment and control of hypertension all significantly increased from 69.8% to 74.5%, 50.3% to 63.7%, and 15.3% to 30.3%, respectively, from 2001 to 2010. These rates are higher than those of Xi et al [16], who reported increases of 38.7% to 54.3% for awareness, 30.5% to 49.0% for treatment, and 6.1% to 12.0% to control from 2000 to 2009 among participants aged ≥60 years. The rates found in the present study are also higher than those of Zhao et al [15], who reported increases of 39.1% to 49.2% for awareness, 28.1% to 43.4% for treatment, and 4.4% to 7.1% for control from 1999 to 2007 among all age groups. Furthermore, the rates of the present study are higher than those of a 2007 southeast Asian study of 19,848 participants aged ≥65 years [35]. Both the increase in the education level of our population in the past decade (from 57.7% to 72.1%) and preventive measures from the government and health professionals during this time might have contributed to the increases in awareness, treatment and control of hypertension. However, the prevalence remained lower than in the US elderly population (73.4% to 84.0% for awareness, 72.4% to 85.3% for treatment, and 34.1% to 54.9% for control from 2001 to 2010) [31] and in participants aged ≥65 years in Macau, China (79%, 75% and 35% for awareness, treatment and control, respectively, in 2012) [11]. Given the rapid social and economic changes occurring in China, public health strategies should be developed to meet the need of the aging population in China, particularly by providing more effective pharmacologic interventions aimed at elderly hypertensive patients.
Previous studies have found that older age and a higher BMI are associated with greater hypertension awareness and treatment but poorer hypertension control, which is in accordance with the current report [8, 9, 36–39]. A family history of hypertension is also significantly associated with greater hypertension awareness, treatment and control [8, 9, 40]. Participants who know their high risk of hypertension pay special attention to their blood pressure. Other studies have reported that being female, being retired, being married and cigarette smoking are all related to hypertension awareness, treatment and control, [8, 10, 39], although these variables did not reach statistical significance in the present study. We found that more females than males were both aware of their hypertension condition and received treatment, but the percentage of controlled hypertension was slightly lower among females than among males. The associations between education level and hypertension awareness, treatment and control are inconsistent among previous studies. A multi-ethnic Asian population study [39] and Wang et al. [9] reported that high education levels were associated with poor hypertension awareness and treatment, but Tian et al. [33] reported that increased awareness and treatment were found among those with high education levels, which is consistent with the findings of the present study. The differences among populations might be partially attributed to differences in education level; thus, a larger sample size is required to detect more factors associated with hypertension in future research. We also found that diagnosed CVD was significantly associated with hypertension awareness, treatment and control, indicating that the control of hypertension is a key treatment for patients who are diagnosed with CVD and that lowering blood pressure can significantly reduce the risk of cardiovascular events [41].
The age of the urban elderly population increased significantly over the decade evaluated in the current study. We previously found the same result in other areas of China [13–15], which suggests the aging of the population. The percentage of individuals more than 60 years old has dramatically increased during this time, and China has entered into an aging society [42, 43]. With the increased aging of the population, China is facing many challenges in adequately meeting the medical demand for chronic disease treatment [44]. The prevalence of multiple chronic conditions (MCC) among individuals increases with age: the older the population, the greater the prevalence of MCC [45]. In the present study, we found that elderly people aged 60–64 years had fewer coexisting diseases than did those greater than 65 years old (data not shown), the latter of which increases the difficulty of treatment and control of hypertension. This may explain the higher control rate of hypertension in the relatively younger elderly population.
The present study has some limitations. First, because of the characteristics of cross-sectional studies, we could only observe the prevalence of hypertension at the two survey times and, thus, cannot infer causation. Second, we did not collect detailed information on diet, such as the amount of salt consumed. Therefore, we were unable to detect relationships between diet conditions and hypertension prevalence rates. Third, we measured blood pressure during a single visit, which might overestimate or underestimate the true prevalence of hypertension [15]. Fourth, we found that the mean age of participants in 2010 was significantly higher than that in 2001 and that the prevalence of hypertension significantly increased with age. Although the age-specific prevalence of hypertension approximately increased in all age groups, age might also be a confounding factor in the present study. Although we adjusted several potential confounding variables in the current analysis, differences between surveys in age and other unmeasured covariates might have affected the results of the present study. As Beijing is the capital of China, residents of this city might be more educated and wealthy than those in rural areas, and they might pay more attention to their health. These characteristics could explain the higher hypertension awareness, treatment and control rates in Beijing compared with other areas. Prospective studies with larger sample sizes are required to examine the causes of the trends of pre-hypertension and hypertension prevalence, awareness, treatment and control in the elderly population in the future.
In conclusion, according to two cross-sectional surveys, hypertension prevalence increased rapidly over the past decade among urban elderly residents in Beijing, northern China. Although the awareness, treatment and control of hypertension improved significantly, they remain low. We should pay greater attention to the elderly, as population aging is occurring worldwide. Thus, urgent action, optimal treatment approaches and proper public health strategies are needed for the prevention and management of hypertension, with the ultimate goal of lowering the incidence of hypertension-related chronic diseases.
Supporting Information
It contains the raw data of 4,346 participants (2,272 participants in 2001 and 2,074 participants in 2010) with 22 variables. Including investigation year (2001, 2010), code, gender (male, female), age, education years (0–6, 7–9, 10–12, 13–16, ≥17 years), marriage status (married, single, divorce, widowed), height (m), weight (kg), waist (cm), hip (cm), SBP (mmHg), DBP (mmHg), TC (mmol/l), TG (mmol/l), HDL-C (mmol/l), LDL-C (mmol/l), FPG (mmol/l), physical exercise (< 1 h/d, ≥1 h/d), smoking status, drinking status, family history of hypertension and doctor-diagnosed CVD.
(XLS)
S1 Table shows the subject characteristics in 2001 and 2010, after excluding the data of the 731 participants who were included in both surveys.
(DOC)
(DOC)
S3 Table shows the control rate of hypertension, according to the new treatment blood pressure goal (JNC-8) of the elderly participants.
(DOC)
Acknowledgments
We thank Drs. Y Jiang, Q Chang, K Feng and WY Kang for research assistance with field work.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by research grants from the National Natural Science Foundation of China, 81373080; Ministry of Science and Technology of China, 2013CB530800; Research Foundation by the Ministry of Health of PLA China, 13CXZ029 and the Beijing Municipal Science and Technology Commission, D121100004912003.
References
- 1. World Health Organization Report 1999 (1999) Making a Difference. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2. World Health Organization report 2008 (2008) Primary health care (now more than ever). World Health Organization, Geneva, Switzerland. [Google Scholar]
- 3. Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, et al. (2003) Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA 289:2363–2369. [DOI] [PubMed] [Google Scholar]
- 4. Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlöf B, et al. (2010) Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol 9:469–480. 10.1016/S1474-4422(10)70066-1 [DOI] [PubMed] [Google Scholar]
- 5. Sun Z, Zheng L, Wei Y, Li J, Zhang X, Liu S, et al. (2007) The prevalence of prehypertension and hypertension among rural adults in Liaoning province of China. Clin Cardiol 30:183–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li H, Meng Q, Sun X, Salter A, Briggs NE, Hiller JE (2010) Prevalence, awareness, treatment, and control of hypertension in rural China: results from Shandong Province. J Hypertens 28:432–438. 10.1097/HJH.0b013e328334b39e [DOI] [PubMed] [Google Scholar]
- 7. Cai L, Liu A, Zhang L, Li S, Wang P (2012) Prevalence, awareness, treatment, and control of hypertension among adults in Beijing, China. Clin Exp Hypertens 34:45–52. 10.3109/10641963.2011.618206 [DOI] [PubMed] [Google Scholar]
- 8. Meng XJ, Dong GH, Wang D, Liu MM, Lin Q, Tian S, et al. (2011) Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens 29:1303–1310. 10.1097/HJH.0b013e328347f79e [DOI] [PubMed] [Google Scholar]
- 9. Wang H, Zhang X, Zhang J, He Q, Hu R, Wang L, et al. (2013) Factors associated with prevalence, awareness, treatment and control of hypertension among adults in Southern China: a community-based, cross-sectional survey. PLoS One 8:e62469 10.1371/journal.pone.0062469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ma WJ, Tang JL, Zhang YH, Xu YJ, Lin JY, Li JS, et al. (2012) Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens 25:590–596. 10.1038/ajh.2012.11 [DOI] [PubMed] [Google Scholar]
- 11. Ke L, Ho J, Feng J, Mpofu E, Dibley MJ, Li Y, et al. (2015) Prevalence, awareness, treatment and control of hypertension in Macau: results from a cross-sectional epidemiological study in Macau, China. Am J Hypertens 28:159–165. 10.1093/ajh/hpu121 [DOI] [PubMed] [Google Scholar]
- 12. Sheng CS, Liu M, Kang YY, Wei FF, Zhang L, Li GL, et al. (2013) Prevalence, awareness, treatment and control of hypertension in elderly Chinese. Hypertension Research 36:824–828. 10.1038/hr.2013.57 [DOI] [PubMed] [Google Scholar]
- 13. Zhao Y, Lu F, Sun H, Liu Z, Zhao Y, Sun S, et al. (2012) Trends in hypertension prevalence, awareness, treatment, and control rates in Shandong Province of China. J Clin Hypertens (Greenwich) 14:637–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang J, Ning X, Yang L, Lu H, Tu J, Jin W, et al. (2014) Trends of hypertension prevalence, awareness, treatment and control in rural areas of northern China during 1991–2011. J Hum Hypertens 28:25–31. 10.1038/jhh.2013.44 [DOI] [PubMed] [Google Scholar]
- 15. Zhao Y, Yan H, Marshall RJ, Dang S, Yang R, Li Q, et al. (2013) Trends in population blood pressure and prevalence, awareness, treatment, and control of hypertension among middle-aged and older adults in a rural area of Northwest China from 1982 to 2010. PLoS One 8:e61779 10.1371/journal.pone.0061779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Xi B, Liang Y, Reilly KH, Wang Q, Hu Y, Tang W (2012) Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991–2009. Int J Cardiol 158:326–329. 10.1016/j.ijcard.2012.04.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bromfield SG, Bowling CB, Tanner RM, Peralta CA, Odden MC, Oparil S, et al. (2014) Trends in hypertension prevalence, awareness, treatment, and control among US adults 80 years and older, 1988–2010. J Clin Hypertens (Greenwich) 16:270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S (2007) Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc 55:1056–1065. [DOI] [PubMed] [Google Scholar]
- 19.Population division of the department of economic and social affairs of the United Nations secretariat, World Population Prospects: The 2010 revision [on-line]. Available at http://esa.un.org/unpd/wpp/unpp/panel_population.htm Accessed March 10, 2013.
- 20. He Y, Jiang B, Wang J, Feng K, Chang Q, Fan L, et al. (2006) Prevalence of the metabolic syndrome and its relation to cardiovascular disease in an elderly Chinese population. J Am Coll Cardiol 47:1588–1594. [DOI] [PubMed] [Google Scholar]
- 21.People’ s republic of China ministry of health disease control division. Overweight and obesity prevention and control guidelines in Chinese adults [R]. 2003 (in Chinese)
- 22. Yang GH, Li Q, Wang CX, Hsia J, Yang Y, Xiao L, et al. (2010) Findings from 2010 Global Adult Tobacco Survey: implementation of MPOWER policy in China. Biomed Environ Sci 23:422–429. 10.1016/S0895-3988(11)60002-0 [DOI] [PubMed] [Google Scholar]
- 23. Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310: 948–959. 10.1001/jama.2013.168118 [DOI] [PubMed] [Google Scholar]
- 24. Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. (1993) Human blood pressure determination by sphygmomanometry. Circulation. 88:2460–2470. [DOI] [PubMed] [Google Scholar]
- 25. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. (2003) Seventh report of joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 26. Wang Y, Wang QJ (2004) The prevalence of prehypertension and hypertension among US adults according to new joint national guidelines. Arch Intern Med 164: 2126–2134. [DOI] [PubMed] [Google Scholar]
- 27. WHO (2001) Prevalence, awareness, treatment and control of hypertension among the elderly in Bangladesh and India: a multicentre study. Bull World Health Organ 179:490–500. [PMC free article] [PubMed] [Google Scholar]
- 28. Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, et al. (2002) Prevalence, awareness, treatment, and control of hypertension in china. Hypertension 40:920–927. [DOI] [PubMed] [Google Scholar]
- 29. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. (2014) 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel member`1s appointed to the Eighth Joint National Committee (JNC 8). JAMA 311:507–520. 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 30.Ministry of health of the people's republic of China. Available: http://wsbmohgovcn/zwgkzt/ptjnj/listshtml.
- 31. Guo F, He D, Zhang W, Walton RG (2012) Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol 60:599–606. 10.1016/j.jacc.2012.04.026 [DOI] [PubMed] [Google Scholar]
- 32. Egan BM, Zhao Y, Axon RN (2010) US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 303:2043–2050. 10.1001/jama.2010.650 [DOI] [PubMed] [Google Scholar]
- 33. Chiu YH, Wu SC, Tseng CD, Yen MF, Chen TH (2006) Progression of pre-hypertension, stage 1 and 2 hypertension (JNC 7): a population-based study in Keelung, Taiwan (Keelung Community-based Integrated Screening No. 9). J Hypertens 24:821–828. [DOI] [PubMed] [Google Scholar]
- 34. Le C, Jun D, Yichun L, Zhankun S, Keying Z (2011) Multilevel analysis of the determinants of pre-hypertension and hypertension in rural southwest China. Public Health Rep 126:420–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Joshi V, Lim J, Nandkumar M (2007) Prevalence and risk factors of undetected elevated blood pressure in an elderly Southeast Asian population. Asia Pac J Public Health 19:3–9. [DOI] [PubMed] [Google Scholar]
- 36. Agyemang C, Bruijnzeels MA, Owusu-Dabo E (2006) Factors associated with hypertension awareness, treatment, and control in Ghana, West Africa. J Hum Hypertens 20:67–71. [DOI] [PubMed] [Google Scholar]
- 37. Agyemang C, van Valkengoed I, Koopmans R, Stronks K (2006) Factors associated with hypertension awareness, treatment and control among ethnic groups in Amsterdam, the Netherlands: the SUNSET study. J Hum Hypertens 20: 874–881. [DOI] [PubMed] [Google Scholar]
- 38. Chen R, Tunstall-Pedoe H, Morrison C, Connaghan J, A Brook R (2003) Trends and social factors in blood pressure control in Scottish MONICA surveys 1986–1995: the rule of halves revisited. J Hum Hypertens 17:751–759. [DOI] [PubMed] [Google Scholar]
- 39. Wu Y, Tai ES, Heng D, Tan CE, Low LP, Lee J (2009) Risk factors associated with hypertension awareness, treatment, and control in a multi-ethnic Asian population. J Hypertens 27:190–197. [DOI] [PubMed] [Google Scholar]
- 40. Tian S, Dong GH, Wang D, Liu MM, Lin Q, Meng XJ, et al. (2011) Factors associated with prevalence, awareness, treatment and control of hypertension in urban adults from 33 communities in China: the CHPSNE Study. Hypertens Res 34:1087–1092. 10.1038/hr.2011.99 [DOI] [PubMed] [Google Scholar]
- 41. Staessen JA, Gasowski J, Wang JG, Thijs L, Den Hond E, Boissel JP, et al. (2000) Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 355:865–872. [DOI] [PubMed] [Google Scholar]
- 42. Smith JP, Strauss J, Zhao Y (2014) Healthy Aging in China. J Econ Ageing 4:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Teng H, Cao Z, Liu J, Liu P, Hua W, Yang Y, Xiong L (2015) Health status and burden of health care costs among urban elderly in china. Asia Pac J Public Health 27:61S–8S. 10.1177/1010539515571579 [DOI] [PubMed] [Google Scholar]
- 44. Parekh AK, Goodman RA, Gordon C, Koh HK; HHS Interagency Workgroup on Multiple Chronic Conditions (2011) Managing multiple chronic conditions: a strategic framework for improving health outcomes and quality of life. Public Health Rep 126:460–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Anderson G, Horvath J (2004) The growing burden of chronic disease in America. Public Health Rep 119:263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
It contains the raw data of 4,346 participants (2,272 participants in 2001 and 2,074 participants in 2010) with 22 variables. Including investigation year (2001, 2010), code, gender (male, female), age, education years (0–6, 7–9, 10–12, 13–16, ≥17 years), marriage status (married, single, divorce, widowed), height (m), weight (kg), waist (cm), hip (cm), SBP (mmHg), DBP (mmHg), TC (mmol/l), TG (mmol/l), HDL-C (mmol/l), LDL-C (mmol/l), FPG (mmol/l), physical exercise (< 1 h/d, ≥1 h/d), smoking status, drinking status, family history of hypertension and doctor-diagnosed CVD.
(XLS)
S1 Table shows the subject characteristics in 2001 and 2010, after excluding the data of the 731 participants who were included in both surveys.
(DOC)
(DOC)
S3 Table shows the control rate of hypertension, according to the new treatment blood pressure goal (JNC-8) of the elderly participants.
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.